Trimipramine Maleate
TRIMIPRAMINE MALEATE CAPSULES
4f31df66-7dc2-1f04-e054-00144ff88e88
HUMAN PRESCRIPTION DRUG LABEL
Mar 15, 2024
Breckenridge Pharmaceutical, Inc.
DUNS: 119102319
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Trimipramine Maleate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (10)
Trimipramine Maleate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Trimipramine Maleate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (13)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
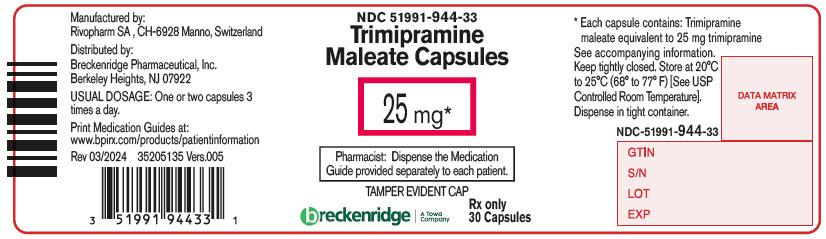
PRINCIPAL DISPLAY PANEL - 25 mg Capsule Bottle Label
NDC 51991-944-33
Trimipramine
Maleate Capsules
25 mg*
Pharmacist: Dispense the Medication
Guide provided separately to each patient.
TAMPER EVIDENT CAP
breckenridge
A Towa
Company
Rx only
30 Capsules
BOXED WARNING SECTION
Suicidality and Antidepressant Drugs
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
Trimipramine maleate capsules are indicated for the relief of symptoms of depression. Endogenous depression is more likely to be alleviated than other depressive states. In studies with neurotic outpatients, the drug appeared to be equivalent to amitriptyline in the less-depressed patients but somewhat less effective than amitriptyline in the more severely depressed patients. In hospitalized depressed patients, trimipramine and imipramine were equally effective in relieving depression.
CONTRAINDICATIONS SECTION
CONTRAINDICATIONS
Monoamine Oxidase Inhibitors (MAOIs)
The use of MAOIs intended to treat psychiatric disorders with trimipramine maleate capsules or within 14 days of stopping treatment with trimipramine maleate capsules is contraindicated because of an increased risk of serotonin syndrome. The use of trimipramine maleate capsules within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated (see WARNINGS andDOSAGE AND ADMINISTRATION).
Starting trimipramine maleate capsules in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome (seeWARNINGS and DOSAGE AND ADMINISTRATION).
Hypersensitivity to Tricyclic Antidepressants
Cross-sensitivity between trimipramine maleate capsules and other dibenzazepines is a possibility.
Myocardial Infarction
The drug is contraindicated during the acute recovery period after a myocardial infarction.
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
Note: The pharmacological similarities among the tricyclic antidepressants require that each of the reactions be considered when trimipramine maleate capsules are administered. Some of the adverse reactions included in this listing have not in fact been reported with trimipramine maleate capsules.
Cardiovascular
Hypotension, hypertension, tachycardia, palpitation, myocardial infarction, arrhythmias, heart block, stroke.
Psychiatric
Confusional states (especially the elderly) with hallucinations, disorientation, delusions; anxiety, restlessness, agitation; insomnia and nightmares; hypomania; exacerbation of psychosis.
Neurological
Numbness, tingling, paresthesias of extremities; incoordination, ataxia, tremors; peripheral neuropathy; extrapyramidal symptoms; seizures, alterations in EEG patterns; tinnitus; syndrome of inappropriate ADH (antidiuretic hormone) secretion.
Anticholinergic
Dry mouth and, rarely, associated sublingual adenitis; blurred vision, disturbances of accommodation, mydriasis, constipation, paralytic ileus; urinary retention, delayed micturition, dilation of the urinary tract.
Allergic
Skin rash, petechiae, urticaria, itching, photosensitization, edema of face and tongue.
Hematologic
Bone marrow depression including agranulocytosis, eosinophilia; purpura; thrombocytopenia. Leukocyte and differential counts should be performed in any patient who develops fever and sore throat during therapy; the drug should be discontinued if there is evidence of pathological neutrophil depression.
Gastrointestinal
Nausea and vomiting, anorexia, epigastric distress, diarrhea, peculiar taste, stomatitis, abdominal cramps, black tongue.
Endocrine
Gynecomastia in the male; breast enlargement and galactorrhea in the female; increased or decreased libido, impotence; testicular swelling; elevation or depression of blood sugar levels.
Other
Jaundice (simulating obstructive); altered liver function; weight gain or loss; perspiration; flushing; urinary frequency; drowsiness, dizziness, weakness, and fatigue; headache; parotid swelling; alopecia.
Withdrawal Symptoms
Though not indicative of addiction, abrupt cessation of treatment after prolonged therapy may produce nausea, headache, and malaise.
SPL UNCLASSIFIED SECTION
Distributed by:
Breckenridge Pharmaceutical, Inc.
Berkeley Heights, NJ 07922
Manufactured by:
Rivopharm SA
6928, Manno, Switzerland
To report SUSPECTED ADVERSE REACTIONS, contact Breckenridge Pharmaceutical, Inc. at 1-800-367-3395, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Revised: March 2024
DESCRIPTION SECTION
DESCRIPTION
Trimipramine maleate is 5-(3-dimethylamino-2-methylpropyl)-10,11-dihydro-5H-dibenz (b,f) azepine acid maleate (racemic form).
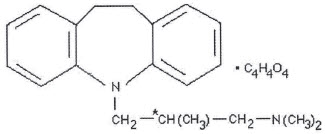
Molecular Formula: C20H26N2 ∙ C4H4O4 Molecular Weight: 410.5
Trimipramine maleate capsules contain trimipramine maleate equivalent to 25 mg, 50 mg, or 100 mg of trimipramine as the base. The inactive ingredients present are lactose monohydrate and magnesium stearate. The capsule shell contains D&C Yellow 10 (25 mg), FD&C Blue 1 (25 mg, 50 mg and 100 mg), FD&C Yellow 6 (25 mg, 50 mg), D&C Red 28 (50 mg), FD&C Red 40 (50 mg), gelatin and titanium dioxide. The capsules are imprinted in black ink that contains shellac glaze, iron oxide black, propylene glycol and ammonium hydroxide.
Trimipramine maleate is prepared as a racemic mixture which can be resolved into levorotatory and dextrorotatory isomers. The asymmetric center responsible for optical isomerism is marked in the formula by an asterisk.
Trimipramine maleate is an almost odorless, white or slightly cream-colored, crystalline substance, melting at 140°-144° C. It is very slightly soluble in ether and water, is slightly soluble in ethyl alcohol and acetone, and freely soluble in chloroform and methanol at 20° C.
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
Trimipramine maleate capsules are an antidepressant with an anxiety-reducing sedative component to its action. The mode of action of trimipramine maleate capsules on the central nervous system is not known. However, unlike amphetamine-type compounds it does not act primarily by stimulation of the central nervous system. It does not act by inhibition of the monoamine oxidase system.
The single-dose pharmacokinetics of trimipramine were evaluated in a comparative study of 24 elderly subjects and 24 younger subjects; no clinically relevant differences were demonstrated based on age or gender.
WARNINGS SECTION
WARNINGS
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (aged 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analysis of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders including a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable with age strada and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
Table 1|
Age Range |
Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|---|---|
|
Increases Compared to Placebo | |
|
< 18 |
14 additional cases |
|
18-24 |
5 additional cases |
|
Decreases Compared to Placebo | |
|
25-64 |
1 fewer case |
|
≥ 65 |
6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo- controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and non- psychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for trimipramine maleate capsules should be written for the smallest quantity of capsules consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depression symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that trimipramine maleate capsules are not approved for use in treating bipolar depression.
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including trimipramine maleate capsules, alone, but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. John's wort) and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of trimipramine maleate capsules with MAOIs intended to treat psychiatric disorders is contraindicated. Trimipramine maleate capsules should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking trimipramine maleate capsules. Trimipramine maleate capsules should be discontinued before initiating treatment with the MAOI (seeCONTRAINDICATIONS andDOSAGE AND ADMINISTRATION).
If concomitant use of trimipramine maleate capsules with other serotonergic drugs, including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan, and St. John's wort is clinically warranted, patients should be made aware of a potential increased risk for serotonin syndrome, particularly during treatment initiation and dose increases.
Treatment with trimipramine maleate capsules and any concomitant serotonergic agents should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including trimipramine maleate capsules may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
General Consideration for Use
Extreme caution should be used when this drug is given to patients with any evidence of cardiovascular disease because of the possibility of conduction defects, arrhythmias, myocardial infarction, strokes, and tachycardia. Caution is advised in patients with history of urinary retention because of the drug's anticholinergic properties; hyperthyroid patients or those on thyroid medication because of the possibility of cardiovascular toxicity; patients with a history of seizure disorder, because this drug has been shown to lower the seizure threshold; patients receiving guanethidine or similar agents, since trimipramine maleate capsules (trimipramine maleate) may block the pharmacologic effects of these drugs.
Since the drug may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as operating an automobile or machinery, the patient should be cautioned accordingly.
OVERDOSAGE SECTION
OVERDOSAGE1
Deaths may occur from overdosage with this class of drugs. Multiple drug ingestion (including alcohol) is common in deliberate tricyclic antidepressant overdose. As the management is complex and changing, it is recommended that the physician contact a poison control center for current information on treatment. Signs and symptoms of toxicity develop rapidly after tricyclic antidepressant overdose, therefore, hospital monitoring is required as soon as possible.
Manifestations
Critical manifestations of overdose include: cardiac dysrhythmias, severe hypotension, convulsions, and CNS depression, including coma. Changes in the electrocardiogram, particularly in QRS axis or width, are clinically significant indicators of tricyclic antidepressant toxicity.
Other signs of overdose may include: confusion, disturbed concentration, transient visual hallucinations, dilated pupils, agitation, hyperactive reflexes, stupor, drowsiness, muscle rigidity, vomiting, hypothermia, hyperpyrexia, or any of the symptoms listed underADVERSE REACTIONS.
Management
General
Obtain an ECG and immediately initiate cardiac monitoring. Protect the patient's airway, establish an intravenous line and initiate gastric decontamination. A minimum of six hours of observation with cardiac monitoring and observation for signs of CNS or respiratory depression, hypotension, cardiac dysrhythmias and/or conduction blocks, and seizures is necessary. If signs of toxicity occur at any time during this period, extended monitoring is required. There are case reports of patients succumbing to fatal dysrhythmias late after overdose; these patients had clinical evidence of significant poisoning prior to death and most received inadequate gastrointestinal decontamination. Plasma drug levels may not reflect the severity of the poisoning. Therefore, monitoring of plasma drug levels alone should not guide management of the patient.
Gastrointestinal Decontamination
All patients suspected of tricyclic antidepressant overdose should receive gastrointestinal decontamination. This should include large volume gastric lavage followed by activated charcoal. If consciousness is impaired, the airway should be secured prior to lavage. Emesis is contraindicated.
Cardiovascular
A maximal limb-lead QRS duration of ≥ 0.10 seconds has been associated with an increased incidence of seizures. A QRS duration of ≥ 0.16 seconds has been associated with an increased incidence of ventricular dysrhythmias. Intravenous sodium bicarbonate should be used to maintain the serum pH in the range of 7.45 to 7.55. If the pH response is inadequate, hyperventilation may also be used. Concomitant use of hyperventilation and sodium bicarbonate should be done with extreme caution, with frequent pH monitoring. A pH > 7.60 or a pCO2 < 20 mm Hg is undesirable. Dysrhythmias unresponsive to sodium bicarbonate therapy/hyperventilation may respond to lidocaine, bretylium or phenytoin. Type 1A and 1C antiarrhythmics are generally contraindicated (e.g., quinidine, disopyramide, and procainamide).
In rare instances, hemoperfusion may be beneficial in acute refractory cardiovascular instability in patients with acute toxicity. However, hemodialysis, peritoneal dialysis, exchange transfusions, and forced diuresis generally have been reported as ineffective in tricyclic antidepressant poisoning.
CNS
In patients with CNS depression, early intubation is advised because of the potential for abrupt deterioration. Seizures should be controlled with benzodiazepines, or if these are ineffective, other anticonvulsants (e.g., phenobarbital, phenytoin). Physostigmine is not recommended except to treat life-threatening symptoms that have been unresponsive to other therapies, and then only in consultation with a poison control center.
Psychiatric Follow-up
Since overdosage is often deliberate, patients may attempt suicide by other means during the recovery phase. Psychiatric referral may be appropriate.
Pediatric Management
The principles of management of child and adult overdosages are similar. It is strongly recommended that the physician contact the local poison control center for specific pediatric treatment.
1
Poisindex® Toxicologic Management. Topic: Antidepressants, Tricyclic Micromedex Inc. Vol. 85.
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
Dosage should be initiated at a low level and increased gradually, noting carefully the clinical response and any evidence of intolerance.
Lower dosages are recommended for elderly patients and adolescents. Lower dosages are also recommended for outpatients as compared to hospitalized patients who will be under close supervision. It is not possible to prescribe a single dosage schedule of trimipramine maleate capsules that will be therapeutically effective in all patients. The physical psychodynamic factors contributing to depressive symptomatology are very complex; spontaneous remissions or exacerbations of depressive symptoms may occur with or without drug therapy. Consequently, the recommended dosage regimens are furnished as a guide which may be modified by factors such as the age of the patient, chronicity and severity of the disease, medical condition of the patient, and degree of psychotherapeutic support.
Most antidepressant drugs have a lag period of ten days to four weeks before a therapeutic response is noted. Increasing the dose will not shorten this period but rather increase the incidence of adverse reactions.
Usual Adult Dose
Outpatients and Office Patients
Initially, 75 mg/day in divided doses, increased to 150 mg/day. Dosages over 200 mg/day are not recommended. Maintenance therapy is in the range of 50 to 150 mg/day. For convenient therapy and to facilitate patient compliance, the total dosage requirement may be given at bedtime.
Hospitalized Patients
Initially, 100 mg/day in divided doses. This may be increased gradually in a few days to 200 mg/day, depending upon individual response and tolerance. If improvement does not occur in 2 to 3 weeks, the dose may be increased to the maximum recommended dose of 250 to 300 mg/day.
Adolescent and Geriatric Patients
Initially, a dose of 50 mg/day is recommended, with gradual increments up to 100 mg/day, depending upon patient response and tolerance.
Maintenance
Following remission, maintenance medication may be required for a longer period of time, at the lowest dose that will maintain remission. Maintenance therapy is preferably administered as a single dose at bedtime. To minimize relapse, maintenance therapy should be continued for about three months.
Switching a Patient To or From a Monoamine Oxidase Inhibitor (MAOI)
Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with trimipramine maleate capsules. Conversely, at least 14 days should be allowed after stopping trimipramine maleate capsules before starting an MAOI intended to treat psychiatric disorders (seeCONTRAINDICATIONS).
Use of Trimipramine Maleate Capsules With Other MAOIs, Such as Linezolid or
Methylene Blue
Do not start trimipramine maleate capsules in a patient who is being treated with linezolid or intravenous methylene blue because there is increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered (seeCONTRAINDICATIONS).
In some cases, a patient already receiving therapy with trimipramine maleate capsules may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, trimipramine maleate capsules should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with trimipramine maleate capsules may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue (seeWARNINGS).
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with trimipramine maleate capsules is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use (seeWARNINGS).
SPL MEDGUIDE SECTION
Medication Guide
Trimipramine Maleate (trye-MIP-ra-meen MAL-ee-ate)
Capsules
Antidepressant Medicines, Depression and other Serious Mental Illnesses, and Suicidal Thoughts or Actions
Dispense with Medication Guide available at: www.bpirx.com/products/patientinformation
Read the Medication Guide that comes with you or your family member's antidepressant medicine. This Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines.Talk to your, or your family member's, healthcare provider about:
- all risks and benefits of treatment with antidepressant medicines
- all treatment choices for depression or other serious mental illness
What is the most important information I should know about antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions?
1. Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment.
2. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic- depressive illness) or suicidal thoughts or actions.
3. How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
- Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.
- Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
- Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
Visual Problems
- eye pain
- changes in vision
- swelling or redness in or around the eye
Only some people are at risk for these problems. You may want to undergo an eye examination to see if you are at risk and receive preventative treatment if you are.
Who should not take trimipramine maleate capsules?
- Do not take trimipramine maleate capsules if you take a monoamine oxidase inhibitor (MAOI). Ask your healthcare provider or pharmacist if you are not sure if you take an MAOI, including the antibiotic linezolid.
- Do not take an MAOI within 2 weeks of stopping trimipramine maleate capsules unless directed to do so by your physician.
- Do not start trimipramine maleate capsules if you stopped taking an MAOI in the last 2 weeks unless directed to do so by your physician.
What else do I need to know about antidepressant medicines?
*Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms. *Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants. *Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member. *Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider. *Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child's healthcare provider for more information.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Revised: March 2024
Distributed by:
Breckenridge Pharmaceutical, Inc.
Berkeley Heights, NJ 07922
Manufactured by:
Rivopharm SA
6928, Manno, Switzerland
PRECAUTIONS SECTION
PRECAUTIONS
General
The possibility of suicide is inherent in any severely depressed patient and persists until a significant remission occurs. When a patient with a serious suicidal potential is not hospitalized, the prescription should be for the smallest amount feasible.
In schizophrenic patients activation of the psychosis may occur and require reduction of dosage or the addition of a major tranquilizer to the therapeutic regimen.
Manic or hypomanic episodes may occur in some patients, in particular those with cyclic-type disorders. In some cases therapy with trimipramine maleate capsules must be discontinued until the episode is relieved, after which therapy may be reinstituted at lower dosages if still required.
Concurrent administration of trimipramine maleate capsules and electroshock therapy may increase the hazards of therapy. Such treatment should be limited to those patients for whom it is essential. When possible, discontinue the drug for several days prior to elective surgery.
Trimipramine maleate capsules should be used with caution in patients with impaired liver function.
Chronic animal studies showed occasional occurrence of hepatic congestion, fatty infiltration, or increased serum liver enzymes at the highest dose of 60 mg/kg/day.
Both elevation and lowering of blood sugar have been reported with tricyclic antidepressants.
Information for Patients
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with trimipramine maleate capsules and should counsel them in its appropriate use. A patient Medication Guide about "Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions" is available for trimipramine maleate capsules. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking trimipramine maleate capsules.
Clinical Worsening and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Patients should be advised that taking trimipramine maleate capsules can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle closure glaucoma. Pre-existing glaucoma is almost always open-angle glaucoma because angle closure glaucoma, when diagnosed, can be treated definitively with iridectomy. Open-angle glaucoma is not a risk factor for angle closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle closure, and have a prophylactic procedure (e.g., iridectomy), if they are susceptible.
Drug Interactions
Cimetidine
There is evidence that cimetidine inhibits the elimination of tricyclic antidepressants. Downward adjustment of trimipramine maleate capsules dosage may be required if cimetidine therapy is initiated; upward adjustment if cimetidine therapy is discontinued.
Alcohol
Patients should be warned that the concomitant use of alcoholic beverages may be associated with exaggerated effects.
Catecholamines/Anticholinergics
It has been reported that tricyclic antidepressants can potentiate the effects of catecholamines. Similarly, atropine-like effects may be more pronounced in patients receiving anticholinergic therapy. Therefore, particular care should be exercised when it is necessary to administer tricyclic antidepressants with sympathomimetic amines, local decongestants, local anesthetics containing epinephrine, atropine or drugs with an anticholinergic effect. In resistant cases of depression in adults, a dose of 2.5 mg/kg/day may have to be exceeded. If a higher dose is needed, ECG monitoring should be maintained during the initiation of therapy and at appropriate intervals during stabilization of dose.
Drugs Metabolized by P450 2D6
The biochemical activity of the drug metabolizing isozyme cytochrome P450 2D6 (debrisoquin hydroxylase) is reduced in a subset of the caucasian population (about 7-10% of caucasians are so called "poor metabolizers"); reliable estimates of the prevalence of reduced P450 2D6 isozyme activity among Asian, African, and other populations are not yet available. Poor metabolizers have higher than expected plasma concentrations of tricyclic antidepressants (TCAs) when given usual doses. Depending on the fraction of drug metabolized by P450 2D6, the increase in plasma concentration may be small, or quite large (8 fold increase in plasma AUC of the TCA).
In addition, certain drugs inhibit the activity of the isozyme and make normal metabolizers resemble poor metabolizers. An individual who is stable on a given dose of TCA may become abruptly toxic when given one of these inhibiting drugs as concomitant therapy. The drugs that inhibit cytochrome P450 2D6 include some that are not metabolized by the enzyme (quinidine; cimetidine) and many that are substrates for P450 2D6 (many other antidepressants, phenothiazines, and the Type 1C antiarrhythmics propafenone and flecainide). While all the selective serotonin reuptake inhibitors (SSRIs), e.g., fluoxetine, sertraline, and paroxetine, inhibit P450 2D6, they may vary in the extent of inhibition. The extent to which SSRI TCA interactions may pose clinical problems will depend on the degree of inhibition and the pharmacokinetics of the SSRI involved. Nevertheless, caution is indicated in the co-administration of TCAs with any of the SSRIs and also in switching from one class to the other. Of particular importance, sufficient time must elapse before initiating TCA treatment in a patient being withdrawn from fluoxetine, given the long half-life of the parent and active metabolite (at least 5 weeks may be necessary).
Concomitant use of tricyclic antidepressants with drugs that can inhibit cytochrome P450 2D6 may require lower doses than usually prescribed for either the tricyclic antidepressant or the other drug. Furthermore, whenever one of these other drugs is withdrawn from co-therapy, an increased dose of tricyclic antidepressant may be required. It is desirable to monitor TCA plasma levels whenever a TCA is going to be co-administered with another drug known to be an inhibitor of P450 2D6.
Monoamine Oxidase Inhibitors (MAOIs)
(SeeCONTRAINDICATIONS,WARNINGS, andDOSAGE AND ADMINISTRATION.)
Serotonergic Drugs
(SeeCONTRAINDICATIONS,WARNINGS, andDOSAGE AND ADMINISTRATION.)
Carcinogenesis, Mutagenesis, Impairment of Fertility
Semen studies in man (four schizophrenics and nine normal volunteers) revealed no significant changes in sperm morphology. It is recognized that drugs having a parasympathetic effect, including tricyclic antidepressants, may alter the ejaculatory response.
Chronic animal studies showed occasional evidence of degeneration of seminiferous tubules at the highest dose of 60 mg/kg/day.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Trimipramine maleate capsules have shown evidence of embryotoxicity and/or increased incidence of major anomalies in rats or rabbits at doses 20 times the human dose. There are no adequate and well-controlled studies in pregnant women. Trimipramine maleate capsules should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (seeBOXED WARNING andWARNINGS -Clinical Worsening and Suicide Risk). Anyone considering the use of trimipramine maleate capsules in a child or adolescent must balance the potential risks with the clinical need.
Geriatric Use
Clinical studies of trimipramine maleate capsules (trimipramine maleate) were not adequate to determine whether subjects aged 65 and over respond differently from younger subjects.
The pharmacokinetics of trimipramine were not substantially altered in the elderly (seeCLINICAL PHARMACOLOGY).
Trimipramine maleate capsules are known to be substantially excreted by the kidney. Clinical circumstances, some of which may be more common in the elderly, such as hepatic or renal impairment, should be considered (see PRECAUTIONS -General).
Greater sensitivity (e.g., confusional states, sedation) of some older individuals cannot be ruled out (seeADVERSE REACTIONS). In general, dose selection for an elderly patient should be cautious, usually starting at a lower dose (seeDOSAGE AND ADMINISTRATION).
HOW SUPPLIED SECTION
HOW SUPPLIED
Trimipramine Maleate Capsules
|
25 mg - #3 |
Capsules, with a yellow opaque body and blue opaque cap in bottles of 100 (NDC
51991-944-01) and in bottles of 30 (NDC 51991-944-33). |
|
50 mg - #2 |
Capsules, with an orange opaque body and blue opaque cap in bottles of 100
(NDC 51991-945-01)and in bottles of 30 (NDC 51991-945-33). |
|
100 mg - #0 |
Capsules, with a white opaque body and light blue opaque cap in bottles of 100
(NDC 51991-946-01) and in bottles of 30 (NDC 51991-946-33). |
Store at 20°-25°C (68°-77°F) [See USP Controlled Room Temperature].
Keep bottles tightly closed.
Dispense in a tight container.
Dispense with Medication Guide available at: www.bpirx.com/products/patientinformation
