ASCENIV
These highlights do not include all the information needed to use ASCENIV safely and effectively. See full prescribing information for ASCENIV. ASCENIV (immune globulin intravenous, human – slra) 10% Liquid Initial U.S. Approval: 2019
d74f4360-3b51-496c-96fb-84c3976958d2
HUMAN PRESCRIPTION DRUG LABEL
Mar 11, 2024
ADMA Biologics, Inc.
DUNS: 117213235
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
HUMAN IMMUNOGLOBULIN G
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Drug Labeling Information
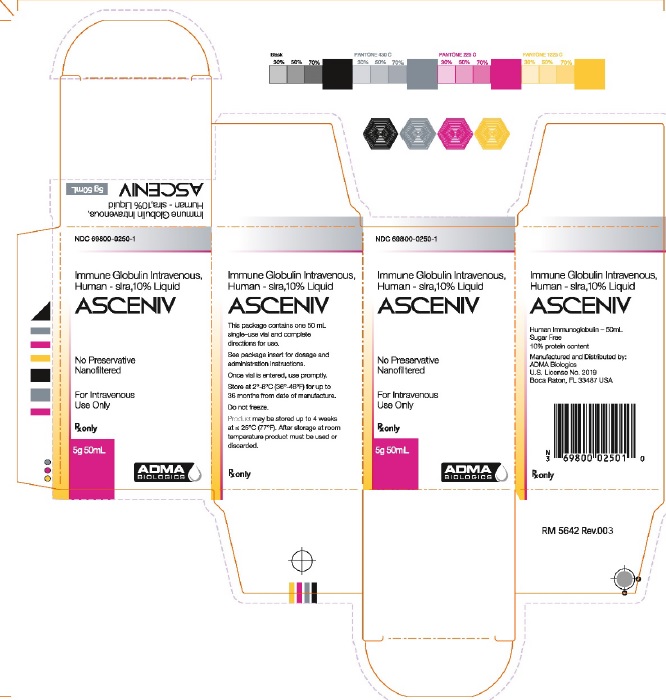
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 69800-0250-1 - Carton Label
BOXED WARNING SECTION
WARNING: THROMBOSIS, RENAL DYSFUNCTION AND ACUTE RENAL FAILURE
****See full prescribing information for complete boxed warning.
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
ASCENIV (immune globulin intravenous, human – slra) is a 10% immune globulin liquid for intravenous injection, indicated for the treatment of primary humoral immunodeficiency (PI) in adults and adolescents (12 to 17 years of age). PI includes, but is not limited to, the humoral immune defect in congenital agammaglobulinemia, common variable immunodeficiency (CVID), X-linked agammaglobulinemia, Wiskott-Aldrich syndrome, and severe combined immunodeficiencies (SCID).
ASCENIV (immune globulin intravenous, human – slra) is a 10% immune globulin liquid for intravenous injection, indicated for the treatment of primary humoral immunodeficiency (PI) in adults and adolescents (12 to 17 years of age). [1]
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
ASCENIV is contraindicated in:
- patients who have had an anaphylactic or severe systemic reaction to the administration of human immune globulin.
- IgA-deficiency patients with antibodies to IgA and a history of hypersensitivity.
- History of anaphylactic or severe systemic reactions to human immunoglobulin. [4]
- IgA-deficient patients with antibodies to IgA and a history of hypersensitivity. [4, 5.1]
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The most common adverse reactions to ASCENIV (reported in ≥5% of clinical study subjects) were headache, sinusitis, diarrhea, gastroenteritis viral, nasopharyngitis, upper respiratory tract infection, bronchitis, and nausea.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials cannot be directly compared to rates in the clinical trials of another product and may not reflect the rates observed in clinical practice.
In a multicenter, open-label, non-randomized clinical trial, 59 subjects with PI, on regular IGIV replacement therapy, received doses of ASCENIV ranging from 284 to 1008 mg/kg (mean dose 505 mg/kg) every 3 weeks or 4 weeks for up to 12 months (mean 346 days; range 36 to 385 days) (see Clinical Studies [14]). The use of pre-medication was discouraged; however, if after two infusions of ASCENIV subjects required pre-medication (antipyretic, antihistamine, or antiemetic agent) for recurrent reactions, they could continue those medications for the duration of the trial. Of the 793 infusions administered during this trial, only 7 (11.9%) subjects received premedication prior to 7 (0.9%) infusions.
Fifty-eight subjects (98%) had an adverse reaction during the study. The proportion of subjects who had at least one adverse reaction was similar for both the 3- and 4-week cycles. The most common adverse reactions observed in this clinical trial were headache (22 subjects, 37%), sinusitis (16 subjects, 27%), diarrhea (14 subjects, 23%), gastroenteritis viral (13 subjects, 22%), nasopharyngitis (13 subjects, 22%), upper respiratory tract infection (13 subjects, 22%), bronchitis (12 subjects, 20%), nausea (12 subjects, 20%), and acute sinusitis (11 subjects, 19%).
Adverse reactions (ARs) occurring during or within 72 hours after the end of an infusion are presented in Table 2. In this study, the upper bound of the 1-sided 95% confidence interval for the proportion of ASCENIV infusions with one or more temporally associated adverse reactions was 16.4%. The total number of adverse reactions was 158 (a rate of 0.20 ARs per infusion).
Table 2: Adverse Reactions (ARs) (within 72 hours after the end of an ASCENIV infusion) in ≥ 5% of Subjects|
Preferred Term (MedDRA v16.0) |
Number (%) of Subjects |
Number (%) of Infusions |
|
Headache |
14 (24) |
21 (2.6) |
|
Sinusitis |
6 (10) |
7 (0.9) |
|
Nausea |
5 (9) |
5 (0.6) |
|
Acute sinusitis |
4 (7) |
4 (0.5) |
|
Fatigue |
4 (7) |
9 (1.1) |
|
Muscle spasms |
4 (7) |
4 (0.5) |
|
Bronchitis |
3 (5) |
3 (0.4) |
|
Diarrhea |
3 (5) |
3 (0.4) |
|
Nose Bleed |
3 (5) |
4 (0.5) |
|
Muscle Pain |
3 (5) |
5 (0.6) |
|
Oropharyngeal pain |
3 (5) |
3 (0.4) |
|
Pain in extremity |
3 (5) |
3 (0.4) |
|
Itching |
3 (5) |
3 (0.4) |
6.2 Postmarketing Experience
Because postmarketing reporting of adverse reactions is voluntary and from a population of uncertain size, it is not always possible to reliably estimate the frequency of these reactions or establish a causal relationship to product exposure. The following adverse reactions have been identified and reported during the post-approval use of IGIV products:
- Respiratory: Apnea, Acute Respiratory Distress Syndrome (ARDS), cyanosis, dyspnea, bronchospasm.
- Cardiovascular: Cardiac arrest, vascular collapse, hypotension.
- Neurological: Coma, loss of consciousness, seizures, tremor.
- Integumentary: Stevens-Johnson syndrome, epidermolysis, erythema multiforme, bullous dermatitis.
- Hematologic: Pancytopenia, leukopenia.
- General/Body as a Whole: Pyrexia, rigors.
- Gastrointestinal: Hepatic dysfunction, abdominal pain.
The most common adverse reactions to ASCENIV (≥5% of study subjects) were headache, sinusitis, diarrhea, gastroenteritis viral, nasopharyngitis, upper respiratory tract infection, bronchitis, and nausea. [6]
To report SUSPECTED ADVERSE REACTIONS, contact ADMA Biologics at (1-800-458-4244) or FDA at 1-800-FDA-1088 or****www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Immunoglobulin administration may transiently impair the efficacy of live attenuated virus vaccines such as measles, mumps, rubella, and varicella because the continued presence of high levels of passively acquired antibody may interfere with an active antibody response. 15,16 The immunizing physician should be informed of recent therapy with ASCENIV so that appropriate measures may be taken ( see Patient Counseling Information [17]).
- Passive transfer of antibodies may transiently interfere with the immune response to live virus vaccines, such as measles, mumps, rubella, and varicella. [7]
- Passive transfer of antibodies may confound the results of serological testing. [5.10]
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Dose
The recommended dose of ASCENIV for replacement therapy in primary humoral immunodeficiency (PI) is 300 to 800 mg/kg body weight administered every 3 to 4 weeks. The dose may be adjusted over time to achieve the desired trough levels and clinical response.
ASCENIV dose adjustments may be required in patients who fail to maintain trough total IgG concentrations of at least 500 mg/ dL with a target of 600 mg/dL. Starting with the second infusion, adjust the dose proportionally, targeting a trough of ≥ 600 mg/dL, based on the previous trough and the associated dose.
For intravenous use only.
Table 1|
Dose |
Initial Infusion |
Maintenance Infusion Rate |
|
300-800 mg/kg every |
0.5 mg/kg/min |
Increase gradually every 15 minutes (if tolerated) up to 8 |
2.2 Preparation and Handling
- ASCENIV is a clear to opalescent, colorless to pale yellow solution. Inspect visually for particulate matter and discoloration prior to administration. Do not use if the liquid is cloudy or turbid, or if it contains visible particulate matter.
- Allow refrigerated product to come to room temperature before use and maintain ASCENIV at room temperature during administration.
- DO NOT MICROWAVE.
- DO NOT SHAKE.
- DO NOT MIX with other IGIV products or other intravenous medications.
- DO NOT DILUTE.
- ASCENIV contains no preservatives. Each vial is for single use only. Do not reuse or save for future use.
- If large doses are required, several vials may be pooled using aseptic technique into sterile infusion bags and infused.
2.3 Administration
Begin with an initial infusion rate of 0.5 mg/kg/min. If there are no adverse reactions, the infusion rate for subsequent infusions can be slowly increased to the maximum rate.
Monitor patient vital signs throughout the infusion. Slow or stop the infusion if adverse reactions occur. If symptoms subside promptly, the infusion may be resumed at a slower rate which is comfortable for the patient.
Ensure that patients with pre-existing renal insufficiency are not volume- depleted. For patients judged to be at risk for renal dysfunction or thrombotic events, administer ASCENIV at the minimum infusion rate practicable, and consider discontinuation of administration if renal function deteriorates ( see Boxed Warning, Warnings and Precautions [5.2, 5.3]).
For intravenous use only.
|
Dose |
Initial Infusion |
Maintenance Infusion Rate |
|
300-800 |
0.5 mg/kg/min |
Increase gradually every 15 |
- Ensure that patients with pre-existing renal insufficiency are not volume depleted; discontinue ASCENIV if renal function deteriorates. [5.3]
- For patients at risk of renal dysfunction or thrombotic events, administer ASCENIV at the minimum infusion rate practicable. [5.2, 5.3]
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
ASCENIV is a liquid solution containing 10% IgG (100 mg/mL) for intravenous infusion.
ASCENIV is a liquid solution containing 10% IgG (100 mg/mL) for intravenous infusion; (5g in 50 mL solution). [3]
DESCRIPTION SECTION
11 DESCRIPTION
ASCENIV is a purified, sterile, ready-to-use preparation of concentrated human immunoglobulin G (IgG) antibodies. The product is a clear to opalescent liquid, which is colorless to pale yellow. The distribution of IgG subclasses is similar to that of normal plasma. The active ingredient is human immunoglobulin purified from source human plasma and processed using a modified classical Cohn Method 6 / Oncley Method 9 fractionation procedure. ASCENIV contains 100 ± 10 mg/mL protein, of which not less than 96% is human immunoglobulin obtained from source human plasma. It is formulated in water for injection containing 0.100-0.140 M sodium chloride, 0.20-0.29 M glycine, 0.15–0.25% polysorbate 80, with pH 4.0–4.6. ASCENIV contains ≤ 200 µg/mL of IgA.
Each plasma donation used for the manufacture of ASCENIV is collected from FDA-licensed facilities. Plasma donations must test negative for hepatitis B virus (HBV) surface antigen (HBsAg), antibodies to human immunodeficiency virus (HIV) strains 1 and 2 (anti-HIV-1/2), and antibodies to the hepatitis C virus (anti-HCV) as determined by enzyme immunoassay (EIA). In addition, each plasma unit must test negative and/or non-reactive for HIV RNA, HCV RNA, HBV DNA, Hepatitis A Virus (HAV) RNA, and Parvovirus B19 (B19 virus) DNA as determined by Nucleic Acid Amplification Testing (NAT) of plasma minipools. NATs for HIV, HAV, HBV, HCV and B19 virus DNA are also performed on a sample of the manufacturing pool. The limit for B19 virus DNA in a manufacturing pool is set not to exceed 10 4 IU/mL and all other NAT results must be negative.
The manufacturing process of ASCENIV employs three steps to remove/inactivate adventitious viruses to minimize the risk of virus transmission. The steps are "Precipitation and removal of fraction III" during cold ethanol fractionation, classical "solvent/detergent treatment" and "35 nm virus filtration." In compliance with current guidelines, the steps have been separately validated in a series of in vitro experiments for their capacity to inactivate or remove both enveloped and nonenveloped viruses.
Precipitation and removal of fraction III removes both enveloped and non- enveloped viruses, solvent/detergent treatment represents a virus inactivation step for enveloped viruses, and 35 nm virus filtration removes both enveloped and non-enveloped viruses by size exclusion. In addition to the steps above, low pH during several steps of the production process contributes to virus inactivation. The results of virus validation studies for ASCENIV are shown in Table 3, expressed as log 10 reduction factors.
Table 3: Virus Validation Data for ASCENIV|
*without depth filtration | |||||||||
|
Virus Reduction (log 10) | |||||||||
|
Virus Type Family |
Enveloped Viruses |
Non-enveloped Viruses | |||||||
|
Retro |
Flavi |
Herpes |
Parvo |
Picorna |
Polyoma | ||||
|
Step / Test Virus |
HIV |
BVDV |
SinV |
WNV |
PRV |
PPV |
BPV |
MEV |
SV40 |
|
Precipitation and |
|
1.87 * |
|
|
|
4.00 |
|
5.29 |
2.00 * |
|
TnBP/Triton X-100 |
|
|
|
|
|
|
|
|
|
|
35 nm Virus |
|
|
|
|
|
< 1.0 |
6.18 |
< 1.0 |
|
|
Total Clearance |
|
|
|
|
|
4.00 |
6.18 |
5.29 |
|
OVERDOSAGE SECTION
10 OVERDOSAGE
With intravenous administration, overdose may lead to fluid overload and hyperviscosity. Patients at risk of complications of fluid overload and hyperviscosity include elderly patients and those with cardiac or renal impairment.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ASCENIV is a replacement therapy for patients with primary humoral immunodeficiency (PI) (e.g. agammaglobulinemia, hypogammaglobulinemia, CVID, SCID).
The broad spectrum of neutralizing IgG antibodies against bacterial and viral pathogens and their toxins helps to avoid recurrent serious opportunistic infections. IgG antibodies are opsonins that increase phagocytosis and elimination of pathogens from the circulation. The mechanism of action has not been fully elucidated in PI.
12.2 Pharmacodynamics
ASCENIV contains mainly immunoglobulin G (IgG) with a broad spectrum of antibodies against various infectious agents, reflecting the IgG activity found in the donor population. ASCENIV which is prepared from pooled plasma from not less than 1,000 donors, has an IgG subclass distribution similar to that of native human plasma. Adequate doses of IGIV can restore an abnormally low IgG level to the normal range. Standard pharmacodynamics studies were not performed.
12.3 Pharmacokinetics
In a prospective, open-label, single-arm, multicenter clinical study, efficacy, safety and pharmacokinetics of ASCENIV were evaluated in 59 subjects with PI ( See Clinical Studies [14]). Serum concentrations of total IgG were measured in 30 subjects (four subjects, ages 7 to 16 years and 26 subjects from 17 to 74 years) following the seventh infusion for subjects on a 4-week dosing interval and the ninth infusion for subjects on a 3-week dosing interval. The dose of ASCENIV used in these subjects ranged from 291 mg/kg to 760 mg/kg. After the infusion, blood samples were taken until Day 28 after infusion for the 4-week dosing interval and until Day 21 after infusion for the 3-week dosing interval. Table 4 summarizes the Total IgG Pharmacokinetic Parameters of ASCENIV, based on serum concentration of total IgG. The mean ± SD half-life of ASCENIV was 28.5 ± 4.4 days for subjects on a 3-week dosing interval and 39.7 ± 11.6 days for subjects on a 4-week dosing interval for the 30 subjects in the pharmacokinetic subgroup. Although no systematic study was conducted to evaluate the effect of sex on the pharmacokinetics of ASCENIV, based on the small sample size (11 males and 19 females) the pharmacokinetics of ASCENIV was comparable between males and females. In adolescents, the pharmacokinetics of ASCENIV was comparable with adults. There were insufficient PK data in children younger than 12 years.
Table 4: Total IgG Pharmacokinetic Parameter Estimates (PK Population) in Subjects|
AUC tau = steady-state area under the plasma concentration versus time curve with tau = dosing interval; CL = total body clearance; C max = maximum concentration; C min = minimum concentration; CV = coefficient of variation; n = number of subjects; NA = not applicable; SD = standard deviation; T max = time of maximum concentration; t ½ = terminal half-life; V ss = Volume of distribution steady-state; a median (range) | ||||
|
3-week cycle ** (n = 10)** |
4-week cycle ** (n = 20)** | |||
|
Statistic |
Mean (SD) |
CV% |
Mean (SD) |
CV% |
|
Cmax (mg/dL) |
2,427 (452) |
18.6 |
2,227 (584) |
26.2 |
|
Cmin (mg/dL) |
1,152 (308) |
26.7 |
954 (245) |
25.7 |
|
**Tmax (h)**a |
2.93 (1.80, 4.52) |
NA |
2.78 (1.43, 99.1) |
NA |
|
AUCtau (d*******mg/dL)** |
32,128 (7,020) |
21.9 |
35,905 (9,351) |
26.0 |
|
t½ (d) |
28.47 (4.4) |
15.4 |
39.70 (11.6) |
29.1 |
|
CL (mL/d/kg) |
1.68 (0.4) |
25.4 |
1.47 (0.5) |
33.6 |
|
Vss(mL/kg) |
76.79 (13.5) |
17.5 |
89.57 (26.2) |
29.2 |
|
AUC (0-t) = steady-state area under the plasma concentration versus time curve with 0-t = dosing interval; CL = total body clearance; Cmax = maximum concentration; Cmin = minimum concentration; CV = coefficient of variation; N = number of subjects; SD = standard deviation; T max = time of maximum concentration; t ½ = terminal half-life; V z = Apparent Volume of distribution during terminal phase; | ||||||
|
3-week cycle |
4-week cycle | |||||
|
Statistic |
Mean (SD) |
CV% |
N |
Mean (SD) |
CV% |
N |
|
Cmax (mg/dL) |
1223 (297) |
24.2 |
10 |
1231 (453) |
37 |
20 |
|
Cmax (mg/dL) |
19 (31) |
166 |
10 |
46 (42) |
178 |
20 |
|
Tmax (h) |
3.04 (0.8) |
27 |
10 |
8 (22) |
282 |
20 |
|
AUC**(0-t)**** (d*mg/dL)** |
6604 (2913) |
44 |
10 |
7936 (3482) |
44 |
20 |
|
t½ (d) |
6 (2) |
41 |
5 |
10 (8) |
80 |
9 |
|
CL (mL/d/kg) |
9 (4) |
42 |
10 |
8 (5) |
61 |
20 |
|
Vz (mL/kg) |
82 (62) |
75 |
5 |
82 (35) |
43 |
9 |
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
A prospective, open-label, single-arm, multicenter trial assessed the efficacy, safety, and pharmacokinetics of ASCENIV in adult and pediatric subjects with PI. Study subjects were receiving regular IGIV replacement therapy, with a stable dose between 300 and 800 mg/kg for at least 3 months prior to participation in this trial. Subjects received an ASCENIV infusion administered every 3 or 4 weeks (both the dose and schedule depending on their prior therapy) for 12 months.
A total of 59 subjects were enrolled into the trial, 28 men and 31 women with a mean age of 42 years; 93% were Caucasian, 5% were Hispanic and 2% African American. Forty-eight subjects were adults (81%) between 17 and 74 years of age. There were 11 pediatric subjects ( see Pediatric Use [8.4]), and 11 subjects (18.6%) ≥65 years of age. The oldest subject was 74 years of age. The youngest subject was 3 years of age.
There were 19 subjects with a 3-week cycle and 40 subjects with a 4-week cycle. There were 45 subjects (76%) with common variable immunodeficiency (CVID) as their primary diagnosis, followed by X-linked Agammaglobulinemia (10%), Antibody Deficiencies and ‘Other’ (7% each). The modified intent-to- treat (mITT) population included 59 subjects and was used for efficacy analysis.
The study assessed the efficacy of ASCENIV in preventing serious bacterial infections (SBIs), defined as a rate of <1.0 cases of bacterial pneumonia, bacteremia/septicemia, osteomyelitis/septic arthritis, visceral abscess, and bacterial meningitis per person-year. Secondary efficacy parameters included time to first SBI and time to first infection of any kind/seriousness, days on antibiotics (excluding prophylaxis), days off school/work due to infections, all confirmed infections of any kind or seriousness, and hospitalizations due to infection.
During the 12-month study period, zero (0) serious acute bacterial infections occurred. Thus, the mean event rate of serious, acute, bacterial infections per year was 0.0 (with an upper 1-sided 99% confidence interval of <1.0 per subject year, which met the study’s primary efficacy endpoint).
Thirty-nine percent (39%) of subjects had days off work, school or daycare due to an infection. Of the infections reported, 1 resulted in hospitalization as a post-op local wound infection from elective surgery (see Table 6). The incidence and severity of infections in adolescents were similar to those in adult subjects.
Table 6: Summary of Efficacy Results in Subjects with PI|
SBI = serious bacterial infections. | |
|
Number of Subjects (mITT Population) |
59 |
|
Infections |
0 |
|
Antibiotic use due to infection****c |
37 (63%) |
|
Days off school/daycare/work due to infection |
23 (39%) |
|
Unscheduled Medical Visits due to infection |
24 (41%) |
|
Hospitalization due to infection |
1 (1.7%) |
REFERENCES SECTION
15 REFERENCES
- Gupta N, Ahmed I, Nissel-Horowitz S, Patel D, Mehrotra B. Intravenous gammaglobulin-associated acute renal failure. Am J Hematol 2001; 66:151-152.
- Cayco, A.V., M.A. Perazella, and J.P. Hayslett. Renal insufficiency after intravenous immune globulin therapy: a report of two cases and an analysis of the literature. J Am Soc Nephrol 1997; 8:1788-1794.
- Steinberger BA, Ford SM, Coleman TA. Intravenous immune globulin therapy results in post-infusional hyperproteinemia, increased serum viscosity, and pseudohyponatremia. Am J Hematol 2003; 73:97-100.
- Dalakas MC. High-dose intravenous immunoglobulin and serum viscosity: risk of precipitating thromboembolic events. Neurology 1994; 44:223-226.
- Woodruff RK, Grigg AP, Firkin FC, Smith IL. Fatal thrombotic events during treatment of autoimmune thrombocytopenia with intravenous immunoglobulin in elderly patients. Lancet 1986; 2:217-218.
- Wolberg AS, Kon RH, Monroe DM, Hoffman M. Coagulation factor XI is a contaminant in intravenous immunoglobulin preparations. Am J Hematol 2000; 65:30-34.
- Casteels-Van Daele, M., et al. Intravenous immune globulin and acute aseptic meningitis [letter]. N Engl J Med 1990; 323:614-615.
- Kato, E., et al. Administration of immune globulin associated with aseptic meningitis [letter]. Jama 1988; 259:3269-3271.
- Scribner, C.L., et al. Aseptic meningitis and intravenous immunoglobulin therapy [editorial, comment]. Ann Intern Med 1994; 121:305-306.
- Copelan EA, Stohm PL, Kennedy MS, Tutschka PJ. Hemolysis following intravenous immune globulin therapy. Transfusion 1986; 26:410-412.
- Thomas MJ, Misbah SA, Chapel HM, Jones M, Elrington G, Newsom-Davis J. Hemolysis after high-dose intravenous Ig. Blood 1993; 15:3789.
- Wilson JR, Bhoopalam N, Fisher M. Hemolytic anemia associated with intravenous immunoglobulin. Muscle & Nerve 1997; 20:1142-1145.
- Kessary-Shoham H, Levy Y, Shoenfeld Y, Lorber M, Gershon H. In vivo administration of intravenous immunoglobulin (IVIg) can lead to enhanced er ythrocyte sequestration. J Autoimmune 1999; 13:129-135.
- Rizk A, Gorson KC, Kenney L, Weinstein R. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion 2001; 41:264-268.
- Siber GA, Werner BG, Halsey NA, et al. Interference of immune globulin with measles and rubella immunization. J Pediatr 1993; 122:204-211.
- Salisbury D, Ramsay M, Noakes K, eds. Immunisation against infectious disease. The Stationery Office (TSO), London: UK Department of Health; 2009:426.
- Hammarstrom L, Smith CIE. Placental transfer of intravenous immunoglobulin. Lancet 1986; 1:681.
- Sidiropoulos D, Herrmann U, Morell A, von Muralt G, Barandun S. Transplacental passage of intravenous immunoglobulin in the last trimester of pregnancy. J Pediatr 1986; 109:505-508.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
ASCENIV is supplied in a single-use, tamper-evident vial. The components used in the packaging for ASCENIV are not made with natural rubber latex. ASCENIV is supplied in 50 mL size containing 5 grams of protein (NDC 69800-0250-1).
- Store at 2 to 8°C (36 to 46°F) for up to 36 months from the date of manufacture. Do not freeze.
- Product may be stored up to 4 weeks at ≤ 25° C (77° F). After storage at room temperature product must be used or discarded.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Instruct patients taking ASCENIV to immediately report symptoms of:
- Thrombosis which includes pain and/or swelling of an arm or legs/feet with warmth over the affected area, discoloration of an arm or leg, unexplained shortness of breath, acute chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, numbness or weakness on one side of the body (see Warning and Precaution [5.2]).
- Acute Renal Dysfunction and Acute Renal Failure which includes decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of breath. Such symptoms may suggest kidney damage (see Boxed Warning, Warnings and Precautions [5.3]).
- Aseptic Meningitis Syndrome (AMS) which includes severe headache, neck stiffness, drowsiness, fever, sensitivity to light, painful eye movements, nausea and vomiting (see Warnings and Precautions [5.5]).
- Hemolysis which includes fatigue, increased heart rate, yellowing of skin or eyes, dark- colored urine (see Warnings and Precautions [5.5]).
- Transfusion-Related Acute Lung Injury (TRALI) which includes trouble breathing, chest pain, blue lips or extremities, fever (see Warnings and Precautions [5.7])
Inform patients that ASCENIV:
- Is made from human plasma and may contain infectious agents that can cause disease. While the risk that ASCENIV can transmit an infection has been reduced by screening plasma donors for prior exposure, testing donated plasma, and inactivating or removing certain viruses during manufacturing, patients should report any symptoms that concern them (see Description [11] and Warnings and Precautions [5]).
- Can interfere with their immune response to live viral vaccines (e.g., measles, mumps, rubella, and varicella). Instruct patients to notify their healthcare professional of this potential interaction when they are receiving vaccinations (see Drug Interactions [7]).
Manufactured by ADMA Biologics
Boca Raton, FL 33487 USA
U.S. License No. 2019
RM-5640 Rev.000
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
No human data are available to indicate the presence or absence of drug- associated risk. Animal reproduction studies have not been conducted with ASCENIV. It is not known whether ASCENIV can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Immune globulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20% respectively. ASCENIV should be given to pregnant women only if clearly needed. 17,18
8.2 Lactation
Risk Summary
No human data are available to indicate the presence or absence drug- associated risk. The developmental and health benefits of breast feeding should be considered along with the mother’s clinical need for ASCENIV and any potential adverse effects on the breast-fed infant from ASCENIV or from the underlying maternal condition.
8.4 Pediatric Use
ASCENIV was evaluated in 11 pediatric subjects (6 children less than 12 years and 5 adolescents age 12 – 16 years) with primary humoral immunodeficiency (PI). The pharmacokinetic (PK), safety, and effectiveness profile of ASCENIV in adolescent subjects appeared to be comparable to that demonstrated in adult subjects. There are insufficient PK, safety, and effectiveness data from pediatric subjects younger than 12 years. Safety and effectiveness has not been studied in pediatric patients with PI who are under the age of 3 years ( see Clinical Studies [14]).
8.5 Geriatric Use
Clinical studies of ASCENIV did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Geriatric Use: In patients over age 65 or in any patient at risk of developing renal insufficiency, do not exceed the recommended dose, and infuse ASCENIV at the minimum infusion rate practicable. [8.5]
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No animal studies were conducted to evaluate the carcinogenic or mutagenic effects of ASCENIV or its effects on fertility.
13.2 Animal Toxicology and/or Pharmacology
No animal studies were conducted to evaluate possible toxicity of ASCENIV.
ASCENIV contains Polysorbate 80; Intravenous administrations of Polysorbate 80 in multiple species have been linked with a decrease in blood pressure. In rats, single doses of Polysorbate 80 that were up to 25 times higher than the amount from 800 mg/kg ASCENIV resulted in an increase of liver enzymes and total bilirubin.
