GONAL-F RFF
These highlights do not include all the information needed to use GONAL-F RFF safely and effectively. See full prescribing information for GONAL-F RFF (follitropin alfa) for injection, for subcutaneous use Initial U.S. Approval: 1997
aa759a1b-2c1d-438b-bd7e-019a2067699d
HUMAN PRESCRIPTION DRUG LABEL
Nov 20, 2023
EMD Serono, Inc.
DUNS: 088514898
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
follitropin alfa
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
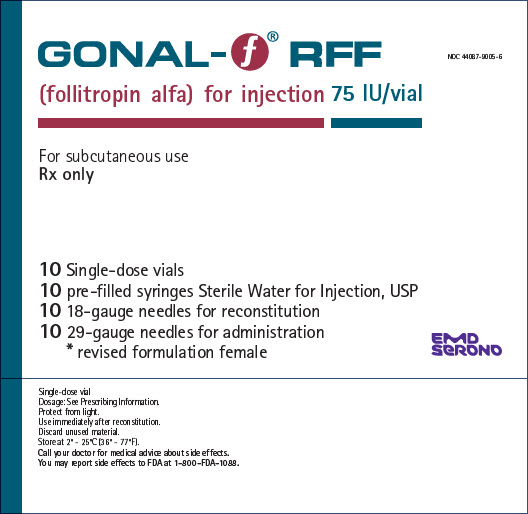
PRINCIPAL DISPLAY PANEL - Kit Carton
GONAL- f® RFF
(follitropin alfa) for injection 75 IU/vial
NDC 44087-9005-6
For subcutaneous use
Rx only
10 Single-dose vials
10 pre-filled syringes Sterile Water for Injection, USP
10 18-gauge needles for reconstitution
10 29-gauge needles for administration
- revised formulation female
EMD
Serono
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions and Anaphylaxis
In the postmarketing experience, serious systemic hypersensitivity reactions, including anaphylaxis, have been reported with use of GONAL-F® and GONAL-F® RFF. Symptoms have included dyspnea, facial edema, pruritus, and urticaria. If an anaphylactic or other serious allergic reaction occurs, initiate appropriate therapy including supportive measures if cardiovascular instability and/or respiratory compromise occur, and discontinue further use.
5.2 Ovarian Hyperstimulation Syndrome (OHSS)
Ovarian Hyperstimulation Syndrome (OHSS) is a medical event distinct from uncomplicated ovarian enlargement and may progress rapidly to become a serious medical event. OHSS is characterized by a dramatic increase in vascular permeability, which can result in a rapid accumulation of fluid in the peritoneal cavity, thorax, and potentially, the pericardium. The early warning signs of the development of OHSS are severe pelvic pain, nausea, vomiting, and weight gain. Abdominal pain, abdominal distension, gastrointestinal symptoms including nausea, vomiting and diarrhea, severe ovarian enlargement [see Warnings and Precautions (5.5)], weight gain, dyspnea, and oliguria have been reported with OHSS. Clinical evaluation may reveal hypovolemia, hemoconcentration, electrolyte imbalances, ascites, hemoperitoneum, pleural effusions, hydrothorax, acute pulmonary distress, and thromboembolic reactions [See Warnings and Precautions (5.3)]. Transient liver function test abnormalities suggestive of hepatic dysfunction with or without morphologic changes on liver biopsy, have been reported in association with OHSS.
OHSS occurs after gonadotropin treatment has been discontinued and it can develop rapidly, reaching its maximum about seven to ten days following treatment. Usually, OHSS resolves spontaneously with the onset of menses. If there is evidence that OHSS may be developing prior to hCG administration [see Dosage and Administration (2.3, 2.4)], withhold hCG. Cases of OHSS are more common, more severe, and more protracted if pregnancy occurs; therefore, assess women for the development of OHSS for at least two weeks after hCG administration.
If serious OHSS occurs, stop gonadotropins, including GONAL-F RFF and hCG, and consider whether the woman needs to be hospitalized. Treatment is primarily symptomatic and overall consists of bed rest, fluid and electrolyte management, and analgesics (if needed). Because the use of diuretics can accentuate the diminished intravascular volume, avoid diuretics except in the late phase of resolution as described below. The management of OHSS is divided into three phases as follows:
-
Acute Phase:
Management is directed at preventing hemoconcentration due to loss of intravascular volume to the third space and minimizing the risk of thromboembolic phenomena and kidney damage. Thoroughly assess daily or more often, based on the clinical need, fluid intake and output, weight, hematocrit, serum and urinary electrolytes, urine specific gravity, BUN and creatinine, total proteins with albumin: globulin ratio, coagulation studies, electrocardiogram to monitor for hyperkalemia, and abdominal girth. Treatment, consisting of limited intravenous fluids, electrolytes, human serum albumin, is intended to normalize electrolytes while maintaining an acceptable but somewhat reduced intravascular volume. Full correction of the intravascular volume deficit may lead to an unacceptable increase in the amount of third space fluid accumulation. -
Chronic Phase:
After the acute phase is successfully managed as above, excessive fluid accumulation in the third space should be limited by instituting severe potassium, sodium, and fluid restriction. -
Resolution Phase:
As third space fluid returns to the intravascular compartment, a fall in hematocrit and increasing urinary output are observed in the absence of any increase in intake. Peripheral and/or pulmonary edema may result if the kidneys are unable to excrete third space fluid as rapidly as it is mobilized. Diuretics may be indicated during the resolution phase, if necessary, to combat pulmonary edema.
Do not remove ascitic, pleural, and pericardial fluid, unless there is the necessity to relieve symptoms such as pulmonary distress or cardiac tamponade.
OHSS increases the risk of injury to the ovary. Avoid pelvic examination or intercourse, as these may cause rupture of an ovarian cyst, which may result in hemoperitoneum.
If bleeding occurs and requires surgical intervention, control the bleeding and retain as much ovarian tissue as possible. A physician experienced in the management of this syndrome, or who is experienced in the management of fluid and electrolyte imbalances should be consulted.
OHSS occurred in 6 of 83 (7.2%) GONAL-F RFF treated women in an induction of ovulation trial; none were classified as severe. In an ART trial, OHSS occurred in 11 of 237 (4.6%) GONAL-F RFF treated women and 1 (0.42%) was classified as severe.
5.3 Pulmonary and Vascular Complications
Serious pulmonary conditions (for example, atelectasis, acute respiratory distress syndrome and exacerbation of asthma) have been reported in women treated with gonadotropins, including GONAL-F RFF. In addition, thromboembolic events both in association with, and separate from OHSS have been reported in women treated with gonadotropins, including GONAL-F RFF. Intravascular thrombosis and embolism, which may originate in venous or arterial vessels, can result in reduced blood flow to critical organs or the extremities. Women with generally recognized risk factors for thrombosis, such as personal or family history, severe obesity, or thrombophilia, may have an increased risk of venous or arterial thromboembolic events, during or following treatment with gonadotropins. Sequelae of such events have included venous thrombophlebitis, pulmonary embolism, pulmonary infarction, cerebral vascular occlusion (stroke), and arterial occlusion resulting in loss of limb and rarely in myocardial infarctions. In rare cases, pulmonary complications and/or thromboembolic events have resulted in death. In women with recognized risk factors, the benefits of ovulation induction and Assisted Reproductive Technology (ART) need to be weighed against the risks. It should be noted that pregnancy also carries an increased risk of thrombosis.
5.4 Ovarian Torsion
Ovarian torsion has been reported after treatment with gonadotropins, including GONAL-F RFF. This may be related to OHSS, pregnancy, previous abdominal surgery, past history of ovarian torsion, previous or current ovarian cyst and polycystic ovaries. Early diagnosis and immediate detorsion limit damage to the ovary due to reduced blood supply.
5.5 Abnormal Ovarian Enlargement
In order to minimize the hazards associated with abnormal ovarian enlargement that may occur with GONAL-F RFF therapy, individualize treatment and use the lowest effective dose [see Dosage and Administration (2.3, 2.4)]. Use of ultrasound monitoring of ovarian response and/or measurement of serum estradiol levels is important to minimize the risk of ovarian stimulation [see Warnings and Precautions (5.12)].
If the ovaries are abnormally enlarged on the last day of GONAL-F RFF therapy, do not administer hCG in order to reduce the chance of developing OHSS [see Warnings and Precautions (5.2)]. Prohibit intercourse for women with significant ovarian enlargement after ovulation because of the danger of hemoperitoneum resulting from rupture of ovarian cysts [see Warnings and Precautions (5.2)].
5.6 Multi-fetal Gestation and Birth
Multi-fetal gestation and births have been reported with all gonadotropin therapy, including therapy with GONAL-F RFF. In a trial of induction of ovulation, 20% of live births were multiple births in women receiving GONAL-F RFF over three treatment cycles.
In an ART trial, 35.1% of live births were multiple births in women receiving GONAL-F RFF. The rate of multiple births is dependent on the number of embryos transferred. Advise the woman and her partner of the potential risk of multi- fetal gestation and birth before beginning therapy with GONAL-F RFF.
5.7 Embryofetal Toxicity
The incidence of congenital malformations (birth defects) after some Assisted Reproductive Technology [(ART) specifically in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)] may be slightly higher than after spontaneous conception. This slightly higher incidence is thought to be related to differences in parental characteristics (e.g., maternal age, maternal and paternal genetic background, sperm characteristics) and to the higher incidence of multi-fetal gestations after IVF or ICSI. There is no evidence that the use of gonadotropins during IVF or ICSI is associated with an increased risk of congenital malformations.
5.8 Ectopic Pregnancy
Since infertile women undergoing ART often have tubal abnormalities, the incidence of ectopic pregnancy may be increased in women who become pregnant as a result of ART. Advise women who become pregnant following ART and have: abdominal/pelvic pain (particularly on one side); shoulder, neck or rectal pain; and nausea and vomiting to seek immediate medical attention. Confirm the presence of an intrauterine pregnancy early by β-hCG testing and transvaginal ultrasound.
5.9 Spontaneous Abortion
The risk of spontaneous abortion (miscarriage) is increased with gonadotropin products, including GONAL-F RFF. However, causality has not been established. The increased risk may be a factor of the underlying infertility.
5.10 Ovarian Neoplasms
There have been infrequent reports of ovarian neoplasms, both benign and malignant, in women who have had multiple drug therapy for controlled ovarian stimulation, however, a causal relationship has not been established.
5.11 Laboratory Tests
In most instances, treatment of women with GONAL-F RFF results only in follicular recruitment and development. In the absence of an endogenous LH surge, hCG is given to trigger ovulation when monitoring of the patient indicates that sufficient follicular development has occurred. This may be estimated by ultrasound alone or in combination with measurement of serum estradiol concentrations. The combination of both ultrasound and serum estradiol measurement are useful for monitoring follicular growth and maturation, timing of the ovulatory trigger, detecting ovarian enlargement and minimizing the risk of the Ovarian Hyperstimulation Syndrome and multiple gestation.
The clinical confirmation of ovulation is obtained by direct or indirect indices of progesterone production, as well as sonographic evidence of ovulation.
Direct or indirect indices of progesterone production:
- Urinary or serum luteinizing hormone (LH) rise
- A rise in basal body temperature
- Increase in serum progesterone
- Menstruation following a shift in basal body temperature
Sonographic evidence of ovulation:
- Collapsed follicle
- Fluid in the cul-de-sac
- Features consistent with corpus luteum formation
- Secretory endometrium
- Hypersensitivity Reactions and Anaphylaxis: If occurs, initiate appropriate therapy, including supportive measures, and discontinue use of GONAL-F RFF (5.1)
- Ovarian Hyperstimulation Syndrome (OHSS): If serious, stop gonadotropins, including hCG, and determine if the woman needs to be hospitalized. Treatment is primarily symptomatic and consists of bed rest, fluid and electrolyte management, and analgesics (5.2)
- Pulmonary and Vascular Complications: In women with recognized risk factors, the benefits of induction of ovulation and ART need to be weighed against the risks. During or after use of GONAL-F RFF, monitor for venous or arterial thromboembolic events (5.3)
- Ovarian Torsion: Early diagnosis and immediate detorsion limit damage to the ovary due to reduced blood supply (5.4)
- Abnormal Ovarian Enlargement: If the ovaries are abnormally enlarged on the last day of GONAL-F RFF therapy, inform women not to administer hCG and to avoid intercourse (5.5)
- Multi-fetal Gestation and Births: The rate of multiple births is dependent on the number of embryos transferred. Advise the woman and her partner of the potential risk of multi-fetal gestation and birth before beginning therapy with GONAL-F RFF (5.6)
- Embryofetal Toxicity: Inform women that the incidence of congenital malformations (birth defects) after some Assisted Reproductive Technology [(ART) specifically in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)] may be slightly higher than after spontaneous conception. There is no evidence that the use of gonadotropins during IVF or ICSI is associated with an increased risk of congenital malformations (5.7)
- Ectopic Pregnancy: Advise women who become pregnant following ART and have: abdominal/pelvic pain (particularly on one side); shoulder, neck or rectal pain; and nausea and vomiting to seek immediate medical attention. Confirm the presence of an intrauterine pregnancy early by β-hCG testing and transvaginal ultrasound (5.8)
- Spontaneous Abortion: The risk of spontaneous abortion (miscarriage) is increased with gonadotropin products, however, causality has not been established (5.9)
- Ovarian Neoplasm: Both benign and malignant ovarian neoplasms are reported in women who have had multiple drug therapy for controlled ovarian stimulation, however, causality has not been established (5.10)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
GONAL-F RFF is not indicated in pregnant women.
The incidence of congenital malformations after some Assisted Reproductive Technology [(ART), specifically in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)], may be slightly higher than that after spontaneous conception. This slightly higher incidence is thought to be related to differences in parental characteristics (e.g., maternal age, maternal and paternal genetic background, sperm characteristics) and to a higher incidence of multi-fetal gestations after IVF or ICSI. There is no human data that the use of gonadotropins (including GONAL-F RFF), alone or as part of IVF or ICSI cycles, increases the risk of congenital malformations.
The risk of spontaneous abortion (miscarriage) is increased in women who have used gonadotropins products (including GONAL-F RFF) to achieve pregnancy.
In animal studies, the continuous administration of recombinant human FSH during pregnancy resulted in a decrease in the number of viable fetuses and difficult and prolonged delivery. No teratogenic effect has been observed.
In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Data on a limited number of GONAL-F RFF- or GONAL-F-exposed pregnancies indicate no adverse reactions of gonadotropins on pregnancy, embryonal or fetal development, parturition or postnatal development following controlled ovarian stimulation.
Animal Data
Embryofetal development studies with recombinant human FSH in rats, where dosing occurred during organogenesis, showed a dose dependent increase in difficult and prolonged parturition in dams, and dose dependent increases in resorptions, pre- and post-implantation losses, and stillborn pups at doses representing 5 and 41 times the lowest clinical dose of 75 International Units based on body surface area. Pre-/post-natal development studies with recombinant human FSH in rats, where dosing occurred from mid-gestation through lactation, showed difficult and prolonged parturition in all dams dosed at 41 times the lowest clinical dose of 75 International Units based on body surface area, along with maternal death and stillborn pups associated with the difficult and prolonged parturition. This toxicity was not observed in dams and offspring dosed at a level 5 times the lowest clinical dose of 75 International Units based on body surface area.
8.2 Lactation
There are no data on the presence of GONAL-F RFF in human milk, the effects on the breastfed infant, or the effects on milk production. Because the secretion of prolactin during lactation can result in inadequate response to ovarian stimulation, advise women not to breast feed during treatment with GONAL F RFF.
8.3 Females and Males of Reproductive Potential
Because GONAL-F RFF is not indicated in pregnant women, verify a negative pregnancy test before administering GONAL-F RFF to a woman [see Dosage and Administration (2.3, 2.4)].
8.4 Pediatric use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Safety and effectiveness of GONAL-F RFF in postmenopausal women have not been established and it is not indicated in this population.
- Lactation: Advise not to breastfeed (8.2)
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of action
GONAL-F RFF stimulates ovarian follicular growth in women who do not have primary ovarian failure. In order to bring about final maturation of the follicle and ovulation in the absence of an endogenous LH surge, human chorionic gonadotropin (hCG) must be given, following the administration of GONAL-F RFF, when monitoring of the patient indicates that sufficient follicular development is achieved.
12.2 Pharmacodynamics
The pharmacodynamics of GONAL-F RFF have not been fully characterized. There is inter-woman variability in response to follitropin alfa administration.
12.3 Pharmacokinetics
The pharmacokinetics of GONAL-F RFF have not been fully characterized. Follitropin alfa mean (%CV) AUClast is 884 International Units hr/L (20%) and Cmax is 9.83 International Units/L (23%) following a single subcutaneous dose of 300 International Units of GONAL-F RFF to 21 pre-menopausal healthy female volunteers who had previously received a GnRH agonist for pituitary down- regulation.
Absorption
The mean (%CV) time to Cmax is 15.5 hrs (43%).
Elimination
The mean (%CV) elimination half-life of follitropin alfa is 53 hrs (52%) and is dependent on the absorption rate.
Drug Interaction Studies
No studies evaluating the drug interaction potential of follitropin alfa have been conducted.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, mutagenesis, impairment of fertility
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of GONAL-F RFF. However, follitropin alfa showed no mutagenic activity in a series of tests performed to evaluate its potential genetic toxicity including, bacterial and mammalian cell mutation tests, a chromosomal aberration test and a micronucleus test.
Impaired fertility has been reported in rats, exposed to pharmacological doses of follitropin alfa (greater than or equal to 40 International Units per kg per day, greater than or equal to 5 times the lowest clinical dose of 75 International Units) for extended periods, through reduced fecundity.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise women to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Hypersensitivity Reactions and Anaphylaxis
Advise women to discontinue Gonal-F RFF and seek immediate medical attention if any signs or symptoms of a hypersensitivity reaction occur [see Warnings and Precautions (5.1)].
Ovarian Hyperstimulation Syndrome
Inform women regarding the risks of OHSS [see Warnings and Precautions (5.2)] and OHSS-associated conditions including pulmonary and vascular complications [see Warnings and Precautions (5.3)], and ovarian torsion [see Warnings and Precautions (5.4)] with the use of GONAL-F RFF. Advise women to seek medical attention if any of these conditions occur.
Abnormal Ovarian Enlargement
Inform women regarding the hazards associated with abnormal ovarian enlargement that may occur with GONAL-F RFF therapy. If the ovaries are abnormally enlarged on the last day of GONAL-F RFF therapy, inform women not to administer hCG and to avoid intercourse [see Warnings and Precautions (5.5)].
Multi-fetal Gestation and Birth
Advise the woman and her partner of the potential risk of multi-fetal gestation and birth before beginning therapy with GONAL-F RFF [see Warnings and Precautions (5.6)].
Embryofetal Toxicity
Inform women that the incidence of congenital malformations (birth defects) after some Assisted Reproductive Technology [(ART) specifically in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)] may be slightly higher than after spontaneous conception [see Warnings and Precautions (5.7)].
Ectopic Pregnancy
Inform women undergoing ART that the incidence of ectopic pregnancy may be increased with these procedures, particularly for women with tubal abnormalities. Advise women who become pregnant and have: abdominal/pelvic pain (particularly on one side); shoulder, neck or rectal pain; and nausea and vomiting to seek immediate medical attention [see Warnings and Precautions (5.8)].
Spontaneous Abortion
Inform women that the risk of spontaneous abortion (miscarriage) is increased with gonadotropin products (including GONAL-F RFF). However, causality has not been established. The increased risk may be a factor of the underlying infertility [see Warnings and Precautions (5.9)].
Lactation
Advise women not to breastfeed because the secretion of prolactin during lactation can result in inadequate response to ovarian stimulation with Gonal-F RFF [see Use in Specific Populations (8.2)].
Dosing and Use of GONAL-F RFF single-use vials
Instruct women on the correct usage and dosing of GONAL-F RFF [see Dosage and Administration (2.3, 2.4)]. Instruct women to reconstitute one or more vials of GONAL-F RFF using 1 mL sterile diluent and the 18G 1-1/2" pink mixing needle provided. Instruct women to safely remove mixing needle and replace with 29G ½" needle for injection. Caution women not to change the dosage or the schedule of administration unless she is told to do so by her healthcare provider.
Duration and Necessary Monitoring in Women Undergoing Therapy with GONAL-F RFF
Prior to beginning therapy with GONAL-F RFF, inform women about the time commitment and monitoring procedures necessary for treatment [see Dosage and Administration (2.3, 2.4) and Warnings and Precautions (5.11)].
Instructions Regarding a Missed Dose
Inform the woman that if she misses or forgets to take a dose of GONAL-F RFF, she should not double the next dose and should call her healthcare provider for further dosing instructions [see Dosage and Administration (2.5)].
