Paliperidone
These highlights do not include all the information needed to use PALIPERIDONE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for PALIPERIDONE EXTENDED-RELEASE TABLETS. PALIPERIDONE extended-release tablets, for oral use Initial U.S. Approval: 2006
ebe3d5b9-4ea7-4840-b8cb-c4c1627e82d9
HUMAN PRESCRIPTION DRUG LABEL
Apr 2, 2024
REMEDYREPACK INC.
DUNS: 829572556
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
paliperidone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (16)
Drug Labeling Information
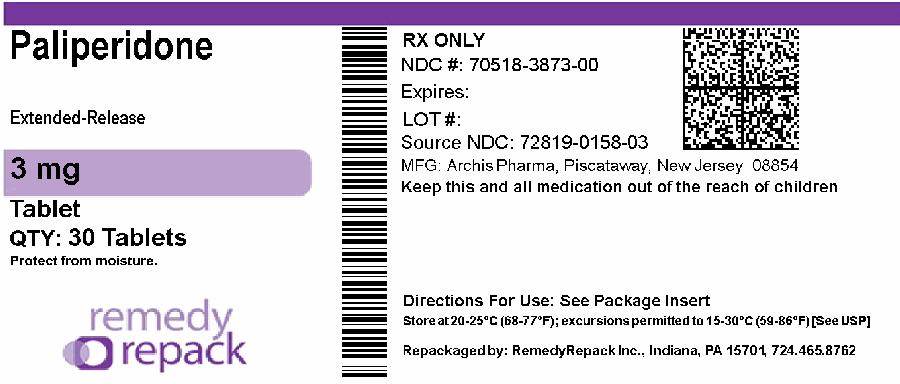
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
DRUG: Paliperidone
GENERIC: paliperidone
DOSAGE: TABLET, FILM COATED, EXTENDED RELEASE
ADMINSTRATION: ORAL
NDC: 70518-3873-0
COLOR: white
SHAPE: ROUND
SCORE: No score
SIZE: 8 mm
IMPRINT: M;PD3
PACKAGING: 30 in 1 BLISTER PACK
ACTIVE INGREDIENT(S):
- PALIPERIDONE 3mg in 1
INACTIVE INGREDIENT(S):
- BUTYLATED HYDROXYTOLUENE
- CELLULOSE ACETATE
- SILICON DIOXIDE
- HYDROXYPROPYL CELLULOSE, UNSPECIFIED
- HYPROMELLOSE, UNSPECIFIED
- POLYETHYLENE GLYCOL, UNSPECIFIED
- POLYETHYLENE OXIDE 200000
- POLYETHYLENE OXIDE 5000000
- FERRIC OXIDE RED
- SODIUM CHLORIDE
- SODIUM STEARYL FUMARATE
- TALC
- TITANIUM DIOXIDE
- FERRIC OXIDE YELLOW
- POLYVINYL ALCOHOL, UNSPECIFIED
BOXED WARNING SECTION
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED
PSYCHOSIS
See full prescribing information for complete boxed warning.
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Paliperidone extended-release tablets are not approved for use in patients with dementia-related psychosis. ( 5.1)
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Schizophrenia
Paliperidone extended-release tablets are indicated for the treatment of schizophrenia [see Clinical Studies (14.1)] .
The efficacy of paliperidone extended-release tablets in schizophrenia was established in three 6-week trials in adults and one 6-week trial in adolescents, as well as one maintenance trial in adults.
1.2 Schizoaffective Disorder
Paliperidone extended-release tablets are indicated for the treatment of schizoaffective disorder as monotherapy and an adjunct to mood stabilizers and/or antidepressant therapy [see Clinical Studies (14.2)] .
The efficacy of paliperidone extended-release tablets in schizoaffective disorder was established in two 6-week trials in adults.
Paliperidone extended-release tablets are an atypical antipsychotic agent indicated for
Treatment of schizophrenia ( 1.1)
- Adults: Efficacy was established in three 6-week trials and one maintenance trial. ( 14.1)
- Adolescents (ages 12-17): Efficacy was established in one 6-week trial. ( 14.1)
Treatment of schizoaffective disorder as monotherapy and as an adjunct to mood stabilizers and/or antidepressants. ( 1.2)
- Efficacy was established in two 6-week trials in adult patients. ( 14.2)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Paliperidone extended-release tablets are contraindicated in patients with a known hypersensitivity to either paliperidone or risperidone, or to any of the excipients in the paliperidone extended-release tablets formulation. Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been reported in patients treated with risperidone and in patients treated with paliperidone. Paliperidone is a metabolite of risperidone.
Known hypersensitivity to paliperidone, risperidone, or to any excipients in paliperidone extended-release tablets. ( 4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Increased mortality in elderly patients with dementia-related psychosis [see Boxed Warningand Warnings and Precautions (5.1)]
- Cerebrovascular adverse reactions, including stroke, in elderly patients with dementia-related psychosis [see Warnings and Precautions (5.2)]
- Neuroleptic malignant syndrome [see Warnings and Precautions (5.3)]
- QT prolongation [see Warnings and Precautions (5.4)]
- Tardive dyskinesia [see Warnings and Precautions (5.5)]
- Metabolic changes [see Warnings and Precautions (5.6)]
- Hyperprolactinemia [see Warnings and Precautions (5.7)]
- Potential for gastrointestinal obstruction [see Warnings and Precautions (5.8)]
- Orthostatic hypotension and syncope [see Warnings and Precautions (5.9)]
- Falls [see Warnings and Precautions (5.10)]
- Leukopenia, neutropenia, and agranulocytosis [see Warnings and Precautions (5.11)]
- Potential for cognitive and motor impairment [see Warnings and Precautions (5.12)]
- Seizures [see Warnings and Precautions (5.13)]
- Dysphagia [see Warnings and Precautions (5.14)]
- Priapism [see Warnings and Precautions (5.15)]
- Disruption of body temperature regulation [see Warnings and Precautions (5.16)]
6.1 Clincal Trails Experience
The most common adverse reactions in clinical trials in adult subjects with schizophrenia (reported in 5% or more of subjects treated with paliperidone extended-release tablets and at least twice the placebo rate in any of the dose groups) were extrapyramidal symptoms, tachycardia, and akathisia. The most common adverse reactions in clinical trials in adult patients with schizoaffective disorder (reported in 5% or more of subjects treated with paliperidone extended-release tablets and at least twice the placebo rate) were extrapyramidal symptoms, somnolence, dyspepsia, constipation, weight increased, and nasopharyngitis.
The most common adverse reactions that were associated with discontinuation from clinical trials in adult subjects with schizophrenia (causing discontinuation in 2% of paliperidone extended-release tablets-treated subjects) were nervous system disorders. The most common adverse reactions that were associated with discontinuation from clinical trials in adult subjects with schizoaffective disorder were gastrointestinal disorders, which resulted in discontinuation in 1% of paliperidone extended-release tablets- treated subjects [see Adverse Reactions (6)].
The safety of paliperidone extended-release tablets was evaluated in 1205 adult subjects with schizophrenia who participated in three placebo- controlled, 6-week, double-blind trials, of whom 850 subjects received paliperidone extended-release tablets at fixed doses ranging from 3 mg to 12 mg once daily. The information presented in this section was derived from pooled data from these three trials. Additional safety information from the placebo-controlled phase of the long-term maintenance study, in which subjects received paliperidone extended-release tablets at daily doses within the range of 3 mg to 15 mg (n = 104), is also included.
The safety of paliperidone extended-release tablets was evaluated in 150 adolescent subjects 12-17 years of age with schizophrenia who received paliperidone extended-release tablets in the dose range of 1.5 mg to 12 mg/day in a 6-week, double-blind, placebo-controlled trial.
The safety of paliperidone extended-release tablets was also evaluated in 622 adult subjects with schizoaffective disorder who participated in two placebo- controlled, 6-week, double-blind trials. In one of these trials, 206 subjects were assigned to one of two dose levels of paliperidone extended-release tablets: 6 mg with the option to reduce to 3 mg (n = 108) or 12 mg with the option to reduce to 9 mg (n = 98) once daily. In the other study, 214 subjects received flexible doses of paliperidone extended-release tablets (3-12 mg once daily). Both studies included subjects who received paliperidone extended- release tablets either as monotherapy or as an adjunct to mood stabilizers and/or antidepressants. Adverse events during exposure to study treatment were obtained by general inquiry and recorded by clinical investigators using their own terminology. Consequently, to provide a meaningful estimate of the proportion of individuals experiencing adverse events, events were grouped in standardized categories using MedDRA terminology.
Throughout this section, adverse reactions are reported. Adverse reactions are adverse events that were considered to be reasonably associated with the use of paliperidone extended-release tablets (adverse drug reactions) based on the comprehensive assessment of the available adverse event information. A causal association for paliperidone extended-release tablets often cannot be reliably established in individual cases. Further, because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials – Schizophrenia in Adults and Adolescents.
Adult Patients with Schizophrenia
Table 4 enumerates the pooled incidences of adverse reactions reported in the three placebo-controlled, 6-week, fixed-dose studies in adults, listing those that occurred in 2% or more of subjects treated with paliperidone extended- release tablets in any of the dose groups, and for which the incidence in paliperidone extended-release tablets-treated subjects in any of the dose groups was greater than the incidence in subjects treated with placebo.
Table 4. Adverse Reactions Reported by ≥ 2% of Paliperidone Extended- Release Tablets-Treated Adult Subjects with Schizophrenia in Three Short-Term, Fixed-Dose, Placebo-Controlled Clinical Trials *
| |||||
|
Percentage of Patients | |||||
|
Paliperidone Extended-Release Tablets | |||||
|
Placebo |
3 mg |
6 mg |
9 mg |
12 mg | |
|
Body System or Organ Class |
(N = 355) |
(N = 127) |
(N = 235) |
(N = 246) |
(N = 242) |
|
Dictionary-Derived Term | |||||
|
Total percentage of subjects with adverse reactions |
37 |
48 |
47 |
53 |
59 |
|
Cardiac disorders | |||||
|
Atrioventricular block first degree |
1 |
2 |
0 |
2 |
1 |
|
Bundle branch block |
2 |
3 |
1 |
3 |
< 1 |
|
Sinus arrhythmia |
0 |
2 |
1 |
1 |
< 1 |
|
Tachycardia |
7 |
14 |
12 |
12 |
14 |
|
Gastrointestinal disorders | |||||
|
Abdominal pain upper |
1 |
1 |
3 |
2 |
2 |
|
Dry mouth |
1 |
2 |
3 |
1 |
3 |
|
Salivary hypersecretion |
< 1 |
0 |
< 1 |
1 |
4 |
|
General disorders | |||||
|
Asthenia |
1 |
2 |
< 1 |
2 |
2 |
|
Fatigue |
1 |
2 |
1 |
2 |
2 |
|
Nervous system disorders | |||||
|
Akathisia |
4 |
4 |
3 |
8 |
10 |
|
Dizziness |
4 |
6 |
5 |
4 |
5 |
|
Extrapyramidal symptoms |
8 |
10 |
7 |
20 |
18 |
|
Headache |
12 |
11 |
12 |
14 |
14 |
|
Somnolence |
7 |
6 |
9 |
10 |
11 |
|
Vascular disorders | |||||
|
Orthostatic hypotension |
1 |
2 |
1 |
2 |
4 |
Adolescent Patients with Schizophrenia
Table 5 lists the adverse reactions reported in a fixed-dose, placebo- controlled study in adolescent subjects 12-17 years of age with schizophrenia, listing those that occurred in 2% or more of subjects treated with paliperidone extended-release tablets in any of the dose groups, and for which the incidence in paliperidone extended-release tablets-treated subjects in any of the dose groups was greater than the incidence in subjects treated with placebo.
Table 5. Adverse Reactions Reported by ≥ 2% of Paliperidone Extended- Release Tablets-Treated Adolescent Subjects with Schizophrenia in a Fixed- Dose, Placebo-Controlled Clinical Trial *
| |||||
|
Percentage of Patients | |||||
|
Paliperidone Extended-Release Tablets | |||||
|
Placebo |
1.5 mg |
3 mg |
6 mg |
12 mg | |
|
Body System or Organ Class |
(N = 51) |
(N = 54) |
(N = 16) |
(N = 45) |
(N = 35) |
|
Dictionary-Derived Term | |||||
|
Total percentage of subjects with adverse reactions |
43 |
37 |
50 |
58 |
74 |
|
Cardiac disorders | |||||
|
Tachycardia |
0 |
0 |
6 |
9 |
6 |
|
Eye disorders | |||||
|
Vision blurred |
0 |
0 |
0 |
0 |
3 |
|
Gastrointestinal disorders | |||||
|
Dry mouth |
2 |
0 |
0 |
0 |
3 |
|
Salivary hypersecretion |
0 |
2 |
6 |
2 |
0 |
|
Swollen tongue |
0 |
0 |
0 |
0 |
3 |
|
Vomiting |
10 |
0 |
6 |
11 |
3 |
|
General disorders | |||||
|
Asthenia |
0 |
0 |
0 |
2 |
3 |
|
Fatigue |
0 |
4 |
0 |
2 |
3 |
|
Infections and infestations | |||||
|
Nasopharyngitis |
2 |
4 |
0 |
4 |
0 |
|
Investigations | |||||
|
Weight increased |
0 |
7 |
6 |
2 |
3 |
|
Nervous system disorders | |||||
|
Akathisia |
0 |
4 |
6 |
11 |
17 |
|
Dizziness |
0 |
2 |
6 |
2 |
3 |
|
Extrapyramidal symptoms |
0 |
4 |
19 |
18 |
23 |
|
Headache |
4 |
9 |
6 |
4 |
14 |
|
Lethargy |
0 |
0 |
0 |
0 |
3 |
|
Somnolence |
4 |
9 |
13 |
20 |
26 |
|
Tongue paralysis |
0 |
0 |
0 |
0 |
3 |
|
Psychiatric disorders | |||||
|
Anxiety |
4 |
0 |
0 |
2 |
9 |
|
Reproductive system and breast disorders | |||||
|
Amenorrhea |
0 |
0 |
6 |
0 |
0 |
|
Galactorrhea |
0 |
0 |
0 |
4 |
0 |
|
Gynecomastia |
0 |
0 |
0 |
0 |
3 |
|
Respiratory, thoracic and mediastinal disorders | |||||
|
Epistaxis |
0 |
0 |
0 |
2 |
0 |
Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials – Schizoaffective Disorder in Adults
Table 6 enumerates the pooled incidences of adverse reactions reported in the two placebo-controlled 6-week studies in adult subjects, listing those that occurred in 2% or more of subjects treated with paliperidone extended-release tablets and for which the incidence in paliperidone extended-release tablets- treated subjects was greater than the incidence in subjects treated with placebo.
Table 6. Adverse Drug Reactions Reported by ≥ 2% of Paliperidone Extended-Release Tablets-Treated Adult Subjects with Schizoaffective Disorder in Two Double-Blind, Placebo-Controlled Clinical Trials *
| ||||
|
Percentage of Patients | ||||
|
Placebo |
Paliperidone Extended-Release Tablets |
Paliperidone Extended-Release Tablets |
Paliperidone Extended-Release Tablets | |
|
3-6 mg |
9-12 mg |
3-12 mg | ||
|
once daily |
once daily |
once daily | ||
|
fixed-dose range |
fixed-dose range |
flexible dose | ||
|
Body System or Organ Class |
(N = 202) |
(N = 108) |
(N = 98) |
(N = 214) |
|
Dictionary-Derived Term | ||||
|
Total percentage of subjects with adverse reactions |
32 |
48 |
50 |
43 |
|
Cardiac disorders | ||||
|
Tachycardia |
2 |
3 |
1 |
2 |
|
Gastrointestinal disorders | ||||
|
Abdominal discomfort/Abdominal pain upper |
1 |
1 |
0 |
3 |
|
Constipation |
2 |
4 |
5 |
4 |
|
Dyspepsia |
2 |
5 |
6 |
6 |
|
Nausea |
6 |
8 |
8 |
5 |
|
Stomach discomfort |
1 |
0 |
1 |
2 |
|
General disorders | ||||
|
Asthenia |
1 |
3 |
4 |
< 1 |
|
Infections and Infestations | ||||
|
Nasopharyngitis |
1 |
2 |
5 |
3 |
|
Rhinitis |
0 |
1 |
3 |
1 |
|
Upper respiratory tract infection |
1 |
2 |
2 |
2 |
|
Investigations | ||||
|
Weight increased |
1 |
5 |
4 |
4 |
|
Metabolism and nutrition disorders | ||||
|
Decreased appetite |
< 1 |
1 |
0 |
2 |
|
Increased appetite |
< 1 |
3 |
2 |
2 |
|
Musculoskeletal and connective tissue disorders | ||||
|
Back pain |
1 |
1 |
1 |
3 |
|
Myalgia |
< 1 |
2 |
4 |
1 |
|
Nervous system disorders | ||||
|
Akathisia |
4 |
4 |
6 |
6 |
|
Dysarthria |
0 |
1 |
4 |
2 |
|
Extrapyramidal symptoms |
8 |
20 |
17 |
12 |
|
Somnolence |
5 |
12 |
12 |
8 |
|
Psychiatric disorders | ||||
|
Sleep disorder |
< 1 |
2 |
3 |
0 |
|
Respiratory, thoracic and mediastinal disorders | ||||
|
Cough |
1 |
1 |
3 |
1 |
|
Pharyngolaryngeal pain |
< 1 |
0 |
2 |
1 |
Monotherapy versus Adjunctive Therapy
The designs of the two placebo-controlled, 6-week, double-blind trials in adult subjects with schizoaffective disorder included the option for subjects to receive antidepressants (except monoamine oxidase inhibitors) and/or mood stabilizers (lithium, valproate, or lamotrigine). In the subject population evaluated for safety, 230 (55%) subjects received paliperidone extended- release tablets as monotherapy and 190 (45%) subjects received paliperidone extended-release tablets as an adjunct to mood stabilizers and/or antidepressants. When comparing these 2 subpopulations, only nausea occurred at a greater frequency (≥ 3% difference) in subjects receiving paliperidone extended-release tablets as monotherapy.
Discontinuations Due to Adverse Reactions
Schizophrenia Trials
The percentages of subjects who discontinued due to adverse reactions in the three schizophrenia placebo-controlled, 6-week, fixed-dose studies in adults were 3% and 1% in paliperidone extended-release tablets- and placebo-treated subjects, respectively. The most common reasons for discontinuation were nervous system disorders (2% and 0% in paliperidone extended-release tablets- and placebo-treated subjects, respectively).
Among the adverse reactions in the 6-week, fixed-dose, placebo-controlled study in adolescents with schizophrenia, only dystonia led to discontinuation (< 1% of paliperidone extended-release tablets-treated subjects).
Schizoaffective Disorder Trials
The percentages of subjects who discontinued due to adverse reactions in the two schizoaffective disorder placebo-controlled 6-week studies in adults were 1% and < 1% in paliperidone extended-release tablets- and placebo-treated subjects, respectively. The most common reasons for discontinuation were gastrointestinal disorders (1% and 0% in paliperidone extended-release tablets- and placebo-treated subjects, respectively).
Dose-Related Adverse Reactions
Schizophrenia Trials
Based on the pooled data from the three placebo-controlled, 6-week, fixed-dose studies in adult subjects with schizophrenia, among the adverse reactions that occurred with a greater than 2% incidence in the subjects treated with paliperidone extended-release tablets, the incidences of the following adverse reactions increased with dose: somnolence, orthostatic hypotension, akathisia, dystonia, extrapyramidal disorder, hypertonia, parkinsonism, and salivary hypersecretion. For most of these, the increased incidence was seen primarily at the 12 mg dose, and, in some cases, the 9 mg dose.
In the 6-week, fixed-dose, placebo-controlled study in adolescents with schizophrenia, among the adverse reactions that occurred with > 2% incidence in the subjects treated with paliperidone extended-release tablets, the incidences of the following adverse reactions increased with dose: tachycardia, akathisia, extrapyramidal symptoms, somnolence, and headache.
Schizoaffective Disorder Trials
In a placebo-controlled, 6-week, high- and low-dose study in adult subjects with schizoaffective disorder, akathisia, dystonia, dysarthria, myalgia, nasopharyngitis, rhinitis, cough, and pharyngolaryngeal pain occurred more frequently (i.e., a difference of at least 2%) in subjects who received higher doses of paliperidone extended-release tablets compared with subjects who received lower doses.
Demographic Differences
An examination of population subgroups in the three placebo-controlled, 6-week, fixed-dose studies in adult subjects with schizophrenia and in the two placebo-controlled, 6-week studies in adult subjects with schizoaffective disorder did not reveal any evidence of clinically relevant differences in safety on the basis of gender or race alone; there was also no difference on the basis of age [see Use in Specific Populations (8.5)] .
Extrapyramidal Symptoms (EPS)
Pooled data from the three placebo-controlled, 6-week, fixed-dose studies in adult subjects with schizophrenia provided information regarding treatment- emergent EPS. Several methods were used to measure EPS: (1) the Simpson-Angus global score (mean change from baseline) which broadly evaluates Parkinsonism, (2) the Barnes Akathisia Rating Scale global clinical rating score (mean change from baseline) which evaluates akathisia, (3) use of anticholinergic medications to treat emergent EPS (Table 7), and (4) incidence of spontaneous reports of EPS (Table 8). For the Simpson-Angus Scale, spontaneous EPS reports and use of anticholinergic medications, there was a dose-related increase observed for the 9 mg and 12 mg doses. There was no difference observed between placebo and paliperidone extended-release tablets 3 mg and 6 mg doses for any of these EPS measures.
Table 7. Treatment-Emergent Extrapyramidal Symptoms (EPS) Assessed by Incidence of Ratings Scales and Use of Anticholinergic Medication Schizophrenia Studies in Adults
| |||||
|
Percentage of Patients | |||||
|
Paliperidone Extended-Release Tablets | |||||
|
Placebo |
3 mg |
6 mg |
9 mg |
12 mg | |
|
once daily |
once daily |
once daily |
once daily | ||
|
EPS Group |
(N = 355) |
(N = 127) |
(N = 235) |
(N = 246) |
(N = 242) |
|
Parkinsonism * |
9 |
11 |
3 |
15 |
14 |
|
Akathisia † |
6 |
6 |
4 |
7 |
9 |
|
Use of anticholinergic medications ‡ |
10 |
10 |
9 |
22 |
22 |
|
Dyskinesia group includes: Dyskinesia, extrapyramidal disorder, muscle
twitching, tardive dyskinesia | |||||
|
Percentage of Patients | |||||
|
Paliperidone Extended-Release Tablets | |||||
|
Placebo |
3 mg |
6 mg |
9 mg |
12 mg | |
|
once daily |
once daily |
once daily |
once daily | ||
|
EPS Group |
(N = 355) |
(N = 127) |
(N = 235) |
(N = 246) |
(N = 242) |
|
Overall percentage of patients with EPS-related AE |
11 |
13 |
10 |
25 |
26 |
|
Dyskinesia |
3 |
5 |
3 |
8 |
9 |
|
Dystonia |
1 |
1 |
1 |
5 |
5 |
|
Hyperkinesia |
4 |
4 |
3 |
8 |
10 |
|
Parkinsonism |
2 |
3 |
3 |
7 |
6 |
|
Tremor |
3 |
3 |
3 |
4 |
3 |
Compared to data from the studies in adult subjects with schizophrenia, pooled data from the two placebo-controlled 6-week studies in adult subjects with schizoaffective disorder showed similar types and frequencies of EPS as measured by rating scales, anticholinergic medication use, and spontaneous reports of EPS-related adverse events. For subjects with schizoaffective disorder, there was no dose-related increase in EPS observed for parkinsonism with the Simpson-Angus scale or akathisia with the Barnes Akathisia Rating Scale. There was a dose-related increase observed with spontaneous EPS reports of hyperkinesia and dystonia and in the use of anticholinergic medications.
Table 9 shows the EPS data from the pooled schizoaffective disorder trials.
Table 9. Treatment-Emergent Extrapyramidal Symptoms (EPS)-Related Adverse Events by MedDRA Preferred Term Schizoaffective Disorder Studies in Adults|
Dyskinesia group includes: Dyskinesia, muscle twitching | ||||
|
Percentage of Patients | ||||
|
Paliperidone Extended-Release Tablets | ||||
|
Placebo |
3-6 mg |
9-12 mg |
3-12 mg | |
|
once daily |
once daily |
once daily | ||
|
fixed-dose range |
fixed-dose range |
flexible dose | ||
|
EPS Group |
(N = 202) |
(N = 108) |
(N = 98) |
(N = 214) |
|
Overall percentage of patients with EPS-related AE |
11 |
23 |
22 |
17 |
|
Dyskinesia |
1 |
3 |
1 |
1 |
|
Dystonia |
1 |
2 |
3 |
2 |
|
Hyperkinesia |
5 |
5 |
8 |
7 |
|
Parkinsonism |
3 |
14 |
7 |
7 |
|
Tremor |
3 |
12 |
11 |
5 |
The incidences of EPS-related adverse events in the adolescent schizophrenia studies showed a similar dose-related pattern to those in the adult studies. There were notably higher incidences of dystonia, hyperkinesia, tremor, and parkinsonism in the adolescent population as compared to the adult studies (Table 10).
Table 10. Treatment-Emergent Extrapyramidal Symptoms (EPS)-Related Adverse Events by MedDRA Preferred Term Schizophrenia Studies in Adolescent Subjects|
Hyperkinesia group includes: Akathisia | |||||
|
Percentage of Patients | |||||
|
Paliperidone Extended-Release Tablets | |||||
|
Placebo |
1.5 mg |
3 mg |
6 mg |
12 mg | |
|
once daily |
once daily |
once daily |
once daily | ||
|
EPS Group |
(N = 51) |
(N = 54) |
(N = 16) |
(N = 45) |
(N = 35) |
|
Overall percentage of patients with EPS-related AE |
0 |
6 |
25 |
22 |
40 |
|
Hyperkinesia |
0 |
4 |
6 |
11 |
17 |
|
Dystonia |
0 |
2 |
0 |
11 |
14 |
|
Tremor |
0 |
2 |
6 |
7 |
11 |
|
Parkinsonism |
0 |
0 |
6 |
2 |
14 |
|
Dyskinesia |
0 |
2 |
6 |
2 |
6 |
Dystonia
Class Effect:Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Laboratory Test Abnormalities
In the pooled data from the three placebo-controlled, 6-week, fixed-dose studies in adult subjects with schizophrenia and from the two placebo- controlled, 6-week studies in adult subjects with schizoaffective disorder, between-group comparisons revealed no medically important differences between paliperidone extended-release tablets and placebo in the proportions of subjects experiencing potentially clinically significant changes in routine serum chemistry, hematology, or urinalysis parameters. Similarly, there were no differences between paliperidone extended-release tablets and placebo in the incidence of discontinuations due to changes in hematology, urinalysis, or serum chemistry, including mean changes from baseline in fasting glucose, insulin, c-peptide, triglyceride, HDL, LDL, and total cholesterol measurements. However, paliperidone extended-release tablets were associated with increases in serum prolactin [see Warnings and Precautions (5.7)] .
Other Adverse Reactions Observed During Premarketing Evaluation of Paliperidone Extended-Release Tablets
The following additional adverse reactions occurred in < 2% of paliperidone extended-release tablets-treated subjects in the above schizophrenia and schizoaffective disorder clinical trial datasets. The following also includes additional adverse reactions reported at any frequency by paliperidone extended-release tablets-treated subjects who participated in other clinical studies.
Cardiac Disorders: bradycardia, palpitations
**Eye Disorders:**eye movement disorder
**Gastrointestinal Disorders:**flatulence
**General Disorders:**edema
**Immune System Disorders:**anaphylactic reaction
**Infections and Infestations:**urinary tract infection
**Investigations:**alanine aminotransferase increased, aspartate aminotransferase increased
**Musculoskeletal and Connective Tissue Disorders:**arthralgia, pain in extremity
**Nervous System Disorders:**opisthotonus
**Psychiatric Disorders:**agitation, insomnia, nightmare
**Reproductive System and Breast Disorders:**breast discomfort, menstruation irregular, retrograde ejaculation
**Respiratory, Thoracic and Mediastinal Disorders:**nasal congestion
**Skin and Subcutaneous Tissue Disorders:**pruritus, rash
**Vascular Disorders:**hypertension
The safety of paliperidone extended-release tablets was also evaluated in a long-term trial designed to assess the maintenance of effect with paliperidone extended-release tablets in adults with schizophrenia [see Clinical Studies (14)] . In general, adverse reaction types, frequencies, and severities during the initial 14-week open-label phase of this study were comparable to those observed in the 6-week, placebo-controlled, fixed-dose studies. Adverse reactions reported during the long-term double-blind phase of this study were similar in type and severity to those observed in the initial 14-week open- label phase.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of paliperidone extended-release tablets; because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency: angioedema, ileus, priapism, somnambulism, swollen tongue, tardive dyskinesia, urinary incontinence, urinary retention.
6.3 Adverse Reactions Reported with Risperidone
Paliperidone is the major active metabolite of risperidone. Adverse reactions reported with risperidone can be found in the ADVERSE REACTIONS section of the risperidone package insert.
Commonly observed adverse reactions (incidence ≥ 5% and at least twice that for placebo) were ( 6)
- Adults with schizophrenia: extrapyramidal symptoms, tachycardia, and akathisia.
- Adolescents with schizophrenia: somnolence, akathisia, tremor, dystonia, cogwheel rigidity, anxiety, weight increased, and tachycardia.
- Adults with schizoaffective disorder: extrapyramidal symptoms, somnolence, dyspepsia, constipation, weight increased, and nasopharyngitis.
To report SUSPECTED ADVERSE REACTIONS, contact RK Pharma Inc at 1-844-757-4276 (1-844-RKPHARM) or FDA at 1-800-FDA-1088 orhttp://www.fda.gov/medwatch
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Potential for Paliperidone Extended-Release Tablets to Affect Other
Drugs
Given the primary CNS effects of paliperidone [see Adverse Reactions (6.1, 6.2)] , paliperidone extended-release tablets should be used with caution in combination with other centrally acting drugs and alcohol. Paliperidone may antagonize the effect of levodopa and other dopamine agonists.
Because of its potential for inducing orthostatic hypotension, an additive effect may be observed when paliperidone extended-release tablets are administered with other therapeutic agents that have this potential [see Warnings and Precautions (5.9)] .
Paliperidone is not expected to cause clinically important pharmacokinetic interactions with drugs that are metabolized by cytochrome P450 isozymes. In vitrostudies in human liver microsomes showed that paliperidone does not substantially inhibit the metabolism of drugs metabolized by cytochrome P450 isozymes, including CYP1A2, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4, and CYP3A5. Therefore, paliperidone is not expected to inhibit clearance of drugs that are metabolized by these metabolic pathways in a clinically relevant manner. Paliperidone is also not expected to have enzyme inducing properties.
Paliperidone is a weak inhibitor of P-glycoprotein (P-gp) at high concentrations. No in vivodata are available and the clinical relevance is unknown.
Pharmacokinetic interaction between lithium and paliperidone extended-release tablets is unlikely.
In a drug interaction study, co-administration of paliperidone extended- release tablets (12 mg once daily for 5 days) with divalproex sodium extended- release tablets (500 mg to 2000 mg once daily) did not affect the steady-state pharmacokinetics (AUC 24hand C max,ss) of valproate in 13 patients stabilized on valproate. In a clinical study, subjects on stable doses of valproate had comparable valproate average plasma concentrations when paliperidone extended- release tablets 3-15 mg/day were added to their existing valproate treatment.
7.2 Potential for Other Drugs to Affect Paliperidone Extended-Release
Tablets
Paliperidone is not a substrate of CYP1A2, CYP2A6, CYP2C9, and CYP2C19, so that an interaction with inhibitors or inducers of these isozymes is unlikely. While in vitrostudies indicate that CYP2D6 and CYP3A4 may be minimally involved in paliperidone metabolism, in vivostudies do not show decreased elimination by these isozymes and they contribute to only a small fraction of total body clearance. In vitrostudies have shown that paliperidone is a P-gp substrate.
Co-administration of paliperidone extended-release tablets 6 mg once daily with carbamazepine, a strong inducer of both CYP3A4 and P-glycoprotein (P-gp), at 200 mg twice daily caused a decrease of approximately 37% in the mean steady-state C maxand AUC of paliperidone. This decrease is caused, to a substantial degree, by a 35% increase in renal clearance of paliperidone. A minor decrease in the amount of drug excreted unchanged in the urine suggests that there was little effect on the CYP metabolism or bioavailability of paliperidone during carbamazepine co-administration. On initiation of carbamazepine, the dose of paliperidone extended-release tablets should be re- evaluated and increased if necessary. Conversely, on discontinuation of carbamazepine, the dose of paliperidone extended-release tablets should be re- evaluated and decreased if necessary.
Paliperidone is metabolized to a limited extent by CYP2D6 [see Clinical Pharmacology (12.3)] . In an interaction study in healthy subjects in which a single 3 mg dose of paliperidone extended-release tablets was administered concomitantly with 20 mg per day of paroxetine (a potent CYP2D6 inhibitor), paliperidone exposures were on average 16% (90% CI: 4, 30) higher in CYP2D6 extensive metabolizers. Higher doses of paroxetine have not been studied. The clinical relevance is unknown.
Co-administration of a single dose of paliperidone extended-release tablets 12 mg with divalproex sodium extended-release tablets (two 500 mg tablets once daily) resulted in an increase of approximately 50% in the C maxand AUC of paliperidone. Dosage reduction for paliperidone extended-release tablets should be considered when paliperidone extended-release tablets are co- administered with valproate after clinical assessment.
Pharmacokinetic interaction between lithium and paliperidone extended-release tablets is unlikely.
- Centrally-acting drugs: Due to CNS effects, use caution in combination. Avoid alcohol. ( 7.1)
- Drugs that may cause orthostatic hypotension: An additive effect may be observed when co-administered with paliperidone extended-release tablets. ( 7.1)
- Strong CYP3A4/P-glycoprotein (P-gp) inducers: It may be necessary to increase the dose of paliperidone extended-release tablets when a strong inducer of both CYP3A4 and P-gp (e.g., carbamazepine) is co-administered. Conversely, on discontinuation of the strong inducer, it may be necessary to decrease the dose of paliperidone extended-release tablets. ( 7.2)
- Co-administration of divalproex sodium increased C maxand AUC of paliperidone by approximately 50%. Adjust dose of paliperidone extended-release tablets if necessary based on clinical assessment. ( 7.2)
RECENT MAJOR CHANGES SECTION
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Schizophrenia
Adults
The recommended dose of paliperidone extended-release tablets for the treatment of schizophrenia in adults is 6 mg administered once daily. Initial dose titration is not required. Although it has not been systematically established that doses above 6 mg have additional benefit, there was a general trend for greater effects with higher doses. This must be weighed against the dose-related increase in adverse reactions. Thus, some patients may benefit from higher doses, up to 12 mg/day, and for some patients, a lower dose of 3 mg/day may be sufficient. Dose increases above 6 mg/day should be made only after clinical reassessment and generally should occur at intervals of more than 5 days. When dose increases are indicated, increments of 3 mg/day are recommended. The maximum recommended dose is 12 mg/day.
In a longer-term study, paliperidone extended-release tablets have been shown to be effective in delaying time to relapse in patients with schizophrenia who were stabilized on paliperidone extended-release tablets for 6 weeks [see Clinical Studies (14)] . Paliperidone extended-release tablets should be prescribed at the lowest effective dose for maintaining clinical stability and the physician should periodically reevaluate the long-term usefulness of the drug in individual patients.
Adolescents (12-17 years of age)
The recommended starting dose of paliperidone extended-release tablets for the treatment of schizophrenia in adolescents 12-17 years of age is 3 mg administered once daily. Initial dose titration is not required. Dose increases, if considered necessary, should be made only after clinical reassessment and should occur at increments of 3 mg/day at intervals of more than 5 days. Prescribers should be mindful that, in the adolescent schizophrenia study, there was no clear enhancement to efficacy at the higher doses, i.e., 6 mg for subjects weighing less than 51 kg and 12 mg for subjects weighing 51 kg or greater, while adverse events were dose-related.
2.2 Schizoaffective Disorder
The recommended dose of paliperidone extended-release tablets for the treatment of schizoaffective disorder in adults is 6 mg administered once daily. Initial dose titration is not required. Some patients may benefit from lower or higher doses within the recommended dose range of 3 to 12 mg once daily. A general trend for greater effects was seen with higher doses. This trend must be weighed against dose-related increase in adverse reactions. Dosage adjustment, if indicated, should occur only after clinical reassessment. Dose increases, if indicated, generally should occur at intervals of more than 4 days. When dose increases are indicated, increments of 3 mg/day are recommended. The maximum recommended dose is 12 mg/day.
2.3 Administration Instructions
Paliperidone extended-release tablets can be taken with or without food.
Paliperidone extended-release tablets must be swallowed whole with the aid of liquids. Tablets should not be chewed, divided, or crushed. The medication is contained within a nonabsorbable shell designed to release the drug at a controlled rate. The tablet shell, along with insoluble core components, is eliminated from the body; patients should not be concerned if they occasionally notice in their stool something that looks like a tablet.
2.4 Use with Risperidone
Concomitant use of paliperidone extended-release tablets with risperidone has not been studied. Since paliperidone is the major active metabolite of risperidone, consideration should be given to the additive paliperidone exposure if risperidone is coadministered with paliperidone extended-release tablets.
2.5 Dosage in Special Populations
Renal Impairment
Dosing must be individualized according to the patient’s renal function status. For patients with mild renal impairment (creatinine clearance ≥ 50 mL/min to < 80 mL/min), the recommended initial dose of paliperidone extended- release tablets is 3 mg once daily. The dose may then be increased to a maximum of 6 mg once daily based on clinical response and tolerability. For patients with moderate to severe renal impairment (creatinine clearance ≥ 10 mL/min to < 50 mL/min), the recommended initial dose of paliperidone extended- release tablets is 1.5 mg once daily, which may be increased to a maximum of 3 mg once daily after clinical reassessment. As paliperidone extended-release tablets have not been studied in patients with creatinine clearance below 10 mL/min, use is not recommended in such patients [see Clinical Pharmacology (12.3)].
Hepatic Impairment
For patients with mild to moderate hepatic impairment, (Child-Pugh Classification A and B), no dose adjustment is recommended [see Clinical Pharmacology (12.3)] . Paliperidone extended-release tablets have not been studied in patients with severe hepatic impairment.
Elderly
Because elderly patients may have diminished renal function, dose adjustments may be required according to their renal function status. In general, recommended dosing for elderly patients with normal renal function is the same as for younger adult patients with normal renal function. For patients with moderate to severe renal impairment (creatinine clearance 10 mL/min to < 50 mL/min), the maximum recommended dose of paliperidone extended-release tablets is 3 mg once daily [see Renal Impairmentabove] .
|
Initial Dose |
Recommended Dose |
Maximum Dose | ||
|
Schizophrenia – adults ( 2.1) |
6 mg/day |
3 - 12 mg/day |
12 mg/day | |
|
Schizophrenia – adolescents ( 2.1) |
Weight < 51 kg |
3 mg/day |
3 - 6 mg/day |
6 mg/day |
|
Weight ≥ 51 kg |
3 mg/day |
3 - 12 mg/day |
12 mg/day | |
|
Schizoaffective disorder – adults ( 2.2) |
6 mg/day |
3 - 12 mg/day |
12 mg/day |
- Tablet should be swallowed whole and should not be chewed, divided, or crushed. ( 2.3)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Paliperidone Extended-Release Tablets are available containing 3 mg, of paliperidone, USP.
- The 3 mg tablets are white, film-coated, round, unscored tablets imprinted withMoverPD3in black ink on one side of the tablet and blank on the other side.
Tablets: 3 mg ( 3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in
women exposed to atypical antipsychotics, including paliperidone extended-
release tablets, during pregnancy. Healthcare providers are encouraged to
register patients by contacting the National Pregnancy Registry for Atypical
Antipsychotics at 1-866-961-2388 or online at
http://womensmentalhealth.org/clinical-and-research-
programs/pregnancyregistry/.
Risk Summary
Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations) . Overall, available data from published epidemiologic studies of pregnant women exposed to paliperidone have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data) . There are risks to the mother associated with untreated schizophrenia and with exposure to antipsychotics, including paliperidone extended-release tablets, during pregnancy (see Clinical Considerations).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
In animal reproduction studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated with paliperidone during the period of organogenesis with up to 8 times the maximum recommended human dose (MRHD) based on mg/m 2body surface area. Additional reproduction toxicity studies were conducted with orally administered risperidone, which is extensively converted to paliperidone (see Animal data).
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
There is a risk to the mother from untreated schizophrenia, including increased risk of relapse, hospitalization, and suicide. Schizophrenia are associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors.
Fetal/Neonatal Adverse Reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs, including paliperidone extended-release tablets, during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization.
Data
Human Data:
Published data from observational studies, birth registries, and case reports on the use of atypical antipsychotics during pregnancy do not report a clear association with antipsychotics and major birth defects. A prospective observational study including 6 women treated with risperidone, the parent compound of paliperidone, demonstrated placental passage of risperidone and paliperidone. A retrospective cohort study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects. There was a small increase in the risk of major birth defects (RR = 1.26, 95% CI 1.02 – 1.56) and of cardiac malformations (RR = 1.26, 95% CI 0.88 – 1.81) in a subgroup of 1566 women exposed to the parent compound of paliperidone, risperidone, during the first trimester of pregnancy; however, there is no mechanism of action to explain the difference in malformation rates.
Animal Data:
In animal reproduction studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated with paliperidone during the period of organogenesis with up to 8 times the MRHD of 12 mg based on mg/m 2body surface area.
Additional reproduction toxicity studies were conducted with orally administered risperidone, which is extensively converted to paliperidone. Cleft palate was observed in the offspring of pregnant mice treated with risperidone at 3 to 4 times the MRHD of 16 mg based on mg/m 2body surface area; maternal toxicity occurred at 4 times the MHRD. There was no evidence of teratogenicity in embryo-fetal developmental toxicity studies with risperidone in rats and rabbits at doses up to 6 times the MRHD of 16 mg/day risperidone based on mg/m 2body surface area. When the offspring of pregnant rats, treated with risperidone at 0.6 times the MRHD based on mg/m 2body surface area, reached adulthood, learning was impaired. Increased neuronal cell death occurred in the fetal brains of the offspring of pregnant rats treated at 0.5 to 1.2 times the MRHD; the postnatal development and growth of the offspring was delayed.
In rat reproduction studies with risperidone, pup deaths occurred at oral doses which are less than the MRHD of risperidone based on mg/m 2body surface area; it is not known whether these deaths were due to a direct effect on the fetuses or pups or to effects on the dams (see RISPERDAL ®package insert).
8.2 Lactation
Risk Summary
Limited data from published literature report the presence of paliperidone in human breast milk. There is no information on the effects on the breastfed infant, or the effects on milk production; however, there are reports of sedation, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements) in breastfed infants exposed to paliperidone's parent compound, risperidone (see Clinical Considerations) . The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for paliperidone extended-release tablets and any potential adverse effects on the breastfed child from paliperidone extended- release tablets or from the mother's underlying condition.
Clinical Considerations
Infants exposed to paliperidone through breastmilk should be monitored for excess sedation, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements).
8.3 Females and Males of Reproductive Potential
Infertility
Females:
Based on the pharmacologic action of paliperidone (D2 receptor antagonism), treatment with paliperidone extended-release tablets may result in an increase in serum prolactin levels, which may lead to a reversible reduction in fertility in females of reproductive potential [see Warnings and Precautions (5.7)].
8.4 Pediatric Use
Safety and effectiveness of paliperidone extended-release tablets in the treatment of schizophrenia were evaluated in 150 adolescent subjects 12-17 years of age with schizophrenia who received paliperidone extended-release tablets in the dose range of 1.5 mg to 12 mg/day in a 6-week, double-blind, placebo-controlled trial.
Safety and effectiveness of paliperidone extended-release tablets for the treatment of schizophrenia in patients < 12 years of age have not been established. Safety and effectiveness of paliperidone extended-release tablets for the treatment of schizoaffective disorder in patients < 18 years of age have not been studied.
Juvenile Animal Studies
In a study in which juvenile rats were treated with oral paliperidone from days 24 to 73 of age, a reversible impairment of performance in a test of learning and memory was seen, in females only, with a no-effect dose of 0.63 mg/kg/day, which produced plasma levels (AUC) of paliperidone similar to those in adolescents at MRHD of 12 mg/day. No other consistent effects on neurobehavioral or reproductive development were seen up to the highest dose tested (2.5 mg/kg/day), which produced plasma levels of paliperidone 2-3 times those in adolescents.
Juvenile dogs were treated for 40 weeks with oral risperidone, which is extensively metabolized to paliperidone in animals and humans, at doses of 0.31, 1.25, or 5 mg/kg/day. Decreased bone length and density were seen with a no-effect dose of 0.31 mg/kg/day, which produced plasma levels (AUC) of risperidone plus paliperidone which were similar to those in children and adolescents receiving the MRHD of risperidone. In addition, a delay in sexual maturation was seen at all doses in both males and females. The above effects showed little or no reversibility in females after a 12-week drug-free recovery period.
The long-term effects of paliperidone extended-release tablets on growth and sexual maturation have not been fully evaluated in children and adolescents.
8.5 Geriatric Use
The safety, tolerability, and efficacy of paliperidone extended-release tablets were evaluated in a 6-week placebo-controlled study of 114 elderly subjects with schizophrenia (65 years of age and older, of whom 21 were 75 years of age and older). In this study, subjects received flexible doses of paliperidone extended-release tablets (3 mg to 12 mg once daily). In addition, a small number of subjects 65 years of age and older were included in the 6-week placebo-controlled studies in which adult schizophrenic subjects received fixed doses of paliperidone extended-release tablets (3 mg to 15 mg once daily) [see Clinical Studies (14)] . There were no subjects ≥ 65 years of age in the schizoaffective disorder studies.
Overall, of the total number of subjects in schizophrenia clinical studies of paliperidone extended-release tablets (n = 1796), including those who received paliperidone extended-release tablets or placebo, 125 (7.0%) were 65 years of age and older and 22 (1.2%) were 75 years of age and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in response between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
This drug is known to be substantially excreted by the kidney and clearance is decreased in patients with moderate to severe renal impairment [see Clinical Pharmacology (12.3)] , who should be given reduced doses. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Dosage and Administration (2.5)] .
8.6 Renal Impairment
Dosing must be individualized according to the patient’s renal function status [see Dosage and Administration (2.5)] .
8.7 Hepatic Impairment
No dosage adjustment is required in patients with mild to moderate hepatic impairment. Paliperidone extended-release tablets have not been studied in patients with severe hepatic impairment.
8.8 Patients with Parkinson’s Disease or Lewy Body Dementia
Patients with Parkinson’s Disease or Dementia with Lewy Bodies can experience increaded sensitivity to paliperidone extended-release tablets. Manifestations can include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with neuroleptic malignant syndrome.
- Renal Impairment: Dosing must be individualized according to renal function status. ( 2.5)
- Elderly: Same as for younger adults (adjust dose according to renal function status). ( 2.4)
- Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. ( 8.1)
- Pediatric Use: Safety and effectiveness in the treatment of schizophrenia not established in patients less than 12 years of age. Safety and effectiveness in the treatment of schizoaffective disorder not established in patients less than 18 years of age. ( 8.4)
OVERDOSAGE SECTION
10 OVERDOSAGE
10.1 Human Experience
While experience with paliperidone overdose is limited, among the few cases of overdose reported in pre-marketing trials, the highest estimated ingestion of paliperidone extended-release tablets was 405 mg. Observed signs and symptoms included extrapyramidal symptoms and gait unsteadiness. Other potential signs and symptoms include those resulting from an exaggeration of paliperidone’s known pharmacological effects, i.e., drowsiness and somnolence, tachycardia and hypotension, and QT prolongation. Torsade de pointes and ventricular fibrillation have been reported in a patient in the setting of overdose.
Paliperidone is the major active metabolite of risperidone. Overdose experience reported with risperidone can be found in the OVERDOSAGE section of the risperidone package insert.
10.2 Management of Overdosage
There is no specific antidote to paliperidone, therefore, appropriate supportive measures should be instituted and close medical supervision and monitoring should continue until the patient recovers. Consideration should be given to the extended-release nature of the product when assessing treatment needs and recovery. Multiple drug involvement should also be considered.
In case of acute overdose, establish and maintain an airway and ensure adequate oxygenation and ventilation. Administration of activated charcoal together with a laxative should be considered.
The possibility of obtundation, seizures, or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis.
Cardiovascular monitoring should commence immediately, including continuous electrocardiographic monitoring for possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of additive QT-prolonging effects when administered in patients with an acute overdose of paliperidone. Similarly, the alpha-blocking properties of bretylium might be additive to those of paliperidone, resulting in problematic hypotension.
Hypotension and circulatory collapse should be treated with appropriate measures, such as intravenous fluids and/or sympathomimetic agents (epinephrine and dopamine should not be used, since beta stimulation may worsen hypotension in the setting of paliperidone-induced alpha blockade). In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered.
DESCRIPTION SECTION
11 DESCRIPTION
Paliperidone Extended-Release Tablets contain paliperidone, USP, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. Paliperidone extended-release tablets contain a racemic mixture of (+)- and (-)- paliperidone. The chemical name is (9 RS)-3-[2-[4-(6-Fluoro-1,2-benzisoxazol-3-yl)piperidin-1-yl]]ethyl]-9-hydroxy-2-methyl-6,7,8,9-tetrahydro-4 H-pyrido[1,2- a]pyrimidin-4-one. Its molecular formula is C 23H 27FN 4O 3and its molecular weight is 426.49. The structural formula is:
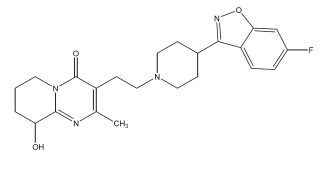
Paliperidone is sparingly soluble in 0.1N HCl and methylene chloride; practically insoluble in water, 0.1N NaOH, and hexane; and slightly soluble in N,N-dimethylformamide.
Paliperidone extended-release tablets are intended for oral administration and are available in 1.5 mg (brown), 3 mg (white), 6 mg (light beige), and 9 mg (pink) strengths. Paliperidone extended-release tablets utilize osmotic drug- release technology [seeDescription (11)].
Inactive ingredients are butylated hydroxytoluene, cellulose acetate, colloidal silicon dioxide, hydroxypropyl cellulose, hypromellose, polyethylene glycol, polyethylene oxide, red iron oxide, sodium chloride, sodium stearyl fumarate, talc, titanium dioxide and yellow iron oxide.
The 1.5 mg tablets also contain black iron oxide and polydextrose. The 3 mg tablets also contain polyvinyl alcohol. The 6 mg tablets also contain black iron oxide, FD&C Blue No. 1 Aluminum Lake and polyvinyl alcohol. The 9 mg tablets also contain FD&C Blue No. 1 Aluminum Lake and polyvinyl alcohol.
The imprinting ink contains the following: black iron oxide, hypromellose and propylene glycol.
Delivery System Components and Performance
Paliperidone extended-release uses osmotic pressure to deliver paliperidone at a controlled rate. The delivery system, which resembles a capsule-shaped tablet in appearance, consists of an osmotically active trilayer core surrounded by a subcoat and semipermeable membrane. The trilayer core is composed of two drug layers containing the drug and excipients, and a push layer containing osmotically active components. There are two precision laser- drilled orifices on the drug-layer dome of the tablet. Each tablet strength has a different colored water-dispersible overcoat and print markings. In an aqueous environment, such as the gastrointestinal tract, the water-dispersible color overcoat erodes quickly. Water then enters the tablet through the semipermeable membrane that controls the rate at which water enters the tablet core, which, in turn, determines the rate of drug delivery. The hydrophilic polymers of the core hydrate and swell, creating a gel containing paliperidone that is then pushed out through the tablet orifices. The biologically inert components of the tablet remain intact during gastrointestinal transit and are eliminated in the stool as a tablet shell, along with insoluble core components.
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Paliperidone is not a controlled substance.
9.2 Abuse
Paliperidone has not been systematically studied in animals or humans for its potential for abuse. It is not possible to predict the extent to which a CNS- active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of paliperidone extended-release tablets misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior).
9.3 Dependence
Paliperidone has not been systematically studied in animals or humans for its potential for tolerance or physical dependence.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Paliperidone is the major active metabolite of risperidone. The mechanism of action of paliperidone in schizophrenia is unclear. However, the drug’s therapeutic effect in schizophrenia could be mediated through a combination of central dopamine Type 2 (D 2) and serotonin Type 2 (5HT 2A) receptor antagonism.
12.2 Pharmacodynamics
In vitro, paliperidone acts as an antagonist at the central dopamine Type 2 (D 2) and serotonin Type 2 (5HT 2A) receptors, with binding affinities (Ki values) of 1.6 – 2.8 nM for D 2and 0.8 – 1.2 nM for 5HT 2Areceptors. Paliperidone is also active as an antagonist at the α 1and α 2adrenergic receptors and H 1histaminergic receptors, which may explain some of the other effects of the drug. Paliperidone has no affinity for cholinergic muscarinic or β 1- and β 2-adrenergic receptors. The pharmacological activity of the (+)- and (-)- paliperidone enantiomers is qualitatively and quantitatively similar in vitro.
12.3 Pharmacokinetics
Following a single dose, the plasma concentrations of paliperidone gradually rise to reach peak plasma concentration (C max) approximately 24 hours after dosing. The pharmacokinetics of paliperidone following paliperidone extended- release tablets administration are dose-proportional within the available dose range. The terminal elimination half-life of paliperidone is approximately 23 hours.
Steady-state concentrations of paliperidone are attained within 4-5 days of dosing with paliperidone extended-release tablets in most subjects. The mean steady-state peak:trough ratio for a paliperidone extended-release tablets dose of 9 mg was 1.7 with a range of 1.2-3.1.
Following administration of paliperidone extended-release tablets, the (+) and (-) enantiomers of paliperidone interconvert, reaching an AUC (+) to (-) ratio of approximately 1.6 at steady-state.
Absorption and Distribution
The absolute oral bioavailability of paliperidone following paliperidone extended-release tablets administration is 28%.
Administration of a 12 mg paliperidone extended-release tablet to healthy ambulatory subjects with a standard high-fat/high-caloric meal gave mean C maxand AUC values of paliperidone that were increased by 60% and 54%, respectively, compared with administration under fasting conditions. Clinical trials establishing the safety and efficacy of paliperidone extended-release tablets were carried out in subjects without regard to the timing of meals. While paliperidone extended-release tablets can be taken without regard to food, the presence of food at the time of paliperidone extended-release tablets administration may increase exposure to paliperidone [see Dosage and Administration (2.3)] .
Based on a population analysis, the apparent volume of distribution of paliperidone is 487 L. The plasma protein binding of racemic paliperidone is 74%.
Metabolism and Elimination
Although in vitrostudies suggested a role for CYP2D6 and CYP3A4 in the metabolism of paliperidone, in vivoresults indicate that these isozymes play a limited role in the overall elimination of paliperidone [see Drug Interactions (7)] .
One week following administration of a single oral dose of 1 mg immediate- release 14C-paliperidone to 5 healthy volunteers, 59% (range 51% - 67%) of the dose was excreted unchanged into urine, 32% (26% - 41%) of the dose was recovered as metabolites, and 6% - 12% of the dose was not recovered. Approximately 80% of the administered radioactivity was recovered in urine and 11% in the feces. Four primary metabolic pathways have been identified in vivo, none of which could be shown to account for more than 10% of the dose: dealkylation, hydroxylation, dehydrogenation, and benzisoxazole scission.
Population pharmacokinetic analyses found no difference in exposure or clearance of paliperidone between extensive metabolizers and poor metabolizers of CYP2D6 substrates.
Special Populations
Renal Impairment:
The dose of paliperidone extended-release tablets should be reduced in patients with moderate or severe renal impairment [see Dosage and Administration (2.5)] . The disposition of a single dose paliperidone 3 mg extended-release tablet was studied in adult subjects with varying degrees of renal function. Elimination of paliperidone decreased with decreasing estimated creatinine clearance. Total clearance of paliperidone was reduced in subjects with impaired renal function by 32% on average in mild (CrCl = 50 mL/min to < 80 mL/min), 64% in moderate (CrCl = 30 mL/min to < 50 mL/min), and 71% in severe (CrCl = 10 mL/min to < 30 mL/min) renal impairment, corresponding to an average increase in exposure (AUC inf) of 1.5 fold, 2.6 fold, and 4.8 fold, respectively, compared to healthy subjects. The mean terminal elimination half-life of paliperidone was 24 hours, 40 hours, and 51 hours in subjects with mild, moderate, and severe renal impairment, respectively, compared with 23 hours in subjects with normal renal function (CrCl ≥ 80 mL/min).
Hepatic Impairment:
In a study in adult subjects with moderate hepatic impairment (Child-Pugh class B), the plasma concentrations of free paliperidone were similar to those of healthy subjects, although total paliperidone exposure decreased because of a decrease in protein binding. Consequently, no dose adjustment is required in patients with mild or moderate hepatic impairment. Paliperidone extended- release tablets have not been studied in patients with severe hepatic impairment.
Adolescents (12 - 17 years of age):
Paliperidone systemic exposure in adolescents weighing ≥ 51 kg (≥ 112 lbs) was similar to that in adults. In adolescents weighing < 51 kg (< 112 lbs), a 23% higher exposure was observed; this is considered not to be clinically significant. Age did not influence the paliperidone exposure.
Elderly:
No dosage adjustment is recommended based on age alone. However, dose adjustment may be required because of age-related decreases in creatinine clearance [see Renal Impairmentabove and Dosage and Administration (2.1, 2.5)] .
Race:
No dosage adjustment is recommended based on race. No differences in pharmacokinetics were observed in a pharmacokinetic study conducted in Japanese and Caucasians.
Gender:
No dosage adjustment is recommended based on gender. No differences in pharmacokinetics were observed in a pharmacokinetic study conducted in men and women.
Smoking:
No dosage adjustment is recommended based on smoking status. Based on in vitrostudies utilizing human liver enzymes, paliperidone is not a substrate for CYP1A2; smoking should, therefore, not have an effect on the pharmacokinetics of paliperidone.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies with paliperidone administered orally have not been performed.
Carcinogenicity studies with risperidone, which is extensively converted to paliperidone in rats, mice, and humans, were conducted in Swiss albino mice and Wistar rats. Risperidone was administered in the diet at daily doses of 0.63, 2.5, and 10 mg/kg for 18 months to mice and for 25 months to rats. A maximum tolerated dose was not achieved in male mice. There were statistically significant increases in pituitary gland adenomas, endocrine pancreas adenomas, and mammary gland adenocarcinomas. The no-effect dose for these tumors was less than or equal to the MRHD of risperidone based on mg/m 2body surface area (see risperidone package insert). An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be mediated by prolonged dopamine D 2antagonism and hyperprolactinemia. The relevance of these tumor findings in rodents to human risk is unclear [see Warnings and Precautions (5.7)] .
Mutagenesis
No evidence of genotoxic potential for paliperidone was found in the Ames reverse mutation test, the mouse lymphoma assay, or the in vivorat micronucleus test.
Impairment of Fertility
In a study of fertility, the percentage of treated female rats that became pregnant was not affected at oral doses of paliperidone of up to 2.5 mg/kg/day which is 2 times the MRHD based on mg/m 2body surface area. However, pre- and post-implantation loss was increased, and the number of live embryos was slightly decreased, at 2.5 mg/kg, a dose that also caused slight maternal toxicity. These parameters were not affected at a dose of 0.63 mg/kg, which is half of the MRHD based on mg/m 2body surface area.
The fertility of male rats was not affected at oral doses of paliperidone of up to 2 times the MRHD of 12 mg/day based on mg/m 2body surface area, although sperm count and sperm viability studies were not conducted with paliperidone. In a subchronic study in Beagle dogs with risperidone, which is extensively converted to paliperidone in dogs and humans, all doses tested (0.31 mg/kg - 5.0 mg/kg) resulted in decreases in serum testosterone and in sperm motility and concentration (0.6 to 10 times the MRHD of 16 mg/day for risperidone, based on mg/m 2body surface area). Serum testosterone and sperm parameters partially recovered, but remained decreased after the last observation (two months after treatment was discontinued).
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Schizophrenia
Adults
The acute efficacy of paliperidone extended-release tablets (3 mg to 15 mg once daily) was established in three placebo-controlled and active-controlled (olanzapine), 6-week, fixed-dose trials in non-elderly adult subjects (mean age of 37) who met DSM-IV criteria for schizophrenia. Studies were carried out in North America, Eastern Europe, Western Europe, and Asia. The doses studied among these three trials included 3 mg/day, 6 mg/day, 9 mg/day, 12 mg/day, and 15 mg/day. Dosing was in the morning without regard to meals.
Efficacy was evaluated using the Positive and Negative Syndrome Scale (PANSS), a validated multi-item inventory composed of five factors to evaluate positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. Efficacy was also evaluated using the Personal and Social Performance (PSP) scale. The PSP is a validated clinician-rated scale that measures personal and social functioning in the domains of socially useful activities (e.g., work and study), personal and social relationships, self-care, and disturbing and aggressive behaviors.
In all 3 studies (n = 1665), paliperidone extended-release tablets were superior to placebo on the PANSS at all doses. Mean effects at all doses were fairly similar, although the higher doses in all studies were numerically superior. Paliperidone extended-release tablets were also superior to placebo on the PSP in these trials.
An examination of population subgroups did not reveal any evidence of differential responsiveness on the basis of gender, age (there were few patients over 65), or geographic region. There were insufficient data to explore differential effects based on race.
In a longer-term trial, adult outpatients meeting DSM-IV criteria for schizophrenia who had clinically responded (defined as PANSS score ≤ 70 or ≤ 4 on pre-defined PANSS subscales, as well as having been on a stable fixed dose of paliperidone extended-release tablets for the last two weeks of an 8-week run-in phase) were entered into a 6-week open-label stabilization phase where they received paliperidone extended-release tablets (doses ranging from 3 mg to 15 mg once daily). After the stabilization phase, patients were randomized in a double-blind manner to either continue on paliperidone extended-release tablets at their achieved stable dose, or to placebo, until they experienced a relapse of schizophrenia symptoms. Relapse was pre-defined as significant increase in PANSS (or pre-defined PANSS subscales), hospitalization, clinically significant suicidal or homicidal ideation, or deliberate injury to self or others. An interim analysis of the data showed a significantly longer time to relapse in patients treated with paliperidone extended-release tablets compared to placebo, and the trial was stopped early because maintenance of efficacy was demonstrated.
Adolescents
The efficacy of paliperidone extended-release tablets in adolescent subjects with schizophrenia was established in a randomized, double-blind, parallel- group, placebo-controlled, 6-week study using a fixed-dose weight-based treatment group design over the dose range of 1.5 to 12 mg/day. The study was carried out in the U.S., India, Romania, Russia, and Ukraine, and involved subjects 12-17 years of age meeting DSM-IV criteria for schizophrenia, with diagnosis confirmation using the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL).
Eligible subjects were randomly assigned to 1 of 4 treatment groups: a placebo group or paliperidone extended-release tablets Low, Medium, or High dose groups. Doses were administered based on body weight to minimize the risk of exposing lower-weight adolescents to high doses of paliperidone extended- release tablets. Subjects weighing between 29 kg and less than 51 kg at the baseline visit were randomly assigned to receive placebo or 1.5 mg (Low dose), 3 mg (Medium dose), or 6 mg (High dose) of paliperidone extended-release tablets daily, and subjects weighing at least 51 kg at the baseline visit were randomly assigned to receive placebo or 1.5 mg (Low dose), 6 mg (Medium dose), or 12 mg (High dose) of paliperidone extended-release tablets daily. Dosing was in the morning without regard to meals.
Efficacy was evaluated using PANSS. Overall, this study demonstrated the efficacy of paliperidone extended-release tablets in adolescents with schizophrenia in the dose range of 3 to 12 mg/day. Doses within this broad range were shown to be effective, however, there was no clear enhancement to efficacy at the higher doses, i.e., 6 mg for subjects weighing less than 51 kg and 12 mg for subjects weighing 51 kg or greater. Although paliperidone was adequately tolerated within the dose range of 3 to 12 mg/day, adverse events were dose-related.
14.2 Schizoaffective Disorder
**Adults:**The acute efficacy of paliperidone extended-release tablets (3 mg to 12 mg once daily) in the treatment of schizoaffective disorder was established in two placebo-controlled, 6-week trials in non-elderly adult subjects. Enrolled subjects 1) met DSM-IV criteria for schizoaffective disorder, as confirmed by the Structured Clinical Interview for DSM-IV Disorders, 2) had a Positive and Negative Syndrome Scale (PANSS) total score of at least 60, and 3) had prominent mood symptoms as confirmed by a score of at least 16 on the Young Mania Rating Scale and/or Hamilton Rating Scale for Depression. The population included subjects with schizoaffective bipolar and depressive types. In one of these trials, efficacy was assessed in 211 subjects who received flexible doses of paliperidone extended-release tablets (3-12 mg once daily). In the other study, efficacy was assessed in 203 subjects who were assigned to one of two dose levels of paliperidone extended- release tablets: 6 mg with the option to reduce to 3 mg (n = 105) or 12 mg with the option to reduce to 9 mg (n = 98) once daily. Both studies included subjects who received paliperidone extended-release tablets either as monotherapy [no mood stabilizers and/or antidepressants (55%)] or as an adjunct to mood stabilizers and/or antidepressants (45%). The most commonly used mood stabilizers were valproate and lithium. The most commonly used antidepressants were SSRIs and SNRIs. Paliperidone extended-release tablets were dosed in the morning without regard to meals. Studies were carried out in the United States, Eastern Europe, Russia, and Asia.
Efficacy was evaluated using the PANSS, a validated multi-item inventory composed of five factors to evaluate positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. As secondary outcomes, mood symptoms were evaluated using the Hamilton Depression Rating Scale (HAM-D-21) and the Young Mania Rating Scale (YMRS).
The paliperidone extended-release tablets group in the flexible-dose study (dosed between 3 and 12 mg/day, mean modal dose of 8.6 mg/day) and the higher dose group of paliperidone extended-release tablets in the 2 dose-level study (12 mg/day with option to reduce to 9 mg/day) were each superior to placebo in the PANSS. Numerical improvements in mood symptoms were also observed, as measured by the HAM-D-21 and YMRS. In the lower dose group of the 2 dose-level study (6 mg/day with option to reduce to 3 mg/day), paliperidone extended- release tablets were not significantly different from placebo as measured by the PANSS.
Taking the results of both studies together, paliperidone extended-release tablets improved the symptoms of schizoaffective disorder at endpoint relative to placebo when administered either as monotherapy or as an adjunct to mood stabilizers and/or antidepressants. An examination of population subgroups did not reveal any evidence of differential responsiveness on the basis of gender, age, or geographic region. There were insufficient data to explore differential effects based on race.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Paliperidone Extended-Release Tablets are available containing 3 mg of paliperidone, USP.
The 3 mg tablets are white, film-coated, round, unscored tablets imprinted with M over PD3 in black ink on one side of the tablet and blank on the other side. They are available as follows:
NDC: 70518-3783-00
PACKAGING: 30 in 1 BLISTER PACK
Storage and Handling: Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Protect from moisture.
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Keep out of reach of children.
Repackaged and Distributed By:
Remedy Repack, Inc.
625 Kolter Dr. Suite #4 Indiana, PA 1-724-465-8762
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Physicians are advised to discuss the following issues with patients for whom they prescribe paliperidone extended-release tablets.
Neuroleptic Malignant Syndrome (NMS)
Counsel patients about a potentially fatal adverse reaction, Neuroleptic
Malignant Syndrome (NMS), that has been reported in association with
administration of antipsychotic drugs. Advise patients, family members, or
caregivers to contact their healthcare provider or report to the emergency
room if they experience signs and symptoms of NMS, including hyperpyrexia,
muscle rigidity, altered mental status including delirium, and evidence of
autonomic instability (irregular pulse or blood pressure, tachycardia,
diaphoresis, and cardiac dysrhythmia) [see Warnings and Precautions (5.3)].
Tardive Dyskinesia
Counsel patients on the signs and symptoms of tardive dyskinesia and to
contact their healthcare provider if these abnormal movements occur [see Warnings and Precautions (5.5)].
Metabolic Changes
Educate patients about the risk of metabolic changes, how to recognize
symptoms of hyperglycemia and diabetes mellitus, and the need for specific
monitoring, including blood glucose, lipids, and weight [see Warnings and Precautions (5.6)].
Orthostatic Hypotension: Educate patients about the risk of orthostatic hypotension and syncope, particularly at the time of initiating treatment, re- initiating treatment, or increasing the dose [see Warnings and Precautions (5.9)].
Leukopenia/Neutropenia
Advise patients with a pre-existing low WBC or a history of drug-induced
leukopenia/neutropenia they should have their CBC monitored while taking
paliperidone extended-release tablets [see Warnings and Precautions (5.11)]
Hyperprolactinemia
Counsel patients on signs and symptoms of hyperprolactinemia that may be
associated with chronic use of paliperidone extended-release tablets. Advise
them to seek medical attention if they experience any of the following:
amenorrhea or galactorrhea in females, erectile dysfunction or gynecomastia in
males [see Warnings and Precautions (5.7)].
**Interference with Cognitive and Motor Performance:**Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery, or operating a motor vehicle, until they are reasonably certain that paliperidone extended-release tablets’ therapy does not affect them adversely [see Warnings and Precautions (5.12)] .
Priapism
Advise patients of the possibility of painful or prolonged penile erections
(priapism). Instruct the patient to seek immediate medical attention in the
event of priapism [see Warnings and Precautions (5.15)].
**Heat Exposure and Dehydration:**Counsel patients on the importance of avoiding overheating and dehydration [see Warnings and Precautions (5.18)] .
Concomitant Medication: Advise patients to inform their healthcare providers if they are taking, or plan to take, any prescription or over-the- counter drugs, as there is a potential for interactions [see Drug Interactions (7)].
**Alcohol:**Patients should be advised to avoid alcohol while taking paliperidone extended-release tablets [see Drug Interactions (7.1)].
**Administration:**Patients should be informed that paliperidone extended- release tablets should be swallowed whole with the aid of liquids. Tablets should not be chewed, divided, or crushed. The medication is contained within a nonabsorbable shell designed to release the drug at a controlled rate. The tablet shell, along with insoluble core components, is eliminated from the body; patients should not be concerned if they occasionally notice something that looks like a tablet in their stool [see Dosage and Administration (2.3)] .
**Pregnancy:**Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with paliperidone extended-release tablets. Advise patients that paliperidone extended-release tablets may cause extrapyramidal and/or withdrawal symptoms in a neonate. Advise patients that there is a pregnancy registry that monitors pregnancy outcomes in women exposed to paliperidone extended-release tablets during pregnancy [see Use in Specific Populations (8.1)] .
**Lactation:**Advise breastfeeding women using paliperidone extended-release tablets to monitor infants for somnolence, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements) and to seek medical care if they notice these signs [see Use in Specific Populations (8.2)].
**Infertility:**Advise females of reproductive potential that paliperidone extended-release tablets may impair fertility due to an increase in serum prolactin levels. The effects on fertility are reversible [see Use in Specific Populations (8.3)] .
The brands listed are trademarks of their respective owners.
Repackaged By / Distributed By: RemedyRepack Inc.
625 Kolter Drive, Indiana, PA 15701
(724) 465-8762
