Fosfomycin Tromethamine
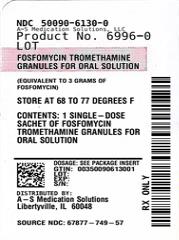
Fosfomycin Tromethamine Granules for Oral Solution Rx only
6b9167a9-80e9-44e1-a609-c3eb78960acf
HUMAN PRESCRIPTION DRUG LABEL
Nov 1, 2023
A-S Medication Solutions
DUNS: 830016429
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Fosfomycin Tromethamine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
FOSFOMYCIN TROMETHAMINE
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
Clinical Trials:
In clinical studies, drug related adverse events which were reported in greater than 1% of the fosfomycin-treated study population are listed below:
|
Drug-Related Adverse Events (%) in Fosfomycin and Comparator Populations | ||||
|
Adverse Events |
Fosfomycin N=1233 |
Nitrofurantoin N=374 |
Trimethoprim/ sulfamethoxazole N=428 |
Ciprofoxacin N=455 |
|
Diarrhea |
9.0 |
6.4 |
2.3 |
3.1 |
|
Vaginitis |
5.5 |
5.3 |
4.7 |
6.3 |
|
Nausea |
4.1 |
7.2 |
8.6 |
3.4 |
|
Headache |
3.9 |
5.9 |
5.4 |
3.4 |
|
Dizziness |
1.3 |
1.9 |
2.3 |
2.2 |
|
Asthenia |
1.1 |
0.3 |
0.5 |
0.0 |
|
Dyspepsia |
1.1 |
2.1 |
0.7 |
1.1 |
In clinical trials, the most frequently reported adverse events occurring in greater than 1% of the study population regardless of drug relationship were: diarrhea 10.4%, headache 10.3%, vaginitis 7.6%, nausea 5.2%, rhinitis 4.5%, back pain 3.0%, dysmenorrheal 2.6%, pharyngitis 2.5%, dizziness 2.3%, abdominal pain 2.2%, pain 2.2%, dyspepsia 1.8%, asthenia 1.7%, and rash 1.4%.
The following adverse events occurred in clinical trials at a rate of less than 1%, regardless of drug relationship: abnormal stools, anorexia, constipation, dry mouth, dysuria, ear disorder, fever, flatulence, flu syndrome, hematuria, infection, insomnia, lymphadenopathy, menstrual disorder, migraine, myalgia, nervousness, paresthesia, pruritus, SGPT increased, skin disorder, somnolence, and vomiting.
One patient developed unilateral optic neuritis, an event considered possibly related to fosfomycin tromethamine therapy.
Post-marketing Experience:
Serious adverse events from the marketing experience with fosfomycin tromethamine outside of the United States have been rarely reported and include: angioedema, aplastic anemia, asthma (exacerbation), cholestatic jaundice, hepatic necrosis, and toxic megacolon.
Although causality has not been established, during post marketing surveillance, the following events have occurred in patients prescribed fosfomycin tromethamine: anaphylaxis and hearing loss.
Laboratory Changes:
Significant laboratory changes reported in U.S. clinical trials of fosfomycin tromethamine without regard to drug relationship include: increased eosinophil count, increased or decreased WBC count, increased bilirubin, increased SGPT, increased SGOT, increased alkaline phosphatase, decreased hematocrit, decreased hemoglobin, increased and decreased platelet count. The changes were generally transient and were not clinically significant.
CLINICAL STUDIES SECTION
CLINICAL STUDIES
In controlled, double-blind studies of acute cystitis performed in the United States, a single-dose of fosfomycin tromethamine was compared to three other oral antibiotics (See table below). The study population consisted of patients with symptoms and signs of acute cystitis of less than 4 days duration, no manifestations of upper tract infection (e.g., flank pain, chills, fever), no history of recurrent urinary tract infections (20% of patients in the clinical studies had a prior episode of acute cystitis within the preceding year), no known structural abnormalities, no clinical or laboratory evidence of hepatic dysfunction, and no known or suspected CNS disorders, such as epilepsy, or other factors which would predispose to seizures. In these studies, the following clinical success (resolution of symptoms) and microbiologic eradication rates were obtained.
|
Treatment Arm |
Treatment Duration (days) |
Microbiologic Eradication Rate |
Clinical Success Rate |
Outcome | |
|
5 to 11 days |
Study day | ||||
|
Fosfomycin |
1 |
630/771 (82%) |
591/771 (77%) |
542/771 (70%) | |
|
Ciprofloxacin |
7 |
219/222 (98%) |
219/222 (98%) |
213/222 (96%) |
Fosfomycin inferior to ciprofloxacin |
|
Trimethoprim/ sulfamethoxazole |
10 |
194/197 (98%) |
194/197 (98%) |
186/197 (94%) |
Fosfomycin inferior to trimethoprim/ sulfamethoxazole |
|
Nitrofurantoin |
7 |
180/238 (76%) |
180/238 (76%) |
183/238 (77%) |
Fosfomycin equivalent to nitrofurantoin |
|
Pathogen |
Fosfomycin 3 gram single dose |
Ciprofloxacin 250 mg bid x 7 days |
Trimethoprim/sulfamethoxazole 160 mg/800 mg bid x 10 days |
Nitrofurantoin 100 mg bid x 7 days |
|
E. coli |
509/644 (79%) |
184/187 (98%) |
171/174 (98%) |
146/187 (78%) |
|
E. faecalis |
10/10 (100%) |
0/0 |
4/4 (100%) |
1/2 (50%) |
