Bupropion Hydrochloride
These highlights do not include all the information needed to use BUPROPION HYDROCHLORIDE EXTENDED-RELEASE TABLETS, safely and effectively. See full prescribing information for BUPROPION HYDROCHLORIDE EXTENDED-RELEASE TABLETS.BUPROPION hydrochloride extended-release tablets, for oral useInitial U.S. Approval: 1985
1af14d2e-c64d-44b7-a402-8869e8e30661
HUMAN PRESCRIPTION DRUG LABEL
Apr 19, 2023
Lupin Pharmaceuticals, Inc.
DUNS: 089153071
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Bupropion Hydrochloride
PRODUCT DETAILS
INGREDIENTS (16)
Bupropion Hydrochloride
PRODUCT DETAILS
INGREDIENTS (16)
Drug Labeling Information
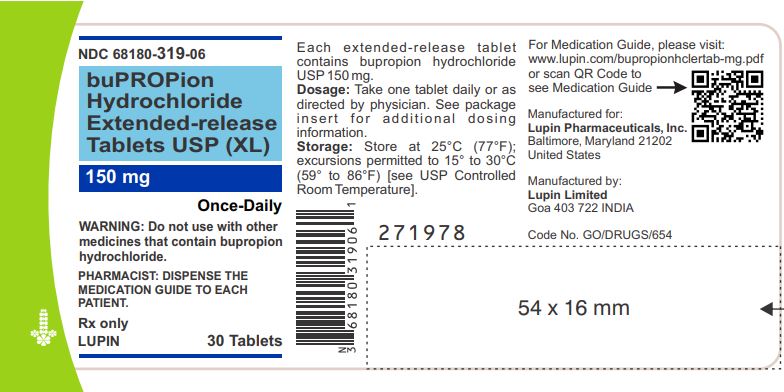
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
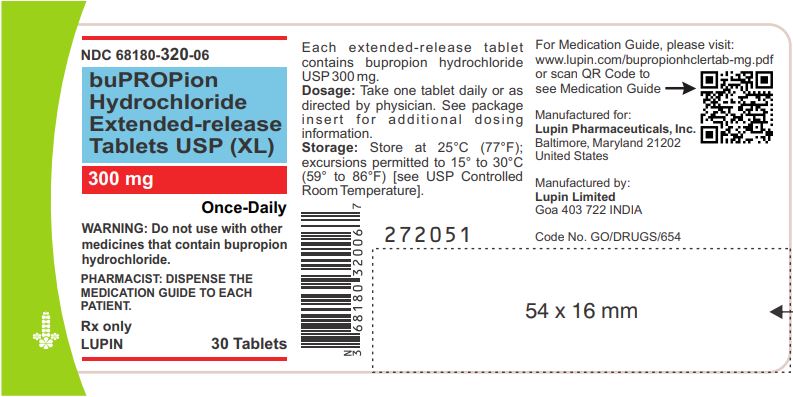
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 68180-319-06
Bupropion Hydrochloride Extended-release Tablets USP (XL)
150 mg
Rx only
Bottle of 30 Tablets
NDC 68180-320-06
Bupropion Hydrochloride Extended-release Tablets USP (XL)
300 mg
Rx only
Bottle of 30 Tablets
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients with seizure disorder.
- Bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients with seizure disorder.
- Bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients with a current or prior diagnosis of bulimia or anorexia nervosa as a higher incidence of seizures was observed in such patients treated with bupropion hydrochloride extended-release tablets (XL) [see WARNINGS AND PRECAUTIONS (5.3)].
- Bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients undergoing abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs [see WARNINGS AND PRECAUTIONS (5.3) and DRUG INTERACTIONS (7.3)].
- The use of MAOIs (intended to treat psychiatric disorders) concomitantly with bupropion hydrochloride extended-release tablets (XL) or within 14 days of discontinuing treatment with bupropion hydrochloride extended-release tablets (XL) are contraindicated. There is an increased risk of hypertensive reactions when bupropion hydrochloride extended-release tablets (XL) are used concomitantly with MAOIs. The use of bupropion hydrochloride extended-release tablets (XL) within 14 days of discontinuing treatment with an MAOI is also contraindicated. Starting bupropion hydrochloride extended-release tablets (XL) in a patient treated with reversible MAOIs such as linezolid or intravenous methylene blue is contraindicated [see DOSAGE AND ADMINISTRATION (2.9), WARNINGS AND PRECAUTIONS (5.4) and DRUG INTERACTIONS (7.6)].
- Bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients with known hypersensitivity to bupropion or other ingredients of bupropion hydrochloride extended-release tablets (XL). Anaphylactoid/anaphylactic reactions and Stevens-Johnson syndrome have been reported [see WARNINGS AND PRECAUTIONS (5.8)].
- Seizure disorder. (4,5.3)
- Current or prior diagnosis of bulimia or anorexia nervosa (4, 5.3)
- Abrupt discontinuation of alcohol, benzodiazepines, barbiturates, antiepileptic drugs. (4,5.3)
- Monoamine Oxidase Inhibitors (MAOIs): Do not use MAOIs intended to treat psychiatric disorders with bupropion hydrochloride extended-release tablets (XL) or within 14 days of stopping treatment with bupropion hydrochloride extended-release tablets (XL). Do not use bupropion hydrochloride extended-release tablets (XL) within 14 days of stopping an MAOI intended to treat psychiatric disorders. In addition, do not start bupropion hydrochloride extended-release tablets (XL) in a patient who is being treated with linezolid or intravenous methylene blue. (4,7.6)
- Known hypersensitivity to bupropion or other ingredients of bupropion hydrochloride extended-release tablets (XL) (4,5.8)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behaviors in Children, Adolescents, and Young
Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment.
Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (Selective Serotonin Reuptake Inhibitors [SSRIs] and others) show that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
Table 1: Risk Differences in the Number of Suicidality Cases by Age Group in the Pooled Placebo-Controlled Trials of Antidepressants in Pediatric and Adult Patients|
** A**** ge Range** |
** D**** rug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated** |
|
Increases Compared to Placebo | |
|
<18 years |
14 additional cases |
|
18 to 24 years |
5 additional cases |
|
Decreases Compared to Placebo | |
|
25 to 64 years |
1 fewer case |
|
≥65 years |
6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo- controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases**[seeBOXED WARNING and USE IN SPECIFIC POPULATIONS (8.4)].**
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for bupropion hydrochloride extended-release tablets (XL) should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
5.2 Neuropsychiatric Adverse Events and Suicide Risk in Smoking Cessation
Treatment
Bupropion hydrochloride extended-release tablets (XL) are not approved for smoking cessation treatment; however, bupropion HCl sustained-release is approved for this use. Serious neuropsychiatric adverse events have been reported in patients taking bupropion for smoking cessation. These postmarketing reports have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide [see ADVERSE REACTIONS (6.2)]. Some patients who stopped smoking may have been experiencing symptoms of nicotine withdrawal, including depressed mood. Depression, rarely including suicidal ideation, has been reported in smokers undergoing a smoking cessation attempt without medication. However, some of these adverse events occurred in patients taking bupropion who continued to smoke.
Neuropsychiatric adverse events occurred in patients without and with pre- existing psychiatric disease; some patients experienced worsening of their psychiatric illnesses. Observe patients for the occurrence of neuropsychiatric adverse events. Advise patients and caregivers that the patient should stop taking bupropion hydrochloride extended-release tablets (XL) and contact a healthcare provider immediately if agitation, depressed mood, or changes in behavior or thinking that are not typical for the patient are observed, or if the patient develops suicidal ideation or suicidal behavior. The healthcare provider should evaluate the severity of the adverse events and the extent to which the patient is benefiting from treatment, and consider options including continued treatment under closer monitoring, or discontinuing treatment. In many postmarketing cases, resolution of symptoms after discontinuation of bupropion was reported. However, the symptoms persisted in some cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve.
5.3 Seizure
Bupropion hydrochloride extended-release tablets (XL) can cause seizure. The risk of seizure is dose-related. The dose should not exceed 300 mg once daily. Increase the dose gradually. Discontinue bupropion hydrochloride extended- release tablets (XL) and do not restart treatment if the patient experiences a seizure.
The risk of seizures is also related to patient factors, clinical situations, and concomitant medications that lower the seizure threshold. Consider these risks before initiating treatment with bupropion hydrochloride extended- release tablets (XL). bupropion hydrochloride extended-release tablets (XL) are contraindicated in patients with a seizure disorder or conditions that increase the risk of seizure (e.g., severe head injury, arteriovenous malformation, CNS tumor or CNS infection, severe stroke, anorexia nervosa or bulimia, or abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs [see CONTRAINDICATIONS (4)]. The following conditions can also increase the risk of seizure: concomitant use of other medications that lower the seizure threshold (e.g., other bupropion products, antipsychotics, tricyclic antidepressants, theophylline, and systemic corticosteroids), metabolic disorders (e.g., hypoglycemia, hyponatremia, severe hepatic impairment, and hypoxia), or use of illicit drugs (e.g., cocaine) or abuse or misuse of prescription drugs such as CNS stimulants. Additional predisposing conditions include diabetes mellitus treated with oral hypoglycemic drugs or insulin, use of anorectic drugs, excessive use of alcohol, benzodiazepines, sedative/hypnotics, or opiates.
Incidence of Seizure with Bupropion Use
The incidence of seizure with bupropion hydrochloride extended-release tablets (XL) have not been formally evaluated in clinical trials. In studies using bupropion HCl sustained-release up to 300 mg per day the incidence of seizure was approximately 0.1% (1/1000 patients). In a large prospective, follow-up study, the seizure incidence was approximately 0.4% (13/3200) with bupropion HCl immediate-release in the range of 300 mg to 450 mg per day.
Additional data accumulated for bupropion immediate-release suggests that the estimated seizure incidence increases almost tenfold between 450 and 600 mg/day. The risk of seizure can be reduced if the bupropion hydrochloride extended-release tablets (XL) dose does not exceed 450 mg once daily and the titration rate is gradual.
5.4 Hypertension
Treatment with bupropion hydrochloride extended-release tablets (XL) can result in elevated blood pressure and hypertension. Assess blood pressure before initiating treatment with bupropion hydrochloride extended-release tablets (XL), and monitor periodically during treatment. The risk of hypertension is increased if bupropion hydrochloride extended-release tablets (XL) are used concomitantly with MAOIs or other drugs that increase dopaminergic or noradrenergic activity [see CONTRAINDICATIONS (4)].
Data from a comparative trial of the sustained-release formulation of bupropion HCl, nicotine transdermal system (NTS), the combination of sustained-release bupropion plus NTS, and placebo as an aid to smoking cessation suggest a higher incidence of treatment-emergent hypertension in patients treated with the combination of sustained-release bupropion and NTS. In this trial, 6.1% of subjects treated with the combination of sustained- release bupropion and NTS had treatment-emergent hypertension compared to 2.5%, 1.6%, and 3.1% of subjects treated with sustained-release bupropion, NTS, and placebo, respectively. The majority of these subjects had evidence of pre-existing hypertension. Three subjects (1.2%) treated with the combination of sustained-release bupropion and NTS and 1 subject (0.4%) treated with NTS had study medication discontinued due to hypertension compared with none of the subjects treated with sustained-release bupropion or placebo. Monitoring of blood pressure is recommended in patients who receive the combination of bupropion and nicotine replacement.
In the 3 trials of bupropion HCl extended-release in seasonal affective disorder, there were significant elevations in blood pressure. Hypertension was reported as an adverse reaction for 2% of the bupropion group (11/537) and none in the placebo group (0/511). In the SAD trials, 2 patients treated with bupropion discontinued from the study because they developed hypertension. None of the placebo group discontinued because of hypertension. The mean increase in systolic blood pressure was 1.3 mmHg in the bupropion group and 0.1 mmHg in the placebo group. The difference was statistically significant (p=0.013). The mean increase in diastolic blood pressure was 0.8 mmHg in the bupropion group and 0.1 mmHg in the placebo group. The difference was not statistically significant (p=0.075). In the SAD trials, 82% of patients were treated with 300 mg per day, and 18% were treated with 150 mg per day. The mean daily dose was 270 mg per day. The mean duration of bupropion exposure was 126 days.
In a clinical trial of bupropion immediate-release in MDD subjects with stable congestive heart failure (CHF) (N=36), bupropion was associated with an exacerbation of pre-existing hypertension in 2 subjects, leading to discontinuation of bupropion treatment. There are no controlled studies assessing the safety of bupropion in patients with a recent history of myocardial infarction or unstable cardiac disease.
5.5 Activation of Mania/Hypomania
Antidepressant treatment can precipitate a manic, mixed, or hypomanic manic episode. The risk appears to be increased in patients with bipolar disorder or who have risk factors for bipolar disorder. Prior to initiating bupropion hydrochloride extended-release tablets (XL), screen patients for a history of bipolar disorder and the presence of risk factors for bipolar disorder (e.g., family history of bipolar disorder, suicide, or depression). Bupropion hydrochloride extended-release tablets (XL) are not approved for the treatment of bipolar depression.
5.6 Psychosis and Other Neuropsychiatric Reactions
Depressed patients treated with bupropion have had a variety of neuropsychiatric signs and symptoms, including delusions, hallucinations, psychosis, concentration disturbance, paranoia, and confusion. Some of these patients had a diagnosis of bipolar disorder. In some cases, these symptoms abated upon dose reduction and/or withdrawal of treatment. Discontinue bupropion hydrochloride extended-release tablets (XL) if these reactions occur.
5.7 Angle-Closure Glaucoma
Angle-Closure Glaucoma: The pupillary dilation that occurs following use of many antidepressant drugs including bupropion hydrochloride extended-release tablets (XL) may trigger an angle-closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.8 Hypersensitivity Reactions
Anaphylactoid/anaphylactic reactions have occurred during clinical trials with bupropion. Reactions have been characterized by pruritus, urticaria, angioedema, and dyspnea, requiring medical treatment. In addition, there have been rare, spontaneous postmarketing reports of erythema multiforme, Stevens- Johnson syndrome, and anaphylactic shock associated with bupropion. Instruct patients to discontinue bupropion hydrochloride extended-release tablets (XL) and consult a healthcare provider if they develop an allergic or anaphylactoid/anaphylactic reaction (e.g., skin rash, pruritus, hives, chest pain, edema, and shortness of breath) during treatment.
There are reports of arthralgia, myalgia, fever with rash and other symptoms of serum sickness suggestive of delayed hypersensitivity.
- Neuropsychiatric Adverse Events During Smoking Cessation:
Postmarketing reports of serious or clinically significant neuropsychiatric adverse events have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe patients attempting to quit smoking with bupropion hydrochloride extended-release tablets (XL) for the occurrence of such symptoms and instruct them to discontinue bupropion hydrochloride extended-release tablets (XL) and contact a healthcare provider if they experience such adverse events. (5.2)
- Seizure Risk: The risk is dose-related. Can minimize risk by limiting daily dose to 450 mg and gradually increasing the dose. Discontinue if seizure occurs. (4,5.3, 7.3)
- Hypertension: Bupropion hydrochloride extended-release tablets (XL) can increase blood pressure. Monitor blood pressure before initiating treatment and periodically during treatment. (5.4)
- Activation of Mania/Hypomania: Screen patients for bipolar disorder and monitor for these symptoms. (5.5)
- Psychosis and Other Neuropsychiatric Reactions: Instruct patients to contact a healthcare professional if such reactions occur. (5.6)
- Angle-Closure Glaucoma: Angle-closure glaucoma has occurred in patients with untreated anatomically narrow angles treated with antidepressants. (5.7)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
• Suicidal thoughts and behaviors in children, adolescents, and young adults [see WARNINGS AND PRECAUTIONS (5.1)]
• Neuropsychiatric adverse events and suicide risk in smoking cessation treatment [see WARNINGS AND PRECAUTIONS (5.2)]
• Seizure [see WARNINGS AND PRECAUTIONS (5.3)]
• Hypertension [see WARNINGS AND PRECAUTIONS (5.4)]
• Activation of mania or hypomania [see WARNINGS AND PRECAUTIONS (5.5)]
• Psychosis and other neuropsychiatric events [see WARNINGS AND PRECAUTIONS (5.6)]
• Angle-Closure Glaucoma [see WARNINGS AND PRECAUTIONS (5.7)]
• Hypersensitivity reactions [see WARNINGS AND PRECAUTIONS (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Commonly Observed Adverse Reactions in Controlled Clinical Trials of Sustained-Release****Bupropion Hydrochloride
Adverse reactions that occurred in at least 5% of patients treated with bupropion HCl sustained- release (300 mg and 400 mg per day) and at a rate at least twice the placebo rate are listed below.
300 mg/day of bupropion HCl sustained-release: anorexia, dry mouth, rash, sweating, tinnitus, and tremor.
400 mg/day of bupropion HCl sustained-release: abdominal pain, agitation, anxiety, dizziness, dry mouth, insomnia, myalgia, nausea, palpitation, pharyngitis, sweating, tinnitus, and urinary frequency.
Bupropion hydrochloride extended-release tablets (XL) have been demonstrated to have similar bioavailability both to the immediate-release and sustained- release formulations of bupropion. The information included under this subsection and under subsection 6.2 is based primarily on data from controlled clinical trials with the sustained-release and extended-release formulations of bupropion hydrochloride.
Major Depressive Disorder
Adverse Reactions Leading to Discontinuation of Treatment with Bupropion HCl Immediate-Release, Bupropion HCl Sustained-Release, and Bupropion HCl Extended-release in Major Depressive Disorder Trials
In placebo-controlled clinical trials with bupropion HCl sustained-release, 4%, 9%, and 11% of the placebo, 300 mg/day and 400 mg/day groups, respectively, discontinued treatment because of adverse reactions. The specific adverse reactions leading to discontinuation in at least 1% of the 300 mg/day or 400 mg/day groups and at a rate at least twice the placebo rate are listed inTable 2.
Table 2: Treatment Discontinuation Due to Adverse Reactions in Placebo-ControlledTrials in MDD|
** A**** dverse Reaction Term** |
** Placebo** |
** Bup**** r**** opion HCl** |
** Bup**** r**** opion HCl** |
|
Rash |
0.0% |
2.4% |
0.9% |
|
Nausea |
0.3% |
0.8% |
1.8% |
|
Agitation |
0.3% |
0.3% |
1.8% |
|
Migraine |
0.3% |
0.0% |
1.8% |
In clinical trials with bupropion HCl immediate-release, 10% of patients and volunteers discontinued due to an adverse reaction. Reactions resulting in discontinuation (in addition to those listed above for the sustained-release formulation) included vomiting, seizures, and sleep disturbances.
Adverse Reactions Occurring at an Incidence of >1% in Patients Treated with Bupropion HCl Immediate-Release or Bupropion HCl Sustained-Release in MDD
Table 3 summarizes the adverse reactions that occurred in placebo- controlled trials in patients treated with bupropion HCl sustained-release 300 mg/day and 400 mg/day. These include reactions that occurred in either the 300 mg or 400 mg group at an incidence of 1% or more and were more frequent than in the placebo group.
Table 3: Adverse Reactions in Placebo-Controlled Trials in Patients with MDD
| |||
|
†Hyphen denotes adverse reactions occurring in greater than 0 but less than 0.5% of patients. | |||
|
** Body System/ Adverse Reaction** |
** Placebo** |
** Bupropion HCl** |
** Bupropion HCl** |
|
Body (General) |
23% |
26% |
25% |
|
Infection |
6% |
8% |
9% |
|
Abdominal pain |
2% |
3% |
9% |
|
Asthenia |
2% |
2% |
4% |
|
Chest pain |
1% |
3% |
4% |
|
Pain |
2% |
2% |
3% |
|
Fever |
‑ |
1% |
2% |
|
Cardiovascular |
2% |
2% |
6% |
|
Flushing |
|
1% |
4% |
|
Migraine |
1% |
1% |
4% |
|
Hot flashes |
1% |
1% |
3% |
|
Digestive |
7% |
17% |
24% |
|
Nausea |
8% |
13% |
18% |
|
Constipation |
7% |
10% |
5% |
|
Diarrhea |
6% |
5% |
7% |
|
Anorexia |
2% |
5% |
3% |
|
Vomiting |
2% |
4% |
2% |
|
Dysphagia |
0% |
0% |
2% |
|
Musculoskeletal | |||
|
Myalgia |
3% |
2% |
6% |
|
Arthralgia |
1% |
1% |
4% |
|
Arthritis |
0% |
0% |
2% |
|
Twitch |
‑ |
1% |
2% |
|
Nervous System |
6% |
11% |
16% |
|
Dizziness |
5% |
7% |
11% |
|
Agitation |
2% |
3% |
9% |
|
Anxiety |
3% |
5% |
6% |
|
Tremor |
1% |
6% |
3% |
|
Nervousness |
3% |
5% |
3% |
|
Somnolence |
2% |
2% |
3% |
|
Irritability |
2% |
3% |
2% |
|
Memory decreased |
1% |
|
3% |
|
Paresthesia |
1% |
1% |
2% |
|
Central nervous system stimulation |
1% |
2% |
1% |
|
Respiratory |
2% |
3% |
11% |
|
Sinusitis |
2% |
3% |
1% |
|
Increased cough |
1% |
1% |
2% |
|
Skin |
2% |
6% |
5% |
|
Rash |
1% |
5% |
4% |
|
Pruritus |
2% |
2% |
4% |
|
Urticaria |
0% |
2% |
1% |
|
Special Senses |
2% |
6% |
6% |
|
Taste perversion |
|
2% |
4% |
|
Blurred vision or diplopia |
2% |
3% |
2% |
|
Urogenital | |||
|
Urinary frequency |
2% |
2% |
5% |
|
Urinary urgency |
0% |
_ |
2% |
|
Vaginal hemorrhage* |
_ |
0% |
2% |
|
Urinary tract infection |
_† |
1% |
0% |
The following additional adverse reactions occurred in controlled trials of bupropion HCl immediate-release (300 to 600 mg per day) at an incidence of at least 1% more frequently than in the placebo group were: cardiac arrhythmia (5% vs. 4%), hypertension (4% vs. 2%), hypotension (3% vs. 2%), menstrual complaints (5% vs. 1%), akathisia (2% vs. 1%), impaired sleep quality (4% vs. 2%), sensory disturbance (4% vs. 3%), confusion (8% vs. 5%), decreased libido (3% vs. 2%), hostility (6% vs. 4%), auditory disturbance (5% vs. 3%), and gustatory disturbance (3% vs. 1%).
Seasonal Affective Disorder
In placebo-controlled clinical trials in SAD, 9% of patients treated with bupropion hydrochloride extended-release tablets (XL) and 5% of patients treated with placebo discontinued treatment because of adverse reactions. The adverse reactions leading to discontinuation in at least 1% of patients treated with bupropion and at a rate numerically greater than the placebo rate were insomnia (2% vs. <1%) and headache (1% vs. <1%).
Table 4 summarizes the adverse reactions that occurred in patients treated with bupropion hydrochloride extended-release tablets (XL) for up to approximately 6 months in 3 placebo-controlled trials. These include reactions that occurred at an incidence of 2% or more and were more frequent than in the placebo group.
Table 4: Adverse Reactions in Placebo-Controlled Trials in Patients with SAD|
** S**** ystem Organ Class/ Preferred Term** |
** P**** lacebo** |
** Bup**** r**** opion HCl** |
|
Gastrointestinal Disorder |
15% |
26% |
|
Nausea |
8% |
13% |
|
Constipation |
2% |
9% |
|
Flatulence |
3% |
6% |
|
Abdominal pain |
<1% |
2% |
|
Nervous System Disorders |
26% |
34% |
|
Dizziness |
5% |
6% |
|
Tremor |
<1% |
3% |
|
Infections and Infestations |
12% |
13% |
|
Upper respiratory tract infection |
8% |
9% |
|
Sinusitis |
4% |
5% |
|
Psychiatric Disorders |
13% |
20% |
|
Anxiety |
5% |
7% |
|
Abnormal dreams |
2% |
3% |
|
Agitation |
<1% |
2% |
|
Musculoskeletal and Connective |
2% |
3% |
|
Pain in extremity |
2% |
3% |
|
Respiratory, Thoracic, and |
3% |
4% |
|
General Disorders and Administration Site Conditions |
2% |
3% |
|
Skin and Subcutaneous Tissue |
2% |
3% |
|
Metabolism and Nutrition |
1% |
4% |
|
Reproductive System and Breast |
<1% |
2% |
|
Ear and Labyrinth Disorders |
<1% |
3% |
|
Vascular Disorders |
0% |
2% |
Changes in Body Weight
Table 5 presents the incidence of body weight changes (≥5 lbs) in the short-term MDD trials using bupropion HCl sustained-release. There was a dose- related decrease in body weight.
Table 5: Incidence of Weight Gain or Weight Loss (≥5 lbs) in MDD Trials Using Bupropion HCl Sustained-Release|
** Weight Change** |
** Bup**** r**** opion HCl** |
** Bup**** r**** opion HCl** |
** P**** lacebo** |
|
Gained >5 lbs |
3% |
2% |
4% |
|
Lost >5 lbs |
14% |
19% |
6% |
Table 6 presents the incidence of body weight changes (≥5 lbs) in the 3 SAD trials using bupropion HCl extended-release. A higher proportion of subjects in the bupropion group (23%) had a weight loss ≥5 lbs, compared to the placebo group (11%). These were relatively long-term trials (up to 6 months).
Table 6: Incidence of Weight Gain or Weight Loss (≥5 lbs) in SAD Trials Using Bupropion HCl Extended-release|
** Weight Change** |
** Bup**** r**** opion HCl Extended-release** |
** P**** lacebo** |
|
Gained >5 lbs |
11% |
21% |
|
Lost >5 lbs |
23% |
11% |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of bupropion hydrochloride extended-release tablets (XL). Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body (General)
Chills, facial edema, edema, peripheral edema, musculoskeletal chest pain, photosensitivity, and malaise.
Cardiovascular
Postural hypotension, hypertension, stroke, vasodilation, syncope, complete atrioventricular block, extrasystoles, myocardial infarction, phlebitis, and pulmonary embolism.
Digestive
Abnormal liver function, bruxism, gastric reflux, gingivitis, glossitis, increased salivation, jaundice, mouth ulcers, stomatitis, thirst, edema of tongue, colitis, esophagitis, gastrointestinal hemorrhage, gum hemorrhage, hepatitis, intestinal perforation, liver damage, pancreatitis, and stomach ulcer.
Endocrine
Hyperglycemia, hypoglycemia, and syndrome of inappropriate antidiuretic hormone secretion.
Hemic and Lymphatic
Ecchymosis, anemia, leukocytosis, leukopenia, lymphadenopathy, pancytopenia, and thrombocytopenia. Altered PT and/or INR, associated with hemorrhagic or thrombotic complications, were observed when bupropion was coadministered with warfarin.
Metabolic and Nutritional
Glycosuria.
Musculoskeletal
Leg cramps, fever/rhabdomyolysis, and muscle weakness.
Nervous System
Abnormal coordination, depersonalization, emotional lability, hyperkinesia, hypertonia, hypesthesia, vertigo, amnesia, ataxia, derealization, abnormal electroencephalogram (EEG), aggression, akinesia, aphasia, coma, dysarthria, dyskinesia, dystonia, euphoria, extrapyramidal syndrome, hypokinesia, increased libido, neuralgia, neuropathy, paranoid ideation, restlessness, suicide attempt, and unmasking tardive dyskinesia.
Respiratory
Bronchospasm and pneumonia.
Skin
Maculopapular rash, alopecia, angioedema, exfoliative dermatitis, and hirsutism, acute generalized exanthematous pustulosis.
Special Senses
Accommodation abnormality, dry eye, deafness, increased intraocular pressure, angle-closure glaucoma, and mydriasis.
Urogenital
Impotence, polyuria, prostate disorder, abnormal ejaculation, cystitis, dyspareunia, dysuria, gynecomastia, menopause, painful erection, salpingitis, urinary incontinence, urinary retention, and vaginitis.
Most common adverse reactions are (incidence ≥5%; ≥2× placebo rate): dry mouth, nausea, insomnia, dizziness, pharyngitis, abdominal pain, agitation, anxiety, tremor, palpitation, sweating, tinnitus, myalgia, anorexia, urinary frequency, rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Lupin Pharmaceuticals, Inc. at 1-800-399-2561 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch**.**
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect Bupropion Hydrochloride Extended-
release Tablets (XL)
Bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between bupropion hydrochloride extended-release tablets (XL) and drugs that are inhibitors or inducers of CYP2B6.
Inhibitors of CYP2B6
Ticlopidine and Clopidogrel: Concomitant treatment with these drugs can increase bupropion exposures but decrease hydroxybupropion exposure. Based on clinical response, dosage adjustment of bupropion hydrochloride extended- release tablets (XL) may be necessary when coadministered with CYP2B6 inhibitors (e.g., ticlopidine or clopidogrel) [see CLINICAL PHARMACOLOGY (12.3)].
Inducers of CYP2B6
Ritonavir, Lopinavir, and Efavirenz: Concomitant treatment with these drugs can decrease bupropion and hydroxybupropion exposure. Dosage increase of bupropion hydrochloride extended-release tablets (XL) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz but should not exceed the maximum recommended dose [see CLINICAL PHARMACOLOGY (12.3)].
Carbamazepine, Phenobarbital, Phenytoin: While not systemically studied, these drugs may induce metabolism of bupropion and may decrease bupropion exposure [see CLINICAL PHARMACOLOGY (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary to increase the dose of bupropion, but the maximum recommended dose should not be exceeded.
7.2 Potential for Bupropion Hydrochloride Extended-release Tablets XL to
Affect Other Drugs
Drugs Metabolized by CYP2D6
Bupropion and its metabolites (erythrohydrobupropion, threohydrobupropion, hydroxybupropion) are CYP2D6 inhibitors. Therefore, coadministration of bupropion hydrochloride extended-release tablets (XL) with drugs that are metabolized by CYP2D6 can increase the exposures of drugs that are substrates of CYP2D6. Such drugs include certain antidepressants (e.g., venlafaxine, nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, and sertraline), antipsychotics (e.g., haloperidol, risperidone, and thioridazine), beta-blockers (e.g., metoprolol), and Type 1C antiarrhythmics (e.g., propafenone, and flecainide). When used concomitantly with bupropion hydrochloride extended-release tablets (XL), it may be necessary to decrease the dose of these CYP2D6 substrates, particularly for drugs with a narrow therapeutic index.
Drugs that require metabolic activation by CYP2D6 to be effective (e.g., tamoxifen), theoretically could have reduced efficacy when administered concomitantly with inhibitors of CYP2D6 such as bupropion. Patients treated concomitantly with bupropion hydrochloride extended-release tablets (XL) and such drugs may require increased doses of the drug [see CLINICAL PHARMACOLOGY (12.3)].
7.3 Drugs That Lower Seizure Threshold
Use extreme caution when coadministering bupropion hydrochloride extended- release tablets (XL) with other drugs that lower the seizure threshold (e.g., other bupropion products, antipsychotics, antidepressants, theophylline, or systemic corticosteroids). Use low initial doses of bupropion hydrochloride extended-release tablets (XL) and increase the dose gradually [see WARNINGS AND PRECAUTIONS (5.3)].
7.4 Dopaminergic Drugs (Levodopa and Amantadine)
Bupropion, levodopa, and amantadine have dopamine agonist effects. CNS toxicity has been reported when bupropion was coadministered with levodopa or amantadine. Adverse reactions have included restlessness, agitation, tremor, ataxia, gait disturbance, vertigo, and dizziness. It is presumed that the toxicity results from cumulative dopamine agonist effects. Use caution when administering bupropion hydrochloride extended-release tablets (XL) concomitantly with these drugs.
7.5 Use with Alcohol
In postmarketing experience, there have been rare reports of adverse neuropsychiatric events or reduced alcohol tolerance in patients who were drinking alcohol during treatment with bupropion hydrochloride extended- release tablets (XL). The consumption of alcohol during treatment with bupropion hydrochloride extended-release tablets (XL) should be minimized or avoided.
7.6 MAO Inhibitors
Bupropion inhibits the reuptake of dopamine and norepinephrine. Concomitant use of MAOIs and bupropion is contraindicated because there is an increased risk of hypertensive reactions if bupropion is used concomitantly with MAOIs. Studies in animals demonstrate that the acute toxicity of bupropion is enhanced by the MAO inhibitor phenelzine. At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of treatment with bupropion hydrochloride extended-release tablets (XL). Conversely, at least 14 days should be allowed after stopping bupropion hydrochloride extended-release tablets (XL) before starting an MAOI antidepressant [see DOSAGE AND ADMINISTRATION (2.8, 2.9) and CONTRAINDICATIONS (4)].
7.7 Drug-Laboratory Test Interactions
False-positive urine immunoassay screening tests for amphetamines have been reported in patients taking bupropion. This is due to lack of specificity of some screening tests. False-positive test results may result even following discontinuation of bupropion therapy. Confirmatory tests, such as gas chromatography/mass spectrometry, will distinguish bupropion from amphetamines.
- CYP2B6 inducers: Dose increase may be necessary if coadministered with CYP2B6 inducers (e.g., ritonavir, lopinavir, efavirenz, carbamazepine, phenobarbital, and phenytoin) based on clinical exposure, but should not exceed the maximum recommended dose. (7.1)
- Drugs metabolized by CYP2D6: Bupropion inhibits CYP2D6 and can increase concentrations of: antidepressants (e.g., venlafaxine, nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, sertraline), antipsychotics (e.g., haloperidol, risperidone, thioridazine), beta-blockers (e.g., metoprolol), and Type 1C antiarrhythmics (e.g., propafenone, flecainide). Consider dose reduction when using with bupropion. (7.2)
- Drugs that lower seizure threshold: Dose bupropion hydrochloride extended-release tablets (XL) with caution. (5.3, 7.3)
- Dopaminergic Drugs (levodopa and amantadine): CNS toxicity can occur when used concomitantly with bupropion hydrochloride extended-release tablets (XL). (7.4)
- MAOIs: Increased risk of hypertensive reactions can occur when used concomitantly with bupropion hydrochloride extended-release tablets (XL). (7.6)
- Drug-laboratory test interactions: Bupropion hydrochloride extended-release tablets (XL) can cause false-positive urine test results for amphetamines. (7.7)
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Bupropion is not a controlled substance.
9.2 Abuse
Humans
Controlled clinical studies of bupropion HCl immediate-release conducted in normal volunteers, in subjects with a history of multiple drug abuse, and in depressed patients demonstrated an increase in motor activity and agitation/excitement.
In a population of individuals experienced with drugs of abuse, a single dose of 400 mg bupropion produced mild amphetamine-like activity as compared to placebo on the Morphine-Benzedrine Subscale of the Addiction Research Center Inventories (ARCI), and a score intermediate between placebo and amphetamine on the Liking Scale of the ARCI. These scales measure general feelings of euphoria and drug desirability.
Findings in clinical trials, however, are not known to reliably predict the abuse potential of drugs. Nonetheless, evidence from single-dose studies does suggest that the recommended daily dosage of bupropion when administered in divided doses is not likely to be significantly reinforcing to amphetamine or CNS stimulant abusers. However, higher doses (that could not be tested because of the risk of seizure) might be modestly attractive to those who abuse CNS stimulant drugs.
Bupropion hydrochloride extended-release tablets are intended for oral use only. The inhalation of crushed tablets or injection of dissolved bupropion has been reported. Seizures and/or cases of death have been reported when bupropion has been administered intranasally or by parenteral injection.
Animals
Studies in rodents and primates demonstrated that bupropion exhibits some pharmacologic actions common to psychostimulants. In rodents, it has been shown to increase locomotor activity, elicit a mild stereotyped behavioral response, and increase rates of responding in several schedule-controlled behavior paradigms. In primate models assessing the positive reinforcing effects of psychoactive drugs, bupropion was self-administered intravenously. In rats, bupropion produced amphetamine-like and cocaine-like discriminative stimulus effects in drug discrimination paradigms used to characterize the subjective effects of psychoactive drugs.
OVERDOSAGE SECTION
10 OVERDOSAGE
10.1 Human Overdose Experience
Overdoses of up to 30 grams or more of bupropion have been reported. Seizure was reported in approximately one third of all cases. Other serious reactions reported with overdoses of bupropion alone included hallucinations, loss of consciousness, sinus tachycardia, ECG changes such as conduction disturbances or arrhythmias, mental status changes,clonus, myoclonus, and hyperreflexia. Fever, muscle rigidity, rhabdomyolysis, hypotension, stupor, coma, and respiratory failure have been reported mainly when bupropion was part of multiple drug overdoses.
Although most patients recovered without sequelae, deaths associated with overdoses of bupropion alone have been reported in patients ingesting large doses of the drug. Multiple uncontrolled seizures, bradycardia, cardiac failure, and cardiac arrest prior to death were reported in these patients.
10.2 Overdosage Management
Consult a Certified Poison Control Center for up-to-date guidance and advice. Call 1-800-222-1222 or refer to www.poison.org.
There are no known antidotes for bupropion. In case of an overdose, provide supportive care, including close medical supervision and monitoring. Consider the possibility of multiple drug overdose.
DESCRIPTION SECTION
11 DESCRIPTION
Bupropion hydrochloride, an antidepressant of the aminoketone class, is chemically unrelated to tricyclic, tetracyclic, selective serotonin reuptake inhibitor, or other known antidepressant agents. Its structure closely resembles that of diethylpropion; it is related to phenylethylamines. It is designated as (±)-1-(3-chorophenyl)-2-[(1,1-dimethylethyl)amino]-1 propanone hydrochloride. The molecular weight is 276.21. The molecular formula is C13H18ClNO•HCl. Bupropion hydrochloride powder is white and soluble in water. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. The structural formula is:
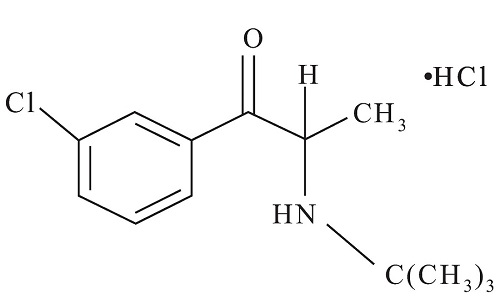
Bupropion hydrochloride extended-release tablet USP (XL) is supplied for oral administration as 150 mg and 300 mg, off-white to pale yellow extended-release tablets. Each tablet contains the labeled amount of bupropion hydrochloride and the inactive ingredients: ammonium hydroxide, colloidal silicon dioxide, dibutyl sebacate, ethylcellulose, glyceryl behenate, hydrophobic colloidal silica, hydroxypropyl cellulose, iron oxide black, L-cysteine hydrochloride monohydrate, methacrylic acid copolymer dispersion, polyvinyl alcohol, povidone, propylene glycol, shellac and triethyl citrate. The tablets are printed with edible black ink.
The insoluble shell of the extended-release tablet may remain intact during gastrointestinal transit and is eliminated in the feces.
The Drug Product Meets USP Dissolution Test 20.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime carcinogenicity studies were performed in rats and mice at doses up to 300 and 150 mg/kg/day bupropion hydrochloride, respectively. These doses are approximately 7 and 2 times the maximum recommended human dose (MRHD), respectively, on a mg/m2 basis. In the rat study there was an increase in nodular proliferative lesions of the liver at doses of 100 to 300 mg/kg/day of bupropion hydrochloride (approximately 2 to 7 times the MRHD on a mg/m2 basis); lower doses were not tested. The question of whether or not such lesions may be precursors of neoplasms of the liver is currently unresolved. Similar liver lesions were not seen in the mouse study, and no increase in malignant tumors of the liver and other organs was seen in either study.
Bupropion produced a positive response (2 to 3 times control mutation rate) in 2 of 5 strains in one Ames bacterial mutagenicity assay, but was negative in another. Bupropion produced an increase in chromosomal aberrations in 1 of 3 in vivo rat bone marrow cytogenetic studies.
A fertility study in rats at doses up to 300 mg/kg/day revealed no evidence of impaired fertility.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Major Depressive Disorder
The efficacy of bupropion in the treatment of major depressive disorder was established with the immediate-release formulation of bupropion hydrochloride in two 4-week, placebo-controlled trials in adult inpatients with MDD and in one 6-week, placebo-controlled trial in adult outpatients with MDD. In the first study, the bupropion dose range was 300 mg to 600 mg per day administered in 3 divided doses; 78% of patients were treated with doses of 300 mg to 450 mg per day. The trial demonstrated the efficacy of bupropion as measured by the Hamilton Depression Rating Scale (HAMD) total score, the HAMD depressed mood item (item 1), and the Clinical Global Impressions-Severity Scale (CGI-S). The second study included 2 fixed doses of bupropion (300 mg and 450 mg per day) and placebo. This trial demonstrated the efficacy of bupropion for only the 450 mg dose. The efficacy results were significant for the HAMD total score and the CGI-S severity score, but not for HAMD item 1. In the third study, outpatients were treated with bupropion 300 mg per day. This study demonstrated the efficacy of bupropion as measured by the HAMD total score, the HAMD item 1, the Montgomery-Asberg Depression Rating Scale (MADRS), the CGI-S score, and the CGI-Improvement Scale (CGI-I) score.
A longer-term, placebo-controlled, randomized withdrawal trial demonstrated the efficacy of bupropion HCl sustained-release in the maintenance treatment of MDD. The trial included adult outpatients meeting DSM-IV criteria for MDD, recurrent type, who had responded during an 8-week open-label trial of bupropion 300 mg per day. Responders were randomized to continuation of bupropion 300 mg per day or placebo for up to 44 weeks of observation for relapse. Response during the open-label phase was defined as a CGI-Improvement Scale score of 1 (very much improved) or 2 (much improved) for each of the final 3 weeks. Relapse during the double-blind phase was defined as the investigator's judgment that drug treatment was needed for worsening depressive symptoms. Patients in the bupropion group experienced significantly lower relapse rates over the subsequent 44 weeks compared to those in the placebo group.
Although there are no independent trials demonstrating the efficacy of bupropion hydrochloride extended-release tablets (XL) in the acute treatment of MDD, studies have demonstrated similar bioavailability between the immediate-, sustained-, and extended-release formulations of bupropion HCl under steady-state conditions (i.e., the exposures [Cmax and AUC] for bupropion and its metabolites are similar among the 3 formulations).
14.2 Seasonal Affective Disorder
The efficacy of bupropion hydrochloride extended-release tablets (XL) in the prevention of seasonal major depressive episodes associated with SAD was established in 3 randomized, double-blind, placebo-controlled trials in adult outpatients with a history of MDD with an autumn-winter seasonal pattern (as defined by DSM-IV criteria). Bupropion treatment was initiated prior to the onset of symptoms in the autumn (September to November). Treatment was discontinued following a 2 week taper that began during the first week of spring (fourth week of March), resulting in a treatment duration of approximately 4 to 6 months for the majority of patients. Patients were randomized to treatment with bupropion hydrochloride extended-release tablets (XL) or placebo. The initial bupropion dose was 150 mg once daily for 1 week, followed by up-titration to 300 mg once daily. Patients who were deemed by the investigator to be unlikely or unable to tolerate 300 mg once daily were allowed to remain on, or had their dose reduced to, 150 mg once daily. The mean bupropion doses in the 3 trials ranged from 257 mg to 280 mg per day. Approximately 59% of patients continued in the study for 3 to 6 months; 26% continued for <3 months, 15% continued for >6 months.
To enter the trials, patients must have had a low level of depressive symptoms, as demonstrated by a score of <7 on the Hamilton Depression Rating Scale-17 (HAMD17) and a HAMD24 score of <14. The primary efficacy measure was the Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders (SIGH-SAD), which is identical to the HAMD24. The SIGH-SAD consists of the HAMD17 plus 7 items specifically assessing core symptoms of seasonal affective disorder: social withdrawal, weight gain, increased appetite, increased eating, carbohydrate craving, hypersomnia, and fatigability. The primary efficacy endpoint was the onset of a seasonal major depressive episode. The criteria for defining an episode included: 1) the investigator's judgment that a major depressive episode had occurred or that the patient required intervention for depressive symptoms, or 2) a SIGH-SAD score of >20 on 2 consecutive weeks. The primary analysis was a comparison of depression-free rates between the bupropion and placebo groups.
In these 3 trials, the percentage of patients who were depression-free (did not have an episode of MDD) at the end of treatment was significantly higher in the bupropion group than in the placebo group: 81.4% vs. 69.7%, 87.2% vs. 78.7%, and 84.0% vs. 69.0% for Trials 1, 2 and 3, respectively. For the 3 trials combined, the depression-free rate was 84.3% versus 72.0% in the bupropion and placebo group, respectively.
