Colchicine
These highlights do not include all the information needed to use colchicine safely and effectively. See full prescribing information for Colchicine Tablets, USP. Colchicine Tablets, USP, for oral use Initial U.S. Approval: 1961
94b45698-ac8a-4929-a9b5-5a16153fbf22
HUMAN PRESCRIPTION DRUG LABEL
Jun 9, 2023
American Health Packaging
DUNS: 929561009
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Colchicine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (14)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Package/Label Display Panel – Blister - 0.6 mg
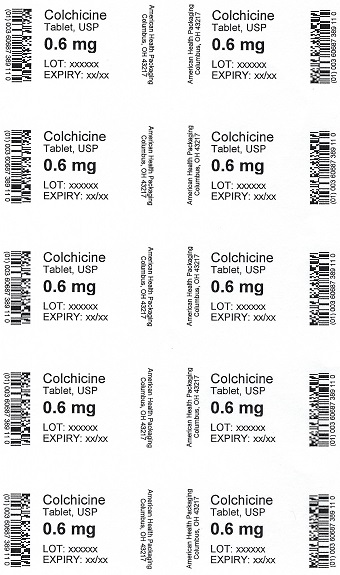
Colchicine
Tablet, USP
0.6 mg
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Gout Flares
Colchicine Tablets, USP are indicated for prophylaxis and the treatment of acute gout flares.
*Prophylaxis of Gout Flares:
Colchicine Tablets, USP are indicated for prophylaxis of gout flares.
*Treatment of Gout Flares:
Colchicine Tablets, USP are indicated for treatment of acute gout flares when
taken at the first sign of a flare.
1.2 Familial Mediterranean Fever (FMF)
Colchicine Tablets, USP are indicated in adults and children four years or older for treatment of familial Mediterranean fever (FMF).
Colchicine Tablets, USP are an alkaloid indicated for:
- Prophylaxis and treatment of gout flares in adults ( 1.1).
- Familial Mediterranean fever (FMF) in adults and children 4 years or older ( 1.2).
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Colchicine is a substrate of the efflux transporter P-glycoprotein (P-gp). Of the cytochrome P450 enzymes tested, CYP3A4 was mainly involved in the metabolism of colchicine. If Colchicine Tablets, USP are administered with drugs that inhibit P-gp, most of which also inhibit CYP3A4, increased concentrations of colchicine are likely. Fatal drug interactions have been reported.
Physicians should ensure that patients are suitable candidates for treatment with Colchicine Tablets, USP and remain alert for signs and symptoms of toxicities related to increased colchicine exposure as a result of a drug interaction. Signs and symptoms of colchicine toxicity should be evaluated promptly and, if toxicity is suspected, Colchicine Tablets, USP should be discontinued immediately.
Table 4 provides recommendations as a result of other potentially significant drug interactions. Table 1 provides recommendations for strong and moderate CYP3A4 inhibitors and P-gp inhibitors.
Table 4. Other Potentially Significant Drug Interactions|
Concomitant Drug Class or Food |
Noted or Anticipated Outcome |
Clinical Comment |
|---|---|---|
|
HMG-Co A Reductase Inhibitors: |
Pharmacokinetic and/or pharmacodynamic interaction: the addition of one drug to a stable long-term regimen of the other has resulted in myopathy and rhabdomyolysis (including a fatality) |
Weigh the potential benefits and risks and carefully monitor patients for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy; monitoring CPK (creatine phosphokinase) will not necessarily prevent the occurrence of severe myopathy. |
|
Other Lipid Lowering Drugs: | ||
|
Digitalis Glycosides: |
P-gp substrate; rhabdomyolysis has been reported |
Coadministration of P-gp and/or CYP3A4 inhibitors (e.g., clarithromycin or cyclosporine) have been demonstrated to alter the concentration of colchicine. The potential for drug-drug interactions must be considered prior to and during therapy. See FPI for a complete list of reported and potential interactions ( 2.4, 5.3, 7).
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Colchicine Tablets, USP 0.6 mg are purple, film-coated, capsule-shaped tablets
debossed with "AR 374" on one side and scored on the other side.
Unit dose packages of 30 (3 x 10) NDC 60687-389-21
16.2 Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Protect from light.
FOR YOUR PROTECTION: Do not use if blister is torn or broken.
SPL MEDGUIDE SECTION
MEDICATION GUIDE
8438921/0422
Colchicine Tablets, USP
Read the Medication Guide that comes with Colchicine Tablets, USP before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. You and your healthcare provider should talk about Colchicine Tablets, USP when you start taking it and at regular checkups.
What is the most important information that I should know about Colchicine
Tablets, USP?
Colchicine Tablets, USP can cause serious side effects or death if levels of
colchicine are too high in your body.
- Taking certain medicines with Colchicine Tablets, USP can cause your level of colchicine to be too high, especially if you have kidney or liver problems.
- Tell your healthcare provider about all your medical conditions, including if you have kidney or liver problems. Your dose of Colchicine Tablets, USP may need to be changed.
- Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins and herbal supplements.
- Even medicines that you take for a short period of time, such as antibiotics, can interact with Colchicine Tablets, USP and cause serious side effects or death.
- Talk to your healthcare provider or pharmacist before taking any new medicine.
- Especially tell your healthcare provider if you take:
|
|
Ask your healthcare provider or pharmacist if you are not sure if you take any of the medicines listed above. This is not a complete list of all the medicines that can interact with Colchicine Tablets, USP.
- Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
- Keep Colchicine Tablets, USP out of the reach of children.
What are Colchicine Tablets, USP?
Colchicine Tablets, USP are a prescription medicine used to:
- prevent and treat gout flares in adults
- treat familial Mediterranean fever (FMF) in adults and children age 4 or older
Colchicine Tablets, USP are not a pain medicine, and should not be taken to treat pain related to other conditions unless specifically prescribed for those conditions.
Who should not take Colchicine Tablets, USP?
Do not take Colchicine Tablets, USP if you have liver or kidney problems and
you take certain other medicines. Serious side effects, including death, have
been reported in these patients even when taken as directed. See**"What is
the most important information that I should know about Colchicine Tablets,
USP?"**
What should I tell my healthcare provider before starting Colchicine
Tablets, USP?
See**"What is the most important information that I should know about
Colchicine Tablets, USP?"**
Before you take Colchicine Tablets, USP tell your healthcare provider about
all your medical conditions, including if you:
- have liver or kidney problems.
- are pregnant or plan to become pregnant. It is not known if Colchicine Tablets, USP will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- are amalewith a female partner who can become pregnant. Receiving treatment with Colchicine Tablets, USP may be related to infertility in some men that is reversible when treatment is stopped.
- are breastfeeding or plan to breastfeed. Colchicine passes into your breast milk. You and your healthcare provider should decide if you will take Colchicine Tablets, USP or breastfeed. If you take Colchicine Tablets, USP and breastfeed, you should talk to your child's healthcare provider about how to watch for side effects in your child.
Tell your healthcare provider about all the medicines you take, including ones that you may only be taking for a short time, such as antibiotics. See**"What is the most important information that I should know about Colchicine Tablets, USP?"** Do not start a new medicine without talking to your healthcare provider.
Using Colchicine Tablets, USP with certain other medicines, such as cholesterol-lowering medications and digoxin, can affect each other, causing serious side effects. Your healthcare provider may need to change your dose of Colchicine Tablets, USP. Talk to your healthcare provider about whether the medications you are taking might interact with Colchicine Tablets, USP and what side effects to look for.
How should I take Colchicine Tablets, USP?
- Take Colchicine Tablets, USP exactly as your healthcare provider tells you to take them.If you are not sure about your dosing, call your healthcare provider.
- Colchicine Tablets, USP can be taken with or without food.
- If you take too many Colchicine Tablets, USP go to the nearest hospital emergency room right away.
- Do not stop taking Colchicine Tablets, USP even if you start to feel better, unless your healthcare provider tells you.
- Your healthcare provider may do blood tests while you take Colchicine Tablets, USP.
- If you take Colchicine Tablets, USP daily and you miss a dose, then take it as soon as you remember. If it is almost time for your next dose, just skip the missed dose. Take the next dose at your regular time. Do not take 2 doses at the same time.
- If you have a gout flare while taking Colchicine Tablets, USP daily, report this to your healthcare provider.
What should I avoid while taking Colchicine Tablets, USP?
- Avoid eating grapefruit or drinking grapefruit juice while taking Colchicine Tablets, USP. It can increase your chances of getting serious side effects.
What are the possible side effects of Colchicine Tablets, USP?
Colchicine Tablets, USP can cause serious side effects or even cause death.
See**"What is the most important information that I should know about
Colchicine Tablets, USP?"**
Get medical help right away if you have:
- Muscle weakness or pain
- Numbness or tingling in your fingers or toes
- Unusual bleeding or bruising
- Increased infections
- Feel weak or tired
- Pale or gray color to your lips, tongue or palms of your hands
- Severe diarrhea or vomiting
**Gout Flares:**The most common side effect of Colchicine Tablets, USP in people who have gout flares is diarrhea.
**FMF:**The most common side effects of Colchicine Tablets, USP in people who have FMF are abdominal pain, diarrhea, nausea and vomiting.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of Colchicine Tablets, USP. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Colchicine Tablets, USP?
- Store Colchicine Tablets, USP at room temperature between 68°F and 77°F (20°C and 25°C).
- Keep Colchicine Tablets, USP out of the light.
Keep Colchicine Tablets, USP and all medicines out of the reach of children.
General Information about Colchicine Tablets, USP
Medicines are sometimes prescribed for purposes other than those listed in a
Medication Guide. Do not use Colchicine Tablets, USP for a condition for which
it was not prescribed. Do not give Colchicine Tablets, USP to other people,
even if they have the same symptoms that you have. It may harm them. This
Medication Guide summarizes the most important information about Colchicine
Tablets, USP. If you would like more information, talk with your healthcare
provider. You can ask your healthcare provider or pharmacist for information
about Colchicine Tablets, USP that is written for healthcare professionals.
What are the ingredients in Colchicine Tablets, USP?
Active Ingredient: colchicine
Inactive Ingredients: carnauba wax, FD&C blue #2, FD&C red #40,
hypromellose, lactose monohydrate, magnesium stearate, microcrystalline
cellulose, polydextrose, polyethylene glycol, pregelatinized starch, sodium
starch glycolate, titanium dioxide and triacetin.
For more information about the drug product, call Takeda Pharmaceuticals
America, Inc. at 1-877-TAKEDA-7 (1-877-825-3327).
For more information about the packaging or labeling, call American Health
Packaging at 1-800-707-4621.
All trademarks are the property of their respective owners.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Distributed by:
American Health Packaging
Columbus, OH 43217
8438921/0422
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from published literature on colchicine use in pregnancy over
several decades have not identified any drug associated risks for major birth
defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
Colchicine crosses the human placenta. Although animal reproductive and
developmental studies were not conducted with Colchicine Tablets, USP,
published animal reproduction and development studies indicate that colchicine
causes embryofetal toxicity, teratogenicity and altered postnatal development
at exposures within or above the clinical therapeutic range. The estimated
background risk of major birth defects and miscarriage for the indicated
population is unknown. All pregnancies have a background risk of birth defect,
loss, or other adverse outcomes. In the US general population, the estimated
background risk of major birth defects and miscarriage in clinically
recognized pregnancies is 2 to 4% and 15 to 20%, respectively
Data
Human Data
Available data from published observational studies, case series, and case
reports over several decades do not suggest an increased risk for major birth
defects or miscarriage in pregnant women with rheumatic diseases (such as
rheumatoid arthritis, Behcet’s disease, or familial Mediterranean fever (FMF)
treated with colchicine at therapeutic doses during pregnancy. Limitations of
these data include the lack of randomization and inability to control for
confounders such as underlying maternal disease and maternal use of
concomitant medications.
8.2 Lactation
Risk Summary
Colchicine is present in human milk (see Data). Adverse events in breastfed
infants have not been reported in the published literature after
administration of colchicine to lactating women. There are no data on the
effects of colchicine on milk production. The developmental and health
benefits of breastfeeding should be considered along with the mother’s
clinical need for Colchicine Tablets, USP and any potential adverse effects on
the breastfed child from Colchicine Tablets, USP or from the underlying
maternal condition.
Data
Limited published data from case reports and a small lactation study
demonstrate that colchicine is present in breastmilk. A systematic review of
literature reported no adverse effects in 149 breastfed children. In a
prospective observational cohort study, no gastrointestinal or other symptoms
were reported in 38 colchicine-exposed breastfed infants.
8.3 Females and Males of Reproductive Potential
Infertility
Case reports and epidemiology studies in human male subjects on colchicine
therapy indicated that infertility from colchicine is rare and may be
reversible. A case report indicated that azoospermia was reversed when therapy
was stopped. Case reports and epidemiology studies in female subjects on
colchicine therapy have not established a clear relationship between
colchicine use and female infertility. However, since the progression of FMF
without treatment may result in infertility, the use of colchicine needs to be
weighed against the potential risks [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and efficacy of colchicine in children of all ages with FMF has been evaluated in uncontrolled studies. There does not appear to be an adverse effect on growth in children with FMF treated long-term with colchicine.
Safety and effectiveness of colchicine in pediatric patients with gout has not been established.
8.5 Geriatric Use
Clinical studies with colchicine for prophylaxis and treatment of gout flares and for treatment of FMF did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient with gout should be cautious, reflecting the greater frequency of decreased renal function, concomitant disease or other drug therapy [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Colchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild (estimated creatinine
clearance Cl cr 50 to 80 mL/min) to moderate (Cl cr 30 to 50 mL/min) renal
function impairment, adjustment of the recommended dose is not required, but
patients should be monitored closely for adverse effects of colchicine.
However, in patients with severe impairment, the starting dose should be 0.3
mg/day and any increase in dose should be done with close monitoring. For the
prophylaxis of gout flares in patients undergoing dialysis, the starting doses
should be 0.3 mg given twice a week with close monitoring [see Dosage and Administration (2.5)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild (Cl cr 50 to 80 mL/min) to
moderate (Cl cr 30 to 50 mL/min) renal function impairment, adjustment of the
recommended dose is not required, but patients should be monitored closely for
adverse effects of colchicine. However, in patients with severe impairment,
while the dose does not need to be adjusted for the treatment of gout flares,
a treatment course should be repeated no more than once every two weeks. For
patients with gout flares requiring repeated courses, consideration should be
given to alternate therapy. For patients undergoing dialysis, the total
recommended dose for the treatment of gout flares should be reduced to a
single dose of 0.6 mg (one tablet). For these patients, the treatment course
should not be repeated more than once every two weeks [see Dosage and Administration (2.5)].
FMF
Although pharmacokinetics of colchicine in patients with mild (Cl cr 50 to 80
mL/min) and moderate (Cl cr 30 to 50 mL/min) renal impairment is not known,
these patients should be monitored closely for adverse effects of colchicine.
Dose reduction may be necessary. In patients with severe renal failure (Cl cr
less than 30 mL/min) and end-stage renal disease requiring dialysis,
Colchicine Tablets, USP may be started at the dose of 0.3 mg/day. Any increase
in dose should be done with adequate monitoring of the patient for adverse
effects of colchicine [see Clinical Pharmacology (12.3), Dosage and Administration (2.5)].
8.7 Hepatic Impairment
The clearance of colchicine may be significantly reduced and plasma half-life prolonged in patients with chronic hepatic impairment compared to healthy subjects [see Clinical Pharmacology (12.3)].
Prophylaxis of Gout Flares
For prophylaxis of gout flares in patients with mild to moderate hepatic
function impairment, adjustment of the recommended dose is not required, but
patients should be monitored closely for adverse effects of colchicine. Dose
reduction should be considered for the prophylaxis of gout flares in patients
with severe hepatic impairment [see Dosage and Administration (2.6)].
Treatment of Gout Flares
For treatment of gout flares in patients with mild to moderate hepatic
function impairment, adjustment of the recommended Colchicine Tablets, USP
dose is not required, but patients should be monitored closely for adverse
effects of colchicine. However, for the treatment of gout flares in patients
with severe impairment, while the dose does not need to be adjusted, the
treatment course should be repeated no more than once every two weeks. For
these patients, requiring repeated courses for the treatment of gout flares,
consideration should be given to alternate therapy [see Dosage and Administration (2.6)].
FMF
In patients with severe hepatic disease, dose reduction should be considered
with careful monitoring [see Clinical Pharmacology (12.3), Dosage and Administration (2.6)].
-
In the presence of mild to moderate renal or hepatic impairment, adjustment of dosing is not required for treatment of gout flare, prophylaxis of gout flare and FMF, but patients should be monitored closely ( 8.6).
-
In patients with severe renal impairment for prophylaxis of gout flares, the starting dose should be 0.3 mg/day for gout flares, no dose adjustment is required, but a treatment course should be repeated no more than once every two weeks. In FMF patients, start with 0.3 mg/day, and any increase in dose should be done with close monitoring ( 8.6).
-
In patients with severe hepatic impairment, a dose reduction may be needed in prophylaxis of gout flares and FMF patients; while a dose reduction may not be needed in gout flares, a treatment course should be repeated no more than once every two weeks ( 8.6, 8.7).
-
For patients undergoing dialysis, the total recommended dose for prophylaxis of gout flares should be 0.3 mg given twice a week with close monitoring. For treatment of gout flares, the total recommended dose should be reduced to 0.6 mg (one tablet) × 1 dose and the treatment course should not be repeated more than once every two weeks. For FMF patients, the starting dose should be 0.3 mg/day and dosing can be increased with close monitoring ( 8.6).
-
Females and Males of Reproductive Potential: Advise males that Colchicine Tablets, USP may transiently impair
fertility ( 8.3). -
Geriatric Use: The recommended dose of colchicine should be based on renal function ( 2.5, 8.5).
