Dexlansoprazole
These highlights do not include all the information needed to use safely and effectively. See full prescribing information for . Initial U.S. Approval: 1995 (lansoprazole)
3f9699b5-7614-41cb-bd1d-ff02930e98f3
HUMAN PRESCRIPTION DRUG LABEL
Jul 15, 2023
Mylan Pharmaceuticals Inc.
DUNS: 059295980
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
dexlansoprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (19)
dexlansoprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (19)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
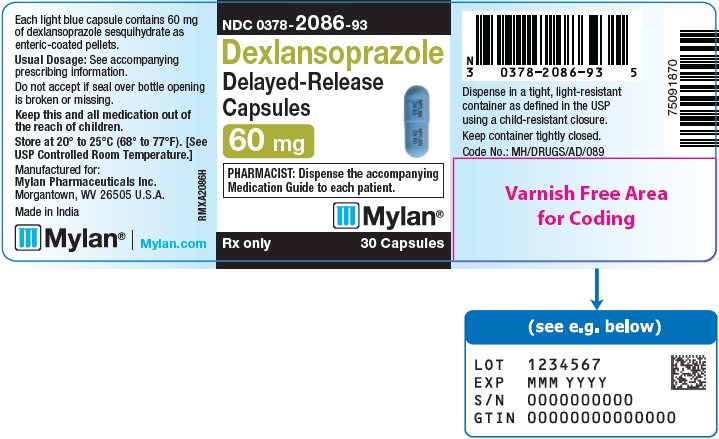
PRINCIPAL DISPLAY PANEL – 60 mg
NDC 0378-2086-93
Dexlansoprazole
Delayed-Release
Capsules
60 mg
PHARMACIST: Dispense the accompanying
Medication Guide to each patient.
Rx only 30 Capsules
Each light blue capsule contains 60 mg
of dexlansoprazole sesquihydrate as
enteric-coated pellets.
Usual Dosage: See accompanying
prescribing information.
Do not accept if seal over bottle opening
is broken or missing.
Keep this and all medication out of
the reach of children.
Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Manufactured for:
Mylan Pharmaceuticals Inc.
****Morgantown, WV 26505 U.S.A.
Made in India
Mylan.com
RMXA2086H
Dispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.
Keep container tightly closed.
Code No.: MH/DRUGS/AD/089
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Presence of Gastric Malignancy
In adults, symptomatic response to therapy with dexlansoprazole extended- release capsules does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing in adult patients who have a suboptimal response or an early symptomatic relapse after completing treatment with a PPI. In older patients, also consider an endoscopy.
5.2 Acute Tubulointerstitial Nephritis
Acute tubulointerstitial nephritis (TIN) has been observed in patients taking PPIs and may occur at any point during PPI therapy. Patients may present with varying signs and symptoms from symptomatic hypersensitivity reactions to non- specific symptoms of decreased renal function (e.g., malaise, nausea, anorexia). In reported case series, some patients were diagnosed on biopsy and in the absence of extra-renal manifestations (e.g., fever, rash or arthralgia).
Discontinue dexlansoprazole extended-release capsules and evaluate patients with suspected acute TIN [see Contraindications (4)].
5.3 Clostridium difficile-Associated Diarrhea
Published observational studies suggest that PPI therapy like dexlansoprazole extended-release capsules may be associated with an increased risk of Clostridium difficile-associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2)].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
5.4 Bone Fracture
Several published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the conditions being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2), Adverse Reactions (6.2)].
5.5 Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported in association with the use of PPIs [see Adverse Reactions (6.2)]. Discontinue dexlansoprazole extended-release capsules at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation.
5.6 Cutaneous and Systemic Lupus Erythematosus
Cutaneous lupus erythematosus (CLE) and systemic lupus erythematosus (SLE) have been reported in patients taking PPIs. These events have occurred as both new onset and an exacerbation of existing autoimmune disease. The majority of PPI-induced lupus erythematosus cases were CLE.
The most common form of CLE reported in patients treated with PPIs was subacute CLE (SCLE) and occurred within weeks to years after continuous drug therapy in patients ranging from infants to the elderly. Generally, histological findings were observed without organ involvement.
Systemic lupus erythematosus (SLE) is less commonly reported than CLE in patients receiving PPIs. PPI-associated SLE is usually milder than nondrug induced SLE. Onset of SLE typically occurred within days to years after initiating treatment primarily in patients ranging from young adults to the elderly. The majority of patients presented with rash; however, arthralgia and cytopenia were also reported.
Avoid administration of PPIs for longer than medically indicated. If signs or symptoms consistent with CLE or SLE are noted in patients receiving dexlansoprazole extended-release capsules, discontinue the drug and refer the patient to the appropriate specialist for evaluation. Most patients improve with discontinuation of the PPI alone in four to 12 weeks. Serological testing (e.g., ANA) may be positive and elevated serological test results may take longer to resolve than clinical manifestations.
5.7 Cyanocobalamin (Vitamin B12) Deficiency
Daily treatment with any acid-suppressing medications over a long period of time (e.g., longer than three years) may lead to malabsorption of cyanocobalamin (Vitamin B12) caused by hypo-or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed in patients treated with dexlansoprazole extended-release capsules.
5.8 Hypomagnesemia and Mineral Metabolism
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. Hypomagnesemia may lead to hypocalcemia and/or hypokalemia and may exacerbate underlying hypocalcemia in at-risk patients. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].
Consider monitoring magnesium and calcium levels prior to initiation of dexlansoprazole delayed-release capsules and periodically while on treatment in patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism). Supplement with magnesium and/or calcium as necessary. If hypocalcemia is refractory to treatment, consider discontinuing the PPI.
5.9 Interactions with Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop dexlansoprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g., for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary [see Drug Interactions (7), Clinical Pharmacology (12.2)].
5.10 Interaction with Methotrexate
Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (7)].
5.11 Fundic Gland Polyps
PPI use is associated with an increased risk of fundic gland polyps that increases with long-term use, especially beyond one year. Most PPI users who developed fundic gland polyps were asymptomatic and fundic gland polyps were identified incidentally on endoscopy. Use the shortest duration of PPI therapy appropriate to the condition being treated.
5.12 Risk of Heart Valve Thickening in Pediatric Patients Less Than Two
Years of Age
Dexlansoprazole delayed-release capsules are not recommended in pediatric patients less than two years of age. Nonclinical studies in juvenile rats with lansoprazole have demonstrated an adverse effect of heart valve thickening. Dexlansoprazole is the R-enantiomer of lansoprazole [see Use in Specific Populations (8.4)].
•
Gastric Malignancy: In adults, symptomatic response with dexlansoprazole delayed-release capsules does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing. (5.1)
•
Acute Tubulointerstitial Nephritis: Discontinue treatment and evaluate patients. (5.2)
•
Clostridium difficile-Associated Diarrhea: PPI therapy may be associated with increased risk. (5.3)
•
Bone Fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. (5.4)
•
Severe Cutaneous Adverse Reactions: Discontinue at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation. (5.5)
•
Cutaneous and Systemic Lupus Erythematosus: Mostly cutaneous; new onset or exacerbation of existing disease; discontinue dexlansoprazole delayed-release capsules and refer to specialist for evaluation. (5.6)
•
Cyanocobalamin (Vitamin B12) Deficiency: Daily long-term use (e.g., longer than 3 years) may lead to malabsorption or a deficiency of cyanocobalamin. (5.7)
•
Hypomagnesemia and Mineral Metabolism: Reported rarely with prolonged treatment with PPIs. (5.8)
•
Interactions with Investigations for Neuroendocrine Tumors: Increases in intragastric pH may result in hypergastrinemia and enterochromaffin-like cell hyperplasia and increased chromogranin A levels which may interfere with diagnostic investigations for neuroendocrine tumors. (5.9, 7)
•
Interaction with Methotrexate: Concomitant use with PPIs may elevate and/or prolong serum concentrations of methotrexate and/or its metabolite, possibly leading to toxicity. With high-dose methotrexate administration, consider a temporary withdrawal of dexlansoprazole delayed-release capsules. (5.10, 7)
•
Fundic Gland Polyps: Risk increases with long-term use, especially beyond 1 year. Use the shortest duration of therapy. (5.11)
•
Risk of Heart Valve Thickening in Pediatric Patients Less than Two Years of Age: Dexlansoprazole delayed-release capsules are not recommended in pediatric patients less than 2 years of age. (5.12, 8.4)
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Healing of Erosive Esophagitis in Adults
Two multicenter, double-blind, active-controlled, randomized, eight week studies were conducted in patients with endoscopically confirmed EE. Severity of the disease was classified based on the Los Angeles Classification Grading System (Grades A-D). Patients were randomized to one of the following three treatment groups: dexlansoprazole 60 mg once daily, dexlansoprazole 90 mg once daily or lansoprazole 30 mg once daily. Patients who were H. pylori positive or who had Barrett’s Esophagus and/or definite dysplastic changes at baseline were excluded from these studies. A total of 4092 patients were enrolled and ranged in age from 18 to 90 years (median age 48 years) with 54% male. Race was distributed as follows: 87% Caucasian, 5% Black and 8% Other. Based on the Los Angeles Classification, 71% of patients had mild EE (Grades A and B) and 29% of patients had moderate to severe EE (Grades C and D) before treatment.
The studies were designed to test noninferiority. If noninferiority was demonstrated then superiority would be tested. Although noninferiority was demonstrated in both studies, the finding of superiority in one study was not replicated in the other.
The proportion of patients with healed EE at Week 4 or 8 is presented below in Table 8.
Table 8. EE Healing Rates* in Adults: All Grades|
CI = Confidence interval | |||||
| |||||
|
Study |
Number of Patients (N)† |
Treatment Group |
Week 4 Healed |
Week 8‡ % Healed |
(95% CI) for the Treatment Difference (Dexlansoprazole–Lansoprazole) by Week 8 |
|
1 |
657 |
Dexlansoprazole 60 mg |
70 |
87 |
(-1.5, 6.1)§ |
|
648 |
Lansoprazole 30 mg |
65 |
85 | ||
|
2 |
639 |
Dexlansoprazole 60 mg |
66 |
85 |
(2.2, 10.5)§ |
|
656 |
Lansoprazole 30 mg |
65 |
79 |
Dexlansoprazole 90 mg once daily was studied and did not provide additional clinical benefit over dexlansoprazole 60 mg once daily.
14.2 Maintenance of Healed Erosive Esophagitis and Relief of Heartburn in
Adults
A multicenter, double-blind, placebo-controlled, randomized study was conducted in patients who successfully completed an EE study and showed endoscopically confirmed healed EE. Maintenance of healing and symptom resolution over a six month period was evaluated with dexlansoprazole 30 or 60 mg once daily compared to placebo. A total of 445 patients were enrolled and ranged in age from 18 to 85 years (median age 49 years), with 52% female. Race was distributed as follows: 90% Caucasian, 5% Black and 5% Other.
Sixty-six percent of patients treated with 30 mg of dexlansoprazole remained healed over the six month time period as confirmed by endoscopy (see Table 9).
Table 9. Maintenance Rates* of Healed EE at Month 6 in Adults
| ||
|
Number of Patients |
Treatment Group |
Maintenance Rate |
|
125 |
Dexlansoprazole 30 mg |
66.4‡ |
|
119 |
Placebo |
14.3 |
Dexlansoprazole 60 mg once daily was studied and did not provide additional clinical benefit over dexlansoprazole 30 mg once daily.
The effect of dexlansoprazole 30 mg on maintenance of relief of heartburn was also evaluated. Upon entry into the maintenance study, a majority of patients’ baseline heartburn severity was rated as none. Dexlansoprazole 30 mg demonstrated a statistically significantly higher percent of 24 hour heartburn-free periods compared to placebo over the six month treatment period (see Table 10). The majority of patients treated with placebo discontinued due to relapse of EE between Month 2 and Month 6.
Table 10. Median Percentage of 24-Hour Heartburn-Free Periods of the Maintenance of Healed EE Study in Adults
| ||||||
|
Overall Treatment* |
Month 1 |
Month 6 | ||||
|
Treatment Group (daily) |
N |
Heartburn-Free 24 hour Periods |
N |
Heartburn-Free 24 hour Periods |
N |
Heartburn-Free 24 hour Periods |
|
Dexlansoprazole |
132 |
96.1† |
126 |
96.7 |
80 |
98.3 |
|
Placebo |
141 |
28.6 |
117 |
28.6 |
23 |
73.3 |
14.3 Treatment of Symptomatic Non-Erosive GERD in Adults
A multicenter, double-blind, placebo-controlled, randomized, four week study was conducted in patients with a diagnosis of symptomatic non-erosive GERD made primarily by presentation of symptoms. These patients who identified heartburn as their primary symptom, had a history of heartburn for six months or longer, had heartburn on at least four of seven days immediately prior to randomization and had no esophageal erosions as confirmed by endoscopy. However, patients with symptoms which were not acid-related may not have been excluded using these inclusion criteria. Patients were randomized to one of the following treatment groups: dexlansoprazole 30 mg daily, 60 mg daily, or placebo. A total of 947 patients were enrolled and ranged in age from 18 to 86 years (median age 48 years) with 71% female. Race was distributed as follows: 82% Caucasian, 14% Black and 4% Other.
Dexlansoprazole 30 mg provided statistically significantly greater percent of days with heartburn-free 24 hour periods over placebo as assessed by daily diary over four weeks (see Table 11). Dexlansoprazole 60 mg once daily was studied and provided no additional clinical benefit over dexlansoprazole 30 mg once daily.
Table 11. Median Percentages of 24 Hour Heartburn-Free Periods During the 4 Week Treatment Period of the Symptomatic Non-Erosive GERD Study in Adults
| ||
|
N |
Treatment Group (daily) |
Heartburn-Free 24hour Periods (%) |
|
312 |
Dexlansoprazole 30 mg |
54.9* |
|
310 |
Placebo |
18.5 |
A higher percentage of patients on dexlansoprazole 30 mg had heartburn-free 24 hour periods compared to placebo as early as the first three days of treatment and this was sustained throughout the treatment period (percentage of patients on Day 3: dexlansoprazole 38% vs placebo 15%; on Day 28: dexlansoprazole 63% vs placebo 40%).
14.4 Pediatric GERD
Use of dexlansoprazole in patients 12 to 17 years of age is supported by evidence from adequate and well-controlled studies of dexlansoprazole delayed- release capsules in adults, with additional safety, efficacy, and pharmacokinetic data from studies performed in pediatric patients.
Healing of EE, Maintenance of Healed EE and Relief of Heartburn
In a multicenter, 36 week trial, 62 patients 12 to 17 years of age with a documented history of GERD for at least three months and endoscopically-proven erosive esophagitis (EE) were enrolled to evaluate the healing of EE, maintenance of healed EE and relief of heartburn, followed by an additional 12 weeks without treatment.
The median age was 15 years, with males accounting for 61% of the patients. Based on the Los Angeles Classification Grading Scale, 97% of patients had mild EE (Grades A and B), and 3% of patients had moderate to severe EE (Grades C and D) before treatment.
In the first eight weeks, 62 patients were treated with dexlansoprazole 60 mg once daily to evaluate the healing of EE. Of the 62 patients, 58 patients completed the eight week trial, and 51 (88%) patients achieved healing of EE, as confirmed by endoscopy, over eight weeks of treatment (see Table 12).
Table 12. Healing of EE at Week 8 in Pediatric Patients 12 to 17 Years of Age
| |
|
Dexlansoprazole 60 mg | |
|
Proportion of randomized patients healed n (%) 95% CI |
51/62 (82%) (70, 91)* |
|
Proportion of evaluable patients healed† n (%) 95% CI |
51/58 (88%) (77, 95)* |
After the initial eight weeks of treatment, all 51 patients with healed EE were randomized to receive treatment with dexlansoprazole 30 mg or placebo, once daily for an additional 16 weeks to evaluate maintenance of healing and symptom resolution. Maintenance of healing was assessed by endoscopy at Week 24. Of the 51 patients randomized, 13 patients discontinued early. Of these, five patients did not undergo postbaseline endoscopy. Eighteen of 22 (82%) evaluable patients treated with dexlansoprazole 30 mg remained healed over the 16 week treatment period as confirmed by endoscopy, compared with 14 of 24 (58%) in placebo (see Table 13).
Table 13. Maintenance of Healed EE at Week 24* in Pediatric Patients 12 to 17 Years of Age
| ||
|
Dexlansoprazole 30 mg |
Placebo | |
|
Proportion of randomized patients who maintained healing of EE n (%) 95% CI |
18/25 (72%) (51, 88)† |
14/26 (54%) (33, 73)† |
|
Proportion of evaluable patients who maintained healing of EE‡ n (%) 95% CI |
18/22 (82%) (60, 95)† |
14/24 (58%) (37, 78)† |
Relief of heartburn was assessed in randomized patients during the 16 week maintenance period. The median percentage of 24 hour heartburn-free periods was 87% for those receiving dexlansoprazole 30 mg compared to 68% for those receiving placebo.
Out of the 32 patients who maintained healing of EE at the end of the 16 week maintenance period, 27 patients (16 treated with dexlansoprazole and 11 treated with placebo during the double-blind phase) were followed for an additional 12 weeks without therapy. Twenty-four of the 27 patients completed the 12 week follow-up period. One patient required treatment with acid suppression therapy.
Treatment of Symptomatic Non-Erosive GERD
In a single-arm, open-label, multicenter trial, 104 pediatric patients 12 to 17 years of age with symptomatic non-erosive GERD were treated with dexlansoprazole 30 mg once daily, for four weeks to evaluate safety and effectiveness. Patients had a documented history of GERD symptoms for at least three months prior to screening, reported heartburn on at least three out of seven days during screening, and had no esophageal erosions as confirmed by endoscopy. The median age was 15 years, with females accounting for 70% of the patients. During the four week treatment period, the median percentage of 24 hour heartburn free periods was 47%.
