Theraprofen-90
Theraprofen-90
334fa37b-f73a-459a-9f67-281022273fed
HUMAN PRESCRIPTION DRUG LABEL
Aug 1, 2011
Physician Therapeutics LLC
DUNS: 931940964
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
IBUPROFEN, .GAMMA.-AMINOBUTYRIC ACID
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Drug Labeling Information
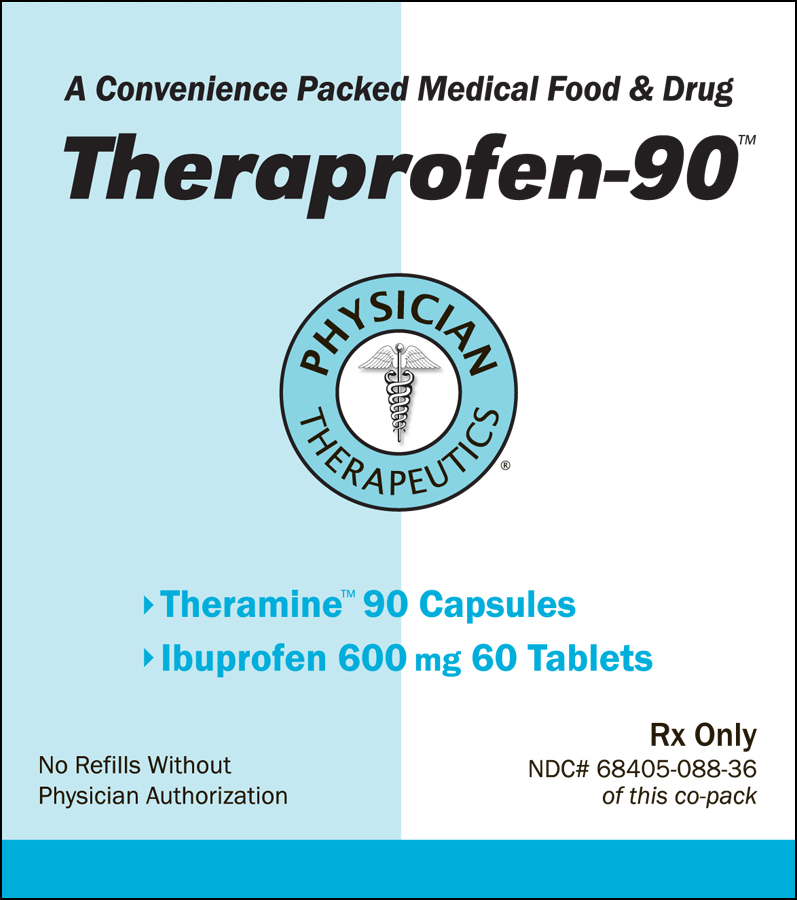
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
DESCRIPTION SECTION
PRODUCT DESCRIPTION
Primary Ingredients Theramine consists of a proprietary blend of amino acids, cocoa, caffeine, cinnamon, and flavonoids in specific proportions. These ingredients fall into the category of Generally Regarded as Safe” (GRAS) as defined by the Food and Drug Administration (FDA) (Sections 201(s) and 409 of the Federal Food, Drug, and Cosmetic Act). A GRAS substance is distinguished from a food additive on the basis of the common knowledge about the safety of the substance for its intended use. The standard for an ingredient to achieve GRAS status requires not only technical demonstration of non-toxicity and safety, but also general recognition of safety through widespread usage and agreement of that safety by experts in the field. Many ingredients have been determined by the U.S. Food and Drug Administration (FDA) to be GRAS, and are listed as such by regulation, in Volume 21 Code of Federal Regulations (CFR) Sections 182, 184, and 186.
Amino Acids
Amino Acids are the building blocks of protein. All amino acids are GRAS
listed as they have been ingested by humans for thousands of years. The doses
of the amino acids in Theramine are equivalent to those found in the usual
human diet. Patients with pain disorders may require an increased amount of
certain amino acids that cannot be obtained from normal diet alone.
Tryptophan, for example, is an obligatory amino acid. The body cannot make
tryptophan and must obtain tryptophan from the diet. Tryptophan is needed to
produce serotonin. Serotonin is required to reduce pain. Patients with pain
disorders and inflammatory conditions have altered serotonin metabolism. Some
patients with pain disorders and inflammatory conditions have a resistance to
the use of tryptophan that is similar to the mechanism found in insulin
resistance. Patients with pain disorders and inflammatory conditions cannot
acquire sufficient tryptophan from the diet to alter the perception of pain
and the inflammatory process without ingesting a prohibitively large amount of
calories, particularly calories from protein.
Flavonoids
Flavonoids are a group of phytochemical compounds found in all vascular plants
including fruits and vegetables. They are a part of a larger class of
compounds known as polyphenols. Many of the therapeutic or health benefits of
colored fruits and vegetables, cocoa, red wine, and green tea are directly
related to their flavonoid content. The specially formulated flavonoids found
in Theramine cannot be obtained from conventional foods in the necessary
proportions to elicit a therapeutic response.
Other Ingredients
Theramine contains the following inactive or other ingredients, as fillers,
excipients, and colorings: magnesium stearate, microcrystalline cellulose,
Maltodextrin NF, gelatin (as the capsule material).
Physical Description
Theramine is a yellow to light brown powder. Theramine contains L-Glutamine,
L-Arginine, L-Histidine, and L-Serine, 5-Hydroxytryptophan as Griffonia Seed
Extract, GABA, Choline Bitartrate, Cinnamon, Cocoa, Hydrolyzed Whey Protein,
and Grape Seed Extract.
WARNINGS SECTION
CARDIOVASCULAR EFFECTS
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID does increase the risk of serious GI events (see GI WARNINGS).
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10-14 days following CABG surgery found an increased incidence of myocardial infarction and stroke (see CONTRAINDICATIONS).
Hypertension
NSAIDs including ibuprofen tablets, can lead to onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including ibuprofen tablets, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
Congestive Heart Failure and Edema
Fluid retention and edema have been observed in some patients taking NSAIDs. Ibuprofen tablets should be used with caution in patients with fluid retention or heart failure.
Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation
NSAIDs, including ibuprofen tablets, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3-6 months, and in about 2-4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients treated with neither of these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population. To minimize the potential risk for an adverse GI event in patients treated with a NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulcerations and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high-risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a NSAID may cause a dose- dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Advanced Renal Disease
No information is available from controlled clinical studies regarding the use of ibuprofen tablets in patients with advanced renal disease. Therefore, treatment with ibuprofen tablets is not recommended in these patients with advanced renal disease. If ibuprofen tablets therapy must be initiated, close monitoring of the patients renal function is advisable.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to ibuprofen tablets. Ibuprofen tablets should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONS and PRECAUTIONS, Preexisting Asthma). Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions
NSAIDs, including ibuprofen tablets, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
PRECAUTIONS SECTION
General
Ibuprofen tablets cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
The pharmacological activity of ibuprofen tablets in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
Hepatic effects
Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs, including ibuprofen tablets. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice, fulminant hepatitis, liver necrosis, and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs suggesting liver dysfunction, or with abnormal liver test values, should be evaluated for evidence of the development of a more severe hepatic reaction while on therapy with ibuprofen tablets. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), ibuprofen tablets should be discontinued.
Hematological effects
Anemia is sometimes seen in patients receiving NSAIDs, including ibuprofen tablets. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including ibuprofen tablets, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
In two postmarketing clinical studies the incidence of a decreased hemoglobin level was greater than previously reported. Decrease in hemoglobin of 1 gram or more was observed in 17.1% of 193 patients on 1600 mg ibuprofen daily (osteoarthritis), and in 22.8% of 189 patients taking 2400 mg of ibuprofen daily (rheumatoid arthritis). Positive stool occult blood tests and elevated serum creatinine levels were also observed in these studies.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients.
Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible.
Patients receiving ibuprofen tablets who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants should be carefully monitored.
Preexisting asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm, which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and NSAIDs has been reported in such aspirin- sensitive patients, ibuprofen tablets should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Ophthalmological effects
Blurred and/or diminished vision, scotomata, and/or changes in color vision have been reported. If a patient develops such complaints while receiving ibuprofen tablets, the drug should be discontinued, and the patient should have an ophthalmologic examination which includes central visual fields and color vision testing.
Aseptic meningitis
Aseptic meningitis with fever and coma has been observed on rare occasions in patients on ibuprofen therapy. Although it is probably more likely to occur in patients with systemic lupus erythematosus and related connective tissue diseases, it has been reported in patients who do not have an underlying chronic disease. If signs or symptoms of meningitis develop in a patient on ibuprofen tablets, the possibility of its being related to ibuprofen tablets should be considered
SPL UNCLASSIFIED SECTION
Theramine™ PRODUCT INFORMATION
Theramine (U.S. patent pending) capsules by oral administration. A specially formulated Medical Food product, consisting of a proprietary blend of amino acids and polyphenol ingredients in specific proportions, for the dietary management of the metabolic processes associated with pain disorders and inflammatory conditions. (PD) (IC). Must be administered under physician supervision.
Medical Foods
Medical Food products are often used in hospitals (e.g., for burn victims or
kidney dialysis patients) and outside of a hospital setting under a
physician’s care for the dietary management of diseases in patients with
particular medical or metabolic needs due to their disease or condition.
Congress defined "Medical Food" in the Orphan Drug Act and Amendments of 1988
as "a food which is formulated to be consumed or administered enterally [or orally] under the supervision of a physician and which is intended for the
specific dietary management of a disease or condition for which distinctive
nutritional requirements, based on recognized scientific principles, are
established by medical evaluation." Medical Foods are complex formulated
products, requiring sophisticated and exacting technology. Theramine has been
developed, manufactured, and labeled in accordance with both the statutory and
the FDA regulatory definition of a Medical Food. Theramine must be used while
the patient is under the ongoing care of a physician.
PAIN DISORDERS (PD) INFLAMMATORY CONDITIONS (IC)
PD and IC as a Metabolic Deficiency Disease
A critical component of the definition of a Medical Food is the requirement
for a distinctive nutritional deficiency. FDA scientists have proposed a
physiologic definition of a distinctive nutritional deficiency as follows:
“the dietary management of patients with specific diseases requires, in some
instances, the ability to meet nutritional requirements that differ
substantially from the needs of healthy persons. For example, in establishing
the recommended dietary allowances for general, healthy population, the Food
and Nutrition Board of the Institute of Medicine National Academy of Sciences,
recognized that different or distinctive physiologic requirements may exist
for certain persons with "special nutritional needs arising from metabolic
disorders, chronic diseases, injuries, premature birth, other medical
conditions and drug therapies. Thus, the distinctive nutritional needs
associated with a disease reflects the total amount needed by a healthy person
to support life or maintain homeostasis, adjusted for the distinctive changes
in the nutritional needs of the patient as a result of the effects of the
disease process on absorption, metabolism and excretion.” It was also proposed
that in patients with certain disease states who respond to nutritional
therapies, a physiologic deficiency of the nutrient is assumed to exist. For
example, if a patient with pain disorders responds to a tryptophan formulation
by decreasing perceived pain, a deficiency of tryptophan is assumed to exist.
Patients with pain disorders and inflammatory conditions are known to have
nutritional deficiencies of tryptophan, choline, arginine, GABA, flavonoids,
and certain antioxidants. Patients with pain disorders and inflammatory
conditions frequently exhibit reduced plasma levels of tryptophan and GABA and
have been shown to respond to oral administration of GABA, arginine,
tryptophan, or a 5-hydoxytryptophan formulation. Research has shown that
tryptophan, arginine or GABA reduced diets result in a fall of circulating
tryptophan, arginine, and/or GABA.
Patients with pain disorders frequently exhibit activation of the degradation pathways that increases the turnover of GABA, arginine and/or tryptophan leading to a reduced level of production of serotonin, GABA or nitric oxide for a given precursor blood level. Research has also shown that a genetic predisposition to accelerated degradation can lead to increased precursor requirements in certain patients with pain disorders and inflammatory conditions.
Choline is required to fully potentiate acetylcholine synthesis by brain neurons. A deficiency of choline leads to reduced acetylcholine production by the neurons. Flavonoids potentiate the production of acetylcholine by the neurons thereby reducing delta pain. Diets deficient in flavonoid rich foods and choline result in inadequate flavonoid concentrations, impeding acetylcholine production in certain patients with pain disorders and/or inflammatory conditions. Acetylcholine in pre-synaptic ganglia is necessary for the production of serotonin and nitric oxide in post-synaptic ganglia. Provision of tryptophan, arginine, GABA, choline and flavonoids with antioxidants, in specific proportions can restore the production of beneficial serotonin, nitric oxide, and acetylcholine, thereby reducing the perception of pain and reducing inflammation. L-Histidine is known to produce brain histamine that stimulates production of ACTH.
