Dutasteride
These highlights do not include all the information needed to use DUTASTERIDE CAPSULES safely and effectively. See full prescribing information for DUTASTERIDE CAPSULES. DUTASTERIDE capsules for oral use Initial U.S. Approval: 2001
b32611f3-50ec-45bb-a671-ea10cec7829d
HUMAN PRESCRIPTION DRUG LABEL
Jan 3, 2023
Aurobindo Pharma Limited
DUNS: 650082092
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Dutasteride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (13)
Drug Labeling Information
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Monotherapy
Dutasteride capsules are indicated for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to:
- improve symptoms,
- reduce the risk of acute urinary retention (AUR), and
- reduce the risk of the need for BPH-related surgery.
1.2 Combination with Alpha-adrenergic Antagonist
Dutasteride capsules in combination with the alpha-adrenergic antagonist, tamsulosin, are indicated for the treatment of symptomatic BPH in men with an enlarged prostate.
1.3 Limitations of Use
Dutasteride capsules are not approved for the prevention of prostate cancer.
Dutasteride capsules are a 5 alpha-reductase inhibitor indicated for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to: (1.1)
- improve symptoms,
- reduce the risk of acute urinary retention, and
- reduce the risk of the need for BPH-related surgery.
Dutasteride in combination with the alpha-adrenergic antagonist, tamsulosin, is indicated for the treatment of symptomatic BPH in men with an enlarged prostate. (1.2)
Limitations of Use: Dutasteride capsules are not approved for the prevention of prostate cancer. (1.3)
DESCRIPTION SECTION
11 DESCRIPTION
Dutasteride is a synthetic 4-azasteroid compound that is a selective inhibitor of both the type 1 and type 2 isoforms of steroid 5 alpha-reductase, an intracellular enzyme that converts testosterone to DHT.
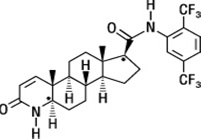
Dutasteride is chemically designated as (5α,17β)-N-{2,5 bis(trifluoromethyl)phenyl}-3-oxo-4-azaandrost-1-ene-17-carboxamide. The molecular formula of dutasteride is C27H30F6N2O2, representing a molecular weight of 528.5 with the following structural formula:
Dutasteride USP is a white to pale yellow powder with a melting point of 242° to 250°C. It is soluble in ethanol (44 mg/mL), methanol (64 mg/mL), and polyethylene glycol 400 (3 mg/mL), but it is insoluble in water.
Each dutasteride capsule, administered orally, contains 0.5 mg of dutasteride USP dissolved in a mixture of mono-di-glycerides of caprylic/capric acid and butylated hydroxytoluene. The inactive excipients in the capsule shell are gelatin (from certified BSE-free bovine sources), glycerin, medium chain triglycerides, opatint white (contains glycerin and titanium dioxide), opatint yellow (contains ferric oxide yellow and glycerin), and soy lecithin. The soft gelatin capsules are printed with edible red ink, opacode red.
The printing ink contains ferric oxide red, isopropyl alcohol, propylene glycol, and simethicone.
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Dutasteride is contraindicated for use in pregnancy because it may cause harm to the male fetus [see Contraindications (4)]. Dutasteride is not indicated for use in women.
Dutasteride is a 5 alpha-reductase inhibitor that prevents conversion of testosterone to dihydrotestosterone (DHT), a hormone necessary for normal development of male genitalia. Abnormalities in the genitalia of male fetuses is an expected physiological consequence of inhibition of this conversion. These results are similar to observations in male infants with genetic 5 alpha-reductase deficiency.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
In animal reproduction studies, dutasteride inhibited normal development of external genitalia in male offspring when given to rats or rabbits during organogenesis at less than the maximum recommended human dose (MRHD) of 0.5 mg daily, in the absence of maternal toxicity. At 15 times the MRHD, prolonged pregnancy, decreased reproductive organ weights, and delayed puberty in male offspring were observed in rats, with no-effect levels less than the MRHD of 0.5 mg daily. Increased placental weights in rabbits were also observed, with no-effect levels less than the MRHD of 0.5 mg daily (see Data).
Although dutasteride is secreted into human semen, the drug concentration in the human female partner is approximately 100 times less than concentrations producing abnormalities of male genitalia in animal studies (see Data). In monkeys dosed during organogenesis at blood concentrations comparable to or above levels to which a human female partner is estimated to be exposed, male offspring external genitalia was not adversely affected. No feminization occurred in male offspring of untreated female rats mated to treated male rats even though detectable blood levels of dutasteride were observed in the female rats [see Nonclinical Toxicology (13.1)].
Data
Human Data: The highest measured semen concentration of dutasteride in treated men was 14 ng/mL. Although dutasteride is detected in semen, assuming exposure of a 50 kg woman to 5 mL of semen and 100% absorption, the woman’s expected dutasteride blood concentration through semen would be about 0.0175 ng/mL. This concentration is approximately 100 times less than blood concentrations producing abnormalities of male genitalia in animal studies. Dutasteride is highly protein bound in human semen (greater than 96%), which may reduce the amount of dutasteride available for vaginal absorption.
Animal Data: In an embryo-fetal development study in rats, oral administration of dutasteride at 10 times less than the MRHD of 0.5 mg daily (based on average blood levels in men) resulted in feminization of male genitalia in the fetus (decreased anogenital distance at 0.05 mg/kg/day, with a lack of a no- effect level) in the absence of maternal toxicity. In addition, nipple development, hypospadias, and distended preputial glands occurred in fetuses of dams treated at doses of 2.5 mg/kg/day or greater (approximately 15 times the MRHD). Reduced fetal body weight and associated delayed ossification in the presence of maternal toxicity (decreased body weight gain) were observed at maternal exposure approximately 15 times the MRHD (dose of 2.5 mg/kg/day or greater). An increase in stillborn pups was observed in dams treated at 30 mg/kg/day (approximately 111 times the MRHD), with a no-effect level of 12.5 mg/kg/day.
In a rabbit embryo-fetal development study, doses 28 times the MRHD (doses of 30 mg/kg/day or greater), based on average blood levels in men, were administered orally on Gestation Days 7 to 29 (during organogenesis and the late period of external genitalia development). Histological evaluation of the genital papilla of fetuses revealed evidence of feminization of the male fetus as well as fused skull bones and increased placental weights at all doses in the absence of maternal toxicity. A second embryo-fetal development study in rabbits dosed throughout pregnancy (organogenesis and later period of external genitalia development [Gestation Days 6 to 29]) at 0.3 times the MRHD (doses of 0.05 mg/kg/day or greater, with no no-effect level), also produced evidence of feminization of the genitalia in male fetuses and increased placental weights at all doses in the absence of maternal toxicity.
In an embryo-fetal development study, pregnant rhesus monkeys were exposed intravenously during organogenesis (Gestation Days 20 to 100) to a dutasteride blood level comparable to or above the estimated dutasteride exposure of a human female partner. Dutasteride was administered on Gestation Days 20 to 100 (during organogenesis) at doses of 400, 780, 1,325, or 2,010 ng/day (12 monkeys/group). No feminization of male external genitalia of monkey offspring was observed. Reduction of fetal adrenal weights, reduction in fetal prostate weights, and increases in fetal ovarian and testis weights were observed at the highest dose tested. Based on the highest measured semen concentration of dutasteride in treated men (14 ng/mL), these doses in the monkey represent up to 16 times the potential maximum exposure of a 50 kg human female to 5 mL of semen daily from a dutasteride-treated male, assuming 100% absorption. The dose levels (on a ng/kg basis) administered to monkeys in this study are 32 to 186 times the nominal (ng/kg) dose to which a female would potentially be exposed via the semen. It is not known whether rabbits or rhesus monkeys produce any of the major human metabolites.
In an oral pre- and post-natal development study in rats, feminization of the male genitalia was observed. Decreased anogenital distance was observed at 0.05 times the MRHD and greater (0.05 mg/kg/day and greater), with a lack of a no-effect level, based on average blood levels in men as an estimation of AUC. Hypospadias and nipple development were observed at 2.5 mg/kg/day or greater (14 times the MRHD or greater, with a no-effect level at 0.05 mg/kg/day). Doses of 2.5 mg/kg/day and greater also resulted in prolonged gestation in the parental females, an increase in time to balano-preputial separation in male offspring, a decrease in time to vaginal patency for female offspring, and a decrease in prostate and seminal vesicle weights in male offspring. Increased stillbirths and decreased neonatal viability in offspring were noted at 30 mg/kg/day (102 times the MRHD in the presence of maternal toxicity [decreased body weights]).
8.2 Lactation
Risk Summary
Dutasteride is not indicated for use in women. There is no information available on the presence of dutasteride in human milk, the effects on the breastfed child, or the effects on milk production.
8.3 Females and Males of Reproductive Potential
Infertility
Males: The effects of dutasteride 0.5 mg/day on semen characteristics were evaluated in normal volunteers aged 18 to 52 years (n = 27 dutasteride, n = 23 placebo) throughout 52 weeks of treatment and 24 weeks of post-treatment follow-up. At 52 weeks, the mean percent reductions from baseline in total sperm count, semen volume, and sperm motility were 23%, 26%, and 18%, respectively, in the dutasteride group when adjusted for changes from baseline in the placebo group. Sperm concentration and sperm morphology were unaffected. After 24 weeks of follow-up, the mean percent change in total sperm count in the dutasteride group remained 23% lower than baseline. While mean values for all semen parameters at all timepoints remained within the normal ranges and did not meet predefined criteria for a clinically significant change (30%), 2 subjects in the dutasteride group had decreases in sperm count of greater than 90% from baseline at 52 weeks, with partial recovery at the 24-week follow-up. The clinical significance of dutasteride’s effect on semen characteristics for an individual patient’s fertility is not known [see Warnings and Precautions (5.6)].
8.4 Pediatric Use
Dutasteride is not indicated for use in pediatric patients. Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Of 2,167 male subjects treated with dutasteride in 3 clinical trials, 60% were aged 65 years and older and 15% were aged 75 years and older. No overall differences in safety or efficacy were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
No dose adjustment is necessary for dutasteride in patients with renal impairment [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
The effect of hepatic impairment on dutasteride pharmacokinetics has not been studied. Because dutasteride is extensively metabolized, exposure could be higher in hepatically impaired patients. However, in a clinical trial where 60 subjects received 5 mg (10 times the therapeutic dose) daily for 24 weeks, no additional adverse events were observed compared with those observed at the therapeutic dose of 0.5 mg [see Clinical Pharmacology (12.3)].
