Naltrexone Hydrochloride
Naltrexone Hydrochloride Tablets, USP 50 mg
94c3e2de-36e4-42d4-b6e8-53b4aff1c4ed
HUMAN PRESCRIPTION DRUG LABEL
Jan 25, 2023
Bryant Ranch Prepack
DUNS: 171714327
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Naltrexone Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
DESCRIPTION SECTION
DESCRIPTION
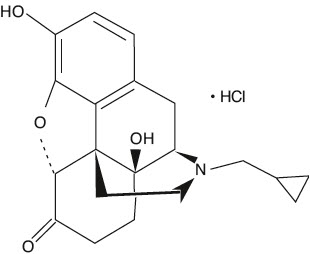
Naltrexone hydrochloride, an opioid antagonist, are a synthetic congener of oxymorphone with no opioid agonist properties. Naltrexone differs in structure from oxymorphone in that the methyl group on the nitrogen atom is replaced by a cyclopropylmethyl group. Naltrexone hydrochloride is also related to the potent opioid antagonist, naloxone, or n-allylnoroxymorphone. The chemical name for naltrexone hydrochloride is Morphinan-6-one, 17-(cyclopropylmethyl)-4,5-epoxy-3,14-dihydroxy-, hydrochloride, (5a)-. The structural formula is as follows:
|
C20H23NO4∙HCl |
|
Molecular Weight: 377.86 |
Naltrexone hydrochloride is a white, crystalline compound. The hydrochloride salt is soluble in water to the extent of about 100 mg/mL. Naltrexone Hydrochloride Tablets USP are available in scored film-coated tablets containing 50 mg of naltrexone hydrochloride. Naltrexone Hydrochloride Tablets USP also contain: carnauba wax powder, colloidal silicon dioxide, croscarmellose sodium, hypromellose, hydroxypropyl cellulose, lactose anhydrous, magnesium stearate, microcrystalline cellulose, polyethylene glycol, titanium dioxide and yellow iron oxide.
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
To reduce the risk of precipitated withdrawal in patients dependent on opioids, or exacerbation of a preexisting subclinical withdrawal syndrome, opioid-dependent patients, including those being treated for alcohol dependence, should be opioid-free (including tramadol) before starting naltrexone hydrochloride tablets treatment. An opioid-free interval of a minimum of 7 to 10 days is recommended for patients previously dependent on short-acting opioids.
Switching from Buprenorphine, Buprenorphine/Naloxone, or Methadone
There are no systematically collected data that specifically address the switch from buprenorphine or methadone to naltrexone hydrochloride tablets; however, review of postmarketing case reports have indicated that some patients may experience severe manifestations of precipitated withdrawal when being switched from opioid agonist therapy to opioid antagonist therapy (see WARNINGS). Patients transitioning from buprenorphine or methadone may be vulnerable to precipitation of withdrawal symptoms for as long as 2 weeks. Healthcare providers should be prepared to manage withdrawal symptomatically with non-opioid medications.
Treatment of Alcoholism
A dose of 50 mg once daily is recommended for most patients. The placebo- controlled studies that demonstrated the efficacy of naltrexone hydrochloride as an adjunctive treatment of alcoholism used a dose regimen of naltrexone hydrochloride 50 mg once daily for up to 12 weeks. Other dose regimens or durations of therapy were not evaluated in these trials.
Naltrexone hydrochloride tablets should be considered as only one of many factors determining the success of treatment of alcoholism. Factors associated with a good outcome in the clinical trials with naltrexone hydrochloride tablets were the type, intensity, and duration of treatment; appropriate management of comorbid conditions; use of community-based support groups; and good medication compliance. To achieve the best possible treatment outcome, appropriate compliance-enhancing techniques should be implemented for all components of the treatment program, especially medication compliance.
Treatment of Opioid Dependence
Treatment should be initiated with an initial dose of 25 mg of naltrexone hydrochloride tablets. If no withdrawal signs occur, the patient may be started on 50 mg a day thereafter.
A dose of 50 mg once a day will produce adequate clinical blockade of the actions of parenterally administered opioids. As with many non-agonist treatments for addiction, naltrexone hydrochloride tablets are of proven value only when given as part of a comprehensive plan of management that includes some measure to ensure the patient takes the medication.
Naloxone Challenge Test
Clinicians are reminded that there is no completely reliable method for determining whether a patient has had an adequate opioid-free period. A naloxone challenge test may be helpful if there is any question of occult opioid dependence. If signs of opioid withdrawal are still observed following naloxone challenge, treatment with naltrexone hydrochloride tablets should not be attempted. The naloxone challenge can be repeated in 24 hours.
The naloxone challenge test should not be performed in a patient showing clinical signs or symptoms of opioid withdrawal, or in a patient whose urine contains opioids. The naloxone challenge test may be administered by either the intravenous or subcutaneous routes.
Intravenous
Inject 0.2 mg naloxone.
Observe for 20 minutes for signs or symptoms of withdrawal.
If no evidence of withdrawal, inject 0.6 mg of naloxone.
Observe for an additional 20 minutes.
Subcutaneous
Administer 0.8 mg naloxone.
Observe for 20 minutes for signs or symptoms of withdrawal.
Note: Individual patients, especially those with opioid dependence, may respond to lower doses of naloxone. In some cases, 0.1 mg IV naloxone has produced a diagnostic response.
Interpretation of the Challenge
Monitor vital signs and observe the patient for signs and symptoms of opioid withdrawal. These may include, but are not limited to: nausea, vomiting, dysphoria, yawning, sweating, tearing, rhinorrhea, stuffy nose, craving for opioids, poor appetite, abdominal cramps, sense of fear, skin erythema, disrupted sleep patterns, fidgeting, uneasiness, poor ability to focus, mental lapses, muscle aches or cramps, pupillary dilation, piloerection, fever, changes in blood pressure, pulse or temperature, anxiety, depression, irritability, backache, bone or joint pains, tremors, sensations of skin crawling or fasciculations. If signs or symptoms of withdrawal appear, the test is positive and no additional naloxone should be administered.
Warning: If the test is positive, do NOT initiate naltrexone therapy. Repeat the challenge in 24 hours. If the test is negative, naltrexone therapy may be started if no other contraindications are present. If there is any doubt about the result of the test, hold naltrexone hydrochloride tablets and repeat the challenge in 24 hours.
Alternative Dosing Schedules
A flexible approach to a dosing regimen may need to be employed in cases of supervised administration. Thus, patients may receive 50 mg of naltrexone hydrochloride every weekday with a 100 mg dose on Saturday, 100 mg every other day, or 150 mg every third day. The degree of blockade produced by naltrexone hydrochloride may be reduced by these extended dosing intervals.
There may be a higher risk of hepatocellular injury with single doses above 50 mg, and use of higher doses and extended dosing intervals should balance the possible risks against the probable benefits (seeWARNINGS).
Patient Compliance
Naltrexone hydrochloride tablets should be considered as only one of many factors determining the success of treatment. To achieve the best possible treatment outcome, appropriate compliance-enhancing techniques should be implemented for all components of the treatment program, including medication compliance.