Osphena
These highlights do not include all the information needed to use OSPHENA safely and effectively. See full prescribing information for OSPHENA. OSPHENA (ospemifene) tablets, for oral use Initial U.S. Approval: 2013
8462d6ab-e3cd-4efa-a360-75bf8f917287
HUMAN PRESCRIPTION DRUG LABEL
Mar 16, 2023
Shionogi Inc.
DUNS: 098241610
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Ospemifene
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (13)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
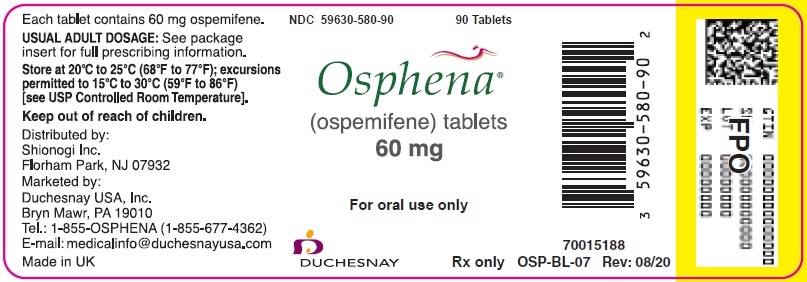
PRINCIPAL DISPLAY PANEL - 60 mg Tablet Bottle Label
NDC 59630-580-90
90 Tablets
Osphena®
(ospemifene) tablets
60 mg
For oral use only
DUCHESNAY
Rx only
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
OSPHENA is indicated for:
1.1 The Treatment of Moderate to Severe Dyspareunia, a Symptom of Vulvar
and Vaginal Atrophy, Due to Menopause.
1.2 The Treatment of Moderate to Severe Vaginal Dryness, a Symptom of
Vulvar and Vaginal Atrophy, Due to Menopause.
OSPHENA is an estrogen agonist/antagonist indicated for:
- The treatment of moderate to severe dyspareunia, a symptom of vulvar and vaginal atrophy, due to menopause. (1.1)
- The treatment of moderate to severe vaginal dryness, a symptom of vulvar and vaginal atrophy, due to menopause. (1.2)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Disorders
Risk factors for cardiovascular disorders, arterial vascular disease (for example, hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (VTE) (for example, personal history or family history of VTE, obesity, and systemic lupus erythematosus) should be managed appropriately.
Stroke
In the clinical trials for OSPHENA (duration of treatment up to 15 months), the incidence rates of thromboembolic and hemorrhagic stroke were 1.13 and 3.39 per thousand women years, respectively in OSPHENA 60 mg treatment group and 3.15 and 0 per thousand women years in placebo.
Should thromboembolic or hemorrhagic stroke occur or be suspected, OSPHENA should be discontinued immediately.
In the WHI estrogen-alone substudy, a statistically significant increased risk of stroke was reported in women 50 to 79 years of age receiving daily CE (0.625 mg)-alone compared to women in the same age group receiving placebo (45 versus 33 per ten thousand women years). The increase in risk was demonstrated in year 1 and persisted.
Coronary Heart Disease
In the OSPHENA clinical trials, two cases of myocardial infarction (MI) occurred in women receiving 60 mg of ospemifene.
In the WHI estrogen-alone substudy, no overall effect on coronary heart disease (CHD) events (defined as nonfatal MI, silent MI, or CHD death) was reported in women receiving estrogen-alone compared to placebo.
Venous Thromboembolism
In the OSPHENA clinical trials, two cases of DVT occurred in women receiving OSPHENA 60 mg. Should a VTE occur or be suspected, OSPHENA should be discontinued immediately.
If feasible, OSPHENA should be discontinued at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
In the WHI estrogen-alone substudy, the risk of VTE (DVT and PE) was increased for women receiving daily CE (0.625 mg)-alone compared to placebo (30 versus 22 per ten thousand women years), although only the increased risk of DVT reached statistical significance (23 versus 15 per ten thousand women years). The increase in VTE risk was demonstrated during the first 2 years.
5.2 Malignant Neoplasms
Endometrial Cancer
OSPHENA is an estrogen agonist/antagonist with tissue selective effects. In the endometrium, OSPHENA has agonistic effects. In the OSPHENA clinical trials (60 mg treatment group), no cases of endometrial cancer were seen with exposure up to 52 weeks. There was a single case of simple hyperplasia without atypia. Endometrial thickening equal to 5 mm or greater was seen in the OSPHENA up to 52 weeks treatment groups at a rate of 101.4 per thousand women vs. 20.9 per thousand women for placebo. The incidence of any type of proliferative (weakly plus active plus disordered) endometrium was 26.3 per thousand women in the OSPHENA up to 52 weeks treatment groups vs. 0 per thousand women for placebo. Uterine polyps occurred at an incidence of 19.6 per thousand women in the OSPHENA up to 52 weeks treatment groups vs. 8.3 per thousand women for placebo.
An increased risk of endometrial cancer has been reported with the use of unopposed estrogen therapy in a woman with a uterus. The reported endometrial cancer risk among unopposed estrogen users is about 2 to 12 times greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with the use of estrogens for less than 1 year. The greatest risk appears to be associated with prolonged use, with increased risks of 15- to 24-fold for 5 to 10 years or more. This risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued. Adding a progestin to postmenopausal estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. There are, however, possible risks that may be associated with the use of progestins with estrogens compared to estrogen-alone regimens. These include an increased risk of breast cancer. The use of progestins with OSPHENA therapy was not evaluated in the clinical trials.
Clinical surveillance of all women using OSPHENA is important. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding.
Breast Cancer
OSPHENA 60 mg has not been adequately studied in women with breast cancer; therefore, it should not be used in women with known or suspected breast cancer.
5.3 Severe Hepatic Impairment
OSPHENA should not be used in women with severe hepatic impairment [see Use in Specific Populations (8.7), and Clinical Pharmacology (12.3)].
- Venous Thromboembolism: Risk of DVT and pulmonary embolism (5.1)
- Known, suspected, or history of breast cancer (5.2)
- Severe Hepatic Impairment (5.3, 8.7, 12.3)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
OSPHENA is primarily metabolized by CYP3A4 and CYP2C9. CYP2C19 and other pathways contribute to the metabolism of ospemifene.
7.1 Estrogens and Estrogen Agonist/Antagonist
Do not use OSPHENA concomitantly with estrogens and estrogen agonists/antagonists. The safety of concomitant use of OSPHENA with estrogens and estrogen agonists/antagonists has not been studied.
7.2 Fluconazole
Fluconazole, a moderate CYP3A / strong CYP2C9 / moderate CYP2C19 inhibitor, should not be used with OSPHENA. Fluconazole increases the systemic exposure of ospemifene by 2.7-fold. Administration of fluconazole with ospemifene may increase the risk of OSPHENA-related adverse reactions [see Clinical Pharmacology (12.3)].
7.3 Rifampin
Rifampin, a strong CYP3A4 / moderate CYP2C9 / moderate CYP2C19 inducer, decreases the systemic exposure of ospemifene by 58%. Therefore, co- administration of OSPHENA with drugs such as rifampin which induce CYP3A4, CYP2C9 and/or CYP2C19 activity would be expected to decrease the systemic exposure of ospemifene, which may decrease the clinical effect [see Clinical Pharmacology (12.3)].
7.4 Ketoconazole
Ketoconazole, a strong CYP3A4 inhibitor, increases the systemic exposure of ospemifene by 1.4-fold. Administration of ketoconazole chronically with ospemifene may increase the risk of OSPHENA-related adverse reactions [see Clinical Pharmacology (12.3)].
7.5 Warfarin
Repeated administration of ospemifene had no effect on the pharmacokinetics of a single 10 mg dose of warfarin. No study was conducted with multiple doses of warfarin. The effect of ospemifene on clotting time such as the International Normalized Ratio (INR) or prothrombin time (PT) was not studied [see Clinical Pharmacology (12.3)].
7.6 Highly Protein-Bound Drugs
Ospemifene is more than 99% bound to serum proteins and might affect the protein binding of other drugs. Use of OSPHENA with other drug products that are highly protein-bound may lead to increased exposure of either that drug or ospemifene [see Clinical Pharmacology (12.3)].
7.7 Multiple Enzyme Inhibition
Co-administration of OSPHENA with a drug known to inhibit CYP3A4 and CYP2C9 isoenzymes may increase the risk of OSPHENA-related adverse reactions.
- Do not use estrogens or estrogen agonist/antagonist concomitantly with OSPHENA. (7.1,12.3)
- Do not use fluconazole concomitantly with OSPHENA. Fluconazole increases serum concentrations of OSPHENA. (7.2, 12.3)
- Do not use rifampin concomitantly with OSPHENA. Rifampin decreases serum concentration of OSPHENA. (7.2, 12.3)
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 2-year carcinogenicity study in female mice, ospemifene was orally administered at 100, 400, or 1500 mg/kg/day. No evaluation for carcinogenicity was conducted in male mice. There was significant increase in adrenal subcapsular cell adenomas at 4 and 5 times the human exposure based on AUC, and adrenal cortical tumors at 5 times the human exposure. In the ovary, an increase in sex cord/stromal tumors, tubulostromal tumors, granulosa cell tumors, and luteomas were also seen. These findings occurred at doses 2 to 5 times the human exposure based on AUC and are probably related to estrogenic/antiestrogenic effect of ospemifene in mice.
In a 2-year carcinogenicity study in rats, ospemifene was orally administered at 10, 50, or 300 mg/kg/day. A significant increase in thymomas was recorded for males and thymomas for females at all ospemifene dose levels, or 0.3 to 1.2 times the human exposure based on AUC. In the liver, an increase in hepatocellular tumors was recorded for females at all ospemifene dose levels.
Mutagenesis
Ospemifene was not genotoxic in vitro in the Ames test in strains of Salmonella typhimurium or at the thymidine kinase (tk) locus of mouse lymphoma L5178Y cells in the absence and in the presence of a metabolic activator system. In in vivo testing, ospemifene was not genotoxic in a standard mouse bone marrow micronucleus test or in a determination of DNA adducts in the liver of rats.
Impairment of Fertility
The effect of ospemifene on fertility was not directly evaluated. In female rats and monkeys, decreases in ovarian and uterine weights, decreased corpora lutea number, increased ovarian cysts, uterine atrophy, and disrupted cycles were observed when given repeated daily oral doses. In male rats, atrophy of the prostate and seminal vesicles was noted. The effects on reproductive organs observed in animals are consistent with the estrogen receptor activity of ospemifene and potential for impairment of fertility.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved labeling (Patient Information).
Hypersensitivity Reactions
Inform postmenopausal women who have had hypersensitivity reactions to OSPHENA, such as angioedema, urticaria, rash, and pruritus, that they should not take OSPHENA [see Contraindications (4)].
Vaginal Bleeding
Inform postmenopausal women of the importance of reporting unusual vaginal bleeding to their healthcare providers as soon as possible [see Warnings and Precautions (5.2)].
Hot Flashes or Flushes
OSPHENA may initiate or increase the occurrence of hot flashes in some women [see Adverse Reactions (6.1)].
SPL PATIENT PACKAGE INSERT SECTION
|
This Patient Information has been approved by the U.S. Food and Drug Administration |
Revised: 01/2019 | |||
|
PATIENT INFORMATION | ||||
|
Read this Patient Information before you start taking OSPHENA and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment. | ||||
|
What is the most important information I should know about OSPHENA?
| ||||
|
What is OSPHENA?
| ||||
|
Who should not take OSPHENA? *have unusual vaginal bleeding. Vaginal bleeding after menopause may be a warning sign of cancer of the lining of the uterus (womb). Your healthcare provider should check any unusual vaginal bleeding to find out the cause. *currently have or have had certain cancers. If you have or have had cancer, talk with your healthcare provider about whether you should take OSPHENA. *currently have or have had blood clots. *had a stroke or heart attack. *are allergic to ospemifene or any of the ingredients in OSPHENA. Allergic reaction to OSPHENA can include swelling of the face or tongue (angioedema), hives (urticaria), rash, and itching (pruritus). See the end of this Patient Information leaflet for a complete list of ingredients in OSPHENA. *are pregnant or plan to become pregnant. OSPHENA is not for pregnant women. | ||||
|
What should I tell my healthcare provider before taking OSPHENA?
Tell your healthcare provider about all medicines you take, including
prescription and over-the-counter medicines, vitamins, and herbal supplements.
Some medicines may affect how OSPHENA works. OSPHENA may also affect how other
medicines work. | ||||
|
How should I take OSPHENA?
| ||||
|
What are the possible side effects of OSPHENA?
Serious, but less common side effects include: | ||||
|
|
| ||
|
Call your healthcare provider right away if you get any of the following warning signs or any other unusual symptoms that concern you:
Less serious, but common side effects include: | ||||
|
| |||
|
These are not all the possible side effects of OSPHENA. For more information,
ask your healthcare provider or pharmacist. Tell your healthcare provider
about any side effects that bother you or do not go away.
| ||||
|
How should I store OSPHENA?
Keep OSPHENA and all medicines out of the reach of children. | ||||
|
General information about the safe and effective use of OSPHENA. | ||||
|
What are the ingredients in OSPHENA? |
OSP-PI-06
