Levothyroxine sodium
These highlights do not include all the information needed to use LEVOTHYROXINE SODIUM TABLETS safely and effectively. See full prescribing information for LEVOTHYROXINE SODIUM TABLETS. LEVOTHYROXINE SODIUM tablets, for oral use Initial U.S. Approval: 2002
3453af75-8c2e-421f-9a08-24751936df41
HUMAN PRESCRIPTION DRUG LABEL
May 25, 2023
A-S Medication Solutions
DUNS: 830016429
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Levothyroxine Sodium
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Drug Labeling Information
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Serious Risks Related to Overtreatment or Undertreatment with
Levothyroxine Sodium Tablets
Levothyroxine sodium tablets has a narrow therapeutic index. Overtreatment or undertreatment with levothyroxine sodium tablets may have negative effects on growth and development, cardiovascular function, bone metabolism, reproductive function, cognitive function, gastrointestinal function, and glucose and lipid metabolism in adult or pediatric patients.
In pediatric patients with congenital and acquired hypothyroidism, undertreatment may adversely affect cognitive development and linear growth, and overtreatment is associated with craniosynostosis and acceleration of bone age [Use in Specific Populations (8.4)].
Titrate the dose of levothyroxine sodium tablets carefully and monitor response to titration to avoid these effects [see Dosage and Administration (2.4)]. Consider the potential for food or drug interactions and adjust the administration or dosage of levothyroxine sodium tablets as needed [see Dosage and Administration (2.1), Drug Interactions (7.1), and Clinical Pharmacology (12.3)].
5.2 Cardiac Adverse Reactions in the Elderly and in Patients with
Underlying Cardiovascular Disease
Over-treatment with levothyroxine may cause an increase in heart rate, cardiac wall thickness, and cardiac contractility and may precipitate angina or arrhythmias, particularly in patients with cardiovascular disease and in elderly patients. Initiate levothyroxine sodium therapy in this population at lower doses than those recommended in younger individuals or in patients without cardiac disease [see Dosage and Administration (2.3), Use in Specific Populations (8.5)] .
Monitor for cardiac arrhythmias during surgical procedures in patients with coronary artery disease receiving suppressive levothyroxine sodium therapy. Monitor patients receiving concomitant levothyroxine sodium and sympathomimetic agents for signs and symptoms of coronary insufficiency.
If cardiac symptoms develop or worsen, reduce the levothyroxine sodium tablets dose or withhold for one week and restart at a lower dose.
5.3 Myxedema Coma
Myxedema coma is a life-threatening emergency characterized by poor circulation and hypometabolism and may result in unpredictable absorption of levothyroxine sodium from the gastrointestinal tract. Use of oral thyroid hormone drug products is not recommended to treat myxedema coma. Administer thyroid hormone products formulated for intravenous administration to treat myxedema coma.
5.4 Acute Adrenal Crisis in Patients with Concomitant Adrenal Insufficiency
Thyroid hormone increases metabolic clearance of glucocorticoids. Initiation of thyroid hormone therapy prior to initiating glucocorticoid therapy may precipitate an acute adrenal crisis in patients with adrenal insufficiency. Treat patients with adrenal insufficiency with replacement glucocorticoids prior to initiating treatment with levothyroxine sodium [see Contraindications (4)] .
5.5 Worsening of Diabetic Control
Addition of levothyroxine therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control after starting, changing, or discontinuing levothyroxine sodium [see Drug Interactions (7.2)] .
5.6 Decreased Bone Mineral Density Associated with Thyroid Hormone Over-
Replacement
Increased bone resorption and decreased bone mineral density may occur as a result of levothyroxine over-replacement, particularly in post-menopausal women. The increased bone resorption may be associated with increased serum levels and urinary excretion of calcium and phosphorous, elevations in bone alkaline phosphatase, and suppressed serum parathyroid hormone levels. Administer the minimum dose of levothyroxine sodium that achieves the desired clinical and biochemical response to mitigate this risk.
5.7 Risk of Allergic Reactions Due to Tartrazine
This product contains FD&C Yellow No. 5 (tartrazine) which may cause allergic- type reactions (including bronchial asthma) in certain susceptible persons. Although the overall incidence of FD&C Yellow No. 5 (tartrazine) sensitivity in the general population is low, it is frequently seen in patients who also have aspirin hypersensitivity.
- Serious risks related to overtreatment or undertreatment with levothyroxine sodium tablets: Titrate the dose of levothyroxine sodium carefully and monitor response to titration. (5.1)
- Cardiac adverse reactions in the elderly and in patients with underlying cardiovascular disease: Initiate levothyroxine sodium at less than the full replacement dose because of the increased risk of cardiac adverse reactions, including atrial fibrillation. (2.3, 5.2, 8.5)
- Myxedema coma: Do not use oral thyroid hormone drug products to treat myxedema coma. (5.3)
- Acute adrenal crisis in patients with concomitant adrenal insufficiency: Treat with replacement glucocorticoids prior to initiation of levothyroxine sodium treatment. (5.4)
- Worsening of diabetic control: Therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control after starting, changing, or discontinuing thyroid hormone therapy. (5.5)
- Decreased bone mineral density associated with thyroid hormone over-replacement: Over-replacement can increase bone resorption and decrease bone mineral density. Give the lowest effective dose. (5.6)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
All tablets having functional scoring
Levothyroxine sodium tablets USP are available as follows (Table 4):
Table 4: Levothyroxine Sodium Tablet Strengths and Identifying Features|
Tablet Strength |
Tablet Description |
|
25 mcg |
Round shaped, Orange colored, uncoated tablets, break line on both side and debossed with "P" and "1" on one side and plain on other side. |
|
50 mcg |
Round shaped, White colored, uncoated tablets, break line on both side and debossed with "P" and "2" on one side and plain on other side. |
|
75 mcg |
Round shaped, Violet colored, uncoated tablets, break line on both side and debossed with "P" and "3" on one side and plain on other side. |
|
88 mcg |
Round shaped, Olive colored, uncoated tablets, break line on both side and debossed with "P" and "4" on one side and plain on other side. |
|
100 mcg |
Round shaped, Yellow colored, uncoated tablets, break line on both side and debossed with "P" and "14" on one side and plain on other side. |
|
112 mcg |
Round shaped, Rose colored, uncoated tablets, break line on both side and debossed with "P" and "6" on one side and plain on other side. |
|
125 mcg |
Round shaped, Brown colored, uncoated tablets, break line on both side and debossed with "P" and "7" on one side and plain on other side. |
|
137 mcg |
Round shaped, Turquoise colored, uncoated tablets, break line on both side and debossed with "P" and "8" on one side and plain on other side. |
|
150 mcg |
Round shaped, Blue colored, uncoated tablets, break line on both side and debossed with "P" and "9" on one side and plain on other side. |
|
175 mcg |
Round shaped, Lilac colored, uncoated tablets, break line on both side and debossed with "P" and "10" on one side and plain on other side. |
|
200 mcg |
Round shaped, Pink colored, uncoated tablets, break line on both side and debossed with "P" and "11" on one side and plain on other side. |
|
300 mcg |
Round shaped, Green colored, uncoated tablets, break line on both side and debossed with "P" and "12" on one side and plain on other side. |
Tablets (Functional Scoring): 25, 50, 75, 88, 100, 112, 125, 137, 150, 175, 200, and 300 mcg (3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The clinical experience, including data from postmarketing studies, in pregnant women treated with oral levothyroxine to maintain euthyroid state have not reported increased rates of major birth defects, miscarriages, or other adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with untreated hypothyroidism in pregnancy. Since TSH levels may increase during pregnancy, TSH should be monitored and levothyroxine sodium dosage adjusted during pregnancy (see Clinical Considerations). Animal reproductive studies have not been conducted with levothyroxine sodium. Levothyroxine sodium should not be discontinued during pregnancy and hypothyroidism diagnosed during pregnancy should be promptly treated.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Maternal hypothyroidism during pregnancy is associated with a higher rate of complications, including spontaneous abortion, gestational hypertension, pre‑eclampsia, stillbirth, and premature delivery. Untreated maternal hypothyroidism may have an adverse effect on fetal neurocognitive development.
Dose Adjustments During Pregnancy and the Postpartum Period
Pregnancy may increase levothyroxine sodium requirements. Serum TSH levels should be monitored and the levothyroxine sodium dosage adjusted during pregnancy. Since postpartum TSH levels are similar to preconception values, the levothyroxine sodium dosage should return to the pre-pregnancy dose immediately after delivery [see Dosage and Administration (2.3)].
8.2 Lactation
Risk Summary
Published studies report that levothyroxine is present in human milk following the administration of oral levothyroxine. No adverse effects on the breastfed infant have been reported there is no information on the effects of levothyroxine on milk production. Adequate levothyroxine treatment during lactation may normalize milk production in hypothyroid lactating mothers with low milk supply. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for levothyroxine sodium and any potential adverse effects on the breastfed infant from levothyroxine sodium or from the underlying maternal condition
8.4 Pediatric Use
Levothyroxine sodium is indicated in patients from birth to less than 17 years of age:
- As a replacement therapy in primary (thyroidal), secondary (pituitary), and tertiary (hypothalamic) congenital or acquired hypothyroidism.
- As an adjunct to surgery and radioiodine therapy in the management of thyrotropin-dependent well-differentiated thyroid cancer.
Rapid restoration of normal serum T4 concentrations is essential for preventing the adverse effects of congenital hypothyroidism on cognitive development as well as on overall physical growth and maturation. Therefore, initiate levothyroxine sodium therapy immediately upon diagnosis. Levothyroxine is generally continued for life in these patients [see Warnings and Precautions (5.1)].
Closely monitor infants during the first 2 weeks of levothyroxine sodium therapy for cardiac overload, arrhythmias.
8.5 Geriatric Use
Because of the increased prevalence of cardiovascular disease among the elderly, initiate levothyroxine sodium at less than the full replacement dose [see Dosage and Administration (2.3) and Warnings and Precautions (5.2)] . Atrial arrhythmias can occur in elderly patients. Atrial fibrillation is the most common of the arrhythmias observed with levothyroxine overtreatment in the elderly.
Pregnancy may require the use of higher doses of levothyroxine sodium. (2.3, 8.1)
OVERDOSAGE SECTION
10 OVERDOSAGE
The signs and symptoms of overdosage are those of hyperthyroidism [see Warnings and Precautions (5) and Adverse Reactions (6)] . In addition, confusion and disorientation may occur. Cerebral embolism, shock, coma, and death have been reported. Seizures occurred in a 3-year-old child ingesting 3.6 mg of levothyroxine. Symptoms may not necessarily be evident or may not appear until several days after ingestion of levothyroxine sodium.
Reduce the levothyroxine sodium dosage or discontinue temporarily if signs or symptoms of overdosage occur. Initiate appropriate supportive treatment as dictated by the patient’s medical status.
For current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
DESCRIPTION SECTION
11 DESCRIPTION
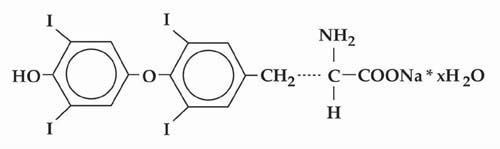
Levothyroxine sodium tablets, USP is L-thyroxine (T4) and contains synthetic crystalline L-3,3’,5,5’-tetraiodothyronine sodium salt. Synthetic T4 is chemically identical to that produced in the human thyroid gland. Levothyroxine (T4) sodium has an empirical formula of C 15H 10I 4N NaO 4• H 2O, molecular weight of 798.86 (anhydrous), and structural formula as shown:
Levothyroxine sodium tablets, USP for oral administration are supplied in the following strengths: 25 mcg, 50 mcg, 75 mcg, 88 mcg, 100 mcg, 112 mcg, 125 mcg, 137 mcg, 150 mcg, 175 mcg, 200 mcg, and 300 mcg. Each levothyroxine sodium tablet contains the inactive ingredients microcrystalline sodium, light magnesium oxide, sodium starch glycolate and sodium stearyl fumarate.
Levothyroxine sodium tablets, USP contain no ingredients made from a gluten- containing grain (wheat, barley, or rye). Table 9 provides a listing of the color additives by tablet strength:
Table 9. Levothyroxine Sodium Tablet Color Additives|
Strength |
Color additive(s) |
|
25 |
FD&C Yellow No. 6 Aluminum Lake |
|
50 |
None |
|
75 |
FD&C Red No. 40 Aluminum Lake, FD&C Blue No. 2 Aluminum Lake |
|
88 |
FD&C Blue No. 2 Aluminum Lake, FD&C Yellow No. 5 Aluminum Lake |
|
100 |
FD&C Yellow No. 5 Aluminum Lake, FD&C Yellow No. 6 Aluminum Lake |
|
112 |
FD&C Red No. 40 Aluminum Lake, Carmine |
|
125 |
FD&C Yellow No. 6 Aluminum Lake, FD&C Red No. 40 Aluminum Lake, FD&C Blue No. 1 Aluminum Lake |
|
137 |
FD&C Blue No. 1 Aluminum Lake |
|
150 |
FD&C Blue No. 2 Aluminum Lake |
|
175 |
FD&C Blue No. 1 Aluminum Lake, Carmine |
|
200 |
FD&C Red No. 40 Aluminum Lake |
|
300 |
D&C Yellow No. 10 Aluminum Lake, FD&C Yellow No. 6 Aluminum Lake, FD&C Blue No. 1 Aluminum Lake |
Levothyroxine sodium tablets, USP meets USP Dissolution Test 7.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Thyroid hormones exert their physiologic actions through control of DNA transcription and protein synthesis. Triiodothyronine (T3) and L-thyroxine (T4) diffuse into the cell nucleus and bind to thyroid receptor proteins attached to DNA. This hormone nuclear receptor complex activates gene transcription and synthesis of messenger RNA and cytoplasmic proteins.
The physiological actions of thyroid hormones are produced predominantly by T3, the majority of which (approximately 80%) is derived from T4 by deiodination in peripheral tissues.
12.2 Pharmacodynamics
Oral levothyroxine sodium is a synthetic T4 hormone that exerts the same physiologic effect as endogenous T4, thereby maintaining normal T4 levels when a deficiency is present.
12.3 Pharmacokinetics
Absorption
Absorption of orally administered T4 from the gastrointestinal tract ranges from 40% to 80%. The majority of the levothyroxine sodium dose is absorbed from the jejunum and upper ileum. The relative bioavailability of levothyroxine sodium tablets, compared to an equal nominal dose of oral levothyroxine sodium solution, is approximately 93%. T4 absorption is increased by fasting, and decreased in malabsorption syndromes and by certain foods such as soybeans. Dietary fiber decreases bioavailability of T4. Absorption may also decrease with age. In addition, many drugs and foods affect T4 absorption [see Drug Interactions (7)] .
Distribution
Circulating thyroid hormones are greater than 99% bound to plasma proteins, including thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and albumin (TBA), whose capacities and affinities vary for each hormone. The higher affinity of both TBG and TBPA for T4 partially explains the higher serum levels, slower metabolic clearance, and longer half-life of T4 compared to T3. Protein-bound thyroid hormones exist in reverse equilibrium with small amounts of free hormone. Only unbound hormone is metabolically active. Many drugs and physiologic conditions affect the binding of thyroid hormones to serum proteins [see Drug Interactions (7)] . Thyroid hormones do not readily cross the placental barrier [see Use in Specific Populations (8.1)] .
Elimination
Metabolism
T4 is slowly eliminated (see Table 10). The major pathway of thyroid hormone metabolism is through sequential deiodination. Approximately 80% of circulating T3 is derived from peripheral T4 by monodeiodination. The liver is the major site of degradation for both T4 and T3, with T4 deiodination also occurring at a number of additional sites, including the kidney and other tissues. Approximately 80% of the daily dose of T4 is deiodinated to yield equal amounts of T3 and reverse T3 (rT3). T3 and rT3 are further deiodinated to diiodothyronine. Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation.
Excretion
Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. Approximately 20% of T4 is eliminated in the stool. Urinary excretion of T4 decreases with age.
Table 10. Pharmacokinetic Parameters of Thyroid Hormones in Euthyroid Patients|
Hormone |
Ratio in Thyroglobulin |
Biologic Potency |
t1/2 (days) |
Protein Binding (%)***** |
|
Levothyroxine (T4) |
10 to 20 |
1 |
6 to 7** |
99.96 |
|
Liothyronine (T3) |
1 |
4 |
≤ 2 |
99.5 |
|
*Includes TBG, TBPA, and TBA |
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies in animals to evaluate the carcinogenic potential of levothyroxine have not been performed. Studies to evaluate mutagenic potential and animal fertility have not been performed.
