Tudorza Pressair
These highlights do not include all the information needed to use TUDORZA PRESSAIR safely and effectively. See full prescribing information for TUDORZA PRESSAIR. TUDORZA PRESSAIR (aclidinium bromide inhalation powder)FOR ORAL INHALATION ONLYInitial U.S. Approval: 2012
acdd5932-375b-4966-8a06-3806ab74c36d
HUMAN PRESCRIPTION DRUG LABEL
Feb 23, 2021
AstraZeneca Pharmaceuticals LP
DUNS: 054743190
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
aclidinium bromide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
Drug Labeling Information
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Not for Acute Use
TUDORZA PRESSAIR is intended as a twice-daily maintenance treatment for COPD and is not indicated for the initial treatment of acute episodes of bronchospasm (i.e., rescue therapy).
5.2 Paradoxical Bronchospasm
Inhaled medicines, including TUDORZA PRESSAIR, may cause paradoxical bronchospasm. If this occurs, treatment with TUDORZA PRESSAIR should be stopped and other treatments considered.
5.3 Worsening of Narrow-Angle Glaucoma
TUDORZA PRESSAIR should be used with caution in patients with narrow-angle glaucoma. Prescribers and patients should be alert for signs and symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos, or colored images in association with red eyes from conjunctival congestion and corneal edema). Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
5.4 Worsening of Urinary Retention
TUDORZA PRESSAIR should be used with caution in patients with urinary retention. Prescribers and patients should be alert for signs and symptoms of prostatic hyperplasia or bladder-neck obstruction (e.g., difficulty passing urine, painful urination). Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
5.5 Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions, including anaphylaxis, angioedema (including swelling of the lips, tongue, or throat), urticaria, rash, bronchospasm, or itching, have occurred after administration of TUDORZA PRESSAIR. If such a reaction occurs, therapy with TUDORZA PRESSAIR should be stopped at once and alternative treatments should be considered.
•
Not for acute use: Not for use as a rescue medication. (5.1)
•
Paradoxical bronchospasm: Discontinue TUDORZA PRESSAIR and consider other treatments if paradoxical bronchospasm occurs. (5.2)
•
Worsening of narrow-angle glaucoma may occur. Use with caution in patients with narrow-angle glaucoma and instruct patients to consult a physician immediately if this occurs. (5.3)
•
Worsening of urinary retention may occur. Use with caution in patients with prostatic hyperplasia or bladder-neck obstruction and instruct patients to consult a physician immediately if this occurs. (5.4)
•
Immediate hypersensitivity reactions: Discontinue TUDORZA PRESSAIR at once and consider alternatives if immediate hypersensitivity reactions, including angioedema, bronchospasm, or anaphylaxis occur. (5.5)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
In vitro studies suggest limited potential for CYP450-related metabolic drug interactions, thus no formal drug interaction studies have been performed with TUDORZA PRESSAIR [see Clinical Pharmacology (12.3)].
7.1 Sympathomimetics, Methylxanthines, Steroids
In clinical studies, concurrent administration of aclidinium bromide and other drugs commonly used in the treatment of COPD including sympathomimetics (short-acting beta2 agonists), methylxanthines, and oral and inhaled steroids showed no increases in adverse drug reactions.
7.2 Anticholinergics
There is a potential for an additive interaction with concomitantly used anticholinergic medications. Therefore, avoid coadministration of TUDORZA PRESSAIR with other anticholinergic-containing drugs as this may lead to an increase in anticholinergic effects.
Anticholinergics: May interact additively with concomitantly used anticholinergic medications. Avoid administrations of TUDORZA PRESSAIR with other anticholinergic-containing drugs. (7.2)
OVERDOSAGE SECTION
10 OVERDOSAGE
10.1 Human Experience
No case of overdose has been reported in clinical studies with TUDORZA PRESSAIR. There were no systemic anticholinergic or other adverse effects following a single inhaled dose of up to 6,000 mcg aclidinium bromide (7.5 times the RHDD) in 16 healthy volunteers.
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate and well controlled studies of TUDORZA PRESSAIR in pregnant women to inform drug associated risks.
No adverse developmental effects were seen with inhalation administration of aclidinium bromide to pregnant rats and rabbits during organogenesis at 15 or 20 times, respectively, the maximum recommended human daily inhaled dose (MRHDID). However, reduced pup weights were seen when pregnant rats continued inhalation administration through lactation at 5 times the MRHDID of aclidinium bromide. Adverse developmental effects occurred when rabbits were orally dosed with aclidinium bromide at approximately 1,400 times the MRHDID [see Data].
The estimated background risk of major birth defects and miscarriage of the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation days 6-17, no evidence of structural alterations was observed at approximately 15 times the MRHDID [based on summed AUCs of aclidinium bromide and its metabolites at inhaled doses less than or equal to 5.0 mg/kg/day]. However, in a pre- and post-natal development study, decreased pup weights were observed when pregnant rats were exposed from gestation day 6 and continuing during the lactation period at approximately 5 times the MRHDID [based on summed AUCs of aclidinium bromide and its metabolites at inhaled doses greater than or equal to 0.2 mg/kg/day]. Maternal toxicity was also observed at inhaled doses greater than or equal to 0.2 mg/kg/day.
In an embryo-fetal development study in pregnant Himalayan rabbits administered inhaled doses of aclidinium bromide during the period of organogenesis from gestation days 6-19, no evidence of structural alterations was observed at approximately 20 times the MRHDID [based on summed AUCs of aclidinium bromide and its metabolites at inhaled doses less than or equal to 3.6 mg/kg/day]. However, in another embryo-fetal development study in pregnant Himalayan rabbits dosed orally from gestation days 6-19, increased incidences of additional liver lobes (3-5%), as compared to 0% in the control group, were observed at approximately 1,400 times the MRHDID [based on summed AUCs of aclidinium bromide and its metabolites at oral doses greater than or equal to 150 mg/kg/day], and decreased fetal body weights were observed at approximately 2,300 times the MRHDID [based on summed AUCs of aclidinium bromide and its metabolites at oral doses greater than or equal to 300 mg/kg/day]. These fetal findings were observed in the presence of maternal toxicity.
8.2 Lactation
Risk Summary
There are no available data on the effects of TUDORZA PRESSAIR or aclidinium bromide on the breastfed child or on milk production or presence in human milk. Aclidinium bromide is present in milk of lactating female rats [see Data]. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for TUDORZA PRESSAIR and any potential adverse effects on the breastfed child from TUDORZA PRESSAIR or from the underlying maternal condition.
Data
In a pharmacokinetic study, levels of radioactivity in milk and plasma in rats were measured after a single intravenous dose of 1 mg/kg of radiolabeled aclidinium bromide on approximately post-natal day 14 [see Use in Specific Populations (8.1)]. The maximum concentration of radioactivity [14C-aclidinium] in milk was measured at 6 hours post-dose and was found to be 10-14 times higher than in plasma.
8.4 Pediatric Use
TUDORZA PRESSAIR is approved for use in the maintenance treatment of bronchospasm associated with COPD. COPD does not normally occur in children. The safety and effectiveness of TUDORZA PRESSAIR in pediatric patients have not been established.
8.5 Geriatric Use
Of the 636 COPD patients exposed to TUDORZA PRESSAIR 400 mcg twice daily for up to 24 weeks in three placebo-controlled clinical trials, 197 were less than 60 years, 272 were greater than or equal to 60 to less than 70 years, and 167 were greater than or equal to 70 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Based on available data for TUDORZA PRESSAIR, no adjustment of dosage in geriatric patients is warranted [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
The pharmacokinetics of TUDORZA PRESSAIR were investigated in subjects with normal renal function and in subjects with mild, moderate, and severe renal impairment [see Clinical Pharmacology (12.3)]. No clinically significant differences in aclidinium pharmacokinetics were noted between these populations. Based on available data for TUDORZA PRESSAIR, no adjustment of dosage in renally impaired subjects is warranted.
8.7 Hepatic Impairment
The effects of hepatic impairment on the pharmacokinetics of TUDORZA PRESSAIR were not studied [see Clinical Pharmacology (12.3)].
DESCRIPTION SECTION
11 DESCRIPTION
TUDORZA PRESSAIR consists of a dry powder formulation of aclidinium bromide for oral inhalation only.
Aclidinium bromide, the active component of TUDORZA PRESSAIR is an anticholinergic with specificity for muscarinic receptors. Aclidinium bromide is a synthetic, quaternary ammonium compound, chemically described as 1-azoniabicyclo[2.2.2]octane, 3-[(hydroxydi-2-thienylacetyl)oxy]-1-(3-phenoxypropyl)-, bromide, (3R)-. The structural formula is:
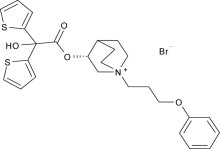
Aclidinium bromide is a white powder with a molecular formula of C26H30NO4S2Br and a molecular mass of 564.56. It is very slightly soluble in water and ethanol and sparingly soluble in methanol.
TUDORZA PRESSAIR is a breath-actuated multi-dose dry powder inhaler. Each actuation of TUDORZA PRESSAIR provides a metered dose of 13 mg of the formulation which contains lactose monohydrate (which may contain milk proteins) as the carrier and 400 mcg of aclidinium bromide (equivalent to 343 mcg of aclidinium). This results in delivery of 375 mcg aclidinium bromide (equivalent to 322 mcg of aclidinium) from the mouthpiece, based on in vitro testing at an average flow rate of 63 L/min with constant volume of 2 L. The amount of drug delivered to the lungs will vary depending on patient factors such as inspiratory flow rate and inspiratory time.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Aclidinium bromide is a long-acting antimuscarinic agent, which is often referred to as an anticholinergic. It has similar affinity to the subtypes of muscarinic receptors M1 to M5. In the airways, it exhibits pharmacological effects through inhibition of M3 receptor at the smooth muscle leading to bronchodilation. The competitive and reversible nature of antagonism was shown with human and animal origin receptors and isolated organ preparations. In preclinical in vitro as well as in vivo studies, prevention of acetylcholine- induced bronchoconstriction effects was dose-dependent and lasted longer than 24 hours. The clinical relevance of these findings is unknown. The bronchodilation following inhalation of aclidinium bromide is predominantly a site-specific effect.
12.2 Pharmacodynamics
Cardiovascular Effects
In a thorough QT Study, 200 mcg and 800 mcg TUDORZA PRESSAIR was administered to healthy volunteers once daily for 3 days; no effects on prolongation of QT interval were observed using QTcF heart-rate correction methods.
Additionally, the effect of TUDORZA PRESSAIR on cardiac rhythm was assessed in 336 COPD patients, 164 patients received aclidinium bromide 400 mcg twice daily and 172 patients received placebo, using 24-hr Holter monitoring. No clinically significant effects on cardiac rhythm were observed.
12.3 Pharmacokinetics
Absorption
The absolute bioavailability of aclidinium bromide is approximately 6% in healthy volunteers. Following twice-daily oral inhalation administration of 400 mcg aclidinium bromide in healthy subjects, peak steady state plasma levels were observed within 10 minutes after inhalation.
Distribution
Aclidinium bromide shows a volume of distribution of approximately 300 L following intravenous administration of 400 mcg in humans.
Metabolism
Clinical pharmacokinetics studies, including a mass balance study, indicate that the major route of metabolism of aclidinium bromide is hydrolysis, which occurs both chemically and enzymatically by esterases. Aclidinium bromide is rapidly and extensively hydrolyzed to its alcohol and dithienylglycolic acid derivatives, neither of which binds to muscarinic receptors and are devoid of pharmacologic activity.
Therefore, due to the low plasma levels achieved at the clinically relevant doses, aclidinium bromide and its metabolites are not expected to alter the disposition of drugs metabolized by the human CYP450 enzymes.
Elimination
Total clearance was approximately 170 L/h after an intravenous dose of aclidinium bromide in young healthy volunteers with an inter-individual variability of 36%. Intravenously administered radiolabeled aclidinium bromide was administered to healthy volunteers and was extensively metabolized with 1% excreted as unchanged aclidinium. Approximately 54% to 65% of the radioactivity was excreted in urine and 20% to 33% of the dose was excreted in feces. The combined results indicated that almost the entire aclidinium bromide dose was eliminated by hydrolysis. After dry powder inhalation, urinary excretion of aclidinium is about 0.09% of the dose and the estimated effective half-life is 5 to 8 hours.
Drug Interactions
Formal drug interaction studies were not performed. In vitro studies using human liver microsomes indicated that aclidinium bromide and its major metabolites do not inhibit CYP450, 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, 3A4/5, or 4A9/11 at concentrations up to 1,000-fold higher than the maximum plasma concentration that would be expected to be achieved at the therapeutic dose. Therefore, it is unlikely that aclidinium bromide causes CYP450 related drug interactions [see Drug Interactions (7)].
Specific Populations
Elderly Patients
The pharmacokinetic profile of aclidinium bromide and its main metabolites was assessed in 12 elderly COPD patients (aged 70 years or older) compared to a younger cohort of 12 COPD patients (40-59 years) that were administered 400 mcg aclidinium bromide once daily for 3 days via inhalation. No clinically significant differences in systemic exposure (AUC and Cmax) were observed when the two groups were compared. No dosage adjustment is necessary in elderly patients [see Use in Specific Populations (8.5)].
Renal Impairment
The impact of renal disease upon the pharmacokinetics of aclidinium bromide was studied in 18 subjects with mild, moderate, or severe renal impairment. Systemic exposure (AUC and Cmax) to aclidinium bromide and its main metabolites following single doses of 400 mcg aclidinium bromide was similar in renally impaired patients compared with 6 matched healthy control subjects. No dose adjustment is necessary in renally impaired patients [see Use in Specific Populations (8.6)].
Hepatic Impairment
The effects of hepatic impairment on the pharmacokinetics of aclidinium bromide were not studied. However, hepatic insufficiency is not expected to have relevant influence on aclidinium bromide pharmacokinetics, since it is predominantly metabolized by chemical and enzymatic hydrolysis to products that do not bind to muscarinic receptors [see Use in Specific Populations (8.7)].
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year inhalation studies were conducted in mice and rats to assess the carcinogenic potential of aclidinium bromide. No evidence of tumorigenicity was observed in rats and mice at aclidinium doses up to 0.20 and 2.4 mg/kg/day, respectively [approximately 10 and 80 times the Maximum Recommended Human Daily Inhalation Dose (MRHDID), respectively, based on summed AUCs of aclidinium bromide and its metabolites].
Aclidinium bromide was positive in the in vitro bacterial gene mutation assay and the in vitro thymidine locus mouse lymphoma assay. However, aclidinium bromide was negative in the in vivo mouse micronucleus assay and the in vivo/in vitro unscheduled DNA synthesis assay with rat liver.
Aclidinium bromide impaired several fertility and reproductive performance indices (increased number of days to mate, decreased conception rate, decreased number of corpora lutea, increased pre-implantation loss with consequent decreased number of implantations, and live embryos) in both male and female rats administered inhaled doses greater than or equal to 0.8 mg/kg/day [approximately 15 times the MRHDID based on summed AUCs of aclidinium bromide and its metabolites]. These adverse fertility effects were observed in the presence of paternal toxicity as evidenced by mortality and decreased body weight gain. However, there were no effects on mating index and sperm number and morphology. In the separate fertility assessments (treated males mated with untreated females; treated females mated with untreated males), no effect was observed in male and female rats at inhaled doses of 1.9 and 0.8 mg/kg/day, respectively [approximately 30 and 15 times the MRHDID, respectively, based on summed AUCs of aclidinium bromide and its metabolites].
