Bupropion Hydrochloride
These highlights do not include all the information needed to use BUPROPION HYDROCHLORIDE EXTENDED-RELEASE TABLETS (XL) safely and effectively. See full prescribing information for BUPROPION HYDROCHLORIDE EXTENDED-RELEASE TABLETS (XL). BUPROPION HYDROCHLORIDE extended-release tablets (XL), for oral use<BR>Initial U.S. Approval: 1985
f0ace3e1-9823-41a0-9fd7-81979c840a65
HUMAN PRESCRIPTION DRUG LABEL
Dec 29, 2022
Wockhardt USA LLC.
DUNS: 170508365
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Bupropion Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (18)
Bupropion Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (18)
Drug Labeling Information
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 General Instructions for Use
To minimize the risk of seizure, increase the dose gradually [ see Warnings and Precautions (5.3)].
Bupropion hydrochloride extended-release tablets, USP (XL) should be swallowed whole and not crushed, divided, or chewed.
Bupropion hydrochloride extended-release tablets, USP (XL) should be administered in the morning and may be taken with or without food.
2.2 Dosage for Major Depressive Disorder (MDD)
The recommended starting dose for MDD is 150 mg once daily in the morning. After 4 days of dosing, the dose may be increased to the target dose of 300 mg once daily in the morning.
It is generally agreed that acute episodes of depression require several months or longer of antidepressant treatment beyond the response in the acute episode. It is unknown whether the bupropion hydrochloride extended-release tablets, USP (XL) dose needed for maintenance treatment is identical to the dose that provided an initial response. Periodically reassess the need for maintenance treatment and the appropriate dose for such treatment.
2.3 Dosage for Seasonal Affective Disorder (SAD)
The recommended starting dose for SAD is 150 mg once daily. After 7 days of dosing, the dose may be increased to the target dose of 300 mg once daily in the morning. Doses above 300 mg of bupropion hydrochloride extended-release were not assessed in the SAD trials.
For the prevention of seasonal MDD episodes associated with SAD, initiate bupropion hydrochloride extended-release tablets, USP (XL) in the autumn, prior to the onset of depressive symptoms. Continue treatment through the winter season. Taper and discontinue bupropion hydrochloride extended-release tablets, USP (XL) in early spring. For patients treated with 300 mg per day, decrease the dose to 150 mg once daily before discontinuing bupropion hydrochloride extended-release tablets, USP (XL). Individualize the timing of initiation, and duration of treatment should be individualized, based on the patient's historical pattern of seasonal MDD episodes.
2.4 Switching Patients from WELLBUTRIN (bupropion hydrochloride tablets) or
from WELLBUTRIN SR (bupropion hydrochloride extended-release tablets (SR))
When switching patients from WELLBUTRIN (bupropion hydrochloride tablets) to bupropion hydrochloride extended-release tablets (XL) or from WELLBUTRIN SR (bupropion hydrochloride extended-release tablets (SR)) to bupropion hydrochloride extended-release tablets, USP (XL), give the same total daily dose when possible.
2.5 To Discontinue Bupropion Hydrochloride Extended-Release Tablets, USP
(XL), Taper the Dose
When discontinuing treatment in patients treated with bupropion hydrochloride extended-release tablets, USP (XL) 300 mg once daily, decrease the dose to 150 mg once daily prior to discontinuation.
2.6 Dosage Adjustment in Patients with Hepatic Impairment
In patients with moderate to severe hepatic impairment (Child-Pugh score: 7 to 15), the maximum dose is150 mg every other day. In patients with mild hepatic impairment (Child-Pugh score: 5 to 6), consider reducing the dose and/or frequency of dosing [ see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
2.7 Dose Adjustment in Patients with Renal Impairment
Consider reducing the dose and/or frequency of bupropion hydrochloride extended-release tablets, USP (XL) in patients with renal impairment (glomerular filtration rate less than 90 mL/min) [ see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.8 Switching a Patient to or from a Monoamine Oxidase Inhibitor (MAOI)
Antidepressant
At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of therapy with bupropion hydrochloride extended-release tablets, USP (XL). Conversely, at least 14 days should be allowed after stopping bupropion hydrochloride extended-release tablets, USP (XL) before starting an MAOI antidepressant [ see Contraindications (4) and Drug Interactions (7.6)].
2.9 Use of Bupropion Hydrochloride Extended-Release Tablets, USP (XL) with
Reversible MAOIs such as Linezolid or Methylene Blue
Do not start bupropion hydrochloride extended-release tablets (XL) in a patient who is being treated with a reversible MAOI such as linezolid or intravenous methylene blue. Drug interactions can increase risk of hypertensive reactions. In a patient who requires more urgent treatment of a psychiatric condition, non-pharmacological interventions, including hospitalization, should be considered [ see Contraindications (4)].
In some cases, a patient already receiving therapy with bupropion hydrochloride extended-release tablets, USP (XL) may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of hypertensive reactions in a particular patient, bupropion hydrochloride extended-release tablets, USP (XL) should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with bupropion hydrochloride extended-release tablets, USP (XL) may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue.
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg per kg with bupropion hydrochloride extended-release tablets, USP (XL) is unclear. The clinician should, nevertheless, be aware of the possibility of a drug interaction with such use [ see Contraindications (4) and Drug Interactions (7.6)].
General:
- Increase dose gradually to reduce seizure risk. ( 2.1, 5.3)
- Periodically reassess the dose and need for maintenance treatment. ( 2.2)
Major Depressive Disorder
- Starting dose: 150 mg once daily. Usual target dose: 300 mg once daily ( 2.2)
- After 4 days,may increase the dose to 300 mg once daily. ( 2.2)
Seasonal Affective Disorder
- Initiate treatment in the autumn prior to onset of seasonal depressive symptoms. ( 2.3)
- Starting dose: 150 mg once daily. Usual target dose: 300 mg once daily. ( 2.3)
- After one week, may increase the dose to 300 mg once daily. ( 2.3)
- Continue treatment through the winter season. ( 2.3)
Hepatic Impairment
- Moderate to severe hepatic impairment: 150 mg every other day ( 2.6)
- Mild hepatic impairment: Consider reducing the dose and/or frequency of dosing. ( 2.6, 8.7)
Renal Impairment
- Consider reducing the dose and/or frequency of dosing. ( 2.7, 8.6)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antidepressants during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or visiting online at https://womensmentalhealth.org/clinical-and-research- programs/pregnancyregistry/ antidepressants/.
Risk Summary
Data from epidemiological studies of pregnant women exposed to bupropion in the first trimester have not identified an increased risk of congenital malformations overall (see Data). There are risks to the mother associated with untreated depression (see Clinical Considerations). When bupropion was administered to pregnant rats during organogenesis, there was no evidence of fetal malformations at doses up to approximately 10 times the maximum recommended human dose (MRHD) of 450 mg/day. When given to pregnant rabbits during organogenesis, non-dose-related increases in incidence of fetal malformations and skeletal variations were observed at doses approximately equal to the MRHD and greater. Decreased fetal weights were seen at doses twice the MRHD and greater (see Animal Data) .
The estimated background risk for major birth defects and miscarriage are unknown for the indicated population. All pregnancies have a background rate of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
A prospective, longitudinal study followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants during pregnancy at the beginning of pregnancy. The women who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressants. Consider the risks to the mother of untreated depression and potential effects on the fetus when discontinuing or changing treatment with antidepressant medications during pregnancy and postpartum.
Data
Human Data
Data from the international bupropion Pregnancy Registry (675 first trimester exposures) and a retrospective cohort study using the United Healthcare database (1,213 first trimester exposures) did not show an increased risk for malformations overall. The Registry was not designed or powered to evaluate specific defects but suggested a possible increase in cardiac malformations.
No increased risk for cardiovascular malformations overall has been observed after bupropion exposure during the first trimester. The prospectively observed rate of cardiovascular malformations in pregnancies with exposure to bupropion in the first trimester from the international Pregnancy Registry was 1.3% (9 cardiovascular malformations/675 first-trimester maternal bupropion exposures), which is similar to the background rate of cardiovascular malformations (approximately 1%). Data from the United Healthcare database, which has a limited number of exposed cases with cardiovascular malformations, and a case-controlled study (6,853 infants with cardiovascular malformations and 5,753 with non-cardiovascular malformations) from the National Birth Defects Prevention Study (NBDPS) did not show an increased risk for cardiovascular malformations overall after bupropion exposure during the first trimester.
Study findings on bupropion exposure during the first trimester and risk left ventricular outflow tract obstruction (LVOTO) are inconsistent and do not allow conclusions regarding possible association. The United Healthcare database lacked sufficient power to evaluate this association; the NBDPS found increased risk for LVOTO (n = 10; adjusted odds ratio (OR) = 2.6; 95% CI 1.2, 5.7), and the Slone Epidemiology case control study did not find increased risk for LVOTO.
Study findings on bupropion exposure during the first trimester and risk for ventricular septal defect (VSD) are inconsistent and do not allow conclusions regarding a possible association. The Slone Epidemiology Study found an increased risk for VSD following first trimester maternal bupropion exposure (n = 17; adjusted OR = 2.5; 95% CI: 1.3, 5.0) but did not find an increased risk for any other cardiovascular malformations studied (including LVOTO as above). The NBDPS and United Healthcare database study did not find an association between first trimester maternal bupropion exposure and VSD.
For the findings of LVOTO and VSD, the studies were limited by the small number of exposed cases, inconsistent findings among studies, and the potential for chance findings from multiple comparisons in case control studies.
Animal Data
In studies conducted in pregnant rats and rabbits, bupropion was administered orally during the period of organogenesis at doses of up to 450 and 150 mg/kg/day, respectively (approximately 10 and 6 times the MRHD, respectively, on a mg/m 2 basis). There was no evidence of fetal malformations in rats. When given to pregnant rabbits during organogenesis, non-dose-related increases in incidence of fetal malformations and skeletal variations were observed at the lowest dose tested (25 mg/kg/day, approximately equal to the MRHD on a mg/m 2 basis) and greater. Decreased fetal weights were observed at doses of 50 mg/kg/day (approximately 2 times the MRHD on a mg/m 2 basis) and greater. No maternal toxicity was evident at doses of 50 mg/kg/day or less.
In a pre- and postnatal development study, bupropion administered orally to pregnant rats at doses of up to 150 mg/kg/day (approximately 3 times the MRHD on a mg/m 2 basis) from embryonic implantation through lactation had no effect on pup growth or development.
8.2 Lactation
Risk Summary
Data from published literature report the presence of bupropion and its metabolites in human milk (see Data). There are no data on the effects of bupropion or its metabolites on milk production. Limited data from postmarketing reports have not identified a clear association of adverse reactions in the breastfed infant. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for bupropion hydrochloride extended-release tablets (XL) and any potential adverse effects on the breastfed child from bupropion hydrochloride extended- release tablets (XL) or from the underlying maternal condition.
Data
In a lactation study of ten women, levels of orally dosed bupropion and its active metabolites were measured in expressed milk. The average daily infant exposure (assuming 150 mL/kg daily consumption) to bupropion and its active metabolites was 2% of the maternal weight-adjusted dose. Postmarketing reports have described seizures in breastfed infants. The relationship of bupropion exposure and these seizures is unclear.
8.4 Pediatric Use
Safety and effectiveness in the pediatric population have not been established. When considering the use of bupropion hydrochloride extended- release tablets (XL) in a child or adolescent, balance the potential risks with the clinical need [ see Boxed Warning and Warnings and Precautions (5.1)].
8.5 Geriatric Use
Of the approximately 6000 patients who participated in clinical trials with bupropion hydrochloride sustained-release tablets (depression and smoking cessation studies), 275 were ≥65 years old and 47 were ≥75 years old. In addition, several hundred patients ≥65 years of age participated in clinical trials using the immediate-release formulation of bupropion hydrochloride (depression studies). No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and excreted by the kidneys. The risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, it may be necessary to consider this factor in dose selection; it may be useful to monitor renal function [ see Dosage and Administration (2.7), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Consider a reduced dose and/or dosing frequency of bupropion hydrochloride extended-release tablets (XL) in patients with renal impairment (glomerular filtration rate: <90 mL/min). Bupropion and its metabolites are cleared renally and may accumulate in such patients to a greater extent than usual. Monitor closely for adverse reactions that could indicate high bupropion or metabolite exposures [ see Dosage and Administration (2.7) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
In patients with moderate to severe hepatic impairment (Child-Pugh score: 7 to 15), the maximum bupropion hydrochloride extended-release tablets (XL) dose is 150 mg every other day. In patients with mild hepatic impairment (Child-Pugh score: 5 to 6), consider reducing the dose and/or frequency of dosing [ see Dosage and Administration (2.6) and Clinical Pharmacology (12.3)].
DESCRIPTION SECTION
11 DESCRIPTION
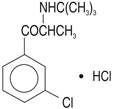
Bupropion hydrochloride, USP, an antidepressant of the aminoketone class, is chemically unrelated to tricyclic, tetracyclic, selective serotonin reuptake inhibitor, or other known antidepressant agents. Its structure closely resembles that of diethylpropion; it is related to phenylethylamines. It is designated as (±)-1-(3-chorophenyl)-2-[(1,1-dimethylethyl)amino]-1-propanone hydrochloride. The molecular weight is 276.2. The molecular formula is C 13H 18ClNO·HCl. Bupropion hydrochloride powder is white, crystalline, and soluble in water, 0.1N HCl and in alcohol. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. The structural formula is:
Bupropion hydrochloride extended-release tablets, USP (XL) are supplied for oral administration as 150 mg and 300 mg white to off white extended-release tablets. Each tablet contains the labeled amount of bupropion hydrochloride and the inactive ingredients: ammonium chloride, colloidal silicon dioxide, ethyl cellulose, eudragit L30D55, glyceryl behenate, iron oxide black, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, propylene glycol, silicon dioxide, shellac glaze, talc, titanium dioxide, triethyl citrate. The tablets are printed with edible black ink.
The insoluble shell of the extended-release tablet may remain intact during gastrointestinal transit and is eliminated in the feces.
Meets USP Dissolution Test 16.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of bupropion is unknown, as is the case with other antidepressants. However, it is presumed that this action is mediated by noradrenergic and/or dopaminergic mechanisms. Bupropion is a relatively weak inhibitor of the neuronal uptake of norepinephrine and dopamine and does not inhibit monoamine oxidase or the reuptake of serotonin.
12.3 Pharmacokinetics
Bupropion is a racemic mixture. The pharmacologic activity and pharmacokinetics of the individual enantiomers have not been studied.
Following chronic dosing, the mean steady-state plasma concentration of bupropion was reached within 8 days. The mean elimination half-life (±SD) of bupropion is 21 (±9) hours.
In a study comparing 14-day dosing with bupropion hydrochloride extended- release tablets (XL), 300 mg once-daily to the immediate-release formulation of bupropion at 100 mg 3 times daily, equivalence was demonstrated for peak plasma concentration and area under the curve for bupropion and the three metabolites (hydroxybupropion, threohydrobupropion, and erythrohydrobupropion). Additionally, in a study comparing 14-day dosing with bupropion hydrochloride extended-release tablets (XL) 300 mg once daily to the sustained-release formulation of bupropion at 150 mg 2 times daily, equivalence was demonstrated for peak plasma concentration and area under the curve for bupropion and the three metabolites.
Absorption
Following single oral administration of bupropion hydrochloride extended- release tablets (XL) tablets to healthy volunteers, the median time to peak plasma concentrations for bupropion was approximately 5 hours. The presence of food did not affect the peak concentration or area under the curve of bupropion.
Distribution
In vitro tests show that bupropion is 84% bound to human plasma proteins at concentrations up to 200 mcg/mL. The extent of protein binding of the hydroxybupropion metabolite is similar to that for bupropion, whereas the extent of protein binding of the threohydrobupropion metabolite is about half that of bupropion.
Metabolism
Bupropion is extensively metabolized in humans. Three metabolites are active: hydroxybupropion, which is formed via hydroxylation of the tert-butyl group of bupropion, and the amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, which are formed via reduction of the carbonyl group. In vitro findings suggest that CYP2B6 is the principal isoenzyme involved in the formation of hydroxybupropion, while cytochrome P450 enzymes are not involved in the formation of threohydrobupropion. Oxidation of the bupropion side chain results in the formation of a glycine conjugate of meta- chlorobenzoic acid, which is then excreted as the major urinary metabolite. The potency and toxicity of the metabolites relative to bupropion have not been fully characterized. However, it has been demonstrated in an antidepressant screening test in mice that hydroxybupropion is one half as potent as bupropion, while threohydrobupropion and erythrohydrobupropion are 5-fold less potent than bupropion. This may be of clinical importance, because the plasma concentrations of the metabolites are as high or higher than those of bupropion.
At steady state, peak plasma concentration of hydroxybupropion occurred approximately 7 hours after administration of bupropion hydrochloride extended-release tablets (XL), and it was approximately 7 times the peak level of the parent drug. The elimination half-life of hydroxybupropion is approximately 20 (±5) hours, and its AUC at steady state is about 13 times that of bupropion. The times to peak concentrations for the erythrohydrobupropion and threohydrobupropion metabolites are similar to that of hydroxybupropion. However, the elimination half-lives of erythrohydrobupropion and threohydrobupropion are longer, approximately 33 (±10) and 37 (±13) hours, respectively, and steady-state AUCs were 1.4 and 7 times that of bupropion, respectively.
Bupropion and its metabolites exhibit linear kinetics following chronic administration of 300 to 450 mg/day.
Elimination
Following oral administration of 200 mg of 14C-bupropion in humans, 87% and 10% of the radioactive dose were recovered in the urine and feces, respectively. Only 0.5% of the oral dose was excreted as unchanged bupropion.
Population Subgroups
Factors or conditions altering metabolic capacity (e.g., liver disease, congestive heart failure [CHF], age, concomitant medications, etc.) or elimination may be expected to influence the degree and extent of accumulation of the active metabolites of bupropion. The elimination of the major metabolites of bupropion may be affected by reduced renal or hepatic function, because they are moderately polar compounds and are likely to undergo further metabolism or conjugation in the liver prior to urinary excretion.
Renal Impairment
There is limited information on the pharmacokinetics of bupropion in patients with renal impairment. An inter-trial comparison between normal subjects and subjects with end-stage renal failure demonstrated that the parent drug C max and AUC values were comparable in the 2 groups, whereas the hydroxybupropion and threohydrobupropion metabolites had a 2.3- and 2.8-fold increase, respectively, in AUC for subjects with end-stage renal failure. A second study, comparing normal subjects and subjects with moderate-to-severe renal impairment (GFR 30.9 ± 10.8 mL/min) showed that after a single 150 mg dose of sustained-release bupropion, exposure to bupropion was approximately 2-fold higher in subjects with impaired renal function, while levels of the hydroxybupropion and threo/erythrohydrobupropion (combined) metabolites were similar in the 2 groups. Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and subsequently excreted by the kidneys. The elimination of the major metabolites of bupropion may be reduced by impaired renal function. Bupropion hydrochloride extended-release tablets (XL) should be used with caution in patients with renal impairment, and a reduced frequency and/or dose should be considered [ see Dosage and Administration (2.7) and Use in Specific Populations (8.6)].
Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of bupropion was characterized in 2 single-dose trials, one in subjects with alcoholic liver disease and one in subjects with mild to severe cirrhosis. The first trial demonstrated that the half-life of hydroxybupropion was significantly longer in 8 subjects with alcoholic liver disease than in 8 healthy volunteers (32±14 hours versus 21±5 hours, respectively). Although not statistically significant, the AUCs for bupropion and hydroxybupropion were more variable and tended to be greater (by 53% to 57%) in patients with alcoholic liver disease. The differences in half-life for bupropion and the other metabolites in the 2 groups were minimal.
The second trial demonstrated no statistically significant differences in the pharmacokinetics of bupropion and its active metabolites in 9 subjects with mild to moderate hepatic cirrhosis compared to 8 healthy volunteers. However, more variability was observed in some of the pharmacokinetic parameters for bupropion (AUC, C max, and T max) and its active metabolites (t ½) in subjects with mild to moderate hepatic cirrhosis. In addition, in patients with severe hepatic cirrhosis, the bupropion C max and AUC were substantially increased (mean difference: by approximately 70% and 3-fold, respectively) and more variable when compared to values in healthy volunteers; the mean bupropion half-life was also longer (29 hours in subjects with severe hepatic cirrhosis vs. 19 hours in healthy subjects). For the metabolite hydroxybupropion, the mean C max was approximately 69% lower. For the combined amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, the mean C max was approximately 31% lower. The mean AUC increased by about 1½-fold for hydroxybupropion and about 2½-fold for threo/erythrohydrobupropion. The median T max was observed 19 hours later for hydroxybupropion and 31 hours later for threo/erythrohydrobupropion. The mean half-lives for hydroxybupropion and threo/erythrohydrobupropion were increased 5- and 2-fold, respectively, in patients with severe hepatic cirrhosis compared to healthy volunteers [ see Dosage and Administration (2.6) and Use in Specific Populations (8.7)].
Left Ventricular Dysfunction
During a chronic dosing study with bupropion in 14 depressed patients with left ventricular dysfunction (history of CHF or an enlarged heart on x-ray), there was no apparent effect on the pharmacokinetics of bupropion or its metabolites, compared to healthy volunteers.
Age
The effects of age on the pharmacokinetics of bupropion and its metabolites have not been fully characterized, but an exploration of steady-state bupropion concentrations from several depression efficacy studies involving patients dosed in a range of 300 to 750 mg/day, on a 3 times daily schedule, revealed no relationship between age (18 to 83 years) and plasma concentration of bupropion. A single-dose pharmacokinetic study demonstrated that the disposition of bupropion and its metabolites in elderly subjects was similar to that in younger subjects. These data suggest that there is no prominent effect of age on bupropion concentration; however, another single- and multiple-dose pharmacokinetic study suggested that the elderly are at increased risk for accumulation of bupropion and its metabolites [ see Use in Specific Populations (8.5)].
Gender
A single-dose study involving 12 healthy male and 12 healthy female volunteers revealed no sex-related differences in the pharmacokinetic parameters of bupropion. In addition, pooled analysis of bupropion pharmacokinetic data from 90 healthy male and 90 healthy female volunteers revealed no sex-related differences in the peak plasma concentrations of bupropion. The mean systemic exposure (AUC) was approximately 13% higher in male volunteers compared to female volunteers.
Smokers
The effects of cigarette smoking on the pharmacokinetics of bupropion hydrochloride were studied in 34 healthy male and female volunteers; 17 were chronic cigarette smokers and 17 were nonsmokers. Following oral administration of a single 150 mg dose of bupropion, there was no statistically significant difference in C max, half-life, T max, AUC, or clearance of bupropion or its active metabolites between smokers and nonsmokers.
Drug Interactions
Potential for Other Drugs to Affect Bupropion Hydrochloride Extended-Release Tablets (XL)
In vitro studies indicate that bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between bupropion hydrochloride extended-release tablets (XL) and drugs that are inhibitors or inducers of CYP2B6. In addition, in vitro studies suggest that paroxetine, sertraline, norfluoxetine, fluvoxamine, and nelfinavir inhibit the hydroxylation of bupropion.
Inhibitors of CYP2B6
Ticlopidine and Clopidogrel: In a study in healthy male volunteers, clopidogrel 75 mg once daily or ticlopidine 250 mg twice daily increased exposures (C max and AUC) of bupropion by 40% and 60% for clopidogrel, by 38% and 85% for ticlopidine, respectively. The exposures of hydroxybupropion were decreased.
Prasugrel: In healthy subjects, prasugrel increased bupropion C max and AUC values by 14% and 18%, respectively, and decreased C max and AUC values of hydroxybupropion by 32% and 24%, respectively.
Cimetidine: Following oral administration of bupropion 300 mg with and without cimetidine 800 mg in 24 healthy young male volunteers, the pharmacokinetics of bupropion and hydroxybupropion were unaffected. However, there were 16% and 32% increases in the AUC and C max, respectively, of the combined moieties of threohydrobupropion and erythrohydrobupropion.
Citalopram: Citalopram did not affect the pharmacokinetics of bupropion and its three metabolites.
Inducers of CYP2B6
Ritonavir and Lopinavir: In a healthy volunteer study, ritonavir 100 mg twice daily reduced the AUC and C max of bupropion by 22% and 21%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 23%, the threohydrobupropion decreased by 38%, and the erythrohydrobupropion decreased by 48%. In a second healthy volunteer study, ritonavir 600 mg twice daily decreased the AUC and C max of bupropion by 66% and 62%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 78%, the threohydrobupropion decreased by 50%, and the erythrohydrobupropion decreased by 68%.
In another healthy volunteer study, lopinavir 400 mg/ritonavir 100 mg twice daily decreased bupropion AUC and C max by 57%. The AUC and C max of hydroxybupropion metabolite were decreased by 50% and 31%, respectively.
Efavirenz: In a study of healthy volunteers, efavirenz 600 mg once daily for 2 weeks reduced the AUC and C max of bupropion by approximately 55% and 34%, respectively. The AUC of hydroxybupropion was unchanged, whereas C max of hydroxybupropion was increased by 50%.
Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs may induce the metabolism of bupropion.
Potential for Bupropion Hydrochloride Extended-Release Tablets (XL) to Affect Other Drugs
Animal data indicated that bupropion may be an inducer of drug-metabolizing enzymes in humans. In a study of 8 healthy male volunteers, following a 14-day administration of bupropion 100 mg three times per day, there was no evidence of induction of its own metabolism. Nevertheless, there may be the potential for clinically important alterations of blood levels of coadministered drugs.
Drugs Metabolized by CYP2D6
In vitro, bupropion and hydroxybupropion are CYP2D6 inhibitors. In a clinical study of 15 male subjects (ages 19 to 35 years) who were extensive metabolizers of CYP2D6, bupropion given as 150 mg twice daily followed by a single dose of 50 mg desipramine increased the C max, AUC, and T ½ of desipramine by an average of approximately 2-, 5-, and 2-fold, respectively. The effect was present for at least 7 days after the last dose of bupropion. Concomitant use of bupropion with other drugs metabolized by CYP2D6 has not been formally studied.
Citalopram: Although citalopram is not primarily metabolized by CYP2D6, in one study bupropion increased the C max and AUC of citalopram by 30% and 40%, respectively.
Lamotrigine: Multiple oral doses of bupropion had no statistically significant effects on the single-dose pharmacokinetics of lamotrigine in 12 healthy volunteers.
