Fluocinolone Acetonide
These highlights do not include all the information needed to use FLUOCINOLONE ACETONIDE TOPICAL OIL safely and effectively. See full prescribing information for FLUOCINOLONE ACETONIDE TOPICAL OIL. FLUOCINOLONE ACETONIDE topical oil (scalp oil) Initial U.S. Approval: 1988
f4a58ecc-cd50-4414-add1-a82b09da2058
HUMAN PRESCRIPTION DRUG LABEL
Sep 19, 2025
RISING PHARMA HOLDINGS, INC.
DUNS: 116880195
Rising Pharmaceuticals, Inc.
DUNS: 041241766
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Fluocinolone Acetonide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
Rising®
PHARMACEUTICALS
NDC 64980-330-04
Fluocinolone
Acetonide
Topical Oil,
0.01%
(SCALP OIL)
FOR TOPICAL USE ONLY
NOT FOR ORAL,
OPHTHALMIC,
or INTRAVAGINAL USE
SHAKE WELL BEFORE USE
Net Contents
118.28 mL
(4 fl. oz.) Rx only


INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Fluocinolone acetonide topical oil, 0.01% is indicated for the treatment of psoriasis of the scalp in adults.
Fluocinolone acetonide topical oil, 0.01% is a corticosteroid indicated for the treatment of psoriasis of the scalp in adults. (1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
None.
None. (4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Endocrine System Adverse Reactions
Systemic absorption of topical corticosteroids can produce reversible
hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for
glucocorticosteroid insufficiency. Cushing's syndrome, hyperglycemia, and
glucosuria can result from systemic absorption of topical corticosteroids.
HPA axis suppression and Cushing's syndrome have been reported in patients
receiving topical corticosteroids.
Conditions which increase systemic absorption include the use of more potent
corticosteroids, use over large surface areas, use over prolonged periods, use
of occlusive dressings, altered skin barrier, liver failure, and young age.
Use of more than one corticosteroid-containing product at the same time may
increase total systemic corticosteroid exposure. Because of the potential for
systemic absorption, use of topical corticosteroids may require that patients
be periodically evaluated for HPA axis suppression. The ACTH stimulation test
may be helpful in evaluating patients for HPA axis suppression.
If HPA axis suppression is documented, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent corticosteroid. Manifestations of adrenal insufficiency may require supplemental systemic corticosteroids. Recovery of HPA axis function is generally prompt upon discontinuation of topical corticosteroids.
5.2 Local Adverse Reactions
Local adverse reactions may occur with use of topical corticosteroids, including fluocinolone acetonide topical oil, 0.01%, and may be more likely to occur with occlusive use, prolonged use or use of higher potency corticosteroids. Some local adverse reactions may be irreversible. Reactions may include atrophy, striae, telangiectasias, burning, itching, irritation, dryness, folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, and miliaria [see Adverse Reactions (6.1)].
5.3 Ophthalmic Adverse Reactions
Use of topical corticosteroids may increase the risks of glaucoma and posterior subcapsular cataract. Glaucoma and cataracts have been reported in postmarketing experience with the use of topical corticosteroid products. Avoid contact of fluocinolone acetonide topical oil, 0.01% with eyes. Advise patients to report any visual symptoms and consider referral to an ophthalmologist for evaluation.
5.4 Allergic Contact Dermatitis
Use of topical corticosteroids can cause allergic contact dermatitis. Allergic contact dermatitis to any component of topical corticosteroids is usually diagnosed by a failure to heal rather than a clinical exacerbation. Clinical diagnosis of allergic contact dermatitis can be confirmed by patch testing.
5.5 Concomitant Skin Infections
Use of topical corticosteroids may delay healing or worsen concomitant skin infections. Treat concomitant skin infections with an appropriate antimicrobial agent. If the infection persists unchanged, discontinue fluocinolone acetonide topical oil, 0.01% until the infection has been adequately treated.
5.6 Use in Peanut-Sensitive Individuals
Use caution in prescribing fluocinolone acetonide topical oil, 0.01% for
peanut-sensitive individuals [see Description (11)].
Should signs of hypersensitivity present (wheal and flare reactions, pruritus,
or other manifestations), or should disease exacerbations occur, discontinue
fluocinolone acetonide topical oil, 0.01% immediately and institute
appropriate therapy.
- Endocrine System Adverse Reactions:
o Topical corticosteroids can produce reversible HPA axis suppression,
Cushing's syndrome, hyperglycemia, and glucosuria. (5.1)
o Systemic absorption may require evaluation for hypothalamic-pituitary-
adrenal (HPA) axis suppression. Potent corticosteroids use on large areas,
prolonged use or occlusive use, altered skin barrier, liver failure, and young
age may increase systemic absorption. Modify use should HPA axis suppression
develop. (5.1)
- Local Adverse Reactions: Local adverse reactions may include atrophy, striae irritation, acneiform eruptions, hypopigmentation, and allergic contact dermatitis, and may be more likely with occlusive use or more potent corticosteroids. (5.2, 6.1)
- Ophthalmic Adverse Reactions: May increase the risks of glaucoma and posterior subcapsular cataract. Avoid contact of fluocinolone acetonide topical oil, 0.01% with eyes. Advise patients to report any visual symptoms and consider referral to an ophthalmologist for evaluation. (5.3)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in more detail in other
sections of the labeling:
• Endocrine System Adverse Reactions [see Warnings and Precautions (5.1)]
• Local Adverse Reactions [see Warnings and Precautions (5.2)]
• Ophthalmic Adverse Reactions [see Warnings and Precautions (5.3)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying condition, adverse
reaction rates observed in the clinical trials of a drug cannot be directly
compared to rates in the clinical trials of another drug and may not reflect
the rates observed in practice.
An open-label safety study was conducted in 29 pediatric subjects 3 months to
2 years old to assess the HPA axis by ACTH stimulation testing following use
of the formulation of fluocinolone acetonide topical oil, 0.01% twice daily
for 4 weeks. Fluocinolone acetonide topical oil, 0.01% is not approved for use
in pediatric patients for the treatment of psoriasis of the scalp. The most
common adverse reactions were reported in the study:
|
Adverse Reaction |
n (%) |
|
Cough |
6 (20) |
|
Rhinorrhea |
4 (13) |
|
Pyrexia |
3 (10) |
|
Nasopharyngitis |
2 (7) |
|
Hypopigmentation |
2 (7) |
|
Abscess |
1 (3) |
|
Atopic Dermatitis |
1 (3) |
|
Eczema |
1 (3) |
|
Hyperpigmentation |
1 (3) |
|
Molluscum |
1 (3) |
|
Rash |
1 (3) |
|
Diarrhea |
1 (3) |
|
Otitis Media |
1 (3) |
|
URI |
1 (3) |
|
Vomiting |
1 (3) |
- Includes one subject who withdrew at Week 2
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of products containing topical corticosteroids. Because postmarketing adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Endocrine Disorders: HPA axis suppression and Cushing’s syndrome
- Eye Disorders: glaucoma and cataracts
- Nervous System Disorders: intracranial hypertension including bulging fontanelles, headaches, and bilateral papilledema
The most common adverse reactions in pediatric subjects treated for atopic dermatitis (≥5%) were cough (20%), rhinorrhea (13%), pyrexia (10%), telangiectasia (7%), nasopharyngitis (7%), and hypopigmentation (7%). (6.1, 6.2)
To report SUSPECTED ADVERSE REACTIONS, contact Rising Pharma Holdings, Inc. at 1-844-874-7464 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
In a vehicle-controlled study for the treatment of psoriasis of the scalp in adults, after 21 days of treatment, 60% of patients on active treatment and 21% of patients on the drug vehicle had excellent to cleared clinical response.
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
Fluocinolone acetonide topical oil, 0.01% is for topical use only. Not for
oral, ophthalmic, or intravaginal use.
Wet or dampen hair and scalp thoroughly. Apply a thin film of fluocinolone
acetonide topical oil, 0.01% on the scalp, massage well and cover scalp with
the supplied shower cap. Leave on overnight or for a minimum of 4 hours then
wash hair with regular shampoo and rinse thoroughly. Use daily as needed.
Discontinue fluocinolone acetonide topical oil, 0.01% when control of disease
is achieved within 2 weeks, or contact the healthcare provider if no
improvement is seen within 2 weeks.
Do not use fluocinolone acetonide topical oil, 0.01% on the face unless
directed by the healthcare provider. Do not apply to intertriginous areas due
to the increased risk of local adverse reactions [see Adverse Reactions (6)].
Do not apply to the diaper area; diapers or plastic pants may constitute
occlusive use. [see Warnings and Precautions (5.1)]
- Fluocinolone acetonide topical oil, 0.01% is not for oral, ophthalmic, or intravaginal use. (2)
- Do not use on face or intertriginous areas. (2)
- Apply a thin film of fluocinolone acetonide topical oil, 0.01% on the wet scalp, massage well and cover scalp with the supplied shower cap. Leave on overnight or for a minimum of 4 hours before washing off. (2)
DESCRIPTION SECTION
11 DESCRIPTION
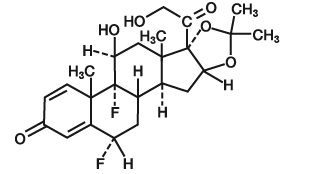
Fluocinolone Acetonide Topical Oil, 0.01% (Scalp Oil) contains fluocinolone acetonide [(6α, 11β, 16α)-6,9-difluoro-11,21-dihydroxy-16,17[(1– methylethylidene) bis(oxy)]-pregna-1,4-diene-3,20-dione, cyclic 16,17 acetal with acetone], a synthetic corticosteroid for topical dermatologic use. Chemically, fluocinolone acetonide is C24H30F2O6. It has the following structural formula:
Fluocinolone acetonide has a molecular weight of 452.50. It is a white crystalline powder that is odorless, stable in light, and melts at 270°C with decomposition; soluble in alcohol, acetone and methanol; slightly soluble in chloroform; insoluble in water.
Each gram of fluocinolone acetonide topical oil, 0.01% contains approximately
0.11 mg of fluocinolone acetonide in a blend of oils, which contains isopropyl
alcohol, isopropyl myristate, light mineral oil, oleth-2 and refined peanut
oil.
Each packaged product contains 2 shower caps. The shower cap is made of low
density polyethylene material with rubber elastic.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action in psoriasis of the scalp is unknown.
12.2 Pharmacodynamics
Vasoconstrictor Assay
Fluocinolone acetonide topical oil, 0.01% is in the low to medium range of
potency as compared with other topical corticosteroids in vasoconstrictor
studies. However, similar blanching scores do not necessarily imply
therapeutic equivalence.
Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression
HPA axis suppression following administration of fluocinolone acetonide
topical oil, 0.01% was not assessed.
12.3 Pharmacokinetics
Topical corticosteroids can be absorbed from intact healthy skin. The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the product formulation and the integrity of the epidermal barrier. Occlusion, inflammation and/or other disease processes in the skin may increase percutaneous absorption. The use of pharmacodynamic endpoints for assessing the systemic exposure of topical corticosteroids may be necessary due to the fact that circulating levels are often below the level of detection. Once absorbed through the skin, topical corticosteroids are metabolized, primarily in the liver, and are then excreted by the kidneys. Some corticosteroids and their metabolites are also excreted in the bile.
HOW SUPPLIED SECTION
16 HOW SUPPLIED / STORAGE AND HANDLING
Fluocinolone Acetonide Topical Oil, 0.01% (Scalp Oil) (NDC # 64980-330-04) is
supplied in bottles containing 4 fluid ounces and with 2 shower caps.
Storage: Keep tightly closed. Store at 20°-25°C (68°-77°F); excursions
permitted to 15°- 30°C (59°-86°F) [see USP Controlled Room Temperature].
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Fluocinolone acetonide topical oil, 0.01% is a topical oil containing 0.01% fluocinolone acetonide, supplied in bottles containing 4 fluid ounces and with 2 shower caps.
Fluocinolone acetonide topical oil, 0.01% is a topical oil containing 0.01% fluocinolone acetonide, supplied in bottles containing 4 fluid ounces and with 2 shower caps. (3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from case reports, case series, and observational studies on
fluocinolone acetonide use in pregnant women have not identified a drug-
associated risk of major birth defects, miscarriage or adverse maternal or
fetal outcomes. Observational studies suggest maternal use of high to super-
high potency topical steroids may be associated with an increased risk of low
birthweight infants. Advise pregnant women to use fluocinolone acetonide
topical oil, 0.01% on the smallest area of skin and for the shortest duration
possible.
Corticosteroids can cause fetal malformations in laboratory animals when
administered systemically at relatively low dosage levels. Some
corticosteroids cause fetal malformations after dermal application in
laboratory animals.
The background risk of major birth defects and miscarriage for the indicated
population is unknown. All pregnancies have a background risk of birth defect,
loss, or other adverse outcomes. In the U.S. general population, the estimated
background risk of major birth defects and miscarriage in clinically
recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of fluocinolone acetonide in
breast milk or its effects on the breastfed infant or on milk production. It
is not known whether topical administration of corticosteroids could result in
sufficient systemic absorption to produce detectable quantities in breast
milk. To minimize potential exposure to the breastfed infant via breast milk,
use fluocinolone acetonide topical oil, 0.01% on the smallest area of skin and
for the shortest duration possible while breastfeeding. Advise breastfeeding
women not to apply fluocinolone acetonide topical oil, 0.01% directly to the
nipple and areola to avoid direct infant exposure [see Warnings and Precautions (5.1)]. The developmental and health benefits of breastfeeding
should be considered along with the mother's clinical need for fluocinolone
acetonide topical oil, 0.01% and any potential adverse effects on the
breastfed infant from fluocinolone acetonide topical oil, 0.01% or from the
underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of fluocinolone acetonide topical oil, 0.01% have
not been established in pediatric patients with psoriasis of the scalp.
Evaluation in Peanut-Sensitive Pediatric Patients
A clinical trial was conducted to assess the safety of the formulation of
fluocinolone acetonide topical oil, 0.01%, which contains refined peanut oil,
in patients with known peanut allergies. The trial enrolled 13 pediatric
subjects with atopic dermatitis, 6 to 17 years of age. Fluocinolone acetonide
topical oil, 0.01% is not approved for the treatment of atopic dermatitis. Of
the 13 subjects, 9 were Radioallergosorbent Test (RAST) positive to peanuts
and 4 had no peanut sensitivity (controls). The trial evaluated the subjects’
responses to both prick test and patch test utilizing refined peanut oil, the
formulation of fluocinolone acetonide topical oil, 0.01% and histamine/saline
controls. Subjects were also treated with the formulation of fluocinolone
acetonide topical oil, 0.01% twice daily for 7 days. Prick test and patch test
results for all 13 subjects were negative to the formulation of fluocinolone
acetonide topical oil, 0.01% and the refined peanut oil. One of the 9 peanut-
sensitive subjects experienced an exacerbation of atopic dermatitis after 5
days of use on the formulation of fluocinolone acetonide topical oil, 0.01%.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, mutagenesis, impairment of fertility
No carcinogenicity, genotoxicity, or fertility studies were conducted with fluocinolone acetonide topical oil, 0.01%. However, some corticosteroids are genotoxic in various genotoxicity tests (i.e., the in vitro human peripheral blood lymphocyte chromosome aberration assay with metabolic activation, the in vivo mouse bone marrow micronucleus assay, the Chinese hamster micronucleus test, and the in vitro mouse lymphoma gene mutation assay).
PATIENT COUNSELING INFORMATION
17 PATIENT COUNSELING INFORMATION
Administration Instructions
Advise patients that fluocinolone acetonide topical oil, 0.01% is for topical
use only [see Dosage and Administration (2)].
Instruct patients not to apply fluocinolone acetonide topical oil, 0.01% to
the diaper area as diapers or plastic pants may constitute occlusive use [see Dosage and Administration (2)].
Advise patients to avoid use of fluocinolone acetonide topical oil, 0.01% on
the face, axillae, or groin unless directed by their healthcare provider [see Dosage and Administration (2)].
Advise patients to discontinue therapy when control of disease is achieved.
Instruct patients to contact their healthcare provider if no improvement is
seen within 2 weeks [see Dosage and Administration (2)].
Endocrine System Adverse Reactions
Instruct patients not to use other corticosteroid-containing products while
using Fluocinolone acetonide topical oil, 0.01% without first consulting their
healthcare provider [see Warnings and Precautions (5.1)].
Ophthalmic Adverse Reactions
Advise patients to avoid contact with the eyes and in case of contact, wash
eyes liberally with water. Instruct patients to tell their healthcare provider
if they develop any visual symptoms [see Warnings and Precautions (5.3)].
Pregnancy and Lactation
Advise women to use fluocinolone acetonide topical oil, 0.01% on the smallest
area of skin and for the shortest duration possible while pregnant or
breastfeeding. Advise patients that are breastfeeding not to apply
fluocinolone acetonide topical oil, 0.01% directly to the nipple and areola to
avoid direct infant exposure [See Use in Specific Populations (8.1 and 8.2)].
Manufactured by:
Lyne Laboratories, Inc.
Brockton, MA 02301
Manufactured for:
Rising Pharma Holdings, Inc.
East Brunswick, NJ 08816
Revised: 09/2025
PIR33004-02
