Olanzapine
These highlights do not include all the information needed to use OLANZAPINE TABLETS safely and effectively. See full prescribing information for OLANZAPINE TABLETS. OLANZAPINE tablets, for oral use Initial U.S. Approval: 1996
b7f27239-c22e-46d4-a313-50270cc19445
HUMAN PRESCRIPTION DRUG LABEL
Mar 5, 2024
REMEDYREPACK INC.
DUNS: 829572556
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Olanzapine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Drug Labeling Information
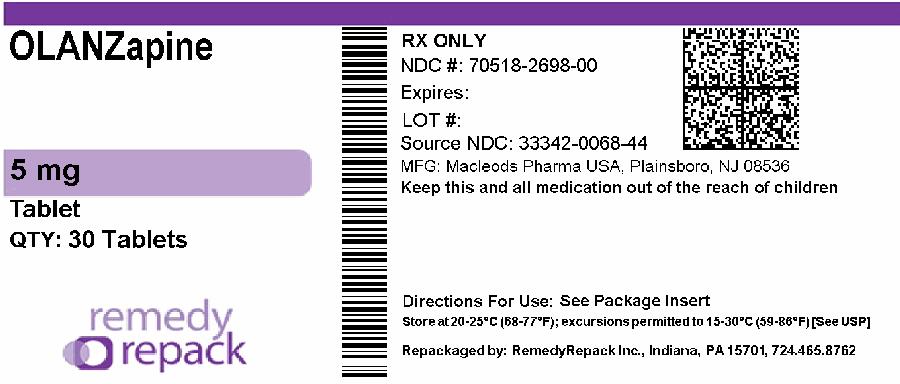
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
DRUG: Olanzapine
GENERIC: Olanzapine
DOSAGE: TABLET, FILM COATED
ADMINSTRATION: ORAL
NDC: 70518-2698-0
COLOR: white
SHAPE: ROUND
SCORE: No score
SIZE: 8 mm
IMPRINT: CL40
PACKAGING: 30 in 1 BLISTER PACK
ACTIVE INGREDIENT(S):
- OLANZAPINE 5mg in 1
INACTIVE INGREDIENT(S):
- CROSPOVIDONE
- HYDROXYPROPYL CELLULOSE, UNSPECIFIED
- MAGNESIUM STEARATE
- CELLULOSE, MICROCRYSTALLINE
- TITANIUM DIOXIDE
BOXED WARNING SECTION
**WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED
PSYCHOSIS**
INDICATIONS & USAGE SECTION
1 INDICATIONS & USAGE
1.1 Schizophrenia
Oral olanzapine tablets are indicated for the treatment of schizophrenia. Efficacy was established in three clinical trials in adult patients with schizophrenia: two 6-week trials and one maintenance trial. In adolescent patients with schizophrenia (ages 13-17), efficacy was established in one 6-week trial [see Clinical Studies ( 14.1)].
When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and dyslipidemia. Clinicians should consider the potential long-term risks when prescribing to adolescents, and in many cases this may lead them to consider prescribing other drugs first in adolescents [see Warnings and Precautions ( 5.5)].
1.2 Bipolar I Disorder (Manic or Mixed Episodes)
Monotherapy — Oral olanzapine tablets are indicated for the acute treatment of manic or mixed episodes associated with bipolar I disorder and maintenance treatment of bipolar I disorder. Efficacy was established in three clinical trials in adult patients with manic or mixed episodes of bipolar I disorder: two 3- to 4-week trials and one monotherapy maintenance trial. In adolescent patients with manic or mixed episodes associated with bipolar I disorder (ages 13-17), efficacy was established in one 3-week trial [see Clinical Studies ( 14.2)].
When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and dyslipidemia. Clinicians should consider the potential long-term risks when prescribing to adolescents, and in many cases this may lead them to consider prescribing other drugs first in adolescents [see Warnings and Precautions ( 5.5)].
Adjunctive Therapy to Lithium or Valproate — Oral olanzapine tablets are indicated for the treatment of manic or mixed episodes associated with bipolar I disorder as an adjunct to lithium or valproate. Efficacy was established in two 6-week clinical trials in adults. The effectiveness of adjunctive therapy for longer-term use has not been systematically evaluated in controlled trials [see Clinical Studies ( 14.2)].
1.3 Special Considerations in Treating Pediatric Schizophrenia and Bipolar
I Disorder
Pediatric schizophrenia and bipolar I disorder are serious mental disorders; however, diagnosis can be challenging. For pediatric schizophrenia, symptom profiles can be variable, and for bipolar I disorder, pediatric patients may have variable patterns of periodicity of manic or mixed symptoms. It is recommended that medication therapy for pediatric schizophrenia and bipolar I disorder be initiated only after a thorough diagnostic evaluation has been performed and careful consideration given to the risks associated with medication treatment. Medication treatment for both pediatric schizophrenia and bipolar I disorder should be part of a total treatment program that often includes psychological, educational and social interventions.
1.5 Olanzapine and Fluoxetine in Combination: Depressive Episodes
Associated with Bipolar I Disorder
Oral olanzapine and fluoxetine in combination is indicated for the treatment of depressive episodes associated with bipolar I disorder, based on clinical studies. When using olanzapine and fluoxetine in combination, refer to the Clinical Studies section of the package insert for Symbyax.
Olanzapine monotherapy is not indicated for the treatment of depressive episodes associated with bipolar I disorder.
1.6 Olanzapine and Fluoxetine in Combination: Treatment Resistant
Depression
Oral olanzapine and fluoxetine in combination is indicated for the treatment
of treatment resistant depression (major depressive disorder in patients who
do not respond to 2 separate trials of different antidepressants of adequate
dose and duration in the current episode), based on clinical studies in adult
patients. When using olanzapine and fluoxetine in combination, refer to the
Clinical Studies section of the package insert for Symbyax.
Olanzapine monotherapy is not indicated for the treatment of treatment
resistant depression.
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
• None with olanzapine tablets monotherapy.
• When using olanzapine and fluoxetine in combination, also refer to the
Contraindications section of the package insert for Symbyax.
• For specific information about the contraindications of lithium or
valproate, refer to the Contraindications section of the package inserts for
these other products.
• None with olanzapine monotherapy. ( 4)
• When using olanzapine and fluoxetine in combination, also refer to the
Contraindications section of the package insert for Symbyax®. ( 4)
• When using olanzapine in combination with lithium or valproate, refer to the
Contraindications section of the package inserts for those products. ( 4)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
The risks of using olanzapine in combination with other drugs have not been extensively evaluated in systematic studies
7.1 Potential for Other Drugs to Affect Olanzapine
Diazepam — The co-administration of diazepam with olanzapine potentiated the orthostatic hypotension observed with olanzapine [see Drug Interactions (7.2)].
Cimetidine and Antacids — Single doses of cimetidine (800 mg) or aluminum- and magnesium-containing antacids did not affect the oral bioavailability of olanzapine.
Inducers of CYP1A2 — Carbamazepine therapy (200 mg bid) causes an approximately 50% increase in the clearance of olanzapine. This increase is likely due to the fact that carbamazepine is a potent inducer of CYP1A2 activity. Higher daily doses of carbamazepine may cause an even greater increase in olanzapine clearance.
Alcohol — Ethanol (45 mg/70 kg single dose) did not have an effect on olanzapine pharmacokinetics. The co-administration of alcohol (i.e., ethanol) with olanzapine potentiated the orthostatic hypotension observed with olanzapine [see Drug Interactions (7.2)].
Inhibitors of CYP1A2
Fluvoxamine: Fluvoxamine, a CYP1A2 inhibitor, decreases the clearance of
olanzapine. This results in a mean increase in olanzapine C max following
fluvoxamine of 54% in female nonsmokers and 77% in male smokers. The mean
increase in olanzapine AUC is 52% and 108%, respectively. Lower doses of
olanzapine should be considered in patients receiving concomitant treatment
with fluvoxamine.
Inhibitors of CYP2D6
Fluoxetine: Fluoxetine (60 mg single dose or 60 mg daily dose for 8 days)
causes a small (mean 16%) increase in the maximum concentration of olanzapine
and a small (mean 16%) decrease in olanzapine clearance. The magnitude of the
impact of this factor is small in comparison to the overall variability
between individuals, and therefore dose modification is not routinely
recommended. When using olanzapine and fluoxetine in combination, also refer
to the Drug Interactions section of the package insert for Symbyax.
Warfarin — Warfarin (20 mg single dose) did not affect olanzapine pharmacokinetics [see Drug Interactions (7.2)].
Inducers of CYP1A2 or Glucuronyl Transferase — Omeprazole and rifampin may
cause an increase in olanzapine clearance.
Charcoal — The administration of activated charcoal (1 g) reduced the C max
and AUC of oral olanzapine by about 60%. As peak olanzapine levels are not
typically obtained until about 6 hours after dosing, charcoal may be a useful
treatment for olanzapine overdose.
Anticholinergic Drugs — Concomitant treatment with olanzapine and other drugs with anticholinergic activity can increase the risk for severe gastrointestinal adverse reactions related to hypomotility. Olanzapine should be used with caution in patients receiving medications having anticholinergic (antimuscarinic) effects [ see Warnings and Precautions (5.14)].
7.2 Potential for Olanzapine to Affect Other Drugs
CNS Acting Drugs — Given the primary CNS effects of olanzapine, caution should be used when olanzapine is taken in combination with other centrally acting drugs and alcohol.
Antihypertensive Agents — Olanzapine, because of its potential for inducing hypotension, may enhance the effects of certain antihypertensive agents.
Levodopa and Dopamine Agonists — Olanzapine may antagonize the effects of levodopa and dopamine agonists.
Lithium — Multiple doses of olanzapine (10 mg for 8 days) did not influence the kinetics of lithium. Therefore, concomitant olanzapine administration does not require dosage adjustment of lithium [see Warnings and Precautions (5.16)] .
Valproate — Olanzapine (10 mg daily for 2 weeks) did not affect the steady state plasma concentrations of valproate. Therefore, concomitant olanzapine administration does not require dosage adjustment of valproate [see Warnings and Precautions (5.16)] .
Effect of Olanzapine on Drug Metabolizing Enzymes — In vitro studies utilizing human liver microsomes suggest that olanzapine has little potential to inhibit CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A. Thus, olanzapine is unlikely to cause clinically important drug interactions mediated by these enzymes.
Imipramine — Single doses of olanzapine did not affect the pharmacokinetics of imipramine or its active metabolite desipramine.
Warfarin — Single doses of olanzapine did not affect the pharmacokinetics of warfarin [see Drug Interactions (7.1)].
Diazepam — Olanzapine did not influence the pharmacokinetics of diazepam or its active metabolite N-desmethyldiazepam. However, diazepam co-administered with olanzapine increased the orthostatic hypotension observed with either drug given alone [see Drug Interactions (7.1)].
Alcohol — Multiple doses of olanzapine did not influence the kinetics of ethanol [see Drug Interactions (7.1)].
Biperiden — Multiple doses of olanzapine did not influence the kinetics of biperiden.
Theophylline — Multiple doses of olanzapine did not affect the pharmacokinetics of theophylline or its metabolites.
• Diazepam: May potentiate orthostatic hypotension. ( 7.1, 7.2)
• Alcohol: May potentiate orthostatic hypotension. ( 7.1)
• Carbamazepine: Increased clearance of olanzapine. ( 7.1)
• Fluvoxamine: May increase olanzapine levels. ( 7.1)
• Olanzapine and Fluoxetine in Combination: Also refer to the Drug
Interactions section of the package insert for Symbyax. ( 7.1)
• CNS Acting Drugs: Caution should be used when taken in combination with
other centrally acting drugs and alcohol. ( 7.2)
• Antihypertensive Agents: Enhanced antihypertensive effect. ( 7.2)
• Levodopa and Dopamine Agonists: May antagonize levodopa/dopamine agonists. (
7.2)
• Other Concomitant Drug Therapy: When using olanzapine in combination with
lithium or valproate, refer to the Drug Interactions sections of the package
insert for those products. ( 7.2)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE & ADMINISTRATION
2.1 Schizophrenia
Adults
Dose Selection - Oral olanzapine should be administered on a once-a-day
schedule without regard to meals, generally beginning with 5 to 10 mg
initially, with a target dose of 10 mg/day within several days. Further dosage
adjustments, if indicated, should generally occur at intervals of not less
than 1 week, since steady state for olanzapine would not be achieved for
approximately 1 week in the typical patient. When dosage adjustments are
necessary, dose increments/decrements of 5 mg QD are recommended.
Efficacy in schizophrenia was demonstrated in a dose range of 10 to 15 mg/day in clinical trials. However, doses above 10 mg/day were not demonstrated to be more efficacious than the 10 mg/day dose. An increase to a dose greater than the target dose of 10 mg/day (i.e., to a dose of 15 mg/day or greater) is recommended only after clinical assessment. Olanzapine is not indicated for use in doses above 20 mg/day.
Dosing in Special Populations - The recommended starting dose is 5 mg in patients who are debilitated, who have a predisposition to hypotensive reactions, who otherwise exhibit a combination of factors that may result in slower metabolism of olanzapine (e.g., nonsmoking female patients ≥65 years of age), or who may be more pharmacodynamically sensitive to olanzapine [see Warnings and Precautions ( 5.14), Drug Interactions ( 7), and Clinical Pharmacology ( 12.3)] . When indicated, dose escalation should be performed with caution in these patients.
Maintenance Treatment - The effectiveness of oral olanzapine, 10 mg/day to 20 mg/day, in maintaining treatment response in schizophrenic patients who had been stable on olanzapine for approximately 8 weeks and were then followed for relapse has been demonstrated in a placebo-controlled trial [see Clinical Studies ( 14.1)] . The healthcare provider who elects to use olanzapine for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
Adolescents
Dose Selection- Oral olanzapine should be administered on a once-a-day schedule without regard to meals with a recommended starting dose of 2.5 or 5 mg, with a target dose of 10 mg/day. Efficacy in adolescents with schizophrenia was demonstrated based on a flexible dose range of 2.5 to 20 mg/day in clinical trials, with a mean modal dose of 12.5 mg/day (mean dose of 11.1 mg/day). When dosage adjustments are necessary, dose increments/decrements of 2.5 or 5 mg are recommended.
The safety and effectiveness of doses above 20 mg/day have not been evaluated in clinical trials [see Clinical Studies ( 14.1)].
Maintenance Treatment - The efficacy of olanzapine for the maintenance treatment of schizophrenia in the adolescent population has not been systematically evaluated; however, maintenance efficacy can be extrapolated from adult data along with comparisons of olanzapine pharmacokinetic parameters in adult and adolescent patients. Thus, it is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
2.2 Bipolar I Disorder (Manic or Mixed Episodes)
Adults
Dose Selection for Monotherapy - Oral olanzapine should be administered on a
once-a-day schedule without regard to meals, generally beginning with 10 or 15
mg. Dosage adjustments, if indicated, should generally occur at intervals of
not less than 24 hours, reflecting the procedures in the placebo-controlled
trials. When dosage adjustments are necessary, dose increments/decrements of 5
mg QD are recommended.
Short-term (3-4 weeks) antimanic efficacy was demonstrated in a dose range of 5 mg to 20 mg/day in clinical trials. The safety of doses above 20 mg/day has not been evaluated in clinical trials [see Clinical Studies ( 14.2)].
Maintenance Monotherapy - The benefit of maintaining bipolar I patients on monotherapy with oral olanzapine at a dose of 5 to 20 mg/day, after achieving a responder status for an average duration of 2 weeks, was demonstrated in a controlled trial [see Clinical Studies ( 14.2)] . The healthcare provider who elects to use olanzapine for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
Dose Selection for Adjunctive Treatment - When administered as adjunctive treatment to lithium or valproate, oral olanzapine dosing should generally begin with 10 mg once-a-day without regard to meals.
Antimanic efficacy was demonstrated in a dose range of 5 mg to 20 mg/day in clinical trials [see Clinical Studies ( 14.2)] . The safety of doses above 20 mg/day has not been evaluated in clinical trials.
Adolescents****
****Dose Selection - Oral olanzapine should be administered on a once-a-day
schedule without regard to meals with a recommended starting dose of 2.5 or 5
mg, with a target dose of 10 mg/day. Efficacy in adolescents with bipolar I
disorder (manic or mixed episodes) was demonstrated based on a flexible dose
range of 2.5 to 20 mg/day in clinical trials, with a mean modal dose of 10.7
mg/day (mean dose of 8.9 mg/day). When dosage adjustments are necessary, dose
increments/decrements of 2.5 or 5 mg are recommended.
The safety and effectiveness of doses above 20 mg/day have not been evaluated in clinical trials [see Clinical Studies ( 14.2)].
Maintenance Treatment - The efficacy of olanzapine for the maintenance treatment of bipolar I disorder in the adolescent population has not been evaluated; however, maintenance efficacy can be extrapolated from adult data along with comparisons of olanzapine pharmacokinetic parameters in adult and adolescent patients. Thus, it is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Olanzapine and Fluoxetine in Combination: Depressive Episodes
Associated with Bipolar I Disorder
When using olanzapine and fluoxetine in combination, also refer to the
Clinical Studies section of the package insert for Symbyax.
Adults
Oral olanzapine should be administered in combination with fluoxetine once
daily in the evening, without regard to meals, generally beginning with 5 mg
of oral olanzapine and 20 mg of fluoxetine. Dosage adjustments, if indicated,
can be made according to efficacy and tolerability within dose ranges of oral
olanzapine 5 to 12.5 mg and fluoxetine 20 to 50 mg. Antidepressant efficacy
was demonstrated with olanzapine and fluoxetine in combination in adult
patients with a dose range of olanzapine 6 to 12 mg and fluoxetine 25 to 50
mg. Safety of co-administration of doses above 18 mg olanzapine with 75 mg
fluoxetine has not been evaluated in clinical studies.
Children and Adolescents (10-17 years of age)
Oral olanzapine should be administered in combination with fluoxetine once
daily in the evening, without regard to meals, generally beginning with 2.5 mg
of oral olanzapine and 20 mg of fluoxetine. Dosage adjustments, if indicated,
can be made according to efficacy and tolerability. Safety of co-
administration of doses above 12 mg olanzapine with 50 mg fluoxetine has not
been evaluated in pediatric clinical studies.
Safety and efficacy of olanzapine and fluoxetine in combination was determined
in clinical trials supporting approval of Symbyax (fixed dose combination of
olanzapine and fluoxetine). Symbyax is dosed between 3 mg/25 mg
(olanzapine/fluoxetine) per day and 12 mg/50 mg (olanzapine/fluoxetine) per
day. The following table demonstrates the appropriate individual component
doses of olanzapine and fluoxetine versus Symbyax. Dosage adjustments, if
indicated, should be made with the individual components according to efficacy
and tolerability.
Table 1: Approximate Dose Correspondence Between Symbyaxa and the
Combination of Olanzapine and Fluoxetine
|
For |
Use in Combination | |
|
Olanzapine Tablets |
Fluoxetine | |
|
3 mg olanzapine/25 mg fluoxetine |
2.5 |
20 |
|
6 mg olanzapine/25 mg fluoxetine |
5 |
20 |
|
12 mg olanzapine/25 mg fluoxetine |
10+2.5 |
20 |
|
6 mg olanzapine/50 mg fluoxetine |
5 |
40+10 |
|
12 mg olanzapine/50 mg fluoxetine |
10+2.5 |
40+10 |
a Symbyax (olanzapine/fluoxetine HCl) is a fixed-dose combination of olanzapine and fluoxetine.
While there is no body of evidence to answer the question of how long a
patient treated with olanzapine and fluoxetine in combination should remain on
it, it is generally accepted that bipolar I disorder, including the depressive
episodes associated with bipolar I disorder, is a chronic illness requiring
chronic treatment. The healthcare provider should periodically reexamine the
need for continued pharmacotherapy.
Olanzapine monotherapy is not indicated for the treatment of depressive
episodes associated with bipolar I disorder.
2.6 Olanzapine and Fluoxetine in Combination: Treatment Resistant
Depression
When using olanzapine and fluoxetine in combination, also refer to the
Clinical Studies section of the package insert for Symbyax.
Oral olanzapine should be administered in combination with fluoxetine once
daily in the evening, without regard to meals, generally beginning with 5 mg
of oral olanzapine and 20 mg of fluoxetine. Dosage adjustments, if indicated,
can be made according to efficacy and tolerability within dose ranges of oral
olanzapine 5 to 20 mg and fluoxetine 20 to 50 mg. Antidepressant efficacy was
demonstrated with olanzapine and fluoxetine in combination in adult patients
with a dose range of olanzapine 6 to 18 mg and fluoxetine 25 to 50 mg.
Safety and efficacy of olanzapine in combination with fluoxetine was
determined in clinical trials supporting approval of Symbyax (fixed dose
combination of olanzapine and fluoxetine). Symbyax is dosed between 3 mg/25 mg
(olanzapine/fluoxetine) per day and 12 mg/50 mg (olanzapine/fluoxetine) per
day. Table 1 above demonstrates the appropriate individual component doses of
olanzapine and fluoxetine versus Symbyax. Dosage adjustments, if indicated,
should be made with the individual components according to efficacy and
tolerability.
While there is no body of evidence to answer the question of how long a
patient treated with olanzapine and fluoxetine in combination should remain on
it, it is generally accepted that treatment resistant depression (major
depressive disorder in adult patients who do not respond to 2 separate trials
of different antidepressants of adequate dose and duration in the current
episode) is a chronic illness requiring chronic treatment. The healthcare
provider should periodically reexamine the need for continued pharmacotherapy.
Safety of co-administration of doses above 18 mg olanzapine with 75 mg
fluoxetine has not been evaluated in clinical studies.
Olanzapine monotherapy is not indicated for treatment of treatment resistant
depression (major depressive disorder in patients who do not respond to 2
antidepressants of adequate dose and duration in the current episode).
2.7 Olanzapine and Fluoxetine in Combination: Dosing in Special Populations
The starting dose of oral olanzapine 2.5-5 mg with fluoxetine 20 mg should be used for patients with a predisposition to hypotensive reactions, patients with hepatic impairment, or patients who exhibit a combination of factors that may slow the metabolism of olanzapine or fluoxetine in combination (female gender, geriatric age, non-smoking status), or those patients who may be pharmacodynamically sensitive to olanzapine. Dosing modification may be necessary in patients who exhibit a combination of factors that may slow metabolism. When indicated, dose escalation should be performed with caution in these patients. Olanzapine and fluoxetine in combination have not been systematically studied in patients over 65 years of age or in patients under 10 years of age [see Warnings and Precautions ( 5.14), Drug Interactions ( 7), and Clinical Pharmacology ( 12.3)].
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS & STRENGTHS
Olanzapine tablets , USP 2.5 mg are white to off white coloured, round shaped, biconvex, film coated tablets debossed 'CL' on one side and '39' on other side, 5 mg, are white to off white coloured, round shaped, biconvex, film coated tablets debossed 'CL 40' on one side, and plain on other side, 7.5 mg are white to off white coloured, round shaped, biconvex, film coated tablets debossed 'CL 41 on one side and plain on other side, 10 mg are white to off white coloured, round shaped, biconvex, film coated tablets debossed 'CL 42' on one side and plain on other side. The 15 mg tablets are blue coloured, oval shaped biconvex film coated tablets having 'CL 43' debossed on one side and plain on other side. The 20 mg tablets are pink coloured, oval shaped biconvex film coated tablets having 'CL 44' debossed on one side and plain on other side. Tablets are not scored. The tablets are available as follows:
|
TABLET STRENGTH | ||||||
|
2.5 mg |
5 mg |
7.5 mg |
10 mg |
15 mg |
20 mg | |
|
Identification |
CL |
CL |
CL |
CL |
CL |
CL |
|
39 |
40 |
41 |
42 |
43 |
44 |
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
When using olanazapine and fluoxetine in combination, also refer to the Use in Specific Populations section of the package insert for Symbyax.
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in
women exposed to atypical antipsychotics, including olanzapine, during
pregnancy. Healthcare providers are encouraged to register patients by
contacting the National Pregnancy Registry for Atypical Antipsychotics at
1-866-961-2388 or visit http://womensmentalhealth.org/clinical-and-
researchprograms/ pregnancyregistry/.
Risk Summary
Neonates exposed to antipsychotic drugs, including olanzapine, during the
third trimester are at risk for extrapyramidal and/or withdrawal symptoms
following delivery (see Clinical Considerations). Overall available data from
published epidemiologic studies of pregnant women exposed to olanzapine have
not established a drug-associated risk of major birth defects, miscarriage, or
adverse maternal or fetal outcomes (see Data). There are risks to the mother
associated with untreated schizophrenia or bipolar I disorder and with
exposure to antipsychotics, including olanzapine, during pregnancy (see
Clinical Considerations).
Olanzapine was not teratogenic when administered orally to pregnant rats and
rabbits at doses that are 9- and 30-times the daily oral maximum recommended
human dose (MRHD), based on mg/m2 body surface area; some fetal toxicities
were observed at these doses (see Data).
The estimated background risk of major birth defects and miscarriage for the
indicated populations is unknown. All pregnancies have a background risk of
birth defects, loss, or other adverse outcomes. In the U.S. general
population, the estimated background risk of major birth defects and
miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%,
respectively.
Clinical Considerations
Disease-associated maternal and embryo/fetal risk
There is a risk to the mother from untreated schizophrenia or bipolar I
disorder, including increased risk of relapse, hospitalization, and suicide.
Schizophrenia and bipolar I disorder are associated with increased adverse
perinatal outcomes, including preterm birth. It is not known if this is a
direct result of the illness or other comorbid factors.
Fetal/Neonatal adverse reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia,
hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have
been reported in neonates who were exposed to antipsychotic drugs, including
olanzapine, during the third trimester of pregnancy. These symptoms have
varied in severity. Monitor neonates for extrapyramidal and/or withdrawal
symptoms and manage symptoms appropriately. Some neonates recovered within
hours or days without specific treatment; others required prolonged
hospitalization.
Data
Human Data
Placental passage has been reported in published study reports; however, the
placental passage ratio was highly variable ranging between 7% to 167% at
birth following exposure during pregnancy. The clinical relevance of this
finding is unknown.
Published data from observational studies, birth registries, and case reports that have evaluated the use of atypical antipsychotics during pregnancy do not establish an increased risk of major birth defects. A retrospective cohort study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects.
Animal Data
In oral reproduction studies in rats at doses up to 18 mg/kg/day and in
rabbits at doses up to 30 mg/kg/day (9 and 30 times the daily oral MRHD based
on mg/m2 body surface area, respectively), no evidence of teratogenicity was
observed. In an oral rat teratology study, early resorptions and increased
numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times
the daily oral MRHD based on mg/m2 body surface area), and gestation was
prolonged at 10 mg/kg/day (5 times the daily oral MRHD based on mg/m body
surface area). In an oral rabbit teratology study, fetal toxicity manifested
as increased resorptions and decreased fetal weight, occurred at a maternally
toxic dose of 30 mg/kg/day (30 times the daily oral MRHD based on mg/m 2 body
surface area).
8.2 Lactation
Risk Summary
Olanzapine is present in human milk. There are reports of excess sedation,
irritability, poor feeding and extrapyramidal symptoms (tremors and abnormal
muscle movements) in infants exposed to olanzapine through breast milk (see
Clinical Considerations). There is no information on the effects of olanzapine
on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for olanzapine and any potential adverse effects on the breastfed child from olanzapine or from the mother’s underlying condition.
Clinical Considerations
Infants exposed to olanzapine should be monitored for excess sedation,
irritability, poor feeding, and extrapyramidal symptoms (tremors and abnormal
muscle movements).
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on the pharmacologic action of olanzapine (D2 receptor antagonism),
treatment with olanzapine may result in an increase in serum prolactin levels,
which may lead to a reversible reduction in fertility in females of
reproductive potential [see Warnings and Precautions ( 5.15)].
8.4 Pediatric Use
The safety and effectiveness of oral olanzapine in the treatment of
schizophrenia and manic or mixed episodes associated with bipolar I disorder
were established in short-term studies in adolescents (ages 13 to 17 years).
Use of olanzapine in adolescents is supported by evidence from adequate and
well-controlled studies of olanzapine in which 268 adolescents received
olanzapine in a range of 2.5 to 20 mg/day [ see Clinical Studies ( 14.1, 14.2) ]. Recommended starting dose for adolescents is lower than that for adults [ see Dosage and Administration ( 2.1, 2.2) ]. Compared to patients from adult
clinical trials, adolescents were likely to gain more weight, experience
increased sedation, and have greater increases in total cholesterol,
triglycerides, LDL cholesterol, prolactin and hepatic aminotransferase levels
[ see Warnings and Precautions ( 5.5, 5.15, 5.17) and Adverse Reactions ( 6.1) ]. When deciding among the alternative treatments available for adolescents,
clinicians should consider the increased potential (in adolescents as compared
with adults) for weight gain and dyslipidemia. Clinicians should consider the
potential long-term risks when prescribing to adolescents, and in many cases
this may lead them to consider prescribing other drugs first in adolescents [ see Indications and Usage ( 1.1, 1.2) ].
Safety and effectiveness of olanzapine in children <13 years of age have not
been established [ see Patient Counseling Information (17) ]
Safety and efficacy of olanzapine and fluoxetine in combination in children
and adolescents (10 to 17 years of age) have been established for the acute
treatment of depressive episodes associated with bipolar I disorder.
Safety and effectiveness of olanzapine and fluoxetine in combination in children <10 years of age have not been established.
8.5 Geriatric Use
Of the 2500 patients in premarketing clinical studies with oral olanzapine, 11% (263) were 65 years of age or over. In patients with schizophrenia, there was no indication of any different tolerability of olanzapine in the elderly compared to younger patients. Studies in elderly patients with dementia- related psychosis have suggested that there may be a different tolerability profile in this population compared to younger patients with schizophrenia. Elderly patients with dementia-related psychosis treated with olanzapine are at an increased risk of death compared to placebo. In placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis, there was a higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) in patients treated with olanzapine compared to patients treated with placebo. In 5 placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis (n=1184), the following adverse reactions were reported in olanzapine-treated patients at an incidence of at least 2% and significantly greater than placebo-treated patients: falls, somnolence, peripheral edema, abnormal gait, urinary incontinence, lethargy, increased weight, asthenia, pyrexia, pneumonia, dry mouth and visual hallucinations. The rate of discontinuation due to adverse reactions was greater with olanzapine than placebo (13% vs 7%). Elderly patients with dementia-related psychosis treated with olanzapine are at an increased risk of death compared to placebo. Olanzapine is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning, Warnings and Precautions ( 5.1), and Patient Counseling Information ( 17)]. Olanzapine is not approved for the treatment of patients with dementia-related psychosis. Also, the presence of factors that might decrease pharmacokinetic clearance or increase the pharmacodynamic response to olanzapine should lead to consideration of a lower starting dose for any geriatric patient [see Boxed Warning, Dosage and Administration ( 2.1), and Warnings and Precautions ( 5.1)].
Clinical studies of olanzapine and fluoxetine in combination did not include sufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger patients.
• Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. ( 8.1)
• Pediatric Use: Safety and effectiveness of olanzapine in children <13 years of age have not been established. Safety and effectiveness of olanzapine and fluoxetine in combination in children <10 years of age have not been established. ( 8.4).
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.3 Dependence
In studies prospectively designed to assess abuse and dependence potential, olanzapine was shown to have acute depressive CNS effects but little or no potential of abuse or physical dependence in rats administered oral doses up to 15 times the daily oral MRHD (20 mg) and rhesus monkeys administered oral doses up to 8 times the daily oral MRHD based on mg/m 2 body surface area.
Olanzapine has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic, and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of olanzapine (e.g., development of tolerance, increases in dose, drug-seeking behavior).
DESCRIPTION SECTION
11 DESCRIPTION
Olanzapine USP is an atypical antipsychotic that belongs to the
thienobenzodiazepine class. The chemical designation is
2-methyl-4-(4-methyl-1-piperazinyl)-10H-thieno[2,3-b] [1,5]benzodiazepine. The
molecular formula is C17H20N4S, which corresponds to a molecular weight of
312.44. The chemical structure is:
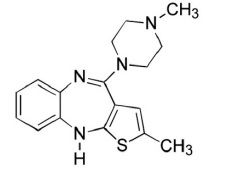
Olanzapine USP is a yellow crystalline solid, which is practically insoluble
in water.
Olanzapine tablets, USP are intended for oral administration only.
Each tablet contains olanzapine equivalent to 2.5 mg (8 μmol), 5 mg (16 μmol),
7.5 mg (24 μmol), 10 mg (32 μmol), 15 mg (48 μmol), or 20 mg (64 μmol).
Inactive ingredients are crospovidone, hydroxypropyl cellulose, magnesium
stearate, microcrystalline cellulose. The color coating contains Titanium
Dioxide (all strengths), FD&C Blue No. 2 indigo carmine Aluminum Lake (15 mg),
or Synthetic Red Iron Oxide (20 mg).
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of olanzapine, in the listed indications is unclear. However, the efficacy of olanzapine in schizophrenia could be mediated through a combination of dopamine and serotonin type 2 (5HT 2) antagonism.
12.2 Pharmacodynamics
Olanzapine binds with high affinity to the following receptors: serotonin 5HT 2A/2C, 5HT 6 (K i=4, 11, and 5 nM, respectively), dopamine D 1-4 (K i=11-31 nM), histamine H 1 (K i=7 nM), and adrenergic α 1 receptors (K i=19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT 3 (K i=57 nM) and muscarinic M 1-5 (K i=73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds with low affinity to GABA A, BZD, and β-adrenergic receptors (K i>10 μM).
12.3 Pharmacokinetics
Oral Administration, Monotherapy — Olanzapine is well absorbed and reaches
peak concentrations in approximately 6 hours following an oral dose. It is
eliminated extensively by first pass metabolism, with approximately 40% of the
dose metabolized before reaching the systemic circulation. Food does not
affect the rate or extent of olanzapine absorption. Pharmacokinetic studies
showed that olanzapine tablets and olanzapine orally disintegrating tablets
dosage forms of olanzapine are bioequivalent.
Olanzapine displays linear kinetics over the clinical dosing range. Its half-
life ranges from 21 to 54 hours (5th to 95th percentile; mean of 30 hr), and
apparent plasma clearance ranges from 12 to 47 L/hr (5th to 95th percentile;
mean of 25 L/hr).
Administration of olanzapine once daily leads to steady-state concentrations
in about 1 week that are approximately twice the concentrations after single
doses. Plasma concentrations, half-life, and clearance of olanzapine may vary
between individuals on the basis of smoking status, gender, and age.
Olanzapine is extensively distributed throughout the body, with a volume of
distribution of approximately 1000 L. It is 93% bound to plasma proteins over
the concentration range of 7 to 1100 ng/mL, binding primarily to albumin and
α1-acid glycoprotein.
Metabolism and Elimination — Following a single oral dose of 14C labeled olanzapine, 7% of the dose of olanzapine was recovered in the urine as unchanged drug, indicating that olanzapine is highly metabolized. Approximately 57% and 30% of the dose was recovered in the urine and feces, respectively. In the plasma, olanzapine accounted for only 12% of the AUC for total radioactivity, indicating significant exposure to metabolites. After multiple dosing, the major circulating metabolites were the 10-N-glucuronide, present at steady state at 44% of the concentration of olanzapine, and 4′-N-desmethyl olanzapine, present at steady state at 31% of the concentration of olanzapine. Both metabolites lack pharmacological activity at the concentrations observed.
Direct glucuronidation and cytochrome P450 (CYP) mediated oxidation are the primary metabolic pathways for olanzapine. In vitro studies suggest that CYPs 1A2 and 2D6, and the flavin-containing monooxygenase system are involved in olanzapine oxidation. CYP2D6 mediated oxidation appears to be a minor metabolic pathway in vivo, because the clearance of olanzapine is not reduced in subjects who are deficient in this enzyme.
Specific Populations
Renal Impairment — Because olanzapine is highly metabolized before excretion and only 7% of the drug is excreted unchanged, renal dysfunction alone is unlikely to have a major impact on the pharmacokinetics of olanzapine. The pharmacokinetic characteristics of olanzapine were similar in patients with severe renal impairment and normal subjects, indicating that dosage adjustment based upon the degree of renal impairment is not required. In addition, olanzapine is not removed by dialysis. The effect of renal impairment on metabolite elimination has not been studied.
Hepatic Impairment — Although the presence of hepatic impairment may be expected to reduce the clearance of olanzapine, a study of the effect of impaired liver function in subjects (n=6) with clinically significant (Childs Pugh Classification A and B) cirrhosis revealed little effect on the pharmacokinetics of olanzapine.
Geriatric — In a study involving 24 healthy subjects, the mean elimination half-life of olanzapine was about 1.5 times greater in elderly (≥65 years) than in nonelderly subjects (<65 years). Caution should be used in dosing the elderly, especially if there are other factors that might additively influence drug metabolism and/or pharmacodynamic sensitivity [see Dosage and Administration (2)].
Gender — Clearance of olanzapine is approximately 30% lower in women than in men. There were, however, no apparent differences between men and women in effectiveness or adverse effects. Dosage modifications based on gender should not be needed.
Smoking Status — Olanzapine clearance is about 40% higher in smokers than in nonsmokers, although dosage modifications are not routinely recommended.
Race — In vivo studies have shown that exposures are similar among Japanese, Chinese and Caucasians, especially after normalization for body weight differences. Dosage modifications for race are, therefore, not recommended.
Combined Effects — The combined effects of age, smoking, and gender could lead to substantial pharmacokinetic differences in populations. The clearance in young smoking males, for example, may be 3 times higher than that in elderly nonsmoking females. Dosing modification may be necessary in patients who exhibit a combination of factors that may result in slower metabolism of olanzapine [see Dosage and Administration (2)].
Adolescents (ages 13 to 17 years)
In clinical studies, most adolescents were nonsmokers and this population had a lower average body weight, which resulted in higher average olanzapine exposure compared to adults.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment of Fertility
Carcinogenesis — Oral carcinogenicity studies were conducted in mice and rats.
Olanzapine was administered to mice in two 78-week studies at doses of 3, 10,
30/20 mg/kg/day (equivalent to 0.8-5 times the daily oral MRHD based on mg/m 2
body surface area) and 0.25, 2, 8 mg/kg/day (equivalent to 0.06-2 times the
daily oral MRHD based on mg/m 2 body surface area). Rats were dosed for 2
years at doses of 0.25, 1, 2.5, 4 mg/kg/day (males) and 0.25, 1, 4, 8
mg/kg/day (females) (equivalent to 0.13-2 and 0.13-4 times the daily oral MRHD
based on mg/m 2 body surface area, respectively).
The incidence of liver hemangiomas and hemangiosarcomas was significantly
increased in 1 mouse study in female mice at 2 times the daily oral MRHD based
on mg/m 2 body surface area. These tumors were not increased in another mouse
study in females dosed up to 2-5 times the daily oral MRHD based on mg/m 2
body surface area; in this study, there was a high incidence of early
mortalities in males of the 30/20 mg/kg/day group. The incidence of mammary
gland adenomas and adenocarcinomas was significantly increased in female mice
dosed at ≥2 mg/kg/day and in female rats dosed at ≥4 mg/kg/day (0.5 and 2
times the daily oral MRHD based on mg/m 2 body surface area, respectively).
Antipsychotic drugs have been shown to chronically elevate prolactin levels in
rodents. Serum prolactin levels were not measured during the olanzapine
carcinogenicity studies; however, measurements during subchronic toxicity
studies showed that olanzapine elevated serum prolactin levels up to 4-fold in
rats at the same doses used in the carcinogenicity study. An increase in
mammary gland neoplasms has been found in rodents after chronic administration
of other antipsychotic drugs and is considered to be prolactin mediated. The
relevance for human risk of the finding of prolactin mediated endocrine tumors
in rodents is unknown [see Warnings and Precautions ( 5.15)].
Mutagenesis — No evidence of genotoxic potential for olanzapine was found in the Ames reverse mutation test, in vivo micronucleus test in mice, the chromosomal aberration test in Chinese hamster ovary cells, unscheduled DNA synthesis test in rat hepatocytes, induction of forward mutation test in mouse lymphoma cells, or in vivo sister chromatid exchange test in bone marrow of Chinese hamsters.
Impairment of Fertility — In an oral fertility and reproductive performance study in rats, male mating performance, but not fertility, was impaired at a dose of 22.4 mg/kg/day and female fertility was decreased at a dose of 3 mg/kg/day (11 and 1.5 times the daily oral MRHD based on mg/m 2 body surface area, respectively). Discontinuance of olanzapine treatment reversed the effects on male mating performance. In female rats, the precoital period was increased and the mating index reduced at 5 mg/kg/day (2.5 times the daily oral MRHD based on mg/m 2 body surface area). Diestrous was prolonged and estrous delayed at 1.1 mg/kg/day (0.6 times the daily oral MRHD based on mg/m 2 body surface area); therefore olanzapine may produce a delay in ovulation.
13.2 Animal Toxicology and/or Pharmacology
In animal studies with olanzapine, the principal hematologic findings were reversible peripheral cytopenias in individual dogs dosed at 10 mg/kg (17 times the daily oral MRHD based on mg/m 2 body surface area), dose-related decreases in lymphocytes and neutrophils in mice, and lymphopenia in rats. A few dogs treated with 10 mg/kg developed reversible neutropenia and/or reversible hemolytic anemia between 1 and 10 months of treatment. Dose-related decreases in lymphocytes and neutrophils were seen in mice given doses of 10 mg/kg (equal to 2 times the daily oral MRHD based on mg/m 2 body surface area) in studies of 3 months' duration. Nonspecific lymphopenia, consistent with decreased body weight gain, occurred in rats receiving 22.5 mg/kg (11 times the daily oral MRHD based on mg/m 2 body surface area) for 3 months or 16 mg/kg (8 times the daily oral MRHD based on mg/m 2 body surface area) for 6 or 12 months. No evidence of bone marrow cytotoxicity was found in any of the species examined. Bone marrows were normocellular or hypercellular, indicating that the reductions in circulating blood cells were probably due to peripheral (non-marrow) factors.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
When using olanzapine and fluoxetine in combination, also refer to the Clinical Studies section of the package insert for Symbyax.
14.1 Schizophrenia
Adults
The efficacy of oral olanzapine in the treatment of schizophrenia was established in 2 short-term (6-week) controlled trials of adult inpatients who met DSM III-R criteria for schizophrenia. A single haloperidol arm was included as a comparative treatment in 1 of the 2 trials, but this trial did not compare these 2 drugs on the full range of clinically relevant doses for both.
Several instruments were used for assessing psychiatric signs and symptoms in these studies, among them the Brief Psychiatric Rating Scale (BPRS), a multi- item inventory of general psychopathology traditionally used to evaluate the effects of drug treatment in schizophrenia. The BPRS psychosis cluster (conceptual disorganization, hallucinatory behavior, suspiciousness, and unusual thought content) is considered a particularly useful subset for assessing actively psychotic schizophrenic patients. A second traditional assessment, the Clinical Global Impression (CGI), reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient. In addition, 2 more recently developed scales were employed; these included the 30-item Positive and Negative Symptoms Scale (PANSS), in which are embedded the 18 items of the BPRS, and the Scale for Assessing Negative Symptoms (SANS). The trial summaries below focus on the following outcomes: PANSS total and/or BPRS total; BPRS psychosis cluster; PANSS negative subscale or SANS; and CGI Severity. The results of the trials follow:
(1) In a 6-week, placebo-controlled trial (n=149) involving 2 fixed olanzapine doses of 1 and 10 mg/day (once daily schedule), olanzapine, at 10 mg/day (but not at 1 mg/day), was superior to placebo on the PANSS total score (also on the extracted BPRS total), on the BPRS psychosis cluster, on the PANSS Negative subscale, and on CGI Severity.
(2) In a 6-week, placebo-controlled trial (n=253) involving 3 fixed dose ranges of olanzapine (5 ± 2.5 mg/day, 10 ± 2.5 mg/day, and 15 ± 2.5 mg/day) on a once daily schedule, the 2 highest olanzapine dose groups (actual mean doses of 12 and 16 mg/day, respectively) were superior to placebo on BPRS total score, BPRS psychosis cluster, and CGI severity score; the highest olanzapine dose group was superior to placebo on the SANS. There was no clear advantage for the high-dose group over the medium-dose group.
(3) In a longer-term trial, adult outpatients (n=326) who predominantly met DSM-IV criteria for schizophrenia and who remained stable on olanzapine during open-label treatment for at least 8 weeks were randomized to continuation on their current olanzapine doses (ranging from 10 to 20 mg/day) or to placebo. The follow-up period to observe patients for relapse, defined in terms of increases in BPRS positive symptoms or hospitalization, was planned for 12 months, however, criteria were met for stopping the trial early due to an excess of placebo relapses compared to olanzapine relapses, and olanzapine was superior to placebo on time to relapse, the primary outcome for this study. Thus, olanzapine was more effective than placebo at maintaining efficacy in patients stabilized for approximately 8 weeks and followed for an observation period of up to 8 months.
Examination of population subsets (race and gender) did not reveal any differential responsiveness on the basis of these subgroupings.
Adolescents
The efficacy of oral olanzapine in the acute treatment of schizophrenia in adolescents (ages 13 to 17 years) was established in a 6-week double-blind, placebo-controlled, randomized trial of inpatients and outpatients with schizophrenia (n=107) who met diagnostic criteria according to DSM-IV-TR and confirmed by the Kiddie Schedule for Affective Disorders and Schizophrenia for School Aged Children-Present and Lifetime Version (K-SADS-PL).
The primary rating instrument used for assessing psychiatric signs and symptoms in this trial was the Anchored Version of the Brief Psychiatric Rating Scale for Children (BPRS-C) total score.
In this flexible-dose trial, olanzapine 2.5 to 20 mg/day (mean modal dose 12.5 mg/day, mean dose of 11.1 mg/day) was more effective than placebo in the treatment of adolescents diagnosed with schizophrenia, as supported by the statistically significantly greater mean reduction in BPRS-C total score for patients in the olanzapine treatment group than in the placebo group.
While there is no body of evidence available to answer the question of how long the adolescent patient treated with olanzapine should be maintained, maintenance efficacy can be extrapolated from adult data along with comparisons of olanzapine pharmacokinetic parameters in adult and adolescent patients. It is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
14.2 Bipolar I Disorder (Manic or Mixed Episodes)
Adults
****Monotherapy — The efficacy of oral olanzapine in the treatment of manic
or mixed episodes was established in 2 short-term (one 3-week and one 4-week)
placebo-controlled trials in adult patients who met the DSM-IV criteria for
bipolar I disorder with manic or mixed episodes. These trials included
patients with or without psychotic features and with or without a rapid-
cycling course.The primary rating instrument used for assessing manic symptoms
in these trials was the Young Mania Rating Scale (Y-MRS), an 11-item
clinician-rated scale traditionally used to assess the degree of manic
symptomatology (irritability, disruptive/aggressive behavior, sleep, elevated
mood, speech, increased activity, sexual interest, language/thought disorder,
thought content, appearance, and insight) in a range from 0 (no manic
features) to 60 (maximum score). The primary outcome in these trials was
change from baseline in the Y-MRS total score. The results of the trials
follow:
(1) In one 3-week placebo-controlled trial (n=67) which involved a dose range of olanzapine (5-20 mg/day, once daily, starting at 10 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score. In an identically designed trial conducted simultaneously with the first trial, olanzapine demonstrated a similar treatment difference, but possibly due to sample size and site variability, was not shown to be superior to placebo on this outcome.
(2) In a 4-week placebo-controlled trial (n=115) which involved a dose range of olanzapine (5-20 mg/day, once daily, starting at 15 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score.
(3) In another trial, 361 patients meeting DSM-IV criteria for a manic or mixed episode of bipolar I disorder who had responded during an initial open- label treatment phase for about 2 weeks, on average, to olanzapine 5 to 20 mg/day were randomized to either continuation of olanzapine at their same dose (n=225) or to placebo (n=136), for observation of relapse. Approximately 50% of the patients had discontinued from the olanzapine group by day 59 and 50% of the placebo group had discontinued by day 23 of double-blind treatment. Response during the open-label phase was defined by having a decrease of the Y-MRS total score to ≤12 and HAM-D 21 to ≤8. Relapse during the double-blind phase was defined as an increase of the Y-MRS or HAM-D 21 total score to ≥15, or being hospitalized for either mania or depression. In the randomized phase, patients receiving continued olanzapine experienced a significantly longer time to relapse.
Adjunct to Lithium or Valproate — The efficacy of oral olanzapine with concomitant lithium or valproate in the treatment of manic or mixed episodes was established in 2 controlled trials in patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These trials included patients with or without psychotic features and with or without a rapid- cycling course. The results of the trials follow:
(1) In one 6-week placebo-controlled combination trial, 175 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5-20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 μg/mL to 125 μg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score
(2) In a second 6-week placebo-controlled combination trial, 169 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5-20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 μg/mL to 125 μg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score.
Adolescents
****Acute Monotherapy — The efficacy of oral olanzapine in the treatment of
acute manic or mixed episodes in adolescents (ages 13 to 17 years) was
established in a 3-week, double-blind, placebo-controlled, randomized trial of
adolescent inpatients and outpatients who met the diagnostic criteria for
manic or mixed episodes associated with bipolar I disorder (with or without
psychotic features) according to the DSM-IV-TR (n=161). Diagnosis was
confirmed by the K-SADS-PL.
The primary rating instrument used for assessing manic symptoms in this trial was the Adolescent Structured Young-Mania Rating Scale (Y-MRS) total score.
In this flexible-dose trial, olanzapine 2.5 to 20 mg/day (mean modal dose 10.7 mg/day, mean dose of 8.9 mg/day) was more effective than placebo in the treatment of adolescents with manic or mixed episodes associated with bipolar I disorder, as supported by the statistically significantly greater mean reduction in Y-MRS total score for patients in the olanzapine treatment group than in the placebo group.
While there is no body of evidence available to answer the question of how long the adolescent patient treated with olanzapine should be maintained, maintenance efficacy can be extrapolated from adult data along with comparisons of olanzapine pharmacokinetic parameters in adult and adolescent patients. It is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Olanzapine tablets, USP 5 mg, are white to off white coloured, round shaped, biconvex, film coated tablets debossed ‘CL 40’ on one side and plain on other side
NDC: 70518-2698-00
PACKAGING: 30 in 1 BLISTER PACK
Store olanzapine tablets, USP at controlled room temperature, 20° to 25°C (68° to 77°F) [see USP]. The USP defines controlled room temperature as a temperature maintained thermostatically that encompasses the usual and customary working environment of 20° to 25°C (68° to 77°F); that results in a mean kinetic temperature calculated to be not more than 25°C; and that allows for excursions between 15° and 30°C (59° and 86°F) that are experienced in pharmacies, hospitals, and warehouses.
Protect olanzapine tablets, USP from light and moisture.
Repackaged and Distributed By:
Remedy Repack, Inc.
625 Kolter Dr. Suite #4 Indiana, PA 1-724-465-8762
SPL MEDGUIDE SECTION
SPL MEDGUIDE SECTION
Olanzapine Tablets
(oh lan’za peen)
Read the Medication Guide that comes with olanzapine tablets before you start taking it and each time you get a refill.
There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or treatment. Talk with your doctor or pharmacist if there is something you do not understand or you want to learn more about olanzapine tablets.
What is the most important information I should know about olanzapine tablets?
Olanzapine tablets may cause serious side effects, including:
1. Increased risk of death in elderly people who are confused, have memory loss and have lost touch with reality (dementia-related psychosis).
2. High blood sugar (hyperglycemia).
3. High fat levels in your blood (increased cholesterol and triglycerides), especially in teenagers age 13 to 17 or when used in combination with fluoxetine in children age 10 to 17.
4. Weight gain, especially in teenagers age 13 to 17 or when used in combination with fluoxetine in children age 10 to 17.
These serious side effects are described below.
**1. Increased risk of death in elderly people who are confused, have memory loss and have lost touch with reality (dementia-related psychosis). **Olanzapine tablets are not approved for treating psychosis in elderly people with dementia.
**2. High blood sugar (hyperglycemia).**High blood sugar can happen if you have diabetes already or if you have never had diabetes. High blood sugar could lead to:
• a build up of acid in your blood due to ketones (ketoacidosis)
• coma
• death
Your doctor should do tests to check your blood sugar before you start taking olanzapine tablets and during treatment.
In people who do not have diabetes, sometimes high blood sugar goes away when olanzapine tablets are stopped.
People with diabetes and some people who did not have diabetes before taking olanzapine tablets need to take medicine for high blood sugar even after they stop taking olanzapine tablets.
If you have diabetes, follow your doctor’s instructions about how often to check your blood sugar while taking olanzapine tablets.
Call your doctorif you have any of these symptoms of high blood sugar (hyperglycemia) while taking olanzapine tablets:
• feel very thirsty
• need to urinate more than usual
• feel very hungry
• feel weak or tired
• feel sick to your stomach
• feel confused or your breath smells fruity
3. High fat levels in your blood (cholesterol and triglycerides). High fat levels may happen in people treated with olanzapine tablets, especially in teenagers (13 to 17 years old), or when used in combination with fluoxetine in children (10 to 17 years old). You may not have any symptoms, so your doctor should do blood tests to check your cholesterol and triglyceride levels before you start taking olanzapine tablets and during treatment.
4. Weight gain. Weight gain is very common in people who take olanzapine tablets. Teenagers (13 to 17 years old) are more likely to gain weight and to gain more weight than adults. Children (10 to 17 years old) are also more likely to gain weight and to gain more weight than adults when olanzapine tablet is used in combination with fluoxetine.Some people may gain a lot of weight while taking olanzapine tablets, so you and your doctor should check your weight regularly. Talk to your doctor about ways to control weight gain, such as eating a healthy, balanced diet, and exercising.
What are olanzapine tablets?
Olanzapine tablets are a prescription medicine used to treat:
** •**schizophrenia in people age 13 or older.
• bipolar disorder, including:
• manic or mixed episodes that happen with bipolar I disorder in people age 13 or older.
• manic or mixed episodes that happen with bipolar I disorder, when used with the medicine lithium or valproate, in adults.
• long-term treatment of bipolar I disorder in adults.
• episodes of depression that happen with bipolar I disorder, when used with the medicine fluoxetine (Prozac®) in people age 10 or older.
• episodes of depression that do not get better after 2 other medicines, also called treatment resistant depression, when used with the medicine fluoxetine (Prozac), in adults.
Olanzapine tablets have not been approved for use in children under 13 years of age. Olanzapine tablets in combination with fluoxetine has not been approved for use in children under 10 years of age.
The symptoms of schizophrenia include hearing voices, seeing things that are not there, having beliefs that are not true, and being suspicious or withdrawn.
The symptoms of bipolar I disorder include alternating periods of depression and high or irritable mood, increased activity and restlessness, racing thoughts, talking fast, impulsive behavior, and a decreased need for sleep.
The symptoms of treatment resistant depression include decreased mood, decreased interest, increased guilty feelings, decreased energy, decreased concentration, changes in appetite, and suicidal thoughts or behavior.
Some of your symptoms may improve with treatment. If you do not think you are getting better, call your doctor.
What should I tell my doctor before taking olanzapine tablets?
Olanzapine tablets may not be right for you. Before starting olanzapine tablets, tell your doctor if you have or had:
• heart problems
• seizures
• diabetes or high blood sugar levels (hyperglycemia)
• high cholesterol or triglyceride levels in your blood
• liver problems
• low or high blood pressure
• strokes or “mini-strokes” also called transient ischemic attacks (TIAs)
• Alzheimer’s disease
• narrow-angle glaucoma
• enlarged prostate in men
• bowel obstruction
• breast cancer
• thoughts of suicide or hurting yourself
• any other medical condition
• are pregnant or plan to become pregnant. It is not known if olanzapine tablets will harm your unborn baby.
• If you become pregnant while receiving olanzapine tablets , talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling 1-866-961-2388 or go to http://womensmentalhealth.org/clinical-and research- programs/pregnancyregistry/.
• are breast-feeding or plan to breast-feed. Olanzapine passes into your breast milk. Talk to your doctor about the best way to feed your baby if you take olanzapine tablets.
Tell your doctor if you exercise a lot or are in hot places often.
The symptoms of bipolar I disorder, treatment resistant depression, or schizophrenia may includethoughts of suicide or of hurting yourself or others. If you have these thoughts at any time, tell your doctor or go to an emergency room right away.
Tell your doctor about all the medicines that you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Olanzapine tablets and some medicines may interact with each other and may not work as well, or cause possible serious side effects. Your doctor can tell you if it is safe to take olanzapine tablets with your other medicines. Do not start or stop any medicine while taking olanzapine tablets without talking to your doctor first.
How should I take olanzapine tablets?
• Take olanzapine tablets exactly as prescribed. Your doctor may need to change (adjust) the dose of olanzapine tablets until it is right for you.
• If you miss a dose of olanzapine tablets, take the missed dose as soon as you remember. If it is almost time for the next dose, just skip the missed dose and take your next dose at the regular time. Do not take two doses of olanzapine tablets at the same time.
•** To prevent serious side effects, do not stop taking olanzapine tablets suddenly. If you need to stop taking olanzapine tablets, your doctor can tell you how to safely stop taking it.**
•If you take too much olanzapine tablets, call your doctor or poison control center at 1-800-222-1222 right away, or get emergency treatment.
• Olanzapine tablets can be taken with or without food.
• Olanzapine tablets are usually taken one time each day.
• Call your doctor if you do not think you are getting better or have any concerns about your condition while taking olanzapine tablets.
What should I avoid while taking olanzapine tablets?
• Olanzapine tablets can cause sleepiness and may affect your ability to make decisions, think clearly, or react quickly. You should not drive, operate heavy machinery, or do other dangerous activities until you know how olanzapine tablets affects you.
• Avoid drinking alcohol while taking olanzapine tablets. Drinking alcohol while you take olanzapine tablets may make you sleepier than if you take olanzapine tablets alone.
What are the possible side effects of olanzapine tablets?
**Serious side effects may happen when you take olanzapine tablets, including: **
** • See “What is the most important information I should know about olanzapine tablets?”, which describes the increased risk of death in elderly people with dementia-related psychosis and the risks of high blood sugar, high cholesterol and triglyceride levels, and weight gain.**
** • Increased incidence of stroke or “mini-strokes” called transient ischemic attacks (TIAs) in elderly people with dementia-related psychosis** (elderly people who have lost touch with reality due to confusion and memory loss). Olanzapine tablets are not approved for these patients.
•Neuroleptic Malignant Syndrome (NMS): NMS is a rare but very serious condition that can happen in people who take antipsychotic medicines, including olanzapine tablets . NMS can cause death and must be treated in a hospital. Call your doctor right away if you become severely ill and have any of these symptoms:
• high fever
• excessive sweating
• rigid muscles
• confusion
• changes in your breathing, heartbeat, and blood pressure.
•Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): DRESS can occur with olanzapine tablets. Features of DRESS may include rash, fever, swollen glands and other internal organ involvement such as liver, kidney, lung and heart. DRESS is sometimes fatal; therefore, tell your doctor immediately if you experience any of these signs.
• Tardive Dyskinesia: This condition causes body movements that keep happening and that you can not control. These movements usually affect the face and tongue. Tardive dyskinesia may not go away, even if you stop taking olanzapine tablets. It may also start after you stop taking olanzapine tablets. Tell your doctor if you get any body movements that you can not control.
• Decreased blood pressure when you change positions, with symptoms of dizziness, fast or slow heartbeat, or fainting.
** • Difficulty swallowing, that can cause food or liquid to get into your lungs.**
** • Seizures: Tell your doctor if you have a seizure during treatment with olanzapine tablets.**
** • Problems with control of body temperature:** You could become very hot, for instance when you exercise a lot or stay in an area that is very hot. It is important for you to drink water to avoid dehydration. Call your doctor right away if you become severely ill and have any of these symptoms of dehydration:
• sweating too much or not at all
• dry mouth
• feeling very hot
• feeling thirsty
• not able to produce urine.
Common side effects of olanzapine tablets include: lack of energy, dry mouth, increased appetite, sleepiness, tremor (shakes), having hard or infrequent stools, dizziness, changes in behavior, or restlessness.
Other common side effects in teenagers (13-17 years old) include: headache, stomach-area (abdominal) pain, pain in your arms or legs, or tiredness. Teenagers experienced greater increases in prolactin, liver enzymes, and sleepiness, as compared with adults.
Tell your doctor about any side effect that bothers you or that does not go away.
These are not all the possible side effects with olanzapine tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or 1-855-926-3384.
How should I store olanzapine tablets?
• Store olanzapine tablets at room temperature, between 68°F to 77°F (20°C to 25°C).
• Keep olanzapine tablets away from light.
• Keep olanzapine tablets dry and away from moisture.
Keep olanzapine tablets and all medicines out of the reach of children.
General information about olanzapine tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use olanzapine tablets for a condition for which it was not prescribed. Do not give olanzapine tablets to other people, even if they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about olanzapine tablets. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about olanzapine tablets that was written for healthcare professionals.For more information about olanzapine tablets call at 1-888-943-3210.
What are the ingredients in olanzapine tablets?
** Active ingredient:** olanzapine
Inactive ingredients:
** Tablets**- crospovidone, hydroxypropyl cellulose, magnesium stearate, microcrystalline cellulose. The color coating contains Titanium Dioxide (all strengths), FD&C Blue No. 2 indigo carmine Aluminum Lake (15 mg), or Synthetic Red Iron Oxide (20 mg).
This Medication Guide has been approved by the U.S. Food and Drug Administration.
All other trademarks are the properties of their respective owners.
Medication Guide revised – September 2022
Repackaged By / Distributed By: RemedyRepack Inc.
625 Kolter Drive, Indiana, PA 15701
(724) 465-8762
OVERDOSAGE SECTION
10 OVERDOSAGE
10.1 Human Experience
In premarketing trials involving more than 3100 patients and/or normal subjects, accidental or intentional acute overdosage of olanzapine was identified in 67 patients. In the patient taking the largest identified amount, 300 mg, the only symptoms reported were drowsiness and slurred speech. In the limited number of patients who were evaluated in hospitals, including the patient taking 300 mg, there were no observations indicating an adverse change in laboratory analytes or ECG. Vital signs were usually within normal limits following overdoses.
In postmarketing reports of overdose with olanzapine alone, symptoms have been reported in the majority of cases. In symptomatic patients, symptoms with ≥10% incidence included agitation/aggressiveness, dysarthria, tachycardia, various extrapyramidal symptoms, and reduced level of consciousness ranging from sedation to coma. Among less commonly reported symptoms were the following potentially medically serious reactions: aspiration, cardiopulmonary arrest, cardiac arrhythmias (such as supraventricular tachycardia and 1 patient experiencing sinus pause with spontaneous resumption of normal rhythm), delirium, possible neuroleptic malignant syndrome, respiratory depression/arrest, convulsion, hypertension, and hypotension. Eli Lilly and Company has received reports of fatality in association with overdose of olanzapine alone. In 1 case of death, the amount of acutely ingested olanzapine was reported to be possibly as low as 450 mg of oral olanzapine; however, in another case, a patient was reported to survive an acute olanzapine ingestion of approximately 2 g of oral olanzapine.
10.2 Management of Overdose
There is no specific antidote to an overdose of olanzapine The possibility of
multiple drug involvement should be considered. Establish and maintain an
airway and ensure adequate oxygenation and ventilation. Cardiovascular
monitoring should commence immediately and should include continuous
electrocardiographic monitoring to detect possible arrhythmias.
Contact a Certified Poison Control Center for the most up to date information
on the management of overdosage (1-800-222-1222).
For specific information about overdosage with lithium or valproate, refer to
the Overdosage section of the prescribing information for those products. For
specific information about overdosage with olanzapine and fluoxetine in
combination, refer to the Overdosage section of the Symbyax prescribing
information.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide) for the oral formulations.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking olanzapine as monotherapy or in combination with fluoxetine. If you do not think you are getting better or have any concerns about your condition while taking olanzapine tablets, call your doctor. When using olanzapine and fluoxetine in combination, also refer to the Patient Counseling Information section of the package insert for Symbyax.
Repackaged By / Distributed By: RemedyRepack Inc.
625 Kolter Drive, Indiana, PA 15701
(724) 465-8762
Neuroleptic Malignant Syndrome (NMS)
Patients and caregivers should be counseled that a potentially fatal symptom
complex sometimes referred to as NMS has been reported in association with
administration of antipsychotic drugs, including olanzapine. Signs and
symptoms of NMS include hyperpyrexia, muscle rigidity, altered mental status,
and evidence of autonomic instability (irregular pulse or blood pressure,
tachycardia, diaphoresis, and cardiac dysrhythmia) [see Warnings and Precautions ( 5.3)].
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Patients should be advised to report to their health care provider at the
earliest onset of any signs and symptoms that may be associated with Drug
Reaction with Eosinophilia and Systemic Symptoms (DRESS) [ see Warnings and Precautions ( 5.4) ]
Hyperglycemia and Diabetes Mellitus
Patients should be advised of the potential risk of hyperglycemia-related
adverse reactions. Patients should be monitored regularly for worsening of
glucose control. Patients who have diabetes should follow their doctor's
instructions about how often to check their blood sugar while taking
olanzapine tablets [see Warnings and Precautions ( 5.5)].
Dyslipidemia
Patients should be counseled that dyslipidemia has occurred during treatment
with olanzapine. Patients should have their lipid profile monitored regularly
[see Warnings and Precautions ( 5.5)].
Weight Gain
Patients should be counseled that weight gain has occurred during treatment
with olanzapine. Patients should have their weight monitored regularly [see Warnings and Precautions ( 5.5)].
Orthostatic Hypotension
Patients should be advised of the risk of orthostatic hypotension, especially
during the period of initial dose titration and in association with the use of
concomitant drugs that may potentiate the orthostatic effect of olanzapine,
e.g., diazepam or alcohol [see Warnings and Precautions ( 5.7) and Drug Interactions ( 7)] . Patients should be advised to change positions carefully
to help prevent orthostatic hypotension, and to lie down if they feel dizzy or
faint, until they feel better. Patients should be advised to call their doctor
if they experience any of the following signs and symptoms associated with
orthostatic hypotension: dizziness, fast or slow heart beat, or fainting.
Potential for Cognitive and Motor Impairment
Because olanzapine has the potential to impair judgment, thinking, or motor
skills, patients should be cautioned about operating hazardous machinery,
including automobiles, until they are reasonably certain that olanzapine
therapy does not affect them adversely [see Warnings and Precautions ( 5.12)].
Body Temperature Regulation
Patients should be advised regarding appropriate care in avoiding overheating
and dehydration. Patients should be advised to call their doctor right away if
they become severely ill and have some or all of these symptoms of
dehydration: sweating too much or not at all, dry mouth, feeling very hot,
feeling thirsty, not able to produce urine [see Warnings and Precautions ( 5.13)].
Concomitant Medication
Patients should be advised to inform their healthcare providers if they are
taking, or plan to take, Symbyax. Patients should also be advised to inform
their healthcare providers if they are taking, plan to take, or have stopped
taking any prescription or over-the-counter drugs, including herbal
supplements, since there is a potential for interactions [see Drug Interactions ( 7)].
Alcohol
Patients should be advised to avoid alcohol while taking olanzapine tablets
[see Drug Interactions ( 7)].
Use in Specific Populations
****Pregnancy — Advise women to notify their healthcare provider if they
become pregnant or intend to become pregnant during treatment with olanzapine
tablets. Advise patients that olanzapine tablets may cause extrapyramidal
and/or withdrawal symptoms (agitation, hypertonia, hypotonia, tremor,
somnolence, respiratory distress, and feeding disorder) in a neonate. Advise
patients that there is a pregnancy exposure registry that monitors pregnancy
outcomes in women exposed to olanzapine tablets during pregnancy [see Use in Specific Populations (8.1)].
Lactation — Advise breastfeeding women using olanzapine tablets to monitor
infants for excess sedation, irritability, poor feeding and extrapyramidal
symptoms (tremors and abnormal muscle movements) and to seek medical care if
they notice these signs. [see Use in Specific Populations ( 8.3)].
Infertility — Advise females of reproductive potential that olanzapine tablets
may impair fertility due to an increase in serum prolactin levels. The effects
on fertility are reversible [see Use in Specific Populations ( 8.3)].
Pediatric Use — Olanzapine tablets are indicated for treatment of
schizophrenia and manic or mixed episodes associated with bipolar I disorder
in adolescents 13 to 17 years of age. Compared to patients from adult clinical
trials, adolescents were likely to gain more weight, experience increased
sedation, and have greater increases in total cholesterol, triglycerides, LDL
cholesterol, prolactin, and hepatic aminotransferase levels. Patients should
be counseled about the potential long-term risks associated with olanzapine
tablets and advised that these risks may lead them to consider other drugs
first [see Indications and Usage ( 1.1, 1.2)]. Safety and effectiveness of
olanzapine tablets in patients under 13 years of age have not been
established. Safety and efficacy of olanzapine tablets and fluoxetine in
combination in patients 10 to 17 years of age have been established for the
acute treatment of depressive episodes associated with bipolar I disorder.
Safety and effectiveness of olanzapine tablets and fluoxetine in combination
in patients <10 years of age have not been established [see Warnings and Precautions ( 5.5) and Use in Specific Populations ( 8.4)].
Need for Comprehensive Treatment Program in Pediatric Patients
Olanzapine is indicated as an integral part of a total treatment program for pediatric patients with schizophrenia and bipolar disorder that may include other measures (psychological, educational, social) for patients with the disorder. Effectiveness and safety of olanzapine have not been established in pediatric patients less than 13 years of age. Atypical antipsychotics are not intended for use in the pediatric patient who exhibits symptoms secondary to environmental factors and/or other primary psychiatric disorders. Appropriate educational placement is essential and psychosocial intervention is often helpful. The decision to prescribe atypical antipsychotic medication will depend upon the healthcare provider's assessment of the chronicity and severity of the patient’s symptoms [see Indications and Usage (1.3)].
All other trademarks are the properties of their respective owners.
Revised : September 2022
Repackaged and Distributed By:
Remedy Repack, Inc.
625 Kolter Dr. Suite #4 Indiana, PA 1-724-465-8762
.
