Teriflunomide
These highlights do not include all the information needed to use TERIFLUNOMIDE TABLET safely and effectively. See full prescribing information for TERIFLUNOMIDE TABLET. TERIFLUNOMIDE tablet, for oral use Initial U.S. Approval: 2012
37f04f8b-001e-66ff-4574-cc34cebce61c
HUMAN PRESCRIPTION DRUG LABEL
Jan 13, 2023
Biocon Pharma Inc.
DUNS: 080000063
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Teriflunomide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Teriflunomide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Drug Labeling Information
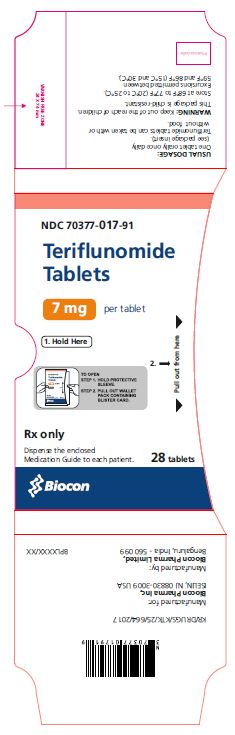
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Teriflunomide Tablets - Sleeve
7 mg per tablet
NDC 70377-017-91
Rx only
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Teriflunomide tablets are contraindicated in/with:
- Patients with severe hepatic impairment [see Warnings and Precautions (5.1)].
- Pregnant women and females of reproductive potential not using effective contraception. Teriflunomide tablet may cause fetal harm [see Warnings and Precautions (5.2, 5.3) and Use in Specific Populations (8.1)].
- Patients with a history of a hypersensitivity reaction to teriflunomide, leflunomide, or to any of the inactive ingredients in teriflunomide tablet. Reactions have included anaphylaxis, angioedema, and serious skin reactions [see Warnings and Precautions (5.5)].
- Coadministration with leflunomide [see Clinical Pharmacology (12.3)].
- Severe hepatic impairment (4, 5.1)
- Pregnancy (4, 5.2, 8.1)
- Hypersensitivity (4, 5.5)
- Current leflunomide treatment (4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Hepatotoxicity
Clinically significant and potentially life-threatening liver injury, including acute liver failure requiring transplant, has been reported in patients treated with teriflunomide in the postmarketing setting. Patients with pre-existing liver disease and patients taking other hepatotoxic drugs may be at increased risk for developing liver injury when taking teriflunomide. Clinically significant liver injury can occur at any time during treatment with teriflunomide.
Patients with pre-existing acute or chronic liver disease, or those with serum alanine aminotransferase (ALT) greater than two times the upper limit of normal (ULN) before initiating treatment, should not normally be treated with teriflunomide. Teriflunomide is contraindicated in patients with severe hepatic impairment [see Contraindications (4)].
In placebo-controlled trials in adult patients, ALT greater than three times the ULN occurred in 61/1045 (5.8%) and 62/1002 (6.2%) of patients receiving teriflunomide 7 mg and 14 mg, respectively, and 38/997 (3.8%) of patients receiving placebo, during the treatment period. These elevations occurred mostly within the first year of treatment. Half of the cases returned to normal without drug discontinuation. In clinical trials, if ALT elevation was greater than three times the ULN on two consecutive tests, teriflunomide was discontinued and patients underwent an accelerated elimination procedure [see Warnings and Precautions (5.3)]. Of the patients who underwent discontinuation and accelerated elimination in controlled trials, half returned to normal or near normal values within 2 months.
One patient in the controlled trials in adult patients developed ALT 32 times the ULN and jaundice 5 months after initiation of teriflunomide 14 mg treatment. The patient was hospitalized for 5 weeks and recovered after plasmapheresis and cholestyramine accelerated elimination procedure. Teriflunomide-induced liver injury in this patient could not be ruled out.
Obtain serum transaminase and bilirubin levels within 6 months before initiation of teriflunomide therapy. Monitor ALT levels at least monthly for six months after starting teriflunomide. Consider additional monitoring when teriflunomide is given with other potentially hepatotoxic drugs.
Consider discontinuing teriflunomide if serum transaminase increase (greater than three times the ULN) is confirmed. Monitor serum transaminase and bilirubin on teriflunomide therapy, particularly in patients who develop symptoms suggestive of hepatic dysfunction, such as unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or jaundice and/or dark urine. If liver injury is suspected to be teriflunomide-induced, discontinue teriflunomide and start an accelerated elimination procedure [see Warnings and Precautions (5.3)] and monitor liver tests weekly until normalized. If teriflunomide-induced liver injury is unlikely because some other probable cause has been found, resumption of teriflunomide therapy may be considered.
5.2 Embryofetal Toxicity
Teriflunomide may cause fetal harm when administered to a pregnant woman. Teratogenicity and embryofetal lethality occurred in animal reproduction studies in multiple animal species at plasma teriflunomide exposures similar to or lower than that in humans at the maximum recommended human dose (MRHD) of 14 mg/day [see Use in Specific Populations (8.1)].
Teriflunomide is contraindicated for use in pregnant women and in females of reproductive potential not using effective contraception [see Contraindications (4)]. Exclude pregnancy before starting treatment with teriflunomide in females of reproductive potential [see Dosage and Administration (2) ]. Advise females of reproductive potential to use effective contraception during teriflunomide treatment and during an accelerated drug elimination procedure after teriflunomide treatment [see Use in Specific Populations (8.3)]. If a woman becomes pregnant while taking teriflunomide, stop treatment with teriflunomide, apprise the patient of the potential risk to a fetus, and perform an accelerated drug elimination procedure to achieve a plasma teriflunomide concentration of less than 0.02 mg/L [see Warnings and Precautions (5.3)].
Upon discontinuing teriflunomide, it is recommended that all females of reproductive potential undergo an accelerated drug elimination procedure. Women receiving teriflunomide treatment who wish to become pregnant must discontinue teriflunomide and undergo an accelerated drug elimination procedure, which includes verification that plasma concentrations of teriflunomide are less than 0.02 mg/L (0.02 mcg/mL). Men wishing to father a child should also discontinue use of teriflunomide and either undergo an accelerated elimination procedure or wait until verification that the plasma teriflunomide concentration is less than 0.02 mg/L (0.02 mcg/mL) [see Use in Specific Populations (8.3)]. Based on animal data, human plasma concentrations of teriflunomide of less than 0.02 mg/L (0.02 mcg/mL) are expected to have minimal embryofetal risk [see Contraindications (4), Warnings and Precautions (5.3), and Use in Specific Populations (8.1)].
5.3 Procedure for Accelerated Elimination of Teriflunomide
Teriflunomide is eliminated slowly from the plasma [see Clinical Pharmacology (12.3)]. Without an accelerated elimination procedure, it takes on average 8 months to reach plasma concentrations less than 0.02 mg/L, although because of individual variations in drug clearance it may take as long as 2 years. An accelerated elimination procedure could be used at any time after discontinuation of teriflunomide. Elimination can be accelerated by either of the following procedures:
- Administration of cholestyramine 8 g every 8 hours for 11 days. If cholestyramine 8 g three times a day is not well tolerated, cholestyramine 4 g three times a day can be used.
- Administration of 50 g oral activated charcoal powder every 12 hours for 11 days.
If either elimination procedure is poorly tolerated, treatment days do not need to be consecutive unless there is a need to lower teriflunomide plasma concentration rapidly.
At the end of 11 days, both regimens successfully accelerated teriflunomide elimination, leading to more than 98% decrease in teriflunomide plasma concentrations.
Use of the accelerated elimination procedure may potentially result in return of disease activity if the patient had been responding to teriflunomide treatment.
5.4 Bone Marrow Effects/Immunosuppression Potential/Infections
Bone Marrow Effects
A mean decrease compared to baseline in white blood cell (WBC) count of
approximately 15% (mainly neutrophils and lymphocytes) and in platelet count
of approximately 10% was observed in placebo-controlled trials in adult
patients with 7 mg and 14 mg of teriflunomide. The decrease in mean WBC count
occurred during the first 6 weeks and WBC count remained low during treatment.
In placebo-controlled studies in adult patients, neutrophil count < 1.5x109/L
was observed in 12% and 16% of patients receiving teriflunomide 7 mg and 14
mg, respectively, compared with 7% of patients receiving placebo; lymphocyte
count <0.8x109/L was observed in 10% and 12% of patients receiving
teriflunomide 7 mg and 14 mg, respectively, compared with 6% of patients
receiving placebo. No cases of serious pancytopenia were reported in
premarketing clinical trials of teriflunomide but rare cases of pancytopenia
and agranulocytosis have been reported in the postmarketing setting with
leflunomide. A similar risk would be expected for teriflunomide [see Clinical Pharmacology (12.3)]. Cases of thrombocytopenia with teriflunomide, including
rare cases with platelet counts less than 50,000/mm3, have been reported in
post-marketing setting. Obtain a complete blood cell count (CBC) within 6
months before the initiation of treatment with teriflunomide. Further
monitoring should be based on signs and symptoms suggestive of bone marrow
suppression.
Risk of Infection / Tuberculosis Screening
Patients with active acute or chronic infections should not start treatment until the infection(s) is resolved. If a patient develops a serious infection consider suspending treatment with teriflunomide and using an accelerated elimination procedure. Reassess the benefits and risks prior to resumption of therapy. Instruct patients receiving teriflunomide to report symptoms of infections to a physician.
Teriflunomide is not recommended for patients with severe immunodeficiency, bone marrow disease, or severe, uncontrolled infections. Medications like teriflunomide that have immunosuppression potential may cause patients to be more susceptible to infections, including opportunistic infections.
In placebo-controlled studies of teriflunomide in adult patients, no overall increase in the risk of serious infections was observed with teriflunomide 7 mg (2.2%) or 14 mg (2.7%) compared to placebo (2.2%).
However, one fatal case of klebsiella pneumonia sepsis occurred in a patient taking teriflunomide 14 mg for 1.7 years. Fatal infections have been reported in the postmarketing setting in patients receiving leflunomide, especially Pneumocystis jirovecii pneumonia and aspergillosis. Most of the reports were confounded by concomitant immunosuppressant therapy and/or comorbid illness which, in addition to rheumatoid disease, may predispose patients to infection. In clinical studies with teriflunomide, cytomegalovirus hepatitis reactivation has been observed.
In clinical studies with teriflunomide in adult patients, cases of tuberculosis have been observed. Prior to initiating teriflunomide, screen patients for latent tuberculosis infection with a tuberculin skin test or with a blood test for mycobacterium tuberculosis infection. Teriflunomide has not been studied in patients with a positive tuberculosis screen, and the safety of teriflunomide in individuals with latent tuberculosis infection is unknown. For patients testing positive in tuberculosis screening, treat by standard medical practice prior to therapy with teriflunomide.
Vaccination
No clinical data are available on the efficacy and safety of live vaccinations in patients taking teriflunomide. Vaccination with live vaccines is not recommended. The long half-life of teriflunomide should be considered when contemplating administration of a live vaccine after stopping teriflunomide.
Malignancy
The risk of malignancy, particularly lymphoproliferative disorders, is increased with the use of some immunosuppressive medications. There is a potential for immunosuppression with teriflunomide. No apparent increase in the incidence of malignancies and lymphoproliferative disorders was reported in the teriflunomide clinical trials, but larger and longer-term studies would be needed to determine whether there is an increased risk of malignancy or lymphoproliferative disorders with teriflunomide.
5.5 Hypersensitivity Reactions
Teriflunomide can cause anaphylaxis and severe allergic reactions [see Contraindications (4)]. Signs and symptoms have included dyspnea, urticaria, and angioedema including lips, eyes, throat, and tongue. Inform patients of the signs and symptoms of anaphylaxis and angioedema.
5.6 Serious Skin Reactions
Cases of serious skin reactions, sometimes fatal, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) [see Warnings and Precautions (5.7)], have been reported with teriflunomide. Fatal outcomes were reported in one case of TEN and one case of DRESS**.** Inform patients of the signs and symptoms that may signal a serious skin reaction. Instruct patients to discontinue teriflunomide and seek immediate medical care should these signs and symptoms occur. Unless the reaction is clearly not drug related, discontinue teriflunomide and begin an accelerated elimination procedure immediately [see Warnings and Precautions (5.3)]. In such cases, patients should not be re-exposed to teriflunomide [see Contraindications (4)].
5.7 Drug Reaction with Eosinophilia and Systemic Symptoms
Drug reaction with eosinophilia and systemic symptoms (DRESS), also known as multiorgan hypersensitivity, has occurred with teriflunomide. One fatal case of DRESS that occurred in close temporal association (34 days) with the initiation of teriflunomide treatment has been reported in the postmarketing setting. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy and/or facial swelling, in association with other organ system involvement, such as hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis, sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. Discontinue teriflunomide, unless an alternative etiology for the signs or symptoms is established, and begin an accelerated elimination procedure immediately [see Warnings and Precautions (5.3)]. In such cases, patients should not be re-exposed to teriflunomide [see Contraindications (4)].
5.8 Peripheral Neuropathy
In placebo-controlled studies in adult patients, peripheral neuropathy, including both polyneuropathy and mononeuropathy (e.g., carpal tunnel syndrome), occurred more frequently in patients taking teriflunomide than in patients taking placebo. The incidence of peripheral neuropathy confirmed by nerve conduction studies was 1.4% (13 patients) and 1.9% (17 patients) of patients receiving 7 mg and 14 mg of teriflunomide, respectively, compared with 0.4% receiving placebo (4 patients). Treatment was discontinued in 0.7% (8 patients) with confirmed peripheral neuropathy (3 patients receiving teriflunomide 7 mg and 5 patients receiving teriflunomide 14 mg). Five of them recovered following treatment discontinuation. Not all cases of peripheral neuropathy resolved with continued treatment. Peripheral neuropathy also occurred in patients receiving leflunomide.
Age older than 60 years, concomitant neurotoxic medications, and diabetes may increase the risk for peripheral neuropathy. If a patient taking teriflunomide develops symptoms consistent with peripheral neuropathy, such as bilateral numbness or tingling of hands or feet, consider discontinuing teriflunomide therapy and performing an accelerated elimination procedure [see Warnings and Precautions (5.3)].
5.9 Increased Blood Pressure
In placebo-controlled studies in adult patients, the mean change from baseline to the end of study in systolic blood pressure was +2.3 mmHg and +2.7 mmHg for teriflunomide 7 mg and 14 mg, respectively, and -0.6 mmHg for placebo. The change from baseline in diastolic blood pressure was +1.4 mmHg and +1.9 mmHg for teriflunomide 7 mg and 14 mg, respectively, and -0.3 mmHg for placebo. Hypertension was an adverse reaction in 3.1% and 4.3% of patients treated with 7 mg or 14 mg of teriflunomide compared with 1.8% for placebo. Check blood pressure before start of teriflunomide treatment and periodically thereafter. Elevated blood pressure should be appropriately managed during treatment with teriflunomide.
5.10 Respiratory Effects
Interstitial lung disease, including acute interstitial pneumonitis, has been reported with teriflunomide in the postmarketing setting.
Interstitial lung disease and worsening of pre-existing interstitial lung disease have been reported during treatment with leflunomide. Interstitial lung disease may be fatal and may occur acutely at any time during therapy with a variable clinical presentation. New onset or worsening pulmonary symptoms, such as cough and dyspnea, with or without associated fever, may be a reason for discontinuation of therapy and for further investigation as appropriate. If discontinuation of the drug is necessary, consider initiation of an accelerated elimination procedure [see Warnings and Precautions (5.3)].
5.11 Pancreatitis in Pediatric Patients
Teriflunomide is not approved for use in pediatric patients. In the pediatric clinical trial, cases of pancreatitis were observed in 1.8% (2/109) of patients receiving teriflunomide; one of these cases was serious [see Use in Specific Populations (8.4)]. If pancreatitis is suspected, discontinue teriflunomide and start an accelerated elimination procedure [see Warnings and Precautions (5.3)].
5.12 Concomitant Use with Immunosuppressive or Immunomodulating Therapies
Coadministration with antineoplastic or immunosuppressive therapies used for treatment of multiple sclerosis has not been evaluated. Safety studies in which teriflunomide was concomitantly administered with other immune modulating therapies for up to one year (interferon beta, glatiramer acetate) did not reveal any specific safety concerns. The long term safety of these combinations in the treatment of multiple sclerosis has not been established. In any situation in which the decision is made to switch from teriflunomide to another agent with a known potential for hematologic suppression, it would be prudent to monitor for hematologic toxicity, because there will be overlap of systemic exposure to both compounds. Use of an accelerated elimination procedure may decrease this risk, but may also potentially result in return of disease activity if the patient had been responding to teriflunomide treatment [see Warnings and Precautions (5.3)].
-
Elimination of teriflunomide can be accelerated by administration of cholestyramine or activated charcoal for 11 days. (5.3)
-
Teriflunomide may decrease WBC. A recent CBC should be available before starting teriflunomide. Monitor for signs and symptoms of infection.
Consider suspending treatment with teriflunomide in case of serious infection. Do not start teriflunomide in patients with active infections. (5.4) -
Stop teriflunomide if patient has anaphylaxis, angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms; initiate rapid elimination. (5.3, 5.5, 5.6, 5.7)
-
If patient develops symptoms consistent with peripheral neuropathy, evaluate patient and consider discontinuing teriflunomide. (5.8)
-
Teriflunomide may increase blood pressure. Measure blood pressure at treatment initiation and monitor blood pressure during treatment. (5.9)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Effect of Teriflunomide on CYP2C8 Substrates
Teriflunomide is an inhibitor of CYP2C8 in vivo. In patients taking
teriflunomide, exposure of drugs metabolized by CYP2C8 (e.g., paclitaxel,
pioglitazone, repaglinide, rosiglitazone) may be increased. Monitor these
patients and adjust the dose of the concomitant drug(s) metabolized by CYP2C8
as required [see Clinical Pharmacology (12.3)].
Effect of Teriflunomide on Warfarin
Coadministration of teriflunomide with warfarin requires close monitoring of
the international normalized ratio (INR) because teriflunomide may decrease
peak INR by approximately 25%.
Effect of Teriflunomide on Oral Contraceptives
Teriflunomide may increase the systemic exposures of ethinylestradiol and
levonorgestrel. Consideration should be given to the type or dose of
contraceptives used in combination with teriflunomide [see Clinical Pharmacology (12.3)].
Effect of Teriflunomide on CYP1A2 Substrates
Teriflunomide may be a weak inducer of CYP1A2 in vivo. In patients taking
teriflunomide, exposure of drugs metabolized by CYP1A2 (e.g., alosetron,
duloxetine, theophylline, tizanidine) may be reduced. Monitor these patients
and adjust the dose of the concomitant drug(s) metabolized by CYP1A2 as
required[see Clinical Pharmacology (12.3)].
Effect of Teriflunomide on Organic Anion Transporter 3 (OAT3) Substrates
Teriflunomide inhibits the activity of OAT3 in vivo. In patients taking
teriflunomide, exposure of drugs which are OAT3 substrates (e.g., cefaclor,
cimetidine, ciprofloxacin, penicillin G, ketoprofen, furosemide, methotrexate,
zidovudine) may be increased. Monitor these patients and adjust the dose of
the concomitant drug(s) which are OAT3 substrates as required [see Clinical Pharmacology (12.3)].
Effect of Teriflunomide on BCRP and Organic Anion Transporting Polypeptide B1
and B3 (OATP1B1/1B3) Substrates
Teriflunomide inhibits the activity of BCRP and OATP1B1/1B3 invivo. For a
patient taking teriflunomide, the dose of rosuvastatin should not exceed 10 mg
once daily. For other substrates of BCRP (e.g., mitoxantrone) and drugs in the
OATP family (e.g., methotrexate, rifampin), especially HMG-Co reductase
inhibitors (e.g., atorvastatin, nateglinide, pravastatin, repaglinide, and
simvastatin), consider reducing the dose of these drugs and monitor patients
closely for signs and symptoms of increased exposures to the drugs while
patients are taking teriflunomide [see Clinical Pharmacology (12.3)].
- Drugs metabolized by CYP2C8 and OAT3 transporters: Monitor patients because teriflunomide may increase exposure of these drugs. (7)
- Teriflunomide may increase exposure of ethinylestradiol and levonorgestrel. Choose an appropriate oral contraceptive. (7)
- Drugs metabolized by CYP1A2: Monitor patients because teriflunomide may decrease exposure of these drugs. (7)
- Warfarin: Monitor INR as teriflunomide may decrease INR. (7)
- Drugs metabolized by BCRP and OATP1B1/B3 transporters: Monitor patients because teriflunomide may increase exposure of these drugs. (7)
- Rosuvastatin: The dose of rosuvastatin should not exceed 10 mg once daily in patients taking teriflunomide. (7)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
The recommended dose of teriflunomide tablet is 7 mg or 14 mg orally once daily. Teriflunomide tablet can be taken with or without food. Monitoring to Assess Safety.
- Obtain transaminase and bilirubin levels within 6 months before initiation of teriflunomide tablet therapy. Monitor ALT levels at least monthly for six months after starting teriflunomide tablets [see Warnings and Precautions (5.1)].
- Obtain a complete blood cell count (CBC) within 6 months before the initiation of treatment with teriflunomide tablets. Further monitoring should be based on signs and symptoms of infection [see Warnings and Precautions (5.4)].
- Prior to initiating teriflunomide tablets, screen patients for latent tuberculosis infection with a tuberculin skin test or blood test for mycobacterium tuberculosis infection [see Warnings and Precautions (5.4)].
- Exclude pregnancy prior to initiation of treatment with teriflunomide tablets in females of reproductive potential [see Warnings and Precautions (5.2)].
- Check blood pressure before start of teriflunomide tablets treatment and periodically thereafter [see Warnings and Precautions (5.9)].
7 mg or 14 mg orally once daily, with or without food. (2)
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No evidence of carcinogenicity was observed in lifetime carcinogenicity
bioassays in mouse and rat. In mouse, teriflunomide was administered orally at
doses up to 12 mg/kg/day for up to 95 to 104 weeks; plasma teriflunomide
exposures (AUC) at the highest dose tested are approximately 3 times that in
humans at the maximum recommended human dose (MRHD, 14 mg/day). In rat,
teriflunomide was administered orally at doses up to 4 mg/kg/day for up to 97
to 104 weeks; plasma teriflunomide AUCs at the highest doses tested are less
than that in humans at the MRHD.
Mutagenesis
Teriflunomide was negative in the in vitro bacterial reverse mutation (Ames)
assay, the in vitro HPRT assay, and in in vivo micronucleus and chromosomal
aberration assays. Teriflunomide was positive in an in vitro chromosomal
aberration assay in human lymphocytes, with and without metabolic activation.
Addition of uridine (to supplement the pyrimidine pool) reduced the magnitude
of the clastogenic effect; however, teriflunomide was positive in the in vitro
chromosomal aberration assay, even in the presence of uridine.
4-Trifluoromethylaniline (4-TFMA), a minor metabolite of teriflunomide, was positive in the in vitro bacterial reverse mutation (Ames) assay, the in vitro HPRT assay, and the in vitro chromosomal aberration assay in mammalian cells. 4-TFMA was negative in in vivo micronucleus and chromosomal aberration assays.
Impairment of Fertility
Oral administration of teriflunomide (0, 1, 3, 10 mg/kg/day) to male rats
prior to and during mating (to untreated females) resulted in no adverse
effects on fertility; however, reduced epididymal sperm count was observed at
the mid and high doses tested. The no-effect dose for reproductive toxicity in
male rats (1 mg/kg) is less than the MRHD on a mg/m2 basis.
Oral administration of teriflunomide (0, 0.84, 2.6, 8.6 mg/kg/day) to female rats, prior to and during mating (to untreated males) and continuing to gestation day 6, resulted in embryolethality, reduced fetal body weight, and/or malformations at all doses tested. Due to marked embryolethality at the highest dose tested, no fetuses were available for evaluation. The lowest dose tested is less than the MRHD on a mg/m2 basis.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
A Medication Guide is required for distribution with teriflunomide tablets.
Hepatotoxicity
Inform patients that teriflunomide may cause liver injury, which can be life-
threatening, and that their liver enzymes will be checked before starting
teriflunomide and at least monthly for 6 months after starting teriflunomide
[see Dosage and Administration (2) and Warnings and Precautions (5.1)]. Advise
patients that they should contact their physician if they have any unexplained
nausea, vomiting, abdominal pain, fatigue, anorexia, or jaundice and/or dark
urine.
Embryofetal Toxicity
- Advise females of reproductive potential
- of the potential for fetal harm if teriflunomide is taken during pregnancy
- to notify their healthcare provider immediately if a pregnancy occurs or is suspected
- to use effective contraception during treatment with teriflunomide and until the teriflunomide plasma concentration is verified to be less than 0.02 mg/L [see Warnings and Precautions (5.2, 5.3), Use in Specific Populations (8.1, 8.3), Clinical Pharmacology (12.3)]
- Instruct men taking teriflunomide and not wishing to father a child to use effective contraception to minimize any possible risk to the fetus; their female partners should also use effective contraception.
- Advise men wishing to father a child to discontinue use of teriflunomide and undergo an accelerated elimination procedure.
Availability of an Accelerated Elimination Procedure
Advise patients that teriflunomide may stay in the blood for up to 2 years after the last dose and that an accelerated elimination procedure may be used if needed [see Warnings and Precautions (5.3)].
Risk of Infections
Inform patients that they may develop a lowering of their white blood cell counts and that their blood counts will be checked before starting teriflunomide.
Inform patients that they may be more likely to get infections when taking teriflunomide and that they should contact their physician if they develop symptoms of infection, particularly in case of fever [see Warnings and Precautions (5.4)].
Advise patients that the use of some vaccines should be avoided during treatment with teriflunomide and for at least 6 months after discontinuation.
Hypersensitivity Reactions
Advise patients to discontinue teriflunomide and seek immediate medical attention if any signs or symptoms of a hypersensitivity reaction occur [see Contraindications (4) and Warnings and Precautions (5.5)]. Signs and symptoms can include dyspnea, urticaria, angioedema involving the lips, eyes, throat, or tongue, or skin rash.
Serious Skin Reactions
Advise patients to discontinue teriflunomide and seek immediate medical attention if any signs of a serious skin reaction, such as SJS or TEN, occur [see Warnings and Precautions (5.6)]. Signs and symptoms can include rash, mouth sores, blisters, or peeling skin.
DRESS/Multi-organ Hypersensitivity
Instruct patients and caregivers that a fever or rash associated with signs of other organ system involvement (e.g., lymphadenopathy, hepatic dysfunction) may be drug-related and should be reported to their healthcare provider immediately. Teriflunomide should be discontinued immediately if a serious hypersensitivity reaction is suspected [see Warnings and Precautions (5.7)].
Peripheral Neuropathy
Inform patients that they may develop peripheral neuropathy. Advise patients that they should contact their physician if they develop symptoms of peripheral neuropathy, such as numbness or tingling of hands or feet [see Warnings and Precautions (5.8)].
Increased Blood Pressure
Inform patients that teriflunomide may increase blood pressure [see Warnings and Precautions (5.9)].
Lactation
Advise females not to breastfeed during treatment with teriflunomide [see Use in Specific Populations (8.2)].
Manufactured by:
Biocon Pharma Limited
Bengaluru,
India - 560099
Manufactured for:
Biocon Pharma Inc.,
Iselin, New Jersey, 08830-3009
United States of America
Revised: 01/2023
