Finasteride
These highlights do not include all the information needed to use finasteride tablets USP safely and effectively. See full prescribing information for finasteride tablets USP. FINASTERIDE Tablets USP, 5 mg for oral use Initial U.S. Approval: 1992
cc9709ce-2d29-48bd-b46b-3f72114f2527
HUMAN PRESCRIPTION DRUG LABEL
Jul 28, 2017
Camber Pharmaceuticals, Inc.
DUNS: 826774775
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Finasteride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Drug Labeling Information
Clinical Pharmacology Section
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The development and enlargement of the prostate gland is dependent on the
potent androgen, 5α-dihydrotestosterone (DHT). Type II 5α-reductase
metabolizes testosterone to DHT in the prostate gland, liver and skin. DHT
induces androgenic effects by binding to androgen receptors in the cell nuclei
of these organs.
Finasteride is a competitive and specific inhibitor of Type II 5α-reductase
with which it slowly forms a stable enzyme complex. Turnover from this complex
is extremely slow (t½∼ 30 days). This has been demonstrated both in vivo and
in vitro. Finasteride has no affinity for the androgen receptor. In man, the
5α-reduced steroid metabolites in blood and urine are decreased after
administration of finasteride.
12.2 Pharmacodynamics
In man, a single 5-mg oral dose of finasteride tablets USP produces a rapid reduction in serum DHT concentration, with the maximum effect observed 8 hours after the first dose. The suppression of DHT is maintained throughout the 24-hour dosing interval and with continued treatment. Daily dosing of finasteride tablets USP at 5 mg/day for up to 4 years has been shown to reduce the serum DHT concentration by approximately 70%. The median circulating level of testosterone increased by approximately 10 to 20% but remained within the physiologic range. In a separate study in healthy men treated with finasteride 1 mg per day (n=82) or placebo (n=69), mean circulating levels of testosterone and estradiol were increased by approximately 15% as compared to baseline, but these remained within the physiologic range.
In patients receiving finasteride tablets USP, 5 mg/day, increases of about
10% were observed in luteinizing hormone (LH) and follicle-stimulating hormone
(FSH), but levels remained within the normal range. In healthy volunteers,
treatment with finasteride tablets USP did not alter the response of LH and
FSH to gonadotropin-releasing hormone indicating that the hypothalamic-
pituitary-testicular axis was not affected.
In patients with BPH, finasteride tablets USP has no effect on circulating
levels of cortisol, prolactin, thyroid-stimulating hormone, or thyroxine. No
clinically meaningful effect was observed on the plasma lipid profile (i.e.,
total cholesterol, low density lipoproteins, high density lipoproteins and
triglycerides) or bone mineral density.
Adult males with genetically inherited Type II 5α-reductase deficiency also have decreased levels of DHT. Except for the associated urogenital defects present at birth, no other clinical abnormalities related to Type II 5α-reductase deficiency have been observed in these individuals. These individuals have a small prostate gland throughout life and do not develop BPH.
In patients with BPH treated with finasteride (1 to 100 mg/day) for 7 to 10 days prior to prostatectomy, an approximate 80% lower DHT content was measured in prostatic tissue removed at surgery, compared to placebo; testosterone tissue concentration was increased up to 10 times over pretreatment levels, relative to placebo. Intraprostatic content of PSA was also decreased.
In healthy male volunteers treated with finasteride tablets USP for 14 days, discontinuation of therapy resulted in a return of DHT levels to pretreatment levels in approximately 2 weeks. In patients treated for three months, prostate volume, which declined by approximately 20%, returned to close to baseline value after approximately three months of discontinuation of therapy.
12.3 Pharmacokinetics
Absorption
In a study of 15 healthy young subjects, the mean bioavailability of
finasteride 5 mg tablets was 63% (range 34 to 108%), based on the ratio of
area under the curve (AUC) relative to an intravenous (IV) reference dose.
Maximum finasteride plasma concentration averaged 37 ng/mL (range, 27 to 49
ng/mL) and was reached 1 to 2 hours postdose. Bioavailability of finasteride
was not affected by food.
Distribution
Mean steady-state volume of distribution was 76 liters (range, 44 to 96
liters). Approximately 90% of circulating finasteride is bound to plasma
proteins. There is a slow accumulation phase for finasteride after multiple
dosing. After dosing with 5 mg/day of finasteride for 17 days, plasma
concentrations of finasteride were 47 and 54% higher than after the first dose
in men 45 to 60 years old (n=12) and ≥70 years old (n=12), respectively. Mean
trough concentrations after 17 days of dosing were 6.2 ng/mL (range, 2.4 to
9.8 ng/mL) and 8.1 ng/mL (range, 1.8 to 19.7 ng/mL), respectively, in the two
age groups. Although steady state was not reached in this study, mean trough
plasma concentration in another study in patients with BPH (mean age, 65
years) receiving 5 mg/day was 9.4 ng/mL (range, 7.1 to 13.3 ng/mL; n=22) after
over a year of dosing.
Finasteride has been shown to cross the blood brain barrier but does not appear to distribute preferentially to the CSF.
In 2 studies of healthy subjects (n=69) receiving finasteride tablets USP 5 mg/day for 6 to 24 weeks, finasteride concentrations in semen ranged from undetectable (<0.1 ng/mL) to 10.54 ng/mL. In an earlier study using a less sensitive assay, finasteride concentrations in the semen of 16 subjects receiving finasteride tablets USP, 5 mg/day ranged from undetectable (<1.0 ng/mL) to 21 ng/mL. Thus, based on a 5 mL ejaculate volume, the amount of finasteride in semen was estimated to be 50- to 100-fold less than the dose of finasteride (5 mcg) that had no effect on circulating DHT levels in men [see also Use in Specific Populations (8.1)].
Metabolism
Finasteride is extensively metabolized in the liver, primarily via the
cytochrome P450 3A4 enzyme subfamily. Two metabolites, the t-butyl side chain
monohydroxylated and monocarboxylic acid metabolites, have been identified
that possess no more than 20% of the 5α-reductase inhibitory activity of
finasteride.
Excretion
In healthy young subjects (n=15), mean plasma clearance of finasteride was 165
mL/min (range, 70 to 279 mL/min) and mean elimination half-life in plasma was
6 hours (range, 3 to 16 hours). Following an oral dose of 14C-finasteride in
man (n=6), a mean of 39% (range, 32 to 46%) of the dose was excreted in the
urine in the form of metabolites; 57% (range, 51 to 64%) was excreted in the
feces.
The mean terminal half-life of finasteride in subjects ≥70 years of age was approximately 8 hours (range, 6 to 15 hours; n=12), compared with 6 hours (range, 4 to 12 hours; n=12) in subjects 45 to 60 years of age. As a result, mean AUC(0 to 24 hr) after 17 days of dosing was 15% higher in subjects ≥70 years of age than in subjects 45 to 60 years of age (p=0.02).
|
Table 3 : Mean (SD) Pharmacokinetic Parameters in Healthy Young Subjects (n=15) | |
|
** Mean (± SD)** | |
|
Bioavailability |
63% (34-108%)* |
|
Clearance (mL/min) |
165 (55) |
|
Volume of Distribution (L) |
76 (14) |
|
Half-Life (hours) |
6.2 (2.1) |
- Range
Pediatric
Finasteride pharmacokinetics have not been investigated in patients <18 years
of age.
Finasteride is not indicated for use in pediatric patients [see Warnings and Precautions (5.4), Use in Specific Populations (8.4)].
Gender
Finasteride is not indicated for use in women [see Contraindications (4), Warnings and Precautions (5.3 and 5.4), Use in Specific Populations (8.1), How Supplied/Storage and Handling (16) and Patient Counseling Information (17.2)]
Geriatric
No dosage adjustment is necessary in the elderly. Although the elimination rate of finasteride is decreased in the elderly, these findings are of no clinical significance. [See Clinical Pharmacology (12.3) and Use in Specific Populations (8.5).]
|
Table 4 : Mean (SD) Noncompartmental Pharmacokinetic Parameters After Multiple Doses of 5 mg/day in Older Men | ||
|
Mean (± SD) | ||
|
45-60 years old (n=12) |
≥70 years old (n=12) | |
|
AUC (ng•hr/mL) |
389 (98) |
463 (186) |
|
Peak Concentration (ng/mL) |
46.2 (8.7) |
48.4 (14.7) |
|
Time to Peak (hours) |
1.8 (0.7) |
1.8 (0.6) |
|
Half-Life (hours)* |
6.0 (1.5) |
8.2 (2.5 ) |
*First-dose values; all other parameters are last-dose values
Race
The effect of race on finasteride pharmacokinetics has not been studied.
Hepatic Impairment
The effect of hepatic impairment on finasteride pharmacokinetics has not been
studied. Caution should be exercised in the administration of finasteride
tablets USP in those patients with liver function abnormalities, as
finasteride is metabolized extensively in the liver.
Renal Impairment
No dosage adjustment is necessary in patients with renal impairment. In
patients with chronic renal impairment, with creatinine clearances ranging
from 9.0 to 55 mL/min, AUC, maximum plasma concentration, half-life, and
protein binding after a single dose of 14C-finasteride were similar to values
obtained in healthy volunteers. Urinary excretion of metabolites was decreased
in patients with renal impairment. This decrease was associated with an
increase in fecal excretion of metabolites. Plasma concentrations of
metabolites were significantly higher in patients with renal impairment (based
on a 60% increase in total radioactivity AUC). However, finasteride has been
well tolerated in BPH patients with normal renal function receiving up to 80
mg/day for 12 weeks, where exposure of these patients to metabolites would
presumably be much greater.
Clinical Studies Section
14 CLINICAL STUDIES
14.1 Monotherapy
Finasteride tablets USP, 5 mg/day was initially evaluated in patients with symptoms of BPH and enlarged prostates by digital rectal examination in two 1-year, placebo-controlled, randomized, double-blind studies and their 5-year open extensions.
Finasteride tablets USP was further evaluated in a long-term efficacy and safety study, a double-blind, randomized, placebo-controlled, 4-year, multicenter study. 3040 patients between the ages of 45 and 78, with moderate to severe symptoms of BPH and an enlarged prostate upon digital rectal examination, were randomized into the study (1524 to finasteride, 1516 to placebo) and 3016 patients were evaluable for efficacy. 1883 patients completed the 4-year study (1000 in the finasteride group, 883 in the placebo group).
Effect on Symptom Score
Symptoms were quantified using a score similar to the American Urological Association Symptom Score, which evaluated both obstructive symptoms (impairment of size and force of stream, sensation of incomplete bladder emptying, delayed or interrupted urination) and irritative symptoms (nocturia, daytime frequency, need to strain or push the flow of urine) by rating on a 0 to 5 scale for six symptoms and a 0 to 4 scale for one symptom, for a total possible score of 34.
Patients in a long-term efficacy and safety study had moderate to severe symptoms at baseline (mean of approximately 15 points on a 0 to 34 point scale). Patients randomized to finasteride tablets USP who remained on therapy for 4 years had a mean (± 1 SD) decrease in symptom score of 3.3 (± 5.8) points compared with 1.3 (± 5.6) points in the placebo group. (See Figure 1.) A statistically significant improvement in symptom score was evident at 1 year in patients treated with finasteride tablets USP vs placebo (–2.3 vs –1.6), and this improvement continued through Year 4.
** Figure 1**
** Symptom Score in A Long-Term Efficacy and Safety Study**
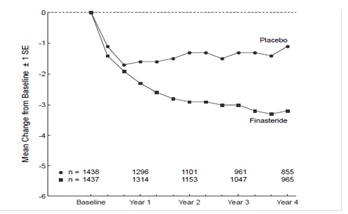
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Although an early improvement in urinary symptoms was seen in some patients, a therapeutic trial of at least 6 months was generally necessary to assess whether a beneficial response in symptom relief had been achieved. The improvement in BPH symptoms was seen during the first year and maintained throughout an additional 5 years of open extension studies.
Effect on the Need for Surgery
In a long-term efficacy and safety study, efficacy was also assessed by
evaluating treatment failures. Treatment failure was prospectively defined as
BPH-related urological events or clinical deterioration, lack of improvement
and/or the need for alternative therapy. BPH-related urological events were
defined as urological surgical intervention . Complete event information was
available for 92% of the patients. The following table summarizes the results.
|
Table 5: All Treatment Failures in A Long-Term Efficacy and Safety Study | |||||
|
Patients (%)* | |||||
|
Event |
Placebo |
Finasteride |
Relative Risk† |
95% CI |
P Value† |
|
All Treatment Failures |
37.1 |
26.2 |
0.68 |
(0.57 to 0.79) |
<0.001 |
|
Surgical Interventions for BPH |
10.1 |
4.6 |
0.45 |
(0.32 to 0.63) |
<0.001 |
|
Two consecutive symptom score ≥ 20 |
9.2 |
6.7 | |||
|
Bladder Stone |
0.4 |
0.5 | |||
|
Incontinence |
2.1 |
1.7 | |||
|
Renal Failure |
0.5 |
0.6 | |||
|
UTI |
5.7 |
4.9 | |||
|
Discontinuation due to worsening of BPH, |
21.8 |
13.3 |
*patients with multiple events may be counted more than once for each type of event
† Hazard ratio based on log rank test
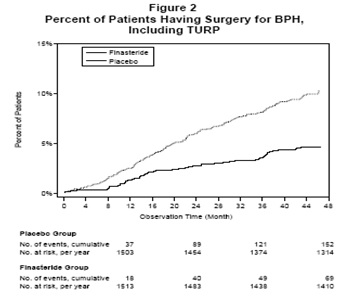
Compared with placebo, finasteride tablets USP was associated with a significantly lower need for BPH-related surgery. Compared with placebo, finasteride tablets USP was associated with a significantly lower risk for surgery [10.1% for placebo vs 4.6% for finasteride tablets USP; 55% reduction in risk, 95% CI: (37 to 68%)]; see Figure 2.
** Effect on Maximum Urinary Flow Rate**
In the patients in a long-term efficacy and safety study who remained on
therapy for the duration of the study and had evaluable urinary flow data,
finasteride tablets USP increased maximum urinary flow rate by 1.9 mL/sec
compared with 0.2 mL/sec in the placebo group.
There was a clear difference between treatment groups in maximum urinary flow
rate in favor of finasteride tablets USP by month 4 (1.0 vs 0.3 mL/sec) which
was maintained throughout the study. In the earlier 1-year studies, increase
in maximum urinary flow rate was comparable to a long-term efficacy and safety
study and was maintained through the first year and throughout an additional 5
years of open extension studies.
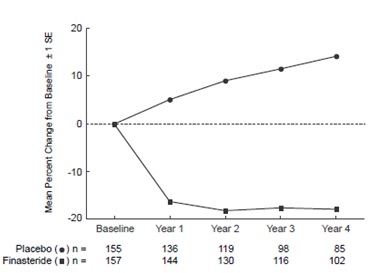
Effect on Prostate Volume
In a long-term efficacy and safety study, prostate volume was assessed yearly
by magnetic resonance imaging (MRI) in a subset of patients. In patients
treated with finasteride tablets USP who remained on therapy, prostate volume
was reduced compared with both baseline and placebo throughout the 4-year
study. Finasteride tablets USP decreased prostate volume by 17.9% (from 55.9
mL at baseline to 45.8 mL at 4 years) compared with an increase of 14.1% (from
51.3 mL to 58.5 mL) in the placebo group (p<0.001). (See Figure 3.)
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Mean prostate volume at baseline ranged between 40 to 50 ml. The reduction in prostate volume was seen during the first year and maintained throughout an additional five years of open extension studies.
** Figure 3**
Prostate Volume in A Long-Term Efficacy and Safety Study
Prostate Volume as a Predictor of Therapeutic Response
A meta-analysis combining 1-year data from seven double-blind, placebo-
controlled studies of similar design, including 4491 patients with symptomatic
BPH, demonstrated that, in patients treated with finasteride tablets USP, the
magnitude of symptom response and degree of improvement in maximum urinary
flow rate were greater in patients with an enlarged prostate at baseline.
14.2 Combination with Alpha-Blocker Therapy
The Medical Therapy of Prostatic Symptoms (MTOPS) Trial was a double-blind, randomized, placebo-controlled, multicenter, 4- to 6-year study (average 5 years) in 3047 men with symptomatic BPH, who were randomized to receive finasteride tablets USP, 5 mg/day (n=768), doxazosin 4 or 8 mg/day (n=756), the combination of finasteride tablets USP, 5 mg/day and doxazosin 4 or 8 mg/day (n=786), or placebo (n=737). All participants underwent weekly titration of doxazosin (or its placebo) from 1 to 2 to 4 to 8 mg/day. Only those who tolerated the 4 or 8 mg dose level were kept on doxazosin (or its placebo) in the study. The participant’s final tolerated dose (either 4 mg or 8 mg) was administered beginning at end-Week 4. The final doxazosin dose was administered once per day, at bedtime.
The mean patient age at randomization was 62.6 years (±7.3 years). Patients were Caucasian (82%), African American (9%), Hispanic (7%), Asian (1%) or Native American (<1%). The mean duration of BPH symptoms was 4.7 years (±4.6 years). Patients had moderate to severe BPH symptoms at baseline with a mean AUA symptom score of approximately 17 out of 35 points. Mean maximum urinary flow rate was 10.5 mL/sec (±2.6 mL/sec). The mean prostate volume as measured by transrectal ultrasound was 36.3 mL (±20.1 mL). Prostate volume was ≤20 mL in 16% of patients, ≥50 mL in 18% of patients and between 21 and 49 mL in 66% of patients.
The primary endpoint was a composite measure of the first occurrence of any of
the following five outcomes: a ≥4 point confirmed increase from baseline in
symptom score, BPH-related renal insufficiency (creatinine rise), recurrent
urinary tract infections or urosepsis, or incontinence. Compared to placebo,
treatment with finasteride tablets USP, doxazosin, or combination therapy
resulted in a reduction in the risk of experiencing one of these five outcome
events by 34% (p=0.002), 39% (p<0.001), and 67% (p<0.001), respectively.
Combination therapy resulted in a significant reduction in the risk of the
primary endpoint compared to treatment with finasteride tablets USP alone
(49%; p≤0.001) or doxazosin alone (46%; p≤0.001). (See Table 6.)
Table 6: Count and Percent Incidence of Primary Outcome Events by Treatment
Group in MTOPS
|
Treatment Group | |||||
|
Placebo |
Doxazosin N=756 |
Finasteride N=768 |
Combination N=786 |
Total | |
|
Event |
N (%) |
N (%) |
N (%) |
N (%) |
N (%) |
|
AUA 4-point rise |
100 (13.6) |
59 (7.8) |
74 (9.6) |
41 (5.2) |
274 (9.0) |
|
Incontinence |
8 (1.1) |
11 (1.5) |
9 (1.2) |
3 (0.4) |
31 (1.0) |
|
Recurrent UTI/urosepsis |
2 (0.3) |
2 (0.3) |
0 (0.0) |
1 (0.1) |
5 (0.2) |
|
Creatinine rise |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
|
Total Events |
128 (17.4) |
85 (11.2) |
89 (11.6) |
49 (6.2) |
351 (11.5) |
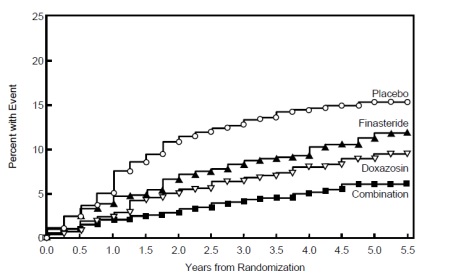
The majority of the events (274 out of 351; 78%) was a confirmed ≥4 point increase in symptom score, referred to as symptom score progression. The risk of symptom score progression was reduced by 30% (p=0.016), 46% (p<0.001), and 64% (p<0.001) in patients treated with finasteride tablets USP, doxazosin, or the combination, respectively, compared to patients treated with placebo (see Figure 4). Combination therapy significantly reduced the risk of symptom score progression compared to the effect of finasteride tablets USP alone (p<0.001) and compared to doxazosin alone (p=0.037).
Figure 4
Cumulative Incidence of a 4-Point Rise in AUA Symptom Score by Treatment Group
Treatment with finasteride tablets USP, doxazosin or the combination of finasteride tablets USP with doxazosin, reduced the mean symptom score from baseline at year 4. Table 7 provides the mean change from baseline for AUA symptom score by treatment group for patients who remained on therapy for four years.
Table 7:Change From Baseline in AUA Symptom Score by Treatment
** Group at Year 4 in MTOPS**
|
** Placebo** |
Doxazosin |
Finasteride |
Combination | |
|
Baseline Mean (SD) |
16.8 (6.0) |
17.0 (5.9) |
17.1 (6.0) |
16.8 (5.8) |
|
Mean Change AUA Symptom Score (SD) |
-4.9 (5.8) |
-6.6 (6.1) |
-5.6 (5.9) |
-7.4 (6.3) |
|
Comparison to Placebo (95% CI) |
-1.8 |
-0.7 |
-2.5 | |
|
Comparison to Doxazosin alone (95% CI) |
-0.7 | |||
|
Comparison to Finasteride alone (95% CI) |
-1.8 |
The results of MTOPS are consistent with the findings of the 4-year, placebo- controlled study a long-term efficacy and safety study [see Clinical Studies (14.1)] in that treatment with finasteride tablets USP reduces the need for BPH-related surgery. Also, the risk of requiring BPH-related invasive therapy was reduced by 64% in patients treated with finasteride tablets USP compared to patients treated with placebo (2.0% for finasteride tablets USP and 5.4% for placebo).
14.3 Summary of Clinical Studies
The data from these studies, showing improvement in BPH-related symptoms, reduction in treatment failure (BPH-related urological events), increased maximum urinary flow rates, and decreasing prostate volume, suggest that finasteride tablets USP arrests the disease process of BPH in men with an enlarged prostate.
