Indomethacin
These highlights do not include all the information needed to use INDOMETHACIN SUPPOSITORIES safely and effectively. See full prescribing information for INDOMETHACIN SUPPOSITORIES. INDOMETHACIN suppositories, for rectal use Initial U.S. Approval: 1965
c81343f2-5ef5-4635-9b94-5ac8d72aa61e
HUMAN PRESCRIPTION DRUG LABEL
Sep 3, 2025
Camber Pharmaceuticals, Inc.
DUNS: 826774775
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Indomethacin
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
Drug Labeling Information
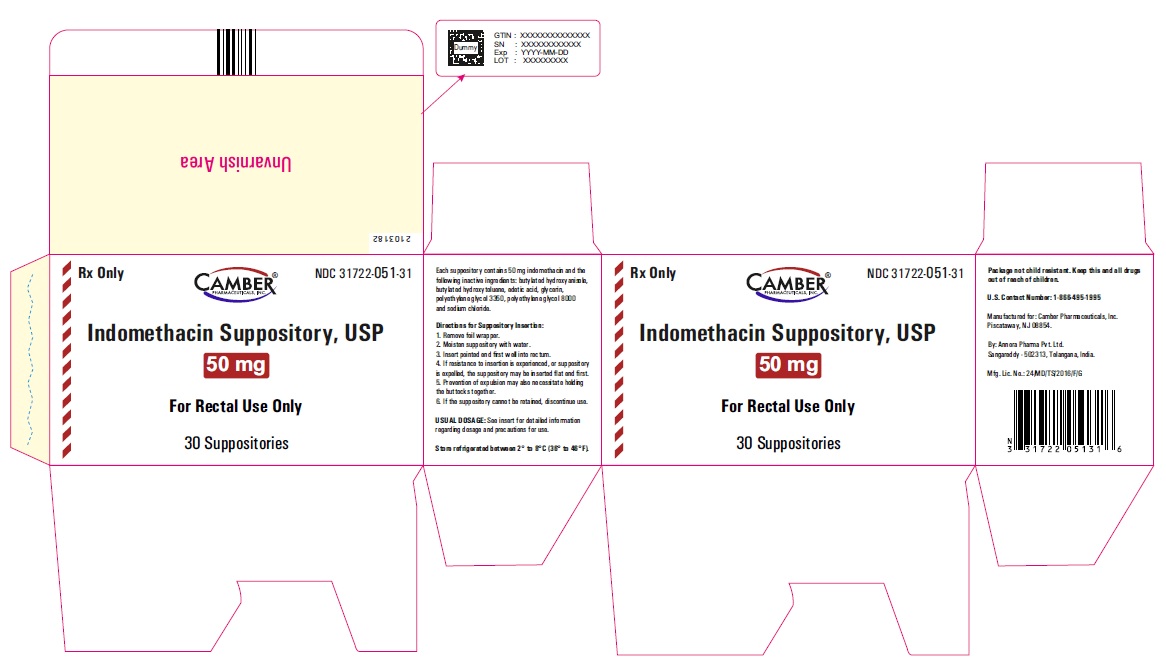
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Indomethacin suppositories USP, 50 mg-Blister carton
BOXED WARNING SECTION
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Indomethacin Suppository is indicated for:
• Moderate to severe rheumatoid arthritis including acute flares of chronic
disease
• Moderate to severe ankylosing spondylitis
• Moderate to severe osteoarthritis
• Acute painful shoulder (bursitis and/or tendinitis)
• Acute gouty arthritis
Indomethacin suppository is a nonsteroidal anti-inflammatory drug indicated
for:
• Moderate to severe rheumatoid arthritis including acute flares of chronic
disease
• Moderate to severe ankylosing spondylitis
• Moderate to severe osteoarthritis
• Acute painful shoulder (bursitis and/or tendinitis)
• Acute gouty arthritis ( 1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Indomethacin suppositories are contraindicated in the following patients:
• Known hypersensitivity (e.g., anaphylactic reactions and serious skin
reactions) to indomethacin or any components of the drug product [ see Warnings and Precautions ( 5.7, 5.9) ]
• History of asthma, urticaria, or other allergic-type reactions after taking
aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to
NSAIDs have been reported in such patients [ see Warnings and Precautions ( 5.7, 5.8) ]
• In the setting of coronary artery bypass graft (CABG) surgery [ see Warnings and Precautions ( 5.1) ]
• In patients with a history of proctitis or recent rectal bleeding
• Known hypersensitivity to indomethacin or any components of the drug product
( 4)
• History of asthma, urticaria, or other allergic-type reactions after taking
aspirin or other NSAIDs ( 4)
• In the setting of CABG surgery ( 4)
• In patients with a history of proctitis or recent rectal bleeding ( 4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to
three years duration have shown an increased risk of serious cardiovascular
(CV) thrombotic events, including myocardial infarction (MI) and stroke, which
can be fatal. Based on available data, it is unclear that the risk for CV
thrombotic events is similar for all NSAIDs. The relative increase in serious
CV thrombotic events over baseline conferred by NSAID use appears to be
similar in those with and without known CV disease or risk factors for CV
disease. However, patients with known CV disease or risk factors had a higher
absolute incidence of excess serious CV thrombotic events, due to their
increased baseline rate. Some observational studies found that this increased
risk of serious CV thrombotic events began as early as the first weeks of
treatment. The increase in CV thrombotic risk has been observed most
consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated
patients, use the lowest effective dose for the shortest duration possible.
Physicians and patients should remain alert for the development of such
events, throughout the entire treatment course, even in the absence of
previous CV symptoms. Patients should be informed about the symptoms of
serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the
increased risk of serious CV thrombotic events associated with NSAID use. The
concurrent use of aspirin and an NSAID, such as indomethacin, increases the
risk of serious gastrointestinal (GI) events [ see Warnings and Precautions ( 5.2) ].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the
treatment of pain in the first 10 to 14 days following CABG surgery found an
increased incidence of myocardial infarction and stroke. NSAIDs are
contraindicated in the setting of CABG [ see Contraindications ( 4) ].
Post-MI Patients
Observational studies conducted in the Danish National Registry have
demonstrated that patients treated with NSAIDs in the post-MI period were at
increased risk of reinfarction, CV-related death, and all-cause mortality
beginning in the first week of treatment. In this same cohort, the incidence
of death in the first year post-MI was 20 per 100 person years in NSAID-
treated patients compared to 12 per 100 person years in non-NSAID exposed
patients. Although the absolute rate of death declined somewhat after the
first year post-MI, the increased relative risk of death in NSAID users
persisted over at least the next four years of follow-up.
Avoid the use of indomethacin suppositories in patients with a recent MI
unless the benefits are expected to outweigh the risk of recurrent CV
thrombotic events. If indomethacin suppositories are used in patients with a
recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including indomethacin, cause serious gastrointestinal (GI) adverse
events including inflammation, bleeding, ulceration, and perforation of the
esophagus, stomach, small intestine, or large intestine, which can be fatal.
These serious adverse events can occur at any time, with or without warning
symptoms, in patients treated with NSAIDs. Only one in five patients who
develop a serious upper GI adverse event on NSAID therapy is symptomatic.
Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in
approximately 1% of patients treated for 3 to 6 months, and in about 2% to 4%
of patients treated for one year. However, even short-term NSAID therapy is
not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who
used NSAIDs had a greater than 10-fold increased risk for developing a GI
bleed compared to patients without these risk factors. Other factors that
increase the risk of GI bleeding in patients treated with NSAIDs include
longer duration of NSAID therapy; concomitant use of oral corticosteroids,
aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs);
smoking; use of alcohol; older age; and poor general health status. Most
postmarketing reports of fatal GI events occurred in elderly or debilitated
patients. Additionally, patients with advanced liver disease and/or
coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients:
• Use the lowest effective dosage for the shortest possible duration.
• Avoid administration of more than one NSAID at a time.
• Avoid use in patients at higher risk unless benefits are expected to
outweigh the increased risk of bleeding. For such patients, as well as those
with active GI bleeding, consider alternate therapies other than NSAIDs.
• Remain alert for signs and symptoms of GI ulceration and bleeding during
NSAID therapy.
• If a serious GI adverse event is suspected, promptly initiate evaluation and
treatment, and discontinue indomethacin until a serious GI adverse event is
ruled out.
• In the setting of concomitant use of low-dose aspirin for cardiac
prophylaxis, monitor patients more closely for evidence of GI bleeding [ see Drug Interactions ( 7) ].
5.3 Hepatotoxicity
Elevations of ALT or AST (three or more times the upper limit of normal [ULN])
have been reported in approximately 1% of NSAID-treated patients in clinical
trials. In addition, rare, sometimes fatal, cases of severe hepatic injury,
including fulminant hepatitis, liver necrosis, and hepatic failure have been
reported.
Elevations of ALT or AST (less than three times ULN) may occur in up to 15% of
patients treated with NSAIDs including indomethacin.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g.,
nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant
tenderness, and "flu-like" symptoms). If clinical signs and symptoms
consistent with liver disease develop, or if systemic manifestations occur
(e.g., eosinophilia, rash, etc.), discontinue indomethacin immediately, and
perform a clinical evaluation of the patient.
5.4 Hypertension
NSAIDs, including indomethacin, can lead to new onset of hypertension or
worsening of preexisting hypertension, either of which may contribute to the
increased incidence of CV events. Patients taking angiotensin converting
enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have
impaired response to these therapies when taking NSAIDs [ see Drug Interactions ( 7) ].
Monitor blood pressure (BP) during the initiation of NSAID treatment and
throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists’ Collaboration meta-analysis of
randomized controlled trials demonstrated an approximately two-fold increase
in hospitalizations for heart failure in COX-2 selective-treated patients and
nonselective NSAID-treated patients compared to placebo-treated patients. In a
Danish National Registry study of patients with heart failure, NSAID use
increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients
treated with NSAIDs. Use of indomethacin may blunt the CV effects of several
therapeutic agents used to treat these medical conditions (e.g., diuretics,
ACE inhibitors, or angiotensin receptor blockers [ARBs]) [ see Drug Interactions ( 7) ].
Avoid the use of indomethacin in patients with severe heart failure unless the
benefits are expected to outweigh the risk of worsening heart failure. If
indomethacin suppositories are used in patients with severe heart failure,
monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis
and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins
have a compensatory role in the maintenance of renal perfusion. In these
patients, administration of an NSAID may cause a dose-dependent reduction in
prostaglandin formation and, secondarily, in renal blood flow, which may
precipitate overt renal decompensation. Patients at greatest risk of this
reaction are those with impaired renal function, dehydration, hypovolemia,
heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or
ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by
recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use
of indomethacin in patients with advanced renal disease. The renal effects of
indomethacin suppositories may hasten the progression of renal dysfunction in
patients with preexisting renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to
initiating indomethacin. Monitor renal function in patients with renal or
hepatic impairment, heart failure, dehydration, or hypovolemia during use of
indomethacin [ see Drug Interactions (7)]. Avoid the use of indomethacin in
patients with advanced renal disease unless the benefits are expected to
outweigh the risk of worsening renal function. If indomethacin is used in
patients with advanced renal disease, monitor patients for signs of worsening
renal function.
It has been reported that the addition of the potassium-sparing diuretic,
triamterene, to a maintenance schedule of indomethacin resulted in reversible
acute renal failure in two of four healthy volunteers. Indomethacin and
triamterene should not be administered together.
Hyperkalemia
Increases in serum potassium concentration, including hyperkalemia, have been
reported with use of NSAIDs, even in some patients without renal impairment.
In patients with normal renal function, these effects have been attributed to
a hyporeninemic-hypoaldosteronism state.
Both indomethacin and potassium-sparing diuretics may be associated with
increased serum potassium levels. The potential effects of indomethacin and
potassium-sparing diuretics on potassium levels and renal function should be
considered when these agents are administered concurrently.
5.7 Anaphylactic Reactions
Indomethacin has been associated with anaphylactic reactions in patients with
and without known hypersensitivity to indomethacin and in patients with
aspirin-sensitive asthma [see Contraindications ( 4) and Warnings and Precautions ( 5.8) ].
Seek emergency help if an anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, indomethacin is contraindicated in patients with this form of aspirin sensitivity [ see Contraindications ( 4) ]. When indomethacin suppositories are used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, includingindomethacin, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. NSAIDs can also cause fixed drug eruption (FDE). FDE may present as a more severe variant known as generalized bullous fixed drug eruption (GBFDE), which can be life-threatening. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of indomethacin at the first appearance of skin rash or any other sign of hypersensitivity. Indomethacin is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been
reported in patients taking NSAIDs such as indomethacin. Some of these
events have been fatal or life-threatening. DRESS typically, although not
exclusively, presents with fever, rash, lymphadenopathy, and/or facial
swelling.
Other clinical manifestations may include hepatitis, nephritis, hematological
abnormalities, myocarditis, or myositis. Sometimes symptoms of DRESS may
resemble an acute viral infection. Eosinophilia is often present. Because this
disorder is variable in its presentation, other organ systems not noted here
may be involved. It is important to note that early manifestations of
hypersensitivity, such as fever or lymphadenopathy, may be present even though
rash is not evident. If such signs or symptoms are present, discontinue
indomethacin and evaluate the patient immediately.
5.11 Fetal Toxicity
Premature Closure of Fetal Ductus Arteriosus
Avoid use of NSAIDS, including indomethacin, in pregnant women at about 30
weeks of gestation and later. NSAIDs, including indomethacin, increase the
risk of premature closure of the fetal ductus arteriosus at approximately this
gestational age.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs, including indomethacin, at about 20 weeks gestation or later in
pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in
some cases, neonatal renal impairment. These adverse outcomes are seen, on
average, after days to weeks of treatment, although oligohydramnios has been
infrequently reported as soon as 48 hours after NSAID initiation.
Oligohydramnios is often, but not always, reversible with treatment
discontinuation. Complications of prolonged oligohydramnios may, for example,
include limb contractures and delayed lung maturation. In some postmarketing
cases of impaired neonatal renal function, invasive procedures such as
exchange transfusion or dialysis were required.
If NSAID treatment is necessary between about 20 weeks and 30 weeks gestation,
limit indomethacin use to the lowest effective dose and shortest duration
possible. Consider ultrasound monitoring of amniotic fluid if indomethacin
treatment extends beyond 48 hours. Discontinue indomethacin if
oligohydramnios occurs and follow up according to clinical practice [see Use in Specific Populations (8.1)].
5.12 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or
gross blood loss, fluid retention, or an incompletely described effect on
erythropoiesis. If a patient treated with indomethacin has any signs or
symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including indomethacin, may increase the risk of bleeding events. Co-
morbid conditions, such as coagulation disorders, or concomitant use of
warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin
reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors
(SNRIs) may increase this risk. Monitor these patients for signs of bleeding
[see Drug Interactions (7)].
5.13 Masking of Inflammation and Fever
The pharmacological activity of indomethacin in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.
5.14 Laboratory Monitoring
Because serious GI bleeding, hepatotoxicity, and renal injury can occur without warning symptoms or signs, consider monitoring patients on long-term NSAID treatment with a CBC and a chemistry profile periodically [ see Warnings and Precautions ( 5.2, 5.3, 5.6) ].
5.15 Central Nervous System Effects
Indomethacin may aggravate depression or other psychiatric disturbances,
epilepsy, and parkinsonism, and should be used with considerable caution in
patients with these conditions. Discontinue indomethacin suppositories if
severe CNS adverse reactions develop.
Indomethacin may cause drowsiness; therefore, caution patients about engaging
in activities requiring mental alertness and motor coordination, such as
driving a car. Indomethacin may also cause headache. Headache which persists
despite dosage reduction requires cessation of therapy with indomethacin.
5.16 Ocular Effects
Corneal deposits and retinal disturbances, including those of the macula, have been observed in some patients who had received prolonged therapy with indomethacin. Be alert to the possible association between the changes noted and indomethacin. It is advisable to discontinue therapy if such changes are observed. Blurred vision may be a significant symptom and warrants a thorough ophthalmological examination. Since these changes may be asymptomatic, ophthalmologic examination at periodic intervals is desirable in patients receiving prolonged therapy. Indomethacin is not indicated for long-term treatment.
• Hepatotoxicity:Inform patients of warning signs and symptoms of
hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if
clinical signs and symptoms of liver disease develop ( 5.3)
• Hypertension:Patients taking some antihypertensive medications may have
impaired response to these therapies when taking NSAIDs. Monitor blood
pressure ( 5.4, 7)
• Heart Failure and Edema:Avoid use of indomethacin in patients with severe
heart failure unless benefits are expected to outweigh risk of worsening heart
failure ( 5.5)
• Renal Toxicity:Monitor renal function in patients with renal or hepatic
impairment, heart failure, dehydration, or hypovolemia. Avoid use of
indomethacin in patients with advanced renal disease unless benefits are
expected to outweigh risk of worsening renal function ( 5.6)
• Anaphylactic Reactions:Seek emergency help if an anaphylactic reaction
occurs ( 5.7)
• Exacerbation of Asthma Related to Aspirin Sensitivity:Indomethacin is
contraindicated in patients with aspirin-sensitive asthma. Monitor patients
with preexisting asthma (without aspirin sensitivity) ( 5.8)
• Serious Skin Reactions:Discontinue indomethacin at first appearance of skin
rash or other signs of hypersensitivity ( 5.9)
• Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS):Discontinue
and evaluate clinically ( 5.10)
• Fetal Toxicity:Limit use of NSAIDs, including indomethacin, between about 20
to 30 weeks in pregnancy due to the risk of oligohydramnios/fetal renal
dysfunction. Avoid use of NSAIDs in women at about 30 weeks gestation and
later in pregnancy due to the risks of oligohydramnios/fetal dysfunction and
premature closure of the fetal ductus arteriosus ( 5.11, 8.1)
• Hematologic Toxicity:Monitor hemoglobin or hematocrit in patients with any
signs or symptoms of anemia ( 5.12, 7)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other
sections of the labeling:
• Cardiovascular Thrombotic Events [ see Warnings and Precautions ( 5.1) ]
• GI Bleeding, Ulceration and Perforation [ see Warnings and Precautions ( 5.2) ]
• Hepatotoxicity [ see Warnings and Precautions ( 5.3) ]
• Hypertension [ see Warnings and Precautions ( 5.4) ]
• Heart Failure and Edema [ see Warnings and Precautions ( 5.5) ]
• Renal Toxicity and Hyperkalemia [ see Warnings and Precautions ( 5.6) ]
• Anaphylactic Reactions [ see Warnings and Precautions ( 5.7) ]
• Serious Skin Reactions [ see Warnings and Precautions ( 5.9) ]
• Hematologic Toxicity [ see Warnings and Precautions ( 5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse
reaction rates observed in the clinical trials of a drug cannot be directly
compared to rates in the clinical trials of another drug and may not reflect
the rates observed in clinical practice.
In a gastroscopic study in 45 healthy subjects, the number of gastric mucosal
abnormalities was significantly higher in the group receiving indomethacin
capsules than in the group taking indomethacin suppositories or placebo.
In a double-blind comparative clinical study involving 175 patients with
rheumatoid arthritis, however, the incidence of upper gastrointestinal adverse
effects with indomethacin suppositories or capsules was comparable. The
incidence of lower gastrointestinal adverse effects was greater in the
suppository group.
The adverse reactions for indomethacin capsules listed in the following table
have been arranged into two groups: (1) incidence greater than 1%; and (2)
incidence less than 1%. The incidence for group (1) was obtained from 33
double-blind controlled clinical trials reported in the literature (1,092
patients). The incidence for group (2) was based on reports in clinical
trials, in the literature, and on voluntary reports since marketing. The
probability of a causal relationship exists between indomethacin and these
adverse reactions, some of which have been reported only rarely.
The adverse reactions reported with indomethacin capsules may occur with use
of the suppositories. In addition, rectal irritation and tenesmus have been
reported in patients who have received the suppositories.
Table 1 Summary of Adverse Reactions for Indomethacin Capsules
|
Incidence greater than 1% |
Incidence less than 1% | |
|
GASTROINTESTINAL | ||
|
nausea* with or |
anorexia |
gastrointestinal bleeding without obvious ulcer formation and perforation of preexisting sigmoid lesions (diverticulum, carcinoma, etc.) development of ulcerative colitis and regional ileitis ulcerative stomatitis toxic hepatitis and jaundice (some fatal cases have been reported) intestinal strictures (diaphragms) pancreatitis |
|
CENTRAL NERVOUS SYSTEM | ||
|
headache (11.7%) |
anxiety (includes nervousness) muscle weakness |
light-headedness |
|
SPECIAL SENSES | ||
|
tinnitus |
ocular — corneal deposits and retinal disturbances, including those of the macula, have been reported in some patients on prolonged therapy with indomethacin |
blurred vision |
|
CARDIOVASCULAR | ||
|
None |
hypertension |
congestive heart failure |
|
METABOLIC | ||
|
None |
edema |
hyperglycemia |
|
INTEGUMENTARY | ||
|
none |
pruritus |
exfoliative dermatitis |
|
HEMATOLOGIC | ||
|
None |
leukopenia |
aplastic anemia |
|
HYPERSENSITIVITY | ||
|
None |
acute anaphylaxis |
dyspnea |
|
GENITOURINARY | ||
|
None |
hematuria |
BUN elevation |
|
MISCELLANEOUS | ||
|
None |
epistaxis | |
|
**Causal relationship unknown:**Other reactions have been reported but
occurred under circumstances where a causal relationship could not be
established. However, in these rarely reported events, the possibility cannot
be excluded. Therefore, these observations are being listed to serve as
alerting information to physicians:
Cardiovascular:Thrombophlebitis
Hematologic:Although there have been several reports of leukemia, the
supporting information is weak
Genitourinary:Urinary frequency
A rare occurrence of fulminant necrotizing fasciitis, particularly in
association with Group Aβ hemolytic streptococcus, has been described in
persons treated with nonsteroidal anti-inflammatory agents, including
indomethacin, sometimes with fatal outcome
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use
of indomethacin. Because these reactions are reported voluntarily from a
population of uncertain size, it is not always possible to reliably estimate
their frequency or establish a causal relationship to drug exposure.
Skin and Appendages: Exfoliative dermatitis, Stevens-Johnson Syndrome (SJS),
toxic epidermal necrolysis (TEN), and fixed drug eruption (FDE).
Most common adverse reactions (incidence ≥ 3%) are headache, dizziness, dyspepsia, and nausea. ( 6)
To report SUSPECTED ADVERSE REACTIONS, contact Annora Pharma Private Limited at 1-866-495-1995 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
See Table 2 for clinically significant drug interactions with indomethacin.
Table 2 Clinically Significant Drug Interactions with Indomethacin
|
Drugs That Interfere with Hemostasis | |
|
Clinical Impact: |
|
|
Intervention: |
Monitor patients with concomitant use of indomethacin with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [ see Warnings and Precautions (5.12)]. |
|
Aspirin | |
|
Clinical Impact: |
Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [ see Warnings and Precautions ( 5.2) ]. |
|
Intervention: |
Concomitant use of indomethacin and analgesic doses of aspirin is not
generally recommended because of the increased risk of bleeding [ see Warnings and Precautions (5.12)]. |
|
ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers | |
|
Clinical Impact: |
|
|
Intervention: |
|
|
Diuretics | |
|
Clinical Impact: |
Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis. It has been reported that the addition of triamterene to a maintenance schedule of indomethacin resulted in reversible acute renal failure in two of four healthy volunteers. Indomethacin and triamterene should not be administered together. Both indomethacin suppository and potassium-sparing diuretics may be associated with increased serum potassium levels. The potential effects of indomethacin and potassium-sparing diuretics on potassium levels and renal function should be considered when these agents are administered concurrently. |
|
Intervention: |
Indomethacin and triamterene should not be administered together. During concomitant use of indomethacin suppository with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects. Be aware that indomethacin and potassium-sparing diuretics may both be associated with increased serum potassium levels [ see Warnings and Precautions ( 5.6) ]. |
|
Digoxin | |
|
Clinical Impact: |
The concomitant use of indomethacin with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. |
|
Intervention: |
During concomitant use of indomethacin suppository and digoxin, monitor serum digoxin levels. |
|
Lithium | |
|
Clinical Impact: |
NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance .The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. |
|
Intervention: |
During concomitant use of indomethacin suppositories and lithium, monitor patients for signs of lithium toxicity. |
|
Methotrexate | |
|
Clinical Impact: |
Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). |
|
Intervention: |
During concomitant use of indomethacin suppositories and methotrexate, monitor patients for methotrexate toxicity. |
|
Cyclosporine | |
|
Clinical Impact: |
Concomitant use of indomethacin and cyclosporine may increase cyclosporine’s nephrotoxicity. |
|
Intervention: |
During concomitant use of indomethacin and cyclosporine, monitor patients for signs of worsening renal function. |
|
NSAIDs and Salicylates | |
|
Clinical Impact: |
Concomitant use of indomethacin with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [ see Warnings and Precautions ( 5.2) ] . Combined use with diflunisal may be particularly hazardous because diflunisal causes significantly higher plasma levels of indomethacin [see Clinical Pharmacology ( 12.3) ]. In some patients, combined use of indomethacin and diflunisal has been associated with fatal gastrointestinal hemorrhage. |
|
Intervention: |
The concomitant use of indomethacin with other NSAIDs or salicylates, especially diflunisal, is not recommended. |
|
Pemetrexed | |
|
Clinical Impact: |
Concomitant use of indomethacin and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). |
|
Intervention: |
During concomitant use of indomethacin and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity. NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed. In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration. |
|
Probenecid | |
|
Clinical Impact: |
When indomethacin is given to patients receiving probenecid, the plasma levels of indomethacin are likely to be increased. |
|
Intervention: |
During the concomitant use of indomethacin and probenecid, a lower total daily dosage of indomethacin may produce a satisfactory therapeutic effect. When increases in the dose of indomethacin are made, they should be made carefully and in small increments. |
Effects on Laboratory Tests
Indomethacin reduces basal plasma renin activity (PRA), as well as those
elevations of PRA induced by furosemide administration, or salt or volume
depletion. These facts should be considered when evaluating plasma renin
activity in hypertensive patients.
False-negative results in the dexamethasone suppression test (DST) in patients
being treated with indomethacin have been reported. Thus, results of the DST
should be interpreted with caution in these patients.
• Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin,
SSRIs/SNRIs):Monitor patients for bleeding who are concomitantly taking
indomethacin with drugs that interfere with hemostasis. Concomitant use of
indomethacin and analgesic doses of aspirin is not generally recommended ( 7)
• ACE Inhibitors, Angiotensin Receptor Blockers (ARB), or Beta-
Blockers:Concomitant use with indomethacin may diminish the antihypertensive
effect of these drugs. Monitor blood pressure ( 7)
• ACE Inhibitors and ARBs: Concomitant use with indomethacin in elderly,
volume depleted, or those with renal impairment may result in deterioration of
renal function. In such high risk patients, monitor for signs of worsening
renal function ( 7)
• Diuretics:NSAIDs can reduce natriuretic effect of furosemide and thiazide
diuretics. Monitor patients to assure diuretic efficacy including
antihypertensive effects ( 7)
• Digoxin:Concomitant use with indomethacin can increase serum concentration
and prolong half-life of digoxin. Monitor serum digoxin levels ( 7)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Indomethacin Suppositories USP: 50 mg of indomethacin white to off-white, bullet shaped.
Indomethacin Suppositories: 50 mg ( 3)
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
Warnings and Precautions (5.9) 11/2024
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
Carefully consider the potential benefits and risks of indomethacin suppositories and other treatment options before deciding to use indomethacin suppositories. Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [ see Warnings and Precautions ( 5) ].
After observing the response to initial therapy with indomethacin, the dose and frequency should be adjusted to suit an individual patient’s needs.
Adverse reactions generally appear to correlate with the dose of indomethacin. Therefore, every effort should be made to determine the lowest effective dosage for the individual patient.
SUPPOSITORIES: Indomethacin Suppositories are available as 50 mg suppositories for rectal use only. Indomethacin Suppositories are not for oral or intravaginal use.
2.2 Suppository Dosing Instructions
THIS SECTION PREDOMINANTLY MAKES REFERENCE TO INDOMETHACIN CAPSULE, USP ORAL
DOSAGE FOR GUIDANCE IN USING SUPPOSITORIES.
Indomethacin suppositories 50 mg can be substituted for indomethacin
capsules, USP; however, there will be significant differences between the two
dosage regimens in indomethacin blood levels [see Clinical Pharmacology ( 12.3)].
Oral dosage recommendations for active stages of the following:
2.3 Moderate to severe rheumatoid arthritis including acute flares of
chronic disease; moderate to severe ankylosing spondylitis; and moderate to severe osteoarthritis
Indomethacin capsules, USP 25 mg twice a day or three times a day. If this is
well tolerated, increase the daily dosage by 25 mg or by 50 mg, if required by
continuing symptoms, at weekly intervals until a satisfactory response is
obtained or until a total daily dose of 150 to 200 mg is reached. Doses above
this amount generally do not increase the effectiveness of the drug.
In patients who have persistent night pain and/or morning stiffness, the
giving of a large portion, up to a maximum of 100 mg, of the total daily dose
at bedtime, either orally or by rectal suppositories, may be helpful in
affording relief. The total daily dose should not exceed 200 mg. In acute
flares of chronic rheumatoid arthritis, it may be necessary to increase the
dosage by 25 mg or, if required, by 50 mg daily.
If minor adverse effects develop as the dosage is increased, reduce the dosage
rapidly to a tolerated dose and observe the patient closely.
If severe adverse reactions occur, stop the drug. After the acute phase of the
disease is under control, an attempt to reduce the daily dose should be made
repeatedly until the patient is receiving the smallest effective dose or the
drug is discontinued.
Careful instructions to, and observations of, the individual patient are
essential to the prevention of serious, irreversible, including fatal, adverse
reactions.
As advancing years appear to increase the possibility of adverse reactions,
indomethacin suppositories should be used with greater care in the elderly.
[see Use in Specific Populations ( 8.5) ]
2.4 Acute painful shoulder (bursitis and/or tendinitis)
Indomethacin capsules, USP 75 to 150 mg daily in 3 or 4 divided doses. The drug should be discontinued after the signs and symptoms of inflammation have been controlled for several days. The usual course of therapy is 7 to 14 days.
2.5 Acute Gouty Arthritis
Indomethacin capsules, USP 50 mg three times a day. Until pain is tolerable. The dose should then be rapidly reduced to complete cessation of the drug. Definite relief of pain has been reported within 2 to 4 hours. Tenderness and heat usually subside in 24 to 36 hours, and swelling gradually disappears in 3 to 5 days.
• Use the lowest effective dosage for shortest duration consistent with
individual patient treatment goals ( 2.1)
• Indomethacin suppositories 50 mg can be substituted for indomethacin
capsules, USP; however, there will be significant differences between the two
dosage regimens in indomethacin blood levels ( 12.3)
• The dosage for moderate to severe rheumatoid arthritis including acute
flares of chronic disease; moderate to severe ankylosing spondylitis; and
moderate to severe osteoarthritis is indomethacin capsules, USP 25 mg two or
three times a day ( 2.3)
• The dosage for acute painful shoulder (bursitis and/or tendinitis) is
indomethacin capsules, USP 75 to 150 mg daily in 3 or 4 divided doses ( 2.4)
• The dosage for acute gouty arthritis is indomethacin capsules, USP 50 mg
three times a day ( 2.5)
• Indomethacin Suppositories are not for oral or intravaginal use
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Use of NSAIDs, including indomethacin, can cause premature closure of the
fetal ductus arteriosus and fetal renal dysfunction leading to oligohydramnios
and, in some cases, neonatal renal impairment. Because of these risks, limit
dose and duration of indomethacin use between about 20 and 30 weeks of
gestation, and avoid indomethacin use at about 30 weeks of gestation and later
in pregnancy ( see Clinical Considerations, Data).
Premature Closure of Fetal Ductus Arteriosus
Use of NSAIDS, including indomethacin, at about 30 weeks gestation or later in
pregnancy increases the risk of premature closure of the fetal ductus
arteriosus.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs at about 20 weeks gestation or later in pregnancy has been
associated with cases of fetal renal dysfunction leading to oligohydramnios,
and in some cases, neonatal renal impairment.
Data from observational studies regarding other potential embryofetal risks of
NSAID use in women in the first or second trimesters of pregnancy are
inconclusive. In animal reproduction studies retarded fetal ossification was
observed with administration of indomethacin to mice and rats during
organogenesis at doses 0.1 and 0.2 times, respectively, the maximum
recommended human dose (MRHD, 200 mg). In published studies in pregnant mice,
indomethacin produced maternal toxicity and death, increased fetal
resorptions, and fetal malformations at 0.1 times the MRHD. When rat and mice
dams were dosed during the last three days of gestation, indomethacin produced
neuronal necrosis in the offspring at 0.1 and 0.05 times the MRHD,
respectively [ see Data]. Based on animal data, prostaglandins have been shown
to have an important role in endometrial vascular permeability, blastocyst
implantation, and decidualization. In animal studies, administration of
prostaglandin synthesis inhibitors such as indomethacin, resulted in increased
pre- and post-implantation loss. Prostaglandins also have been shown to have
an important role in fetal kidney development. In published animal studies,
prostaglandin synthesis inhibitors have been reported to impair kidney
development when administered at clinically relevant doses.
The estimated background risk of major birth defects and miscarriage for the
indicated population(s) is unknown. All pregnancies have a background risk of
birth defect, loss, or other adverse outcomes. In the U.S. general population,
the estimated background risk of major birth defects and miscarriage in
clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Premature Closure of Fetal Ductus Arteriosus:
Avoid use of NSAIDs in women at about 30 weeks gestation and later in
pregnancy, because NSAIDs, including indomethacin, can cause premature closure
of the fetal ductus arteriosus ( see Data).
Oligohydramnios/Neonatal Renal Impairment:
If an NSAID is necessary at about 20 weeks gestation or later in pregnancy,
limit the use to the lowest effective dose and shortest duration possible. If
indomethacin treatment extends beyond 48 hours, consider monitoring with
ultrasound for oligohydramnios. If oligohydramnios occurs, discontinue
indomethacin and follow up according to clinical practice ( see Data).
Data
Human Data
Premature Closure of Fetal Ductus Arteriosus:
Published literature reports that the use of NSAIDs at about 30 weeks of
gestation and later in pregnancy may cause premature closure of the fetal
ductus arteriosus.
Oligohydramnios/Neonatal Renal Impairment:
Published studies and postmarketing reports describe maternal NSAID use at
about 20 weeks gestation or later in pregnancy associated with fetal renal
dysfunction leading to oligohydramnios, and in some cases, neonatal renal
impairment. These adverse outcomes are seen, on average, after days to weeks
of treatment, although oligohydramnios has been infrequently reported as soon
as 48 hours after NSAID initiation. In many cases, but not all, the decrease
in amniotic fluid was transient and reversible with cessation of the drug.
There have been a limited number of case reports of maternal NSAID use and
neonatal renal dysfunction without oligohydramnios, some of which were
irreversible. Some cases of neonatal renal dysfunction required treatment with
invasive procedures, such as exchange transfusion or dialysis.
Methodological limitations of these postmarketing studies and reports include
lack of a control group; limited information regarding dose, duration, and
timing of drug exposure; and concomitant use of other medications. These
limitations preclude establishing a reliable estimate of the risk of adverse
fetal and neonatal outcomes with maternal NSAID use. Because the published
safety data on neonatal outcomes involved mostly preterm infants, the
generalizability of certain reported risks to the full-term infant exposed to
NSAIDs through maternal use is uncertain.
Animal data
Reproductive studies were conducted in mice and rats at dosages of 0.5, 1.0,
2.0, and 4.0 mg/kg/day. Except for retarded fetal ossification at 4 mg/kg/day
(0.1 times [mice] and 0.2 times [rats] the MRHD on a mg/m 2basis,
respectively) considered secondary to the decreased average fetal weights, no
increase in fetal malformations was observed as compared with control groups.
Other studies in mice reported in the literature using higher doses (5 to 15
mg/kg/day, 0.1 to 0.4 times MRHD on a mg/m 2basis) have described maternal
toxicity and death, increased fetal resorptions, and fetal malformations.
Comparable studies in rodents using high doses of aspirin have shown similar
maternal and fetal effects.
In rats and mice, maternal indomethacin administration of 4.0 mg/kg/day (0.2 times and 0.1 times the MRHD on a mg/m 2basis) during the last 3 days of gestation was associated with an increased incidence of neuronal necrosis in the diencephalon in the live-born fetuses however no increase in neuronal necrosis was observed at 2.0 mg/kg/day as compared to the control groups (0.1 times and 0.05 times the MRHD on a mg/m 2basis). Administration of 0.5 or 4.0 mg/kg/day to offspring during the first 3 days of life did not cause an increase in neuronal necrosis at either dose level.
8.2 Lactation
Risk Summary
Based on available published clinical data, indomethacin may be present in
human milk. The developmental and health benefits of breastfeeding should be
considered along with the mother’s clinical need for indomethacin and any
potential adverse effects on the breastfed infant from the indomethacin or
from the underlying maternal condition.
Data
In one study, levels of indomethacin in breast milk were below the sensitivity
of the assay (<20 mcg/L) in 11 of 15 women using doses ranging from 75 mg
orally to 300 mg rectally daily (0.94 to 4.29 mg/kg daily) in the postpartum
period. Based on these levels, the average concentration present in breast
milk was estimated to be 0.27% of the maternal weight- adjusted dose. In
another study indomethacin levels were measured in breast milk of eight
postpartum women using doses of 75 mg daily and the results were used to
calculate an estimated infant daily dose. The estimated infant dose of
indomethacin from breast milk was less than 30 mcg/day or 4.5 mcg/kg/day
assuming breast milk intake of 150 mL/kg/day. This is 0.5% of the maternal
weight-adjusted dosage or about 3% of the neonatal dose for treatment of
patent ductus arteriosus.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs,
including indomethacin, may delay or prevent rupture of ovarian follicles,
which has been associated with reversible infertility in some women. Published
animal studies have shown that administration of prostaglandin synthesis
inhibitors has the potential to disrupt prostaglandin- mediated follicular
rupture required for ovulation. Small studies in women treated with NSAIDs
have also shown a reversible delay in ovulation. Consider withdrawal of
NSAIDs, including indomethacin, in women who have difficulties conceiving or
who are undergoing investigation of infertility.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients 14 years of age and younger has
not been established.
Indomethacin suppositories should not be prescribed for pediatric patients 14
years of age and younger unless toxicity or lack of efficacy associated with
other drugs warrants the risk.
In experience with more than 900 pediatric patients reported in the literature
or to the manufacturer who were treated with indomethacin capsules, side
effects in pediatric patients were comparable to those reported in adults.
Experience in pediatric patients has been confined to the use of indomethacin
capsules.
If a decision is made to use indomethacin for pediatric patients two years of age or older, such patients should be monitored closely and periodic assessment of liver function is recommended. There have been cases of hepatotoxicity reported in pediatric patients with juvenile rheumatoid arthritis, including fatalities. If indomethacin treatment is instituted, a suggested starting dose is 1 to 2 mg/kg/day given in divided doses. Maximum daily dosage should not exceed 3 mg/kg/day or 150 to 200 mg/day, whichever is less. Limited data are available to support the use of a maximum daily dosage of 4 mg/kg/day or 150 to 200 mg/day, whichever is less. As symptoms subside, the total daily dosage should be reduced to the lowest level required to control symptoms, or the drug should be discontinued.
8.5 Geriatric Use
Elderly patients, compared to younger patients, are at greater risk for NSAID-
associated serious cardiovascular, gastrointestinal, and/or renal adverse
reactions. If the anticipated benefit for the elderly patient outweighs these
potential risks, start dosing at the low end of the dosing range, and monitor
patients for adverse effects [ see Warnings and Precautions ( 5.1, 5.2, 5.3, 5.6, 5.13) ].
Indomethacin may cause confusion or rarely, psychosis [ see Adverse Reactions ( 6.1) ]; physicians should remain alert to the possibility of such adverse
effects in the elderly.
Indomethacin and its metabolites are known to be substantially excreted by the
kidneys, and the risk of adverse reactions to this drug may be greater in
patients with impaired renal function. Because elderly patients are more
likely to have decreased renal function, use caution in this patient
population, and it may be useful to monitor renal function [see Clinical Pharmacology ( 12.3) ].
Infertility:NSAIDs are associated with reversible infertility. Consider withdrawal of indomethacin suppositories in women who have difficulties conceiving ( 8.3)
OVERDOSAGE SECTION
10 OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to
lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been
generally reversible with supportive care. Gastrointestinal bleeding has
occurred. Hypertension, acute renal failure, respiratory depression, and coma
have occurred, but were rare [ see Warnings and Precautions ( 5.1, 5.2, 5.4, 5.6) ].
Manage patients with symptomatic and supportive care following an NSAID
overdosage. There are no specific antidotes. Consider emesis and/or activated
charcoal (60 to 100 grams in adults, 1 to 2 grams per kg of body weight in
pediatric patients) and/or osmotic cathartic in symptomatic patients seen
within four hours of ingestion or in patients with a large overdosage (5 to 10
times the recommended dosage). Forced diuresis, alkalinization of urine,
hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdosage treatment contact a poison control
center (1- 800-222-1222).
DESCRIPTION SECTION
11 DESCRIPTION
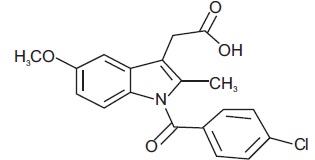
Indomethacin Suppositories USP is a nonsteroidal anti-inflammatory drug, available as a suppository containing 50 mg of indomethacin administered for rectal use. The chemical name is 1-(4-chlorobenzoyl)-5-methoxy-2-methyl-1H-indole-3-acetic acid. The molecular weight is 357.79. Its molecular formula is C 19H 16ClNO 4, and it has the following chemical structure.
Indomethacin USP is a white to yellow crystalline powder. It is sparingly
soluble in absolute alcohol, chloroform and ether and insoluble in water. It
has a pKa of 4.7.
The inactive ingredients in indomethacin suppositories include: Butylated
hydroxy anisole, butylated hydroxy toluene, edetic acid, glycerin,
polyethylene
glycol 3350, polyethylene glycol 8000 and sodium chloride. Indomethacin
suppositories, 50 mg each, are white to off-white, bullet shaped, rectal
suppositories.
FDA approved dissolution test specifications differ from USP.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Indomethacin has analgesic, anti-inflammatory, and antipyretic properties.
The mechanism of action of indomethacin suppositories, like that of other
NSAIDs, is not completely understood but involves inhibition of cyclooxygenase
(COX-1 and COX-2).
Indomethacin is a potent inhibitor of prostaglandin synthesis in vitro.
Indomethacin concentrations reached during therapy have produced in
vivoeffects. Prostaglandins sensitize afferent nerves and potentiate the
action of bradykinin in inducing pain in animal models. Prostaglandins are
mediators of inflammation. Because indomethacin is an inhibitor of
prostaglandin synthesis, its mode of action may be due to a decrease of
prostaglandins in peripheral tissues.
12.3 Pharmacokinetics
Absorption
Following single oral doses of indomethacin capsules 25 mg or 50 mg,
indomethacin is readily absorbed, attaining peak plasma concentrations of
about 1 and 2 mcg/mL, respectively, at about 2 hours. Orally administered
indomethacin capsules are virtually 100% bioavailable, with 90% of the dose
absorbed within 4 hours. With a typical therapeutic regimen of 25 or 50 mg
three times a day, the steady-state plasma concentrations of indomethacin are
an average 1.4 times those following the first dose.
The rate of absorption is more rapid from the rectal suppository than from
indomethacin capsules. Ordinarily, therefore, the total amount absorbed from
the suppository would be expected to be at least equivalent to the capsule. In
controlled clinical trials, however, the amount of indomethacin absorbed was
found to be somewhat less (80 to 90%) than that absorbed from indomethacin
capsules. This is probably because some subjects did not retain the material
from the suppository for the one hour necessary to assure complete absorption.
Since the suppository dissolves rather quickly rather than melting slowly, it
is seldom recovered in recognizable form if the patient retains the
suppository for more than a few minutes.
Distribution
Indomethacin is highly bound to protein in plasma (about 99%) over the
expected range of therapeutic plasma concentrations. Indomethacin has been
found to cross the blood-brain barrier and the placenta, and appears in breast
milk.
Elimination
Metabolism
Indomethacin exists in the plasma as the parent drug and its desmethyl,
desbenzoyl, and desmethyldesbenzoyl metabolites, all in the unconjugated form.
Appreciable formation of glucuronide conjugates of each metabolite and of
indomethacin are formed.
Excretion
Indomethacin is eliminated via renal excretion, metabolism, and biliary
excretion. Indomethacin undergoes appreciable enterohepatic circulation. About
60% of an oral dose is recovered in urine as drug and metabolites (26% as
indomethacin and its glucuronide), and 33% is recovered in feces (1.5% as
indomethacin). The mean half-life of indomethacin is estimated to be about 4.5
hours.
Specific Populations
Pediatric:The pharmacokinetics of indomethacin has not been investigated in
pediatric patients.
Race:Pharmacokinetic differences due to race have not been identified.
Hepatic Impairment:The pharmacokinetics of indomethacin has not been
investigated in patients with hepatic impairment.
Renal Impairment:The pharmacokinetics of indomethacin has not been
investigated in patients with renal impairment [ see Warnings and Precautions ( 5.6) ].
Drug Interaction Studies
Aspirin:
In a study in normal volunteers, it was found that chronic concurrent
administration of 3.6 g of aspirin per day decreases indomethacin blood levels
approximately 20% [ see Drug Interactions ( 7) ].
When NSAIDs were administered with aspirin, the protein binding of NSAIDs were
reduced, although the clearance of free NSAID was not altered. The clinical
significance of this interaction is not known. See Table 2 for clinically
significant drug interactions of NSAIDs with aspirin [ see Drug Interactions ( 7) ].
Diflunisal:
In normal volunteers receiving indomethacin, the administration of diflunisal
decreased the renal clearance and significantly increased the plasma levels of
indomethacin [ see Drug Interactions ( 7) ].
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In an 81-week chronic oral toxicity study in the rat at doses up to 1
mg/kg/day (0.05 times the MRHD on a mg/m 2basis), indomethacin had no
tumorigenic effect. Indomethacin produced no neoplastic or hyperplastic
changes related to treatment in carcinogenic studies in the rat (dosing period
73 to 110 weeks) and the mouse (dosing period 62 to 88 weeks) at doses up to
1.5 mg/kg/day (0.04 times [mice] and 0.07 times [rats] the MRHD on a mg/m
2basis, respectively).
Mutagenesis
Indomethacin did not have any mutagenic effect in in vitrobacterial tests and
a series of in vivotests including the host-mediated assay, sex-linked
recessive lethals in Drosophila, and the micronucleus test in mice.
Impairment of Fertility
Indomethacin at dosage levels up to 0.5 mg/kg/day had no effect on fertility
in mice in a two generation reproduction study (0.01 times the MRHD on a mg/m
2basis) or a two litter reproduction study in rats (0.02 times the MRHD on a
mg/m 2basis).
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
Indomethacin has been shown to be an effective anti-inflammatory agent,
appropriate for long- term use in rheumatoid arthritis, ankylosing
spondylitis, and osteoarthritis.
Indomethacin affords relief of symptoms; it does not alter the progressive
course of the underlying disease.
Indomethacin suppresses inflammation in rheumatoid arthritis as demonstrated
by relief of pain, and reduction of fever, swelling and tenderness.
Improvement in patients treated with indomethacin for rheumatoid arthritis has
been demonstrated by a reduction in joint swelling, average number of joints
involved, and morning stiffness; by increased mobility as demonstrated by a
decrease in walking time; and by improved functional capability as
demonstrated by an increase in grip strength. Indomethacin may enable the
reduction of steroid dosage in patients receiving steroids for the more severe
forms of rheumatoid arthritis. In such instances the steroid dosage should be
reduced slowly and the patients followed very closely for any possible adverse
effects.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Indomethacin suppositories USP, 50 mg each, are white to off-white, bullet shaped suppository packed in Alu/PE molds.
Boxes of 30 Suppositories NDC 31722-051-31
Storage
Store at 2° to 8°C (36° to 46°F).
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication
Guide) that accompanies each prescription dispensed. Inform patients,
families, or their caregivers of the following information before initiating
therapy with indomethacin suppositories and periodically during the course of
ongoing therapy. Indomethacin suppositories are for rectal use only. Advise
patients not to use indomethacin suppositories orally or intra-vaginally.
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic
events, including chest pain, shortness of breath, weakness, or slurring of
speech, and to report any of these symptoms to their health care provider
immediately [ see Warnings and Precautions ( 5.1) ].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including
epigastric pain, dyspepsia, melena, and hematemesis to their health care
provider. In the setting of concomitant use of low-dose aspirin for cardiac
prophylaxis, inform patients of the increased risk for and the signs and
symptoms of GI bleeding [ see Warnings and Precautions ( 5.2) ].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g.,
nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant
tenderness, and “flu-like” symptoms). If these occur, instruct patients to
stop indomethacin suppositories and seek immediate medical therapy [ see Warnings and Precautions ( 5.3) ].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure
including shortness of breath, unexplained weight gain, or edema and to
contact their healthcare provider if such symptoms occur [ see Warnings and Precautions ( 5.5) ].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty
breathing, swelling of the face or throat). Instruct patients to seek
immediate emergency help if these occur [ see Contraindications ( 4) and Warnings and Precautions ( 5.7) ].
Serious Skin Reactions, including DRESS
Advise patients to stop taking indomethacin suppositories immediately if they
develop any type of rash or fever and to contact their healthcare provider as
soon as possible [ see Warnings and Precautions ( 5.9, 5.10) ].
Female Fertility
Advise females of reproductive potential who desire pregnancy that NSAIDs,
including indomethacin, may be associated with a reversible delay in ovulation
[ see Use in Specific Populations ( 8.3) ].
Fetal Toxicity
Inform pregnant women to avoid use of indomethacin suppositories and other
NSAIDs starting at 30 weeks gestation because of the risk of the premature
closing of the fetal ductus arteriosus. If treatment with indomethacin
suppositories is needed for a pregnant woman between about 20 to 30 weeks
gestation, advise her that she may need to be monitored for oligohydramnios,
if treatment continues for longer than 48 hours [see Warnings and Precautions ( 5.11) and Use in Specific Populations ( 8.1) ].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of indomethacin suppositories with
other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended
due to the increased risk of gastrointestinal toxicity, and little or no
increase in efficacy [see Warnings and Precautions ( 5.2) and Drug Interactions ( 7) ]. Alert patients that NSAIDs may be present in “over the
counter” medications for treatment of colds, fever, or insomnia.
Use of NSAIDs and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with indomethacin
suppositories until they talk to their healthcare provider [ see Drug Interactions ( 7) ].

Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854.
By: Annora Pharma Pvt. Ltd.
Sangareddy - 502313, Telangana, India.
Revised: 09/2025
SPL UNCLASSIFIED SECTION
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
|
What is the most important information I should know about medicines called
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)? |
|
What are NSAIDs? |
|
Who should not take NSAIDs? |
|
Before taking NSAIDs, tell your healthcare provider about all of your
medical conditions, including if you: |
|
What are the possible side effects of NSAIDs? |
|
Other information about NSAIDs |
|
General information about the safe and effective use of NSAIDs |
|
By: Annora Pharma Pvt. Ltd. For more information, call Annora Pharma Private Limited at 1-866-495-1995. |
This Medication Guide has been approved by the U.S. Food and Drug
Administration.
Revised: 09/2025
