KETOROLAC TROMETHAMINE
KETOROLAC TROMETHAMINE TABLETS USP, 10 mgRx only
5f2c3dd1-8715-47ba-98f8-311d4656be90
HUMAN PRESCRIPTION DRUG LABEL
Jan 25, 2023
WOODWARD PHARMA SERVICES LLC
DUNS: 080406260
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
ketorolac tromethamine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (4)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
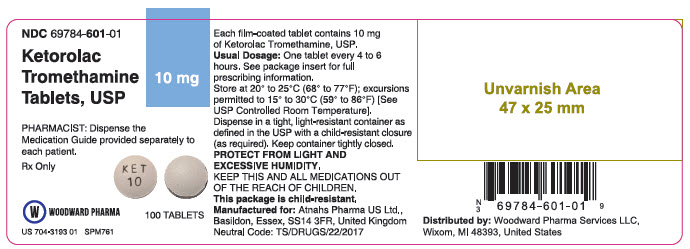
PRINCIPAL DISPLAY PANEL - 10 mg Tablet Bottle Label
NDC 69784-601-01
Ketorolac Tromethamine Tablets, USP
10 mg
PHARMACIST: Dispense the Medication Guide provided separately to each patient.
Rx Only
100 TABLETS
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
PROTECT FROM LIGHT AND EXCESSIVE HUMIDITY.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
US 704-3193 01 SPM761
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
Carefully consider the potential benefits and risks of Ketorolac Tromethamine Tablets USP and other treatment options before deciding to use Ketorolac Tromethamine Tablets USP. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals.
Acute Pain in Adult Patients
Ketorolac Tromethamine Tablets USP are indicated for the short-term (≤ 5 days) management of moderately severe acute pain that requires analgesia at the opioid level, usually in a postoperative setting. Therapy should always be initiated with IV or IM dosing of ketorolac tromethamine and Ketorolac Tromethamine Tablets USP are to be used only as continuation treatment, if necessary.
The total combined duration of use of Ketorolac Tromethamine Tablets USP and ketorolac tromethamine is not to exceed 5 days of use because of the potential of increasing the frequency and severity of adverse reactions associated with the recommended doses (seeWARNINGS****,PRECAUTIONS,DOSAGE AND ADMINISTRATION, andADVERSE REACTIONS). Patients should be switched to alternative analgesics as soon as possible, but Ketorolac Tromethamine Tablet USP therapy is not to exceed 5 days.
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
Adverse reaction rates increase with higher doses of ketorolac tromethamine. Practitioners should be alert for the severe complications of treatment with ketorolac tromethamine, such as GI ulceration, bleeding and perforation, postoperative bleeding, acute renal failure, anaphylactic and anaphylactoid reactions and liver failure (seeBoxed WARNING****,WARNINGS, PRECAUTIONS, andDOSAGE AND ADMINISTRATION). These NSAID-related complications can be serious in certain patients for whom ketorolac tromethamine is indicated, especially when the drug is used inappropriately.
In patients taking ketorolac tromethamine or other NSAIDs in clinical trials, the most frequently reported adverse experiences in approximately 1% to 10% of patients are:
Gastrointestinal (GI) experiences including:
| ||
|
abdominal pain* |
constipation/diarrhea |
dyspepsia* |
|
flatulence |
GI fullness |
GI ulcers (gastric/duodenal) |
|
gross bleeding/perforation |
heartburn |
nausea* |
|
stomatitis |
vomiting | |
|
Other experiences: | ||
|
abnormal renal function |
anemia |
dizziness |
|
drowsiness |
edema |
elevated liver enzymes |
|
headaches* |
hypertension |
increased bleeding time |
|
injection site pain |
pruritus |
purpura |
|
rashes |
tinnitus |
sweating |
Additional adverse experiences reported occasionally (< 1% in patients taking ketorolac tromethamine or other NSAIDs in clinical trials) include:
Body as a Whole: fever, infections, sepsis
Cardiovascular: congestive heart failure, palpitation, pallor, tachycardia, syncope
Dermatologic: alopecia, photosensitivity, urticaria
Gastrointestinal: anorexia, dry mouth, eructation, esophagitis, excessive thirst, gastritis, glossitis, hematemesis, hepatitis, increased appetite, jaundice, melena, rectal bleeding
Hemic and Lymphatic: ecchymosis, eosinophilia, epistaxis, leukopenia, thrombocytopenia
Metabolic and Nutritional: weight change
Nervous System: abnormal dreams, abnormal thinking, anxiety, asthenia, confusion, depression, euphoria, extrapyramidal symptoms, hallucinations, hyperkinesis, inability to concentrate, insomnia, nervousness, paresthesia, somnolence, stupor, tremors, vertigo, malaise
Reproductive, female: infertility
Respiratory: asthma, cough, dyspnea, pulmonary edema, rhinitis
Special Senses: abnormal taste, abnormal vision, blurred vision, hearing loss
Urogenital: cystitis, dysuria, hematuria, increased urinary frequency, interstitial nephritis, oliguria/polyuria, proteinuria, renal failure, urinary retention
Other rarely observed reactions (reported from postmarketing experience in patients taking ketorolac tromethamine or other NSAIDs) are:
Body as a Whole: angioedema, death, hypersensitivity reactions such as anaphylaxis, anaphylactoid reaction, laryngeal edema, tongue edema (see WARNINGS), myalgia
Cardiovascular: arrhythmia, bradycardia, chest pain, flushing, hypotension, myocardial infarction, vasculitis
Dermatologic: exfoliative dermatitis, erythema multiforme, Lyell's syndrome, bullous reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis
Gastrointestinal: acute pancreatitis, liver failure, ulcerative stomatitis, exacerbation of inflammatory bowel disease (ulcerative colitis, Crohn's disease)
Hemic and Lymphatic: agranulocytosis, aplastic anemia, hemolytic anemia, lymphadenopathy, pancytopenia, postoperative wound hemorrhage (rarely requiring blood transfusion - see**Boxed WARNING****,**WARNINGS, and PRECAUTIONS)
Metabolic and Nutritional: hyperglycemia, hyperkalemia, hyponatremia
Nervous System: aseptic meningitis, convulsions, coma, psychosis
Respiratory: bronchospasm, respiratory depression, pneumonia
Special Senses: conjunctivitis
Urogenital: flank pain with or without hematuria and/or azotemia, hemolytic uremic syndrome
Postmarketing Surveillance Study
A large postmarketing observational, nonrandomized study, involving approximately 10,000 patients receiving ketorolac tromethamineIV/IM, demonstrated that the risk of clinically serious gastrointestinal (GI) bleeding was dose-dependent (seeTables 3A and3B). This was particularly true in elderly patients who received an average daily dose greater than 60 mg/day of ketorolac tromethamineIV/IM (seeTable 3A).
Table 3: Incidence of Clinically Serious GI Bleeding as Related to Age, Total Daily Dose, and History of GI Perforation, Ulcer, Bleeding (PUB) After up to 5 Days of Treatment With Ketorolac TromethamineIV/IM|
A. Adult Patients Without History of PUB | ||||
|
Age of Patients |
Total Daily Dose of Ketorolac TromethamineIV/IM | |||
|
≤ 60 mg |
|
|
| |
|
< 65 years of age |
0.4% |
0.4% |
0.9% |
4.6% |
|
≥ 65 years of age |
1.2% |
2.8% |
2.2% |
7.7% |
|
B. Adult Patients With History of PUB | ||||
|
Age of Patients |
Total Daily Dose of Ketorolac TromethamineIV/IM | |||
|
≤ 60 mg |
|
|
| |
|
< 65 years of age |
2.1% |
4.6% |
7.8% |
15.4% |
|
≥ 65 years of age |
4.7% |
3.7% |
2.8% |
25% |
CLINICAL STUDIES SECTION
CLINICAL STUDIES
Adult Patients
In a postoperative study, where all patients received morphine by a PCA device, patients treated with ketorolac tromethamineIV as fixed intermittent boluses (e.g., 30 mg initial dose followed by 15 mg q3h), required significantly less morphine (26%) than the placebo group. Analgesia was significantly superior, at various postdosing pain assessment times, in the patients receiving ketorolac tromethamineIV plus PCA morphine as compared to patients receiving PCA-administered morphine alone.
Pediatric Patients
There are no data available to support the use of ketorolac tromethamine tablets in pediatric patients.
WARNINGS SECTION
WARNINGS
** (See alsoBoxed WARNING)**
The total combined duration of use of ketorolac tromethamine tablets and IV or IM dosing of ketorolac tromethamine is not to exceed 5 days in adults. Ketorolac tromethamine tablets are not indicated for use in pediatric patients.
The most serious risks associated with ketorolac tromethamine are:
Gastrointestinal Effects – Risk of Ulceration, Bleeding, and Perforation
Ketorolac tromethamine is contraindicated in patients with previously documented peptic ulcers and/or GI bleeding. Ketorolac tromethamine can cause serious gastrointestinal (GI) adverse events including bleeding, ulceration and perforation, of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with ketorolac tromethamine.
Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Minor upper gastrointestinal problems, such as dyspepsia, are common and may also occur at any time during NSAID therapy. The incidence and severity of gastrointestinal complications increases with increasing dose of, and duration of treatment with, ketorolac tromethamine. Do not use ketorolac tromethamine for more than five days. However, even short- term therapy is not without risk. In addition to past history of ulcer disease, other factors that increase the risk for GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids, or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population.
To minimize the potential risk for an adverse GI event, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. This should include discontinuation of ketorolac tromethamine until a serious GI adverse event is ruled out. For high risk patients, alternate therapies that do not involve NSAIDs should be considered.
NSAIDs should be given with care to patients with a history of inflammatory bowel disease (ulcerative colitis, Crohn's disease) as their condition may be exacerbated.
Hemorrhage
Because prostaglandins play an important role in hemostasis and NSAIDs affect platelet aggregation as well, use of ketorolac tromethamine in patients who have coagulation disorders should be undertaken very cautiously, and those patients should be carefully monitored. Patients on therapeutic doses of anticoagulants (e.g., heparin or dicumarol derivatives) have an increased risk of bleeding complications if given ketorolac tromethamine concurrently; therefore, physicians should administer such concomitant therapy only extremely cautiously. The concurrent use of ketorolac tromethamine and therapy that affects hemostasis, including prophylactic low-dose heparin (2500 to 5000 units q12h), warfarin and dextrans have not been studied extensively, but may also be associated with an increased risk of bleeding. Until data from such studies are available, physicians should carefully weigh the benefits against the risks and use such concomitant therapy in these patients only extremely cautiously. Patients receiving therapy that affects hemostasis should be monitored closely.
In postmarketing experience, postoperative hematomas and other signs of wound bleeding have been reported in association with the peri-operative use of IV or IM dosing of ketorolac tromethamine. Therefore, peri-operative use of ketorolac tromethamine should be avoided and postoperative use be undertaken with caution when hemostasis is critical (seePRECAUTIONS).
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a NSAID may cause a dose- dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Ketorolac tromethamine and its metabolites are eliminated primarily by the kidneys, which, in patients with reduced creatinine clearance, will result in diminished clearance of the drug (seeCLINICAL PHARMACOLOGY). Therefore, ketorolac tromethamine should be used with caution in patients with impaired renal function (seeDOSAGE AND ADMINISTRATION) and such patients should be followed closely. With the use of ketorolac tromethamine, there have been reports of acute renal failure, interstitial nephritis and nephrotic syndrome.
Impaired Renal Function
Ketorolac tromethamine is contraindicated in patients with serum creatinine concentrations indicating advanced renal impairment (see CONTRAINDICATIONS). Ketorolac tromethamine should be used with caution in patients with impaired renal function or a history of kidney disease because it is a potent inhibitor of prostaglandin synthesis. Because patients with underlying renal insufficiency are at increased risk of developing acute renal decompensation or failure, the risks and benefits should be assessed prior to giving ketorolac tromethamine to these patients.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without a known previous exposure or hypersensitivity to ketorolac tromethamine. Ketorolac tromethamine should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONS andPRECAUTIONS, Preexisting Asthma). Anaphylactoid reactions, like anaphylaxis, may have a fatal outcome. Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Cardiovascular Effects
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as ketorolac tromethamine, increases the risk of serious gastrointestinal (GI) events (seeWARNINGS).
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG (seeCONTRAINDICATIONS).
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post MI was 20 per 100 person years in NSAID- treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of ketorolac tromethamine tablets in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If ketorolac tromethamine tablets are used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
Hypertension
NSAIDs, including ketorolac tromethamine, can lead to onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including ketorolac tromethamine, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
HEART FAILURE AND EDEMA
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of ketorolac tromethamine may blunt the CV effects of several therapeutic agents used to treat these medical conditions [e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers (ARBs)] (see DRUG INTERACTIONS).
Avoid the use of ketorolac tromethamine tablets in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If ketorolac tromethamine tablets are used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
Skin Reactions
NSAIDs, including ketorolac tromethamine, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash, mucosal lesions, or any other sign of hypersensitivity.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been reported in patients taking NSAIDs such as ketorolac tromethamine tablets. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling. Other clinical manifestations may include hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis. Sometimes symptoms of DRESS may resemble an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its presentation, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, discontinue ketorolac tromethamine tablets and evaluate the patient immediately.
FETAL TOXICITY
Premature Closure of Fetal Ductus Arteriosus:
Avoid use of NSAIDs, including ketorolac tromethamine tablets, in pregnant women at about 30 weeks gestation and later. NSAIDs including ketorolac tromethamine tablets, increase the risk of premature closure of the fetal ductus arteriosus at approximately this gestational age.
Oligohydramnios/Neonatal Renal Impairment:
Use of NSAIDs, including ketorolac tromethamine tablets, at about 20 weeks gestation or later in pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation.
Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may, for example, include limb contractures and delayed lung maturation. In some postmarketing cases of impaired neonatal renal function, invasive procedures such as exchange transfusion or dialysis were required.
If NSAID treatment is necessary between about 20 weeks and 30 weeks gestation, limit ketorolac tromethamine tablets use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if ketorolac tromethamine tablets treatment extends beyond 48 hours. Discontinue ketorolac tromethamine tablets if oligohydramnios occurs and follow up according to clinical practice (see PRECAUTIONS; Pregnancy).
HOW SUPPLIED SECTION
HOW SUPPLIED
Ketorolac Tromethamine Tablets are available as follows:
10 mg: White to off white, round and biconvex film coated tablets debossed with "KET10" on one side. They are available in bottles of 100 tablets (NDC 69784-601-01).
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
PROTECT FROM LIGHT AND EXCESSIVE HUMIDITY.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
