POSACONAZOLE
These highlights do not include all the information needed to use POSACONAZOLE DELAYED-RELEASE TABLETS safely and effectively. See full prescribing information for POSACONAZOLE DELAYED-RELEASE TABLETS.POSACONAZOLE delayed-release tablets, for oral use.Initial U.S. Approval: 2006
111ab7c6-b0c3-4d15-9f40-6c03d3d16bc2
HUMAN PRESCRIPTION DRUG LABEL
Sep 27, 2023
Cardinal Health 107, LLC
DUNS: 118546603
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
POSACONAZOLE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (15)
Drug Labeling Information
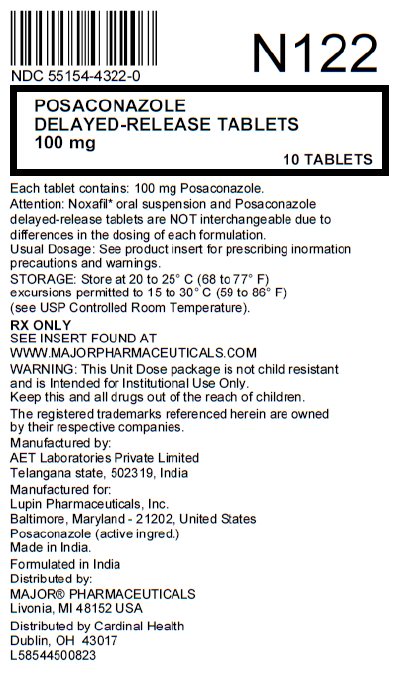
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Package/Label Display Panel
Posaconazole Delayed-Release Tablets
100 mg
10 Tablets
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Prophylaxis of Invasive Aspergillus and Candida Infections
Posaconazole is indicated for the prophylaxis of invasive Aspergillus and Candida infections in patients who are at high risk of developing these infections due to being severely immunocompromised, such as hematopoietic stem cell transplant (HSCT) recipients with graft-versus-host disease (GVHD) or those with hematologic malignancies with prolonged neutropenia from chemotherapy [see Clinical Studies (14.1)] as follows:
Posaconazole delayed-release tablets: adults and pediatric patients 13 years of age and older.
Additional Pediatric Use information is approved for Merck Sharp & Dohme Corp.'s NOXAFIL (posaconazole) delayed-release tablets. However, due to Merck Sharp & Dohme Corp.'s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Posaconazole is an azole antifungal indicated as follows: (1)
•
Posaconazole is indicated for the prophylaxis of invasive Aspergillus and Candida infections in patients who are at high risk of developing these infections due to being severely immunocompromised, such as hematopoietic stem cell transplant (HSCT) recipients with graft-versus-host disease (GVHD)or those with hematologic malignancies with prolonged neutropenia from chemotherapy as follows: (1.1)
•
**Posaconazole delayed-release tablets:** adults and pediatric patients 13 years of age and older
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Calcineurin-Inhibitor Drug Interactions
Concomitant administration of posaconazole with cyclosporine or tacrolimus increases the whole blood trough concentrations of these calcineurin- inhibitors [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)]. Nephrotoxicity and leukoencephalopathy (including deaths) have been reported in clinical efficacy studies in patients with elevated cyclosporine or tacrolimus concentrations. Frequent monitoring of tacrolimus or cyclosporine whole blood trough concentrations should be performed during and at discontinuation of posaconazole treatment and the tacrolimus or cyclosporine dose adjusted accordingly.
5.2 Arrhythmias and QT Prolongation
Some azoles, including posaconazole, have been associated with prolongation of the QT interval on the electrocardiogram. In addition, cases of torsades de pointes have been reported in patients taking posaconazole.
Results from a multiple time-matched ECG analysis in healthy volunteers did not show any increase in the mean of the QTc interval. Multiple, time-matched ECGs collected over a 12-hour period were recorded at baseline and steady- state from 173 healthy male and female volunteers (18-85 years of age) administered posaconazole oral suspension 400 mg twice daily with a high-fat meal. In this pooled analysis, the mean QTc (Fridericia) interval change from baseline was –5 msec following administration of the recommended clinical dose. A decrease in the QTc(F) interval (–3 msec) was also observed in a small number of subjects (n=16) administered placebo. The placebo-adjusted mean maximum QTc(F) interval change from baseline was <0 msec (–8 msec). No healthy subject administered posaconazole had a QTc(F) interval ≥500 msec or an increase ≥60 msec in their QTc(F) interval from baseline.
Posaconazole should be administered with caution to patients with potentially proarrhythmic conditions. Do not administer with drugs that are known to prolong the QTc interval and are metabolized through CYP3A4 [see Contraindications (4.3) and Drug Interactions (7.2)].
5.3 Electrolyte Disturbances
Electrolyte disturbances, especially those involving potassium, magnesium or calcium levels, should be monitored and corrected as necessary before and during posaconazole therapy.
5.4 Hepatic Toxicity
Hepatic reactions (e.g., mild to moderate elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, total bilirubin, and/or clinical hepatitis) have been reported in clinical trials. The elevations in liver tests were generally reversible on discontinuation of therapy, and in some instances these tests normalized without drug interruption. Cases of more severe hepatic reactions including cholestasis or hepatic failure including deaths have been reported in patients with serious underlying medical conditions (e.g., hematologic malignancy) during treatment with posaconazole. These severe hepatic reactions were seen primarily in subjects receiving the posaconazole oral suspension 800 mg daily (400 mg twice daily or 200 mg four times a day) in clinical trials.
Liver tests should be evaluated at the start of and during the course of posaconazole therapy. Patients who develop abnormal liver tests during posaconazole therapy should be monitored for the development of more severe hepatic injury. Patient management should include laboratory evaluation of hepatic function (particularly liver tests and bilirubin). Discontinuation of posaconazole must be considered if clinical signs and symptoms consistent with liver disease develop that may be attributable to posaconazole.
5.5 Renal Impairment
Due to the variability in exposure with Posaconazole delayed-release tablets, patients with severe renal impairment should be monitored closely for breakthrough fungal infections [see Dosage and Administration (2.9) and Use in Specific Populations (8.6)].
5.6 Concomitant Use with Midazolam
Concomitant administration of posaconazole with midazolam increases the midazolam plasma concentrations by approximately 5-fold. Increased plasma midazolam concentrations could potentiate and prolong hypnotic and sedative effects. Patients must be monitored closely for adverse effects associated with high plasma concentrations of midazolam and benzodiazepine receptor antagonists must be available to reverse these effects [see Drug Interactions (7.5) and Clinical Pharmacology (12.3)].
5.7 Vincristine Toxicity
Concomitant administration of azole antifungals, including posaconazole, with vincristine has been associated with neurotoxicity and other serious adverse reactions, including seizures, peripheral neuropathy, syndrome of inappropriate antidiuretic hormone secretion, and paralytic ileus. Reserve azole antifungals, including posaconazole, for patients receiving a vinca alkaloid, including vincristine, who have no alternative antifungal treatment options [see Drug Interactions (7.10)].
5.9 Breakthrough Fungal Infections
Patients who have severe diarrhea or vomiting should be monitored closely for breakthrough fungal infections when receiving posaconazole delayed-release tablets.
•
Calcineurin-Inhibitor Toxicity: posaconazole increases concentrations of cyclosporine or tacrolimus; reduce dose of cyclosporine and tacrolimus and monitor concentrations frequently. (5.1)
•
Arrhythmias and QTc Prolongation: posaconazole has been shown to prolong the QTc interval and cause cases of TdP. Administer with caution to patients with potentially proarrhythmic conditions. Do not administer with drugs known to prolong QTc interval and metabolized through CYP3A4. (5.2)
•
Electrolyte Disturbances: Monitor and correct, especially those involving potassium (K+), magnesium (Mg++), and calcium (Ca++), before and during posaconazole therapy. (5.3)
•
Hepatic Toxicity: Elevations in liver tests may occur. Discontinuation should be considered in patients who develop abnormal liver tests or monitor liver tests during treatment. (5.4)
•
Concomitant use with Midazolam: posaconazole can prolong hypnotic/sedative effects. Monitor patients and benzodiazepine receptor antagonists should be available. (5.6, 7.5)
•
Vincristine Toxicity: Concomitant administration of azole antifungals, including posaconazole, with vincristine has been associated with neurotoxicity and other serious adverse reactions; reserve azole antifungals, including posaconazole, for patients receiving a vinca alkaloid, including vincristine, who have no alternative antifungal treatment options. (5.7, 7.10)
•
Breakthrough Fungal Infections: Monitor patients with severe diarrhea or vomiting when receiving posaconazole delayed-release tablets. (5.9)
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Prophylaxis of Aspergillus and Candida Infections with Posaconazole
Oral Suspension
Two randomized, controlled studies were conducted using posaconazole as prophylaxis for the prevention of invasive fungal infections (IFIs) among patients at high risk due to severely compromised immune systems.
The first study (Oral Suspension Study 1) was a randomized, double-blind trial that compared posaconazole oral suspension (200 mg three times a day) with fluconazole capsules (400 mg once daily) as prophylaxis against invasive fungal infections in allogeneic hematopoietic stem cell transplant (HSCT) recipients with Graft versus Host Disease (GVHD). Efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy (patients may have met more than one of these criteria). This assessed all patients while on study therapy plus 7 days and at 16 weeks post-randomization. The mean duration of therapy was comparable between the 2 treatment groups (80 days, posaconazole; 77 days, fluconazole).Table 28contains the results from Oral Suspension Study 1.
Table 28: Results from Blinded Clinical Study in Prophylaxis of IFI in All Randomized Patients with Hematopoietic Stem Cell Transplant (HSCT) and Graft-vs.-Host Disease (GVHD): Oral Suspension Study 1|
** Posaconazole n=301** |
** Fluconazole n=299** | |
|
On therapy plus 7 days | ||
|
** Clinical Failure*** |
50 (17%) |
55 (18%) |
|
** Failure due to:** | ||
|
Proven/Probable IFI |
7 (2%) |
22 (7%) |
|
(Aspergillus ) |
3 (1%) |
17 (6%) |
|
(Candida ) |
1 (<1%) |
3 (1%) |
|
(Other) |
3 (1%) |
2 (1%) |
|
All Deaths |
22 (7%) |
24 (8%) |
|
SAF† |
27 (9%) |
25 (8%) |
|
Through 16 weeks | ||
|
** Clinical Failure*,‡** |
99 (33%) |
110 (37%) |
|
** Failure due to:** | ||
|
Proven/Probable IFI |
16 (5%) |
27 (9%) |
|
(Aspergillus ) |
7 (2%) |
21 (7%) |
|
(Candida ) |
4 (1%) |
4 (1%) |
|
(Other) |
5 (2%) |
2 (1%) |
|
All Deaths |
58 (19%) |
59 (20%) |
|
SAF† |
26 (9%) |
30 (10%) |
|
Event free lost to follow-up§ |
24 (8%) |
30 (10%) |
|
The second study (Oral Suspension Study 2) was a randomized, open-label study that compared posaconazole oral suspension (200 mg 3 times a day) with fluconazole suspension (400 mg once daily) or itraconazole oral solution (200 mg twice a day) as prophylaxis against IFIs in neutropenic patients who were receiving cytotoxic chemotherapy for AML or MDS. As in Oral Suspension Study 1, efficacy of prophylaxis was evaluated using a composite endpoint of proven/probable IFIs, death, or treatment with systemic antifungal therapy (Patients might have met more than one of these criteria). This study assessed patients while on treatment plus 7 days and 100 days postrandomization. The mean duration of therapy was comparable between the 2 treatment groups (29 days, posaconazole; 25 days, fluconazole or itraconazole).**Table 29 **contains the results from Oral Suspension Study 2.
Table 29: Results from Open-Label Clinical Study 2 in Prophylaxis of IFI in All Randomized Patients with Hematologic Malignancy and Prolonged Neutropenia: Oral Suspension Study 2|
** Posaconazole n=304** |
** Fluconazole/Itraconazole n=298** | |
|
On therapy plus 7 days | ||
|
** Clinical Failure*,†** |
82 (27%) |
126 (42%) |
|
** Failure due to:** | ||
|
Proven/Probable IFI |
7 (2%) |
25 (8%) |
|
(Aspergillus ) |
2 (1%) |
20 (7%) |
|
(Candida ) |
3 (1%) |
2 (1%) |
|
(Other) |
2 (1%) |
3 (1%) |
|
All Deaths |
17 (6%) |
25 (8%) |
|
SAF‡ |
67 (22%) |
98 (33%) |
|
Through 100 days postrandomization | ||
|
** Clinical Failure†** |
158 (52%) |
191 (64%) |
|
** Failure due to:** | ||
|
Proven/Probable IFI |
14 (5%) |
33 (11%) |
|
(Aspergillus ) |
2 (1%) |
26 (9%) |
|
(Candida ) |
10 (3%) |
4 (1%) |
|
(Other) |
2 (1%) |
3 (1%) |
|
All Deaths |
44 (14%) |
64 (21%) |
|
SAF‡ |
98 (32%) |
125 (42%) |
|
Event free lost to follow-up§ |
34 (11%) |
24 (8%) |
|
In summary, 2 clinical studies of prophylaxis were conducted with the posaconazole oral suspension. As seen in the accompanying tables (Tables 28 and 29), clinical failure represented a composite endpoint of breakthrough IFI, mortality and use of systemic antifungal therapy. In Oral Suspension Study 1 (Table 28), the clinical failure rate of posaconazole (33%) was similar to fluconazole (37%), (95% CI for the difference posaconazole–comparator -11.5% to 3.7%) while in Oral Suspension Study 2 (Table 29) clinical failure was lower for patients treated with posaconazole (27%) when compared to patients treated with fluconazole or itraconazole (42%), (95% CI for the difference posaconazole–comparator -22.9% to 7.8%).
All-cause mortality was similar at 16 weeks for both treatment arms in Oral Suspension Study 1 [POS 58/301 (19%) vs. FLU 59/299 (20%)]; all-cause mortality was lower at 100 days for posaconazole-treated patients in Oral Suspension Study 2 [POS 44/304 (14%) vs. FLU/ITZ 64/298 (21%)]. Both studies demonstrated fewer breakthrough infections caused by Aspergillus species in patients receiving posaconazole prophylaxis when compared to patients receiving fluconazole or itraconazole.
