methimazole
Methimazole Tablets, USPRx only
05a8fed7-f805-4c59-8840-630174b6d130
HUMAN PRESCRIPTION DRUG LABEL
Sep 10, 2025
Viona Pharmaceuticals Inc.
DUNS: 081468959
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
methimazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
methimazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
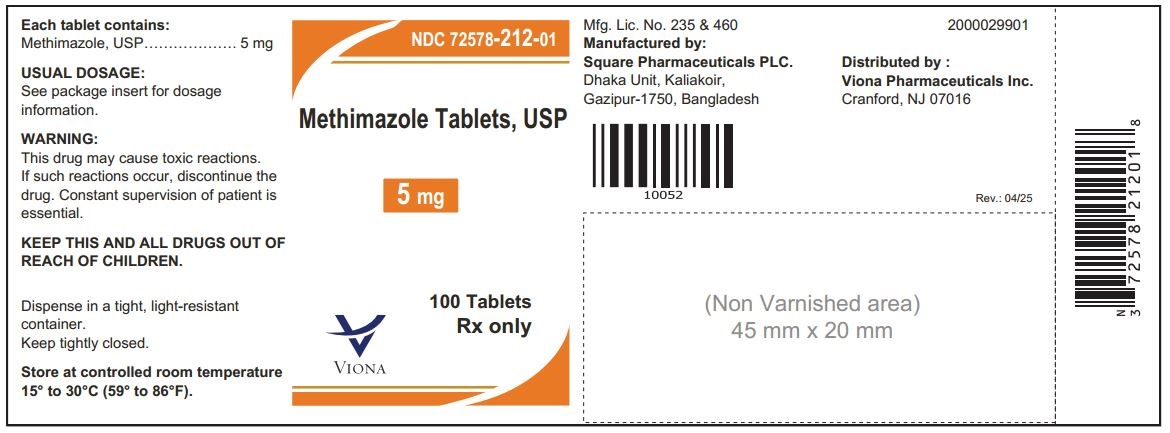
PRINCIPLE DISPLAY PANEL – 5 mg
NDC 72578-212-01
Methimazole Tablets, USP 5 mg
Rx only
100 Tablets
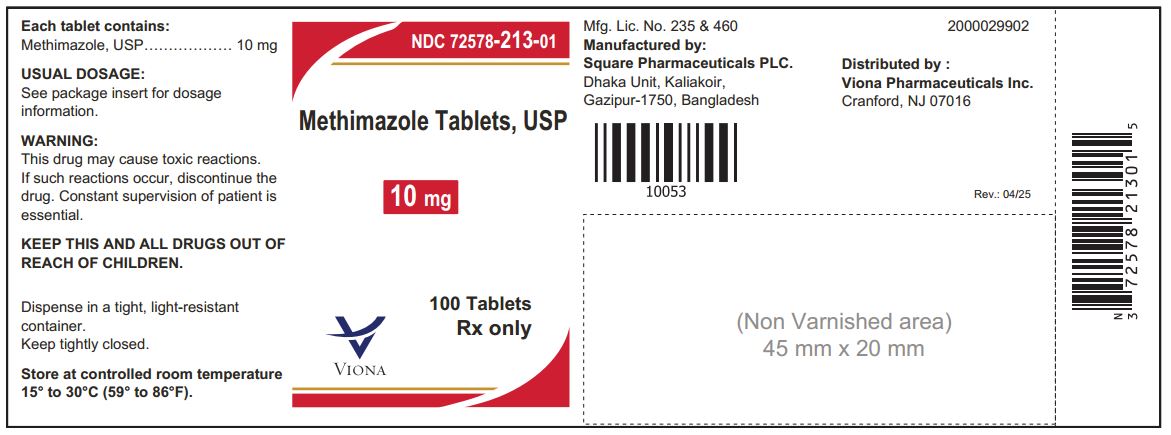
PRINCIPLE DISPLAY PANEL – 10 mg
NDC 72578-213-01
Methimazole Tablets, USP 10 mg
Rx only
100 Tablets
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
CONTRAINDICATIONS SECTION
CONTRAINDICATIONS
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
DESCRIPTION SECTION
DESCRIPTION
SPL UNCLASSIFIED SECTION
Methimazole Tablets, USP 5 mg - White to off-white, round, flat face beveled edge tablets, debossed "C" above bisect"1" below bisect on one side and plain on the other side.
They are available in:
Bottles of 100 NDC 72578-212-01
Methimazole Tablets, USP 10 mg - White to off-white, round, flat face beveled edge tablets, debossed "C" above bisect "11" below bisect on one side and plain on the other side.
They are available in:
Bottles of 100 NDC 72578-213-01
Store at controlled room temperature 15° to 30°C (59° to 86°F).
Dispense in tight, light-resistant container.
Manufactured by:
Square Pharmaceuticals PLC.
Dhaka Unit, Kaliakoir,
Gazipur-1750, Bangladesh
Revised: 04/25
Distributed by:
Viona Pharmaceuticals Inc.
Cranford, NJ 07016
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
WARNINGS SECTION
WARNINGS
First Trimester Use of Methimazole and Congenital Malformations
Methimazole crosses the placental membranes and can cause fetal harm when administered in the first trimester of pregnancy. Rare instances of congenital defects, including aplasia cutis, craniofacial malformations (facial dysmorphism; choanal atresia), gastrointestinal malformations (esophageal atresia with or without tracheoesophageal fistula), omphalocele and abnormalities of the omphalomesenteric duct have occurred in infants born to mothers who received methimazole in the first trimester of pregnancy. If methimazole is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be warned of the potential hazard to the fetus.
Because of the risk for congenital malformations associated with use of methimazole in the first trimester of pregnancy, it may be appropriate to use other agents in pregnant women requiring treatment for hyperthyroidism. If methimazole is used, the lowest possible dose to control the maternal disease should be given.
Agranulocytosis
Agranulocytosis is a potentially life-threatening adverse reaction of methimazole therapy. Patients should be instructed to immediately report to their physicians any symptoms suggestive of agranulocytosis, such as fever or sore throat. Leukopenia, thrombocytopenia, and aplastic anemia (pancytopenia) may also occur. The drug should be discontinued in the presence of agranulocytosis or aplastic anemia (pancytopenia), and the patient's bone marrow indices should be monitored.
Liver Toxicity
Although there have been reports of hepatotoxicity (including acute liver failure) associated with methimazole, the risk of hepatotoxicity appears to be less with methimazole than with propylthiouracil, especially in the pediatric population. Symptoms suggestive of hepatic dysfunction (anorexia, pruritus, right upper quadrant pain, etc.) should prompt evaluation of liver function (bilirubin, alkaline phosphatase) and hepatocellular integrity (ALT, AST). Drug treatment should be discontinued promptly in the event of clinically significant evidence of liver abnormality including hepatic transaminase values exceeding 3 times the upper limit of normal.
Hypothyroidism
Methimazole can cause hypothyroidism necessitating routine monitoring of TSH and free T4 levels with adjustments in dosing to maintain a euthyroid state. Because the drug readily crosses placental membranes, methimazole can cause fetal goiter and cretinism when administered to a pregnant woman. For this reason, it is important that a sufficient, but not excessive, dose be given during pregnancy (see PRECAUTIONS, Pregnancy).
Vasculitis
Cases of vasculitis resulting in severe complications have been reported in patients receiving methimazole therapy. These cases of vasculitis include: leukocytoclastic cutaneous vasculitis, acute kidney injury and glomerulonephritis, alveolar/pulmonary hemorrhage, CNS vasculitis, and neuropathy. Most cases were associated with antineutrophilic cytoplasmic antibodies (ANCA)-positive vasculitis. In some cases, vasculitis resolved/improved with drug discontinuation; however, more severe cases required treatment with additional measures including corticosteroids, immunosuppressant therapy, and plasmapheresis. If vasculitis is suspected, discontinue therapy and initiate appropriate intervention.
PRECAUTIONS SECTION
PRECAUTIONS
General
Patients who receive methimazole should be under close surveillance and should be cautioned to report immediately any evidence of illness, particularly sore throat, skin eruptions, fever, headache, or general malaise. In such cases, white-blood-cell and differential counts should be obtained to determine whether agranulocytosis has developed. Particular care should be exercised with patients who are receiving additional drugs known to cause agranulocytosis.
Information for Patients
Patients should be advised that if they become pregnant or intend to become pregnant while taking an antithyroid drug, they should contact their physician immediately about their therapy.
Inform patients that cases of vasculitis resulting in severe complications have occurred with methimazole tablets. Inform patients to promptly report symptoms that may be associated with vasculitis including new rash, hematuria or decreased urine output, dyspnea or hemoptysis (see WARNINGS and ADVERSE REACTIONS).
Laboratory Tests
Because methimazole may cause hypoprothrombinemia and bleeding, prothrombin time should be monitored during therapy with the drug, especially before surgical procedures. Thyroid function tests should be monitored periodically during therapy. Once clinical evidence of hyperthyroidism has resolved, the finding of a rising serum TSH indicates that a lower maintenance dose of methimazole should be employed.
Drug Interactions
Anticoagulants (oral)
Due to potential inhibition of vitamin K activity by methimazole, the activity of oral anticoagulants (e.g., warfarin) may be increased; additional monitoring of PT/INR should be considered, especially before surgical procedures.
ß-adrenergic blocking agents
Hyperthyroidism may cause an increased clearance of beta blockers with a high extraction ratio. A dose reduction of beta-adrenergic blockers may be needed when a hyperthyroid patient becomes euthyroid.
Digitalis glycosides
Serum digitalis levels may be increased when hyperthyroid patients on a stable digitalis glycoside regimen become euthyroid; a reduced dosage of digitalis glycosides may be needed.
Theophylline
Theophylline clearance may decrease when hyperthyroid patients on a stable theophylline regimen become euthyroid; a reduced dose of theophylline may be needed.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2 year study, rats were given methimazole at doses of 0.5, 3, and 18 mg/kg/day. These doses were 0.3, 2, and 12 times the 15 mg/day maximum human maintenance dose (when calculated on the basis of surface area). Thyroid hyperplasia, adenoma, and carcinoma developed in rats at the two higher doses. The clinical significance of these findings is unclear.
Pregnancy
(See WARNINGS)
If methimazole is used during the first trimester of pregnancy or if the patient becomes pregnant while taking this drug, the patient should be warned of the potential hazard to the fetus.
In pregnant women with untreated or inadequately treated Graves' disease, there is an increased risk of adverse events of maternal heart failure, spontaneous abortion, preterm birth, stillbirth and fetal or neonatal hyperthyroidism.
Because methimazole crosses placental membranes and can induce goiter and cretinism in the developing fetus, hyperthyroidism should be closely monitored in pregnant women and treatment adjusted such that a sufficient, but not excessive, dose be given during pregnancy. In many pregnant women, the thyroid dysfunction diminishes as the pregnancy proceeds; consequently, a reduction of dosage may be possible. In some instances, anti-thyroid therapy can be discontinued several weeks or months before delivery.
Due to the rare occurrence of congenital malformations associated with methimazole use, it may be appropriate to use an alternative anti-thyroid medication in pregnant women requiring treatment for hyperthyroidism, particularly in the first trimester of pregnancy during organogenesis.
Given the potential maternal adverse effects of propylthiouracil (e.g., hepatotoxicity), it may be preferable to switch from propylthiouracil to methimazole for the second and third trimesters.
Nursing Mothers
Methimazole is present in breast milk. However, several studies found no effect on clinical status in nursing infants of mothers taking methimazole. A long-term study of 139 thyrotoxic lactating mothers and their infants failed to demonstrate toxicity in infants who are nursed by mothers receiving treatment with methimazole. Monitor thyroid function at frequent (weekly or biweekly) intervals.
Pediatric Use
Because of postmarketing reports of severe liver injury in pediatric patients treated with propylthiouracil, methimazole is the preferred choice when an antithyroid drug is required for a pediatric patient. (See DOSAGE AND ADMINISTRATION.)
OVERDOSAGE SECTION
OVERDOSAGE
Signs and Symptoms
Symptoms may include nausea, vomiting, epigastric distress, headache, fever, joint pain, pruritus, and edema. Aplastic anemia (pancytopenia) or agranulocytosis may be manifested in hours to days. Less frequent events are hepatitis, nephrotic syndrome, exfoliative dermatitis, neuropathies, and CNS stimulation or depression.
No information is available on the median lethal dose of the drug or the concentration of methimazole in biologic fluids associated with toxicity and/or death.
Treatment
To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center. In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in the patient.
In the event of an overdose, appropriate supportive treatment should be initiated as dictated by the patient's medical status.
