Milnacipran HCl
These highlights do not include all the information needed to use MILNACIPRAN HYDROCHLORIDE TABLETS safely and effectively. See full prescribing information for MILNACIPRAN HYDROCHLORIDE TABLETS. MILNACIPRAN HYDROCHLORIDE tablets, for oral useInitial U.S. Approval: 2009
eaa14195-1b9c-423c-9412-d2fe0857e39d
HUMAN PRESCRIPTION DRUG LABEL
Mar 22, 2023
Amneal Pharmaceuticals LLC
DUNS: 123797875
Products 4
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Milnacipran HCl
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (10)
Milnacipran HCl
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (10)
Milnacipran HCl
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Milnacipran HCl
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
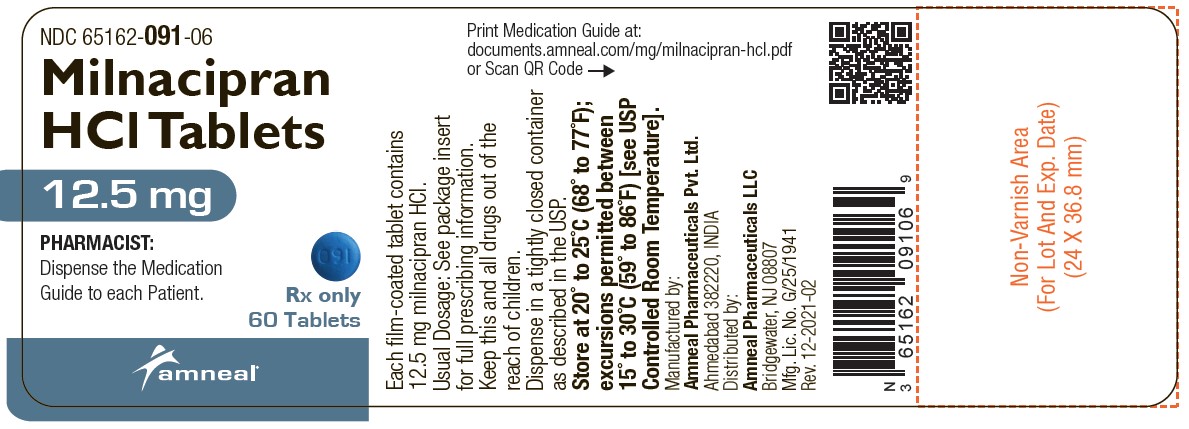
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
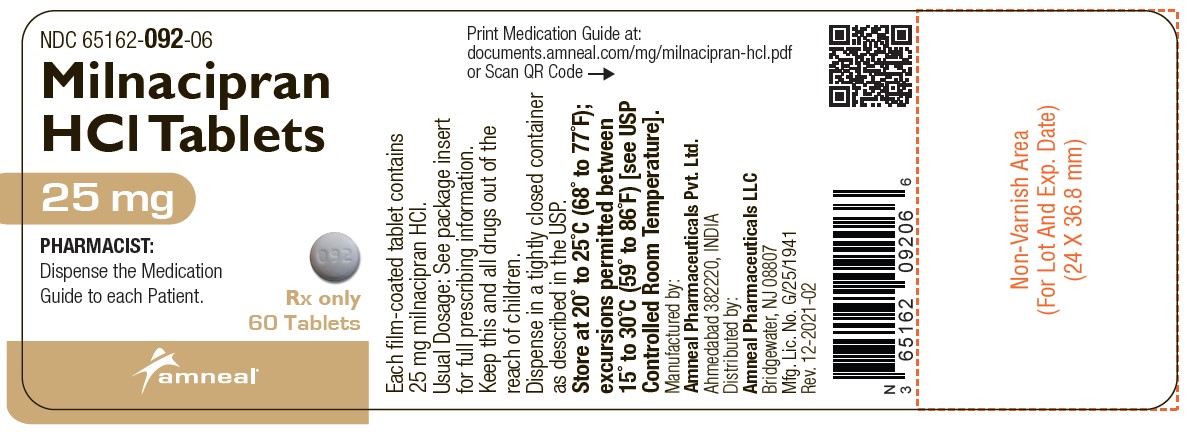
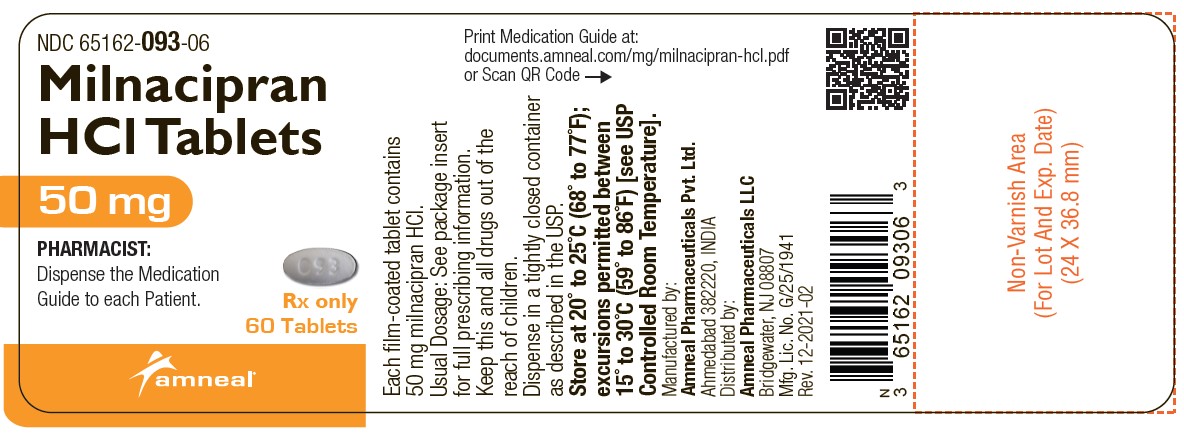
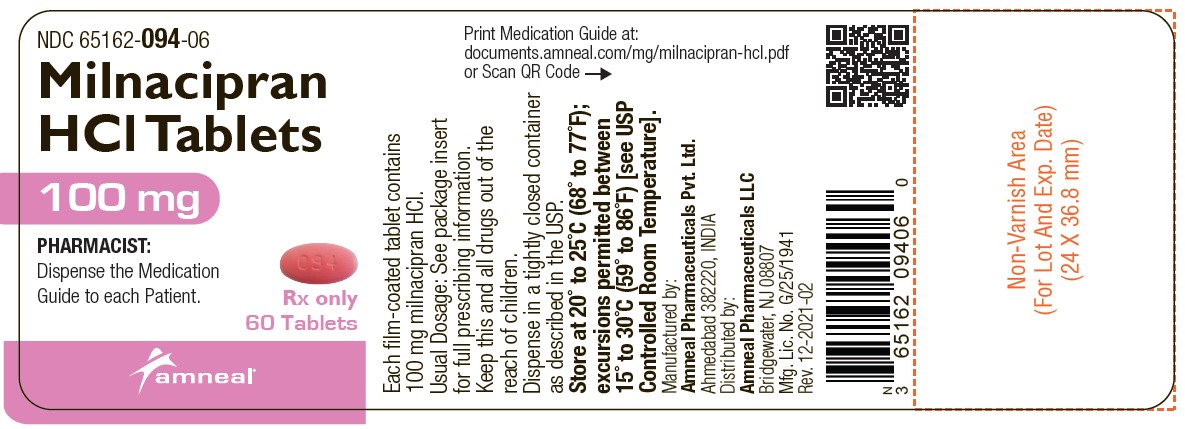
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 65162-091-06
Milnacipran HCl tablets, 12.5 mg
Rx only
60 Tablets
Amneal Pharmaceuticals LLC
NDC 65162-092-06
Milnacipran HCl tablets, 25 mg
Rx only
60 Tablets
Amneal Pharmaceuticals LLC
NDC 65162-093-06
Milnacipran HCl tablets, 50 mg
Rx only
60 Tablets
Amneal Pharmaceuticals LLC
NDC 65162-094-06
Milnacipran HCl tablets, 100 mg
Rx only
60 Tablets
Amneal Pharmaceuticals LLC
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
4.1 Monoamine Oxidase Inhibitors (MAOIs)
The use of MAOIs intended to treat psychiatric disorders with milnacipran HCl or within 5 days of stopping treatment with milnacipran HCl is contraindicated because of an increased risk of serotonin syndrome. The use of milnacipran HCl within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated [see Dosage and Administration (2.5), Warnings and Precautions (5.2)].
Starting milnacipran HCl in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome [see Dosage and Administration (2.6), Warnings and Precautions (5.2)].
- Serotonin Syndrome and MAOIs: Do not use MAOIs intended to treat psychiatric disorders with milnacipran HCl or within 5 days of stopping treatment with milnacipran HCl. Do not use milnacipran HCl within 14 days of stopping an MAOI intended to treat psychiatric disorders. In addition, do not start milnacipran HCl in a patient who is being treated with linezolid or intravenous methylene blue. (4.1, 5.2)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Suicide Risk
Milnacipran HCl is a selective serotonin and norepinephrine re-uptake inhibitor (SNRI), similar to some drugs used for the treatment of depression and other psychiatric disorders.
Patients, both adult and pediatric, with depression or other psychiatric disorders may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking these medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants, including drugs that inhibit the reuptake of norepinephrine and/or serotonin, may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment.
In the placebo-controlled clinical trials of adults with fibromyalgia, among the patients who had a history of depression at treatment initiation, the incidence of suicidal ideation was 0.5% in patients treated with placebo, 0% in patients treated with milnacipran HCl 100 mg/day, and 1.3% in patients treated with milnacipran HCl 200 mg/day. No suicides occurred in the short- term or longer-term (up to 1 year) fibromyalgia trials.
Pooled analyses of short-term placebo-controlled trials of drugs used to treat depression (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with these drugs compared to placebo in adults beyond age 24; there was a reduction in suicidality risk with antidepressants compared to placebo in adults age 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 drugs used to treat depression in over 4,400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short- term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients.
There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk of differences (drug versus placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 patients treated) are provided inTable 1.
Table 1: Risk Differences (Drug – Placebo) in the number of Cases of Suicidality, per 1,000 patients treated
|
Age Range |
Drug-Placebo Difference in Number of Cases of Suicidality per 1,000 Patients Treated |
|
< 18 |
14 additional cases |
|
18 to 24 |
5 additional cases |
|
Decreases Compared to Placebo | |
|
25 to 64 |
1 fewer case |
|
≥ 65 |
6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e. beyond several months.
However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with drugs inhibiting the reuptake of norepinephrine and/or serotonin for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, have been reported in adult and pediatric patients being treated with drugs inhibiting the reuptake of norepinephrine and/or serotonin for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients who may experience worsening depressive symptoms, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe or abrupt in onset, or were not part of the patient’s presenting symptoms.
If the decision has been made to discontinue treatment due to worsening depressive symptoms or emergent suicidality, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can produce withdrawal symptoms [see Dosage and Administration (2.1, 2.4) and Warnings and Precautions (5.7)].
Families and caregivers of patients being treated with drugs inhibiting the reuptake of norepinephrine and/or serotonin for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for milnacipran HCl should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
5.2 Serotonin Syndrome
Selective-serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), including milnacipran HCl, can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin i.e. MAOIs [see Contraindications (4), Drug Interactions (7.1)]. Serotonin syndrome can also occur when these drugs are used alone.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of milnacipran HCl with MAOIs is contraindicated. In addition, do not initiate milnacipran HCl in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection). If it is necessary to initiate treatment with a MAOI such as linezolid or intravenous methylene blue in a patient taking milnacipran HCl, discontinue milnacipran HCl before initiating treatment with the MAOI [see Dosage and Administration (2.5, 2.6), Contraindications (4), Drug Interactions (7.1)].
Monitor all patients taking milnacipran HCl for the emergence of serotonin syndrome. Discontinue treatment with milnacipran HCl and any concomitant serotonergic agents immediately if the above events occur and initiate supportive symptomatic treatment. If concomitant use of milnacipran HCl with other serotonergic drugs is clinically warranted, inform patients of the increased risk for serotonin syndrome and monitor for symptoms.
5.3 Elevated Blood Pressure
A double-blind, placebo-controlled ambulatory blood pressure monitoring (ABPM) study was conducted to evaluate the effects of milnacipran (up to 200 mg/day) on blood pressure in 321 fibromyalgia patients. Among fibromyalgia patients who were normotensive at baseline, an analysis of the blood pressure findings demonstrated a substantially higher proportion of milnacipran HCl-treated patients had a hypertensive blood pressure measurement at the Week 4, 50 mg BID steady-state visit (17.7% [n=21/119]) and the Week 7, 100 mg BID steady- state visit (14.3% [n=15/105]) as compared to placebo-treated patients (3.7% [n=2/54] and 0% [0/49] at the Week 4 and Week 7 visits, respectively). Hypertension was defined as mean systolic blood pressure (SBP) ≥ 140 mmHg and change from baseline in mean SBP ≥ 10 mmHg or mean diastolic blood pressure (DBP) ≥ 90 mmHg and change from baseline in mean DBP ≥ 5 mmHg for the 12-hour period post AM study drug measurement at that visit. Furthermore, 1.9% (4/210) of milnacipran HCl-treated and 0.9% (1/111) of placebo patients discontinued treatment for increases in blood pressure.
The increased risk of blood pressure measurements in the hypertensive range in milnacipran HCl-treated patients is supported by substantial increases in mean SBP and DBP measurements observed in the ABPM study.Table 2 shows that, following treatment with milnacipran HCl 50 mg BID for three weeks in patients who were normotensive at baseline, the mean increase from baseline was 5 mmHg in systolic blood pressure (SBP) and diastolic blood pressure (DBP). After further treatment with milnacipran HCl 100 mg BID for two weeks, the mean increase from baseline in SBP and DBP was 6 mmHg. Similar elevations occurred in milnacipran HCl-treated patients who were hypertensive at baseline.
Table 2: Mean (Standard Error) Change from Baseline in Mean 24-hour Systolic and Diastolic Blood Pressure (mmHg) of Milnacipran or Placebo following 4 Weeks of Treatment (50mg BID) and a Subsequent 2 Weeks of Treatment (100mg BID)
|
Normotensive |
Hypertensive | |||||
|
n |
Systolic |
Diastolic |
n |
Systolic |
Diastolic | |
|
Placebo |
39 |
0(2) |
-1(1) |
50 |
0(2) |
0(2) |
|
50 mg BID* |
92 |
5(1) |
5(1) |
84 |
5(2) |
4(1) |
|
Placebo |
37 |
0(2) |
-1(1) |
47 |
-1(2) |
0(1) |
|
100 mg BID^ |
82 |
6(1) |
6(1) |
80 |
5(2) |
4(1) |
|
*Blood pressure measurements made after 3 weeks of milnacipran 50mg BID | ||||||
|
^Blood pressure measurements made after 2 weeks of milnacipran 100mg BID |
Similar patterns of treatment-emergent blood pressure elevations were observed in Phase 3 and clinical pharmacology studies as manifested by an increased risk of new onset hypertension or substantial increases in end of study blood pressure measurements in patients with hypertension at baseline**(Table 3)**.
Table 3: Blood pressure changes in Phase 3 randomized controlled trials
|
Milnacipran |
Milnacipran |
Placebo | |
|
FM patients normotensive at baseline |
20% |
17% |
7% |
|
FM patients with sustained increases in |
9% |
6% |
2% |
|
FM patients with sustained increases in |
13% |
10 % |
4% |
|
FM patients hypertensive at baseline |
10% |
7% |
4% |
|
FM patients hypertensive at baseline |
8% |
6% |
3% |
Sustained increases in blood pressure may have adverse consequences. Cases of elevated blood pressure requiring immediate treatment have been reported.
Concomitant use of milnacipran HCl with drugs that increase blood pressure and heart rate has not been evaluated and such combinations should be used with caution [see Drug Interactions (7)].
Effects of milnacipran HCl on blood pressure in patients with significant hypertension or cardiac disease have not been systematically evaluated. Milnacipran HCl should be used with caution in these patients.
Measure blood pressure prior to initiating treatment and periodically monitor blood pressure throughout milnacipran HCl treatment. Treat pre-existing hypertension and other cardiovascular disease before starting therapy with milnacipran HCl. For patients who experience a sustained increase in blood pressure while receiving milnacipran HCl, either reduce the dose or discontinue treatment with milnacipran HCl if clinically warranted.
5.4 Elevated Heart Rate
A double-blind, placebo-controlled ABPM study was conducted to evaluate the effects of milnacipran (up to 200 mg/day) on blood pressure in 321 fibromyalgia patients [see Warnings and Precautions (5.3)]. Information on heart rate was also collected. Following treatment with milnacipran HCl 50 mg BID for three weeks in patients who were normotensive at baseline, the mean increase in mean 24-hour heart rate from baseline was 13 beats per minute. After further treatment with milnacipran HCl 100 mg BID for two weeks, the mean increase from baseline in heart rate was 13 beats per minute.
Similar trends were observed in the clinical trials where milnacipran HCl treatment was associated with mean increases in heart rate of approximately 7 to 8 beats per minute [see Adverse Reactions (6.1)].
Increases in heart rate ≥ 20 beats per minute occurred more frequently in milnacipran HCl-treated patients when compared to placebo (8% in the milnacipran HCl 50 mg BID and 100 mg BID treatment arms versus 0.3% in the placebo arm).
Milnacipran HCl has not been systematically evaluated in patients with a cardiac rhythm disorder.
Measure heart rate prior to initiating treatment and periodically monitor the heart rate throughout milnacipran HCl treatment. Treat pre-existing tachyarrhythmias and other cardiac disease before starting therapy with milnacipran HCl. For patients who experience a sustained increase in heart rate while receiving milnacipran HCl, either reduce the dose or discontinue treatment with milnacipran HCl if clinically warranted.
5.5 Seizures
Milnacipran HCl has not been systematically evaluated in patients with a seizure disorder. In clinical trials evaluating milnacipran HCl in patients with fibromyalgia, seizures/convulsions have not been reported. However, seizures have been reported infrequently in patients treated with milnacipran HCl for disorders other than fibromyalgia. Milnacipran HCl should be prescribed with care in patients with a history of a seizure disorder.
5.6 Hepatotoxicity
In the placebo-controlled fibromyalgia trials, increases in the number of patients treated with milnacipran HCl with mild elevations of ALT or AST (1 to 3 times the upper limit of normal, ULN) were observed. Increases in ALT were more frequently observed in the patients treated with milnacipran HCl 100 mg/day (6%) and milnacipran HCl 200 mg/day (7%), compared to the patients treated with placebo (3%). One patient receiving milnacipran HCl 100 mg/day (0.2%) had an increase in ALT greater than 5 times the upper limit of normal but did not exceed 10 times the upper limit of normal. Increases in AST were more frequently observed in the patients treated with milnacipran HCl 100 mg/day (3%) and milnacipran HCl 200 mg/day (5%) compared to the patients treated with placebo (2%).
The increases of bilirubin observed in the fibromyalgia clinical trials were not clinically significant.
No case met the criteria of elevated ALT > 3x ULN and associated with an increase in bilirubin ≥ 2x ULN.
There have been cases of increased liver enzymes and reports of severe liver injury, including fulminant hepatitis with milnacipran from foreign post- marketing experience. In the cases of severe liver injury, there were significant underlying clinical conditions and/or the use of multiple concomitant medications. Because of underreporting, it is impossible to provide an accurate estimate of the true incidence of these reactions.
Discontinue milnacipran HCl in patients who develop jaundice or other evidence of liver dysfunction. Treatment with milnacipran HCl should not be resumed unless another cause can be established.
Milnacipran HCl should ordinarily not be prescribed to patients with substantial alcohol use or evidence of chronic liver disease.
5.7 Discontinuation of Treatment with Milnacipran HCl
Withdrawal symptoms have been observed in clinical trials following discontinuation of milnacipran, as with other SNRIs and SSRIs.
During marketing of milnacipran, and other SNRIs and SSRIs, there have been spontaneous reports of adverse events indicative of withdrawal and physical dependence occurring upon discontinuation of these drugs, particularly when discontinuation is abrupt. The adverse events include the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. Although these events are generally self-limiting, some have been reported to be severe.
Monitor patients for these symptoms when discontinuing treatment with milnacipran HCl. Milnacipran HCl should be tapered after extended use. Do not abruptly discontinue. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate [see Dosage and Administration (2.4)].
5.8 Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including milnacipran HCl. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SNRIs, SSRIs, or milnacipran HCl. Also, patients taking diuretics or who are otherwise volume-depleted may be at greater risk [see Geriatric Use (8.5)]. Consider discontinuation of milnacipran HCl in patients with symptomatic hyponatremia.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.9 Increased Risk of Bleeding
Drugs that interfere with serotonin reuptake, including milnacipran HCl, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDS), warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs have ranged from ecchymosis, hematoma, epistaxis, and petechiae to life-threatening hemorrhages.
Inform patients about the risk of bleeding associated with the concomitant use of milnacipran HCl and NSAIDs, aspirin, or other drugs that affect coagulation [see Drug Interactions (7.1)].
5.10 Activation of Mania
No activation of mania or hypomania was reported in the clinical trials evaluating effects of milnacipran HCl in patients with fibromyalgia. However, those clinical trials excluded patients with current major depressive episode. Activation of mania and hypomania have been reported in patients with mood disorders who were treated with other similar drugs for major depressive disorder. As with these other agents, use milnacipran HCl cautiously in patients with a history of mania.
5.11 Patients with a History of Dysuria
Because of their noradrenergic effect, SNRIs including milnacipran HCl, can affect urethral resistance and micturition. In the controlled fibromyalgia trials, dysuria occurred more frequently in patients treated with milnacipran HCl (1%) than in placebo-treated patients (0.5%). Caution is advised in use of milnacipran HCl in patients with a history of dysuria, notably in male patients with prostatic hypertrophy, prostatitis, and other lower urinary tract obstructive disorders. Male patients are more prone to genitourinary adverse effects, such as dysuria or urinary retention, and may experience testicular pain or ejaculation disorders.
5.12 Sexual Dysfunction
Use of SNRIs, including milnacipran HCl, may cause symptoms of sexual dysfunction [see Adverse Reactions (6.1, 6.2)]. In male patients, SNRI use may result in ejaculatory delay or failure, decreased libido, and erectile dysfunction. In female patients, SNRI use may result in decreased libido and delayed or absent orgasm.
It is important for prescribers to inquire about sexual function prior to initiation of milnacipran HCl and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported. When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including the underlying psychiatric disorder. Discuss potential management strategies to support patients in making informed decisions about treatment.
5.13 Angle Closure Glaucoma
The pupillary dilation that occurs following use of SNRI drugs including milnacipran HCl may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.14 Concomitant Use with Alcohol
In clinical trials, more patients treated with milnacipran HCl developed elevated transaminases than did placebo treated patients [see Warnings and Precautions (5.6)]. Because it is possible that milnacipran may aggravate pre- existing liver disease, milnacipran HCl should not be prescribed to patients with substantial alcohol use or evidence of chronic liver disease.
- Suicidality: Monitor for worsening of depressive symptoms and suicide risk. (5.1)
- Serotonin Syndrome: Increased risk when co-administered with other serotonergic agents (e.g., SSRI, SNRI, triptans), but also when taken alone. If it occurs, discontinue Milnacipran HCl, and initiate supportive treatment. (5.2)
- Elevated Blood Pressure and Heart Rate: Milnacipran HCl may increase blood pressure and heart rate. Measure blood pressure and heart rate prior to initiating treatment with milnacipran HCl and monitor periodically throughout treatment. (5.3, 5.4)
- Seizures: Cases have been reported with milnacipran HCl therapy. Prescribe milnacipran HCl with care in patients with a history of seizure disorder. (5.5)
- Hepatotoxicity: Milnacipran HCl may cause elevations of ALT and AST. Avoid concomitant use of milnacipran HCl in patients with substantial alcohol use or chronic liver disease. (5.6)
- Discontinuation: Withdrawal symptoms have been reported in patients when discontinuing treatment with milnacipran HCl. A gradual dose reduction is recommended. (5.7)
- Abnormal Bleeding: Milnacipran HCl may increase the risk of bleeding events. Caution patients about the risk of bleeding associated with the concomitant use of milnacipran HCl and NSAIDs, aspirin, or other drugs that affect coagulation. (5.9)
- History of Dysuria: Male patients with a history of obstructive uropathies may experience higher rates of genitourinary adverse events. (5.11)
- Sexual Dysfunction: Milnacipran HCl use may cause symptoms of sexual dysfunction. (5.12)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Patient Exposure
Milnacipran HCl was evaluated in three double-blind placebo-controlled trials involving 2,209 fibromyalgia patients (1,557 patients treated with milnacipran HCl and 652 patients treated with placebo) for a treatment period up to 29 weeks.
The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation.
Adverse Reactions Leading to Discontinuation
In placebo-controlled trials in patients with fibromyalgia, 23% of patients treated with milnacipran HCl 100 mg/day, 26% of patients treated with milnacipran HCl 200 mg/day discontinued prematurely due to adverse reactions, compared to 12% of patients treated with placebo. The adverse reactions that led to withdrawal in ≥ 1% of patients in the milnacipran HCl treatment group and with an incidence rate greater than that in the placebo treatment group were nausea (milnacipran 6%, placebo 1%), palpitations (milnacipran 3%, placebo 1%), headache (milnacipran 2%, placebo 0%), constipation (milnacipran 1%, placebo 0%), heart rate increased (milnacipran 1%, placebo 0%), hyperhidrosis (milnacipran 1%, placebo 0%), vomiting (milnacipran 1%, placebo 0%), and dizziness (milnacipran 1% and placebo 0.5%). Discontinuation due to adverse reactions was generally more common among patients treated with milnacipran HCl 200 mg/day compared to milnacipran HCl 100 mg/day.
Most Common Adverse Reactions in Placebo Controlled Trials
In the placebo-controlled fibromyalgia patient trials, the most frequently occurring adverse reaction in clinical trials was nausea. The most common adverse reactions (incidence ≥ 5% and twice placebo) in patients treated with milnacipran HCl were constipation, hot flush, hyperhidrosis, vomiting, palpitations, heart rate increased, dry mouth, and hypertension.
Table 4 lists all adverse reactions that occurred in at least 2% of patients treated with milnacipran HCl at either 100 or 200 mg/day and at an incidence greater than that of placebo.
**Table 4: Treatment-Emergent Adverse Reaction Incidence in Placebo Controlled Trials in Fibromyalgia Patients (Events Occurring in at Least 2% of All ****Milnacipran HCl-Treated Patients and Occurring More Frequently in Either **Milnacipran HCl Treatment Group Than in the Placebo Treatment Group)
|
System Organ Class– |
Milnacipran HCl |
Milnacipran HCl |
All****Milnacipran HCl |
Placebo |
|
Cardiac Disorders | ||||
|
Palpitations |
8 |
7 |
7 |
2 |
|
Tachycardia |
3 |
2 |
2 |
1 |
|
Eye Disorders | ||||
|
Vision blurred |
1 |
2 |
2 |
1 |
|
Gastrointestinal Disorders | ||||
|
Nausea |
35 |
39 |
37 |
20 |
|
Constipation |
16 |
15 |
16 |
4 |
|
Vomiting |
6 |
7 |
7 |
2 |
|
Dry mouth |
5 |
5 |
5 |
2 |
|
Abdominal pain |
3 |
3 |
3 |
2 |
|
General Disorders | ||||
|
Chest pain |
3 |
2 |
2 |
2 |
|
Chills |
1 |
2 |
2 |
0 |
|
Chest discomfort |
2 |
1 |
1 |
1 |
|
Infections | ||||
|
Upper respiratory tract infection |
7 |
6 |
6 |
6 |
|
Investigations | ||||
|
Heart rate increased |
5 |
6 |
6 |
1 |
|
Blood pressure increased |
3 |
3 |
3 |
1 |
|
Metabolism and Nutrition | ||||
|
Decreased appetite |
1 |
2 |
2 |
0 |
|
Nervous System Disorders | ||||
|
Headache |
19 |
17 |
18 |
14 |
|
Dizziness |
11 |
10 |
10 |
6 |
|
Migraine |
6 |
4 |
5 |
3 |
|
Paresthesia |
2 |
3 |
2 |
2 |
|
Tremor |
2 |
2 |
2 |
1 |
|
Hypoesthesia |
1 |
2 |
1 |
1 |
|
Tension headache |
2 |
1 |
1 |
1 |
|
Psychiatric Disorders | ||||
|
Insomnia |
12 |
12 |
12 |
10 |
|
Anxiety |
5 |
3 |
4 |
4 |
|
Respiratory Disorders | ||||
|
Dyspnea |
2 |
2 |
2 |
1 |
|
Skin Disorders | ||||
|
Hyperhidrosis |
8 |
9 |
9 |
2 |
|
Rash |
3 |
4 |
3 |
2 |
|
Pruritus |
3 |
2 |
2 |
2 |
|
Vascular Disorders | ||||
|
Hot flush |
11 |
12 |
12 |
2 |
|
Hypertension |
7 |
4 |
5 |
2 |
|
Flushing |
2 |
3 |
3 |
1 |
Weight Changes
In placebo-controlled fibromyalgia clinical trials, patients treated with milnacipran HCl for up to 3 months experienced a mean weight loss of approximately 0.8 kg in both the milnacipran HCl 100 mg/day and the milnacipran HCl 200 mg/day treatment groups, compared with a mean weight loss of approximately 0.2 kg in placebo-treated patients.
Genitourinary Adverse Reactions in Males
In the placebo-controlled fibromyalgia studies, the following treatment- emergent adverse reactions related to the genitourinary system were observed in at least 2% of male patients treated with milnacipran HCl, and occurred at a rate greater than in placebo-treated male patients: dysuria, ejaculation disorder, erectile dysfunction, ejaculation failure, libido decreased, prostatitis, scrotal pain, testicular pain, testicular swelling, urinary hesitation, urinary retention, urethral pain, and urine flow decreased.
Other Adverse Reactions Observed During Clinical Trials of****Milnacipran HCl in Fibromyalgia
Following is a list of frequent (those occurring on one or more occasions in at least 1/100 patients) treatment-emergent adverse reactions reported from 1,824 fibromyalgia patients treated with milnacipran HCl for periods up to 68 weeks. The listing does not include those events already listed inTable 4, those events for which a drug cause was remote, those events which were so general as to be uninformative, and those events reported only once which did not have a substantial probability of being acutely life threatening.
Adverse reactions are categorized by body system and listed in order of decreasing frequency. Adverse reactions of major clinical importance are described in the Warnings and Precautions section (5).
Gastrointestinal Disorders - diarrhea, dyspepsia, gastroesophageal reflux
disease, flatulence, abdominal distension
General Disorders - fatigue, peripheral edema, irritability, pyrexia
Infections - urinary tract infection, cystitis
Injury, Poisoning, and Procedural Complications - contusion, fall
Investigations - weight decreased or increased
Metabolism and Nutrition Disorders - hypercholesterolemia
Nervous System Disorders - somnolence, dysgeusia
Psychiatric Disorders - depression, stress
Skin Disorders - night sweats
6.2 Post-marketing Experience
The following additional adverse reactions have been identified from spontaneous reports of milnacipran HCl received worldwide. These adverse reactions have been chosen for inclusion because of a combination of seriousness, frequency of reporting, or potential causal connection to milnacipran HCl. However, because these adverse reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events include:
Blood and Lymphatic System Disorders - leukopenia, neutropenia, thrombocytopenia
Cardiac Disorders - supraventricular tachycardia, Takotsubo cardiomyopathy
Eye Disorders - accommodation disorder
Endocrine Disorders - hyperprolactinemia
Gastrointestinal Disorders - acute pancreatitis
Hepatobiliary Disorders - hepatitis
Metabolism and Nutrition Disorders - anorexia, hyponatremia
Musculoskeletal and Connective Tissue Disorders - rhabdomyolysis
Nervous System Disorders - convulsions (including grand mal), loss of consciousness, Parkinsonism
Psychiatric Disorders - aggression, anger, delirium, hallucination, homicidal ideation
Renal and Urinary Disorders - acute renal failure
Reproductive System and Breast Disorders - galactorrhea, decreased libido, delayed or absent orgasm
Skin Disorders - erythema multiforme, Stevens Johnson syndrome
Vascular Disorders - hypertensive crisis
The most frequently occurring adverse reactions (≥ 5% and greater than placebo) were nausea, headache, constipation, dizziness, insomnia, hot flush, hyperhidrosis, vomiting, palpitations, heart rate increased, dry mouth, and hypertension. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals, at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Milnacipran undergoes minimal CYP450 related metabolism, with the majority of the dose excreted unchanged in urine (55%), and has a low binding to plasma proteins (13%). In vitro and in vivo studies showed that milnacipran HCl is unlikely to be involved in clinically significant pharmacokinetic drug interactions [see Pharmacokinetics in Special Populations (12.3)].
7.1 Monoamine Oxidase Inhibitors (MAOIs)
[See Dosage and Administration (2.5 and 2.6), Contraindications (4.1), Warnings and Precautions (5.2)].
7.2 Serotonergic Drugs
[See Dosage and Administration (2.5 and 2.6), Contraindications (4.1), Warnings and Precautions (5.2)].
7.3 Triptans
There have been rare post-marketing reports of serotonin syndrome with use of an SSRI and a triptan. If concomitant treatment of milnacipran HCl with a triptan is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases [see Warnings and Precautions (5.2)].
7.4 Catecholamines
Milnacipran HCl inhibits the reuptake of norepinephrine. Therefore, concomitant use of milnacipran HCl with epinephrine and norepinephrine may be associated with paroxysmal hypertension and possible arrhythmia [see Warnings and Precautions (5.3, 5.4)].
7.5 CNS-active drugs
Given the primary CNS effects of milnacipran HCl, use caution when it is taken in combination with other centrally acting drugs, including those with a similar mechanism of action.
Clomipramine: In a drug-drug interaction study, an increase in euphoria and postural hypotension was observed in patients who switched from clomipramine to milnacipran HCl.
7.6 Clinically Important Interactions with Select Cardiovascular Agents
Digoxin: Use of milnacipran HCl concomitantly with digoxin may be associated with potentiation of adverse hemodynamic effects. Postural hypotension and tachycardia have been reported in combination therapy with intravenously administered digoxin (1 mg). Avoid co-administration of milnacipran HCl and intravenous digoxin [see Warnings and Precautions (5.3, 5.4)].
Clonidine: Because milnacipran HCl inhibits norepinephrine reuptake, co- administration with clonidine may inhibit clonidine’s anti-hypertensive effect.
- Milnacipran HCl is unlikely to be involved in clinically significant pharmacokinetic drug interactions. (7)
- Pharmacodynamic interactions of milnacipran HCl with other drugs can occur. (7)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
Milnacipran HCl tablets are given orally with or without food.
Taking milnacipran HCl tablets with food may improve the tolerability of the drug.
2.1 Recommended Dosing
The recommended dose of milnacipran HCl tablets is 100 mg/day (50 mg twice daily).
Based on efficacy and tolerability dosing may be titrated according to the
following schedule:
Day 1: 12.5 mg once
Days 2 to 3: 25 mg/day (12.5 mg twice daily)
Days 4 to 7: 50 mg/day (25 mg twice daily)
After Day 7: 100 mg/day (50 mg twice daily)
Based on individual patient response, the dose may be increased to 200 mg/day (100 mg twice daily).
Doses above 200 mg/day have not been studied.
Taper milnacipran HCl tablets and do not abruptly discontinue after extended use [see Dosage and Administration (2.4) and Warnings and Precautions (5.7)].
2.2 Patients with Renal Insufficiency
No dosage adjustment is necessary in patients with mild renal impairment.
Use milnacipran HCl tablets with caution in patients with moderate renal impairment.
For patients with severe renal impairment (indicated by an estimated creatinine clearance of 5 to 29 mL/min), reduce the maintenance dose by 50% to 50 mg/day (25 mg twice daily).
Based on individual patient response, the dose may be increased to 100 mg/day (50 mg twice daily).
Milnacipran HCl tablets are not recommended for patients with end-stage renal disease.
2.3 Patients with Hepatic Insufficiency
No dosage adjustment is necessary for patients with hepatic impairment.
As with any drug, exercise caution in patients with severe hepatic impairment.
2.4 Discontinuing Milnacipran HCl Tablets
Withdrawal symptoms have been observed in clinical trials following discontinuation of milnacipran, as with other serotonin and norepinephrine re- uptake inhibitors (SNRIs) and selective serotonin re-uptake inhibitors (SSRIs). Monitor patients for these symptoms when discontinuing treatment. Taper milnacipran HCl tablets and do not abruptly discontinue after extended use [see Warnings and Precautions (5.7)].
2.5 Switching a Patient to or from a Monoamine Oxidase Inhibitor (MAOI)
Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of a MAOI intended to treat psychiatric disorders and initiation of therapy with milnacipran HCl tablets. Conversely, allow at least 5 days after stopping milnacipran HCl tablets before starting a MAOI intended to treat psychiatric disorders [see Contraindications (4.1)].
2.6 Use of Milnacipran HCl Tablets with other MAOIs such as Linezolid or
Methylene Blue
Do not start milnacipran HCl tablets in a patient being treated with linezolid or intravenous methylene blue because there is increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, consider other interventions, including hospitalization [see Contraindications (4.1)].
In some cases, a patient already receiving milnacipran HCl tablets therapy may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, discontinue milnacipran HCl tablets promptly, and consider administering linezolid or intravenous methylene blue. Monitor the patient for symptoms of serotonin syndrome for 5 days or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with milnacipran HCl tablets may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue [see Warnings and Precautions (5.2)].
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with milnacipran HCl tablets are unclear. The clinician should nevertheless be aware of the possibility of emergent symptoms of serotonin syndrome with such use [see Warnings and Precautions (5.2)].
- Administer milnacipran HCl tablets in two divided doses per day. (2.1)
- Based on efficacy and tolerability, dosing may be titrated according to the following schedule (2.1):
Day 1: 12.5 mg once
Days 2 to 3: 25 mg/day (12.5 mg twice daily)
Days 4 to 7: 50 mg/day (25 mg twice daily)
After Day 7: 100 mg/day (50 mg twice daily)
- Recommended dose is 100 mg/day. (2.1)
- May be increased to 200 mg/day based on individual patient response. (2.1)
- Adjust dose in patients with severe renal impairment. (2.2)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to milnacipran HCl during pregnancy.
Physicians are advised to recommend that pregnant patients taking milnacipran HCl enroll in the milnacipran HCl Pregnancy Registry. Enrollment is voluntary and may be initiated by pregnant patients or their healthcare providers by contacting the registry at X-XXX-XXX-XXXX or by email at xxxxxxxx@xxxxxx.com. Data forms may also be downloaded from the registry website at www.xxxxxxxxxxxx.com.
Risk Summary
The available data on milnacipran HCl use in pregnant women are insufficient to evaluate for a drug associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. There are risks associated with exposure to serotonin and norepinephrine reuptake inhibitors (SNRIs) and selective- serotonin reuptake inhibitors (SSRIs), including milnacipran HCl, during pregnancy (see Clinical Considerations). Animal reproduction studies have been performed in rats, rabbits and mice. Milnacipran was shown to increase embryofetal and perinatal lethality in rats and the incidence of a minor skeletal variation in rabbits at doses below (rat) or approximately equal to (rabbit) the maximum recommended human dose (MRHD) of 200 mg/day on a mg/m2 basis. No effects were seen in mice when treated with milnacipran during the period of organogenesis at doses up to 3 times the MHRD on a mg/m2 basis (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Consideration
Maternal adverse reactions
Use of SNRIs in late pregnancy may be associated with an increased risk of postpartum hemorrhage [see Warnings and Precautions (5.9)].
Fetal/Neonatal adverse reactions
Neonates exposed to SNRIs or SSRIs, including milnacipran, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These findings are consistent with either a direct toxic effect of SSRIs and SNRIs or possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome [see Warnings and Precautions (5.2, 5.7)].
Data
Animal Data
Studies were conducted in rats, rabbits and mice with dosing of milnacipran during the period of organogenesis. In rats, milnacipran was shown to increase embryo fetal lethality at doses of 5 mg/kg/day (0.25 times the MRHD on a mg/m2 basis). In rabbits, dose-dependent increases in the incidence of the skeletal variation of an extra single rib were observed in several pups from multiple litters in the absence of maternal toxicity at 15 mg/kg/day (1.5 times the MRHD on a mg/m2 basis). The clinical significance of this finding is unknown. In mice, no embryotoxic or teratogenic effects were seen at doses up to 125 mg/kg/day (3 times the MRHD on a mg/m2 basis).
With peri- and postnatal exposure to oral milnacipran in rats, decreases in viability and body weight were observed on Postpartum Day 4 at a dose of 5 mg/kg/day (approximately 0.25 times the MRHD on a mg/m2 basis). The no-effect dose for maternal and offspring toxicity was 2.5 mg/kg/day (approximately 0.1 times the MRHD on a mg/m2 basis).
8.2 Lactation
Risk Summary
Milnacipran is present in human milk [see Data]. There are no reports on the effects of milnacipran on the breastfed child and on milk production/excretion. However, there are reports of agitation, irritability, poor feeding, and poor weight gain in infants exposed to SSRIs or SNRIs through breast milk (see Clinical Considerations).
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for milnacipran and any potential adverse effects on the breastfed child from milnacipran or from the underlying maternal conditions.
Clinical Considerations
Monitor infants exposed to milnacipran for agitation, irritability, poor feeding and poor weight gain.
Data
Human Data
Milnacipran is present in the milk of lactating women treated with milnacipran. In a lactation pharmacokinetic study with milnacipran, a single, oral dose of 50 mg milnacipran HCl tablet was administered to 8 lactating women who were at least 12 weeks postpartum and weaning their infants. The milk/plasma AUC ratio of milnacipran was 1.85 ± 0.38. The maximum estimated weight adjusted daily infant dose for milnacipran from breast milk (assuming mean milk consumption of 150 mL/kg/day) was 5% of the maternal dose based on peak plasma concentrations.
8.4 Pediatric Use
Safety and effectiveness of milnacipran HCl in a fibromyalgia pediatric population below the age of 18 have not been established [see Boxed Warning, Indications and Usage (1), and Warnings and Precautions (5.1)]. The use of milnacipran HCl is not recommended in pediatric patients.
8.5 Geriatric Use
In controlled clinical studies of milnacipran HCl, 402 patients were 60 years or older, and no overall differences in safety and efficacy were observed between these patients and younger patients.
In view of the predominant excretion of unchanged milnacipran via kidneys and the expected decrease in renal function with age, renal function should be considered prior to use of milnacipran HCl in the elderly [see Dosage and Administration (2.2)].
SNRIs, SSRIs, and milnacipran HCl, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event [see Warnings and Precautions (5.8)].
- Pregnancy: Third trimester use may increase risk for symptoms of poor adaptation (respiratory distress, temperature instability, feeding difficulty, hypotonia, tremor, irritability) in the neonate. (8.1)
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Milnacipran is not a controlled substance.
9.2 Abuse
Milnacipran did not produce behavioral signs indicative of abuse potential in animal or human studies.
9.3 Dependence
Milnacipran produces physical dependence, as evidenced by the emergence of withdrawal symptoms following drug discontinuation, similar to other SNRIs and SSRIs. These withdrawal symptoms can be severe. Thus, taper milnacipran HCl and do not abruptly discontinue after extended use [see Warnings and Precautions (5.7)].
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The exact mechanism of the central pain inhibitory action of milnacipran and its ability to improve the symptoms of fibromyalgia in humans are unknown. Preclinical studies have shown that milnacipran is a potent inhibitor of neuronal norepinephrine and serotonin reuptake; milnacipran inhibits norepinephrine uptake with approximately 3-fold higher potency in vitro than serotonin without directly affecting the uptake of dopamine or other neurotransmitters. Milnacipran has no significant affinity for serotonergic (5-HT1-7), α- and β-adrenergic, muscarinic (M1-5), histamine (H1-4), dopamine (D1-5), opiate, benzodiazepine, and γ-aminobutyric acid (GABA) receptors in vitro. Pharmacologic activity at these receptors is hypothesized to be associated with the various anticholinergic, sedative, and cardiovascular effects seen with other psychotropic drugs.
Milnacipran has no significant affinity for Ca++, K+, Na+ and Cl– channels and does not inhibit the activity of human monoamine oxidases (MAO-A and MAO-B) or acetylcholinesterase.
12.2 Pharmacodynamics
Cardiac Electrophysiology
The effect of milnacipran HCl on the QTcF interval was measured in a double- blind placebo-and positive-controlled parallel study in 88 healthy subjects using 600 mg/day milnacipran HCl (3 to 6 times the recommended therapeutic dose for fibromyalgia). After baseline and placebo adjustment, the maximum mean QTcF change was 8 ms (2-sided 90% CI, 3 to 12 ms). This increase is not considered to be clinically significant.
12.3 Pharmacokinetics
Milnacipran is well absorbed after oral administration with an absolute bioavailability of approximately 85% to 90%. The exposure to milnacipran increased proportionally within the therapeutic dose range. It is excreted predominantly unchanged in urine (55%) and has a terminal elimination half- life of about 6 to 8 hours. Steady-state levels are reached within 36 to 48 hours and can be predicted from single-dose data. The active enantiomer, d-milnacipran, has a longer elimination half-life (8 to 10 hours) than the l-enantiomer (4 to 6 hours). There is no interconversion between the enantiomers.
Absorption
Milnacipran HCl is absorbed following oral administration with maximum concentrations (Cmax) reached within 2 to 4 hours post dose. Absorption of milnacipran HCl is not affected by food. The absolute bioavailability is approximately 85% to 90%.
Distribution
The mean volume of distribution of milnacipran following a single intravenous dose to healthy subjects is approximately 400 L.
Plasma protein binding is 13%.
Elimination
Metabolism
Milnacipran and its metabolites are eliminated primarily by renal excretion.
Excretion
Following oral administration of 14C-milnacipran hydrochloride, approximately 55% of the dose was excreted in urine as unchanged milnacipran (24% as l-milnacipran and 31% as d-milnacipran). The l-milnacipran carbamoyl-O- glucuronide was the major metabolite excreted in urine and accounted for approximately 17% of the dose; approximately 2% of the dose was excreted in urine as d-milnacipran carbamoyl-O-glucuronide. Approximately 8% of the dose was excreted in urine as the N-desethyl milnacipran metabolite.
Specific Populations
Geriatric Patients
Cmax and AUC parameters of milnacipran were about 30% higher in elderly (> 65 years) subjects compared with young subjects due to age-related decreases in renal function.
No dosage adjustment is necessary based on age unless renal function is severely impaired [see Dosage and Administration (2.2)].
Male and Female Patients
Cmax and AUC parameters of milnacipran were about 20% higher in female subjects compared with male subjects. Dosage adjustment based on gender is not necessary.
Patients with Renal Impairment
Milnacipran pharmacokinetics were evaluated following single oral administration of 50 mg milnacipran HCl to subjects with mild (creatinine clearance [CLcr] 50 to 80 mL/min), moderate (CLcr 30 to 49 mL/min), and severe (CLcr 5 to 29 mL/min) renal impairment and to healthy subjects (CLcr > 80 mL/min). The mean AUC0-∞ increased by 16%, 52%, and 199%, and terminal elimination half-life increased by 38%, 41%, and 122% in subjects with mild, moderate, and severe renal impairment, respectively, compared with healthy subjects.
No dosage adjustment is necessary for patients with mild renal impairment. Exercise caution in patients with moderate renal impairment. Dose adjustment is necessary in severe renal impairment patients [see Dosage and Administration (2.2)].
Patients with Hepatic Impairment
Milnacipran pharmacokinetics were evaluated following single oral administration of 50 mg milnacipran HCl to subjects with mild (Child-Pugh A), moderate (Child-Pugh B), and severe (Child-Pugh C) hepatic impairment and to healthy subjects. AUC0-∞ and T½ were similar in healthy subjects and subjects with mild and moderate hepatic impairment. However, subjects with severe hepatic impairment had a 31% higher AUC0-∞ and a 55% higher T½ than healthy subjects. Exercise caution in patients with severe hepatic impairment.
Drug Interaction Studies
In Vitro Studies
In general, milnacipran, at concentrations that were at least 25 times those attained in clinical trials, did not inhibit human CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4 or induce human CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP3A4/5 enzyme systems, indicating a low potential of interactions with drugs metabolized by these enzymes.
In vitro studies have shown that the biotransformation rate of milnacipran by human hepatic microsomes and hepatocytes was low. A low biotransformation was also observed following incubation of milnacipran with cDNA-expressed human CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4 isozymes.
In Vivo Studies
The drug interaction studies described in this section were conducted in healthy adult subjects.
Carbamazepine - There were no clinically significant changes in the pharmacokinetics of milnacipran following co-administration of milnacipran HCl (100 mg/day) and carbamazepine (200 mg twice a day). No changes were observed in the pharmacokinetics of carbamazepine or its epoxide metabolite due to co- administration with milnacipran HCl.
Clomipramine - Switching from clomipramine (75 mg once a day) to milnacipran (100 mg/day) without a washout period did not lead to clinically significant changes in the pharmacokinetics of milnacipran. Because an increase in adverse events (e.g., euphoria and postural hypotension) was observed after switching from clomipramine to milnacipran, monitoring of patients during treatment switch is recommended.
Digoxin - There was no pharmacokinetic interaction between milnacipran HCl (200 mg/day) and digoxin (0.2 mg/day Lanoxicaps) following multiple-dose administration to healthy subjects.
Fluoxetine - Switching from fluoxetine (20 mg once a day), a strong inhibitor of CYP2D6 and a moderate inhibitor of CYP2C19, to milnacipran (100 mg/day) without a washout period did not affect the pharmacokinetics of milnacipran.
Lithium - Multiple doses of milnacipran HCl (100 mg/day) did not affect the pharmacokinetics of lithium.
Lorazepam - There was no pharmacokinetic interaction between a single dose of milnacipran HCl (50 mg) and lorazepam (1.5 mg).
Pregabalin - There were no clinically significant changes in the steady-state pharmacokinetics of milnacipran or pregabalin following twice a day co- administration of 50 mg milnacipran and 150 mg pregabalin.
Warfarin - Steady-state milnacipran (200 mg/day) did not affect the pharmacokinetics of R-warfarin and S-warfarin or the pharmacodynamics (as assessed by measurement of prothrombin INR) of a single dose of 25 mg warfarin. The pharmacokinetics of milnacipran HCl were not altered by warfarin.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Dietary administration of milnacipran to rats at doses of 50 mg/kg/day (2 times the MRHD on a mg/m2 basis) for 2 years caused a statistically significant increase in the incidence of thyroid C-cell adenomas and combined adenomas and carcinomas in males. A carcinogenicity study was conducted in Tg.rasH2 mice for 6 months at oral gavage doses of up to 125 mg/kg/day.
Milnacipran did not induce tumors in Tg.rasH2 mice at any dose tested.
Mutagenesis
Milnacipran was not mutagenic in the in vitro bacterial reverse mutation assay (Ames test) or in the L5178Y TK +/-mouse lymphoma forward mutation assay. Milnacipran was also not clastogenic in an in vitro chromosomal aberration test in human lymphocytes or in the in vivo mouse micronucleus assay.
Impairment of Fertility
Although administration of milnacipran to male and female rats had no statistically significant effect on mating or fertility at doses up to 80 mg/kg/day (4 times the MRHD on an mg/m2 basis), there was an apparent dose- related decrease in the fertility index at clinically relevant doses based on body surface area.
13.2 Animal Toxicology and/or Pharmacology
Hepatic Effects
Chronic administration (2 years) of milnacipran to rats at 15 mg/kg (0.6 times the MRHD on an mg/m2 basis) and higher doses showed increased incidences of centrilobular vacuolation of the liver in male rats and eosinophilic foci in male and female rats in the absence of any change in hepatic enzymes. The clinical significance of the finding is not known. Chronic (1 year) administration in the primate at doses up to 25 mg/kg (2 times the MRHD on a mg/m2 basis) did not demonstrate similar evidence of hepatic changes.
Ocular Effects
Chronic (2 years) administration of milnacipran to rats at 15 mg/kg (0.6 times the MRHD on a mg/m2 basis) and higher doses showed increased incidence of keratitis of the eye. One-year studies in the rat and primate did not show this response.
