JANUVIA
These highlights do not include all the information needed to use JANUVIA safely and effectively. See full prescribing information for JANUVIA. JANUVIA (sitagliptin) tablets, for oral useInitial U.S. Approval: 2006
f2751b06-9978-4c4f-9309-7130f3197d0b
HUMAN PRESCRIPTION DRUG LABEL
Jun 16, 2023
A-S Medication Solutions
DUNS: 830016429
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
sitagliptin
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (12)
Drug Labeling Information
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
JANUVIA® is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
Limitations of Use
JANUVIA should not be used in patients with type 1 diabetes.
JANUVIA has not been studied in patients with a history of pancreatitis. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using JANUVIA. [See Warnings and Precautions (5.1).]
JANUVIA is a dipeptidyl peptidase-4 (DPP-4) inhibitor indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1)
Limitations of Use:
- JANUVIA should not be used in patients with type 1 diabetes (1)
- JANUVIA has not been studied in patients with a history of pancreatitis. (1, 5.1)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Pancreatitis
There have been postmarketing reports of acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, in patients taking JANUVIA. After initiation of JANUVIA, patients should be observed carefully for signs and symptoms of pancreatitis. If pancreatitis is suspected, JANUVIA should promptly be discontinued and appropriate management should be initiated. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using JANUVIA.
5.2 Heart Failure
An association between dipeptidyl peptidase-4 (DPP-4) inhibitor treatment and heart failure has been observed in cardiovascular outcomes trials for two other members of the DPP-4 inhibitor class. These trials evaluated patients with type 2 diabetes mellitus and atherosclerotic cardiovascular disease.
Consider the risks and benefits of JANUVIA prior to initiating treatment in patients at risk for heart failure, such as those with a prior history of heart failure and a history of renal impairment, and observe these patients for signs and symptoms of heart failure during therapy. Advise patients of the characteristic symptoms of heart failure and to immediately report such symptoms. If heart failure develops, evaluate and manage according to current standards of care and consider discontinuation of JANUVIA.
5.3 Acute Renal Failure
There have been postmarketing reports of worsening renal function, including acute renal failure, sometimes requiring dialysis. A subset of these reports involved patients with renal impairment, some of whom were prescribed inappropriate doses of sitagliptin. A return to baseline levels of renal impairment has been observed with supportive treatment and discontinuation of potentially causative agents. Consideration can be given to cautiously reinitiating JANUVIA if another etiology is deemed likely to have precipitated the acute worsening of renal function.
Assessment of renal function is recommended prior to initiating JANUVIA and periodically thereafter. A dosage adjustment is recommended in patients with moderate or severe renal impairment and in patients with ESRD requiring hemodialysis or peritoneal dialysis. [See Dosage and Administration (2.2); Use in Specific Populations (8.6).]
5.4 Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues
When JANUVIA was used in combination with insulin or insulin secretagogues (e.g., sulfonylurea), medications known to cause hypoglycemia, the incidence of hypoglycemia was increased over that of placebo used in combination with a sulfonylurea or with insulin. [See Adverse Reactions (6.1).] Therefore, a lower dose of sulfonylurea or insulin may be required to reduce the risk of hypoglycemia. [See Drug Interactions (7.1).]
5.5 Hypersensitivity Reactions
There have been postmarketing reports of serious hypersensitivity reactions in patients treated with JANUVIA. These reactions include anaphylaxis, angioedema, and exfoliative skin conditions including Stevens-Johnson syndrome. Onset of these reactions occurred within the first 3 months after initiation of treatment with JANUVIA, with some reports occurring after the first dose. If a hypersensitivity reaction is suspected, discontinue JANUVIA, assess for other potential causes for the event, and institute alternative treatment for diabetes. [See Adverse Reactions (6.2).]
Angioedema has also been reported with other DPP-4 inhibitors. Use caution in a patient with a history of angioedema with another DPP-4 inhibitor because it is unknown whether such patients will be predisposed to angioedema with JANUVIA.
5.6 Severe and Disabling Arthralgia
There have been postmarketing reports of severe and disabling arthralgia in patients taking DPP-4 inhibitors. The time to onset of symptoms following initiation of drug therapy varied from one day to years. Patients experienced relief of symptoms upon discontinuation of the medication. A subset of patients experienced a recurrence of symptoms when restarting the same drug or a different DPP-4 inhibitor. Consider DPP-4 inhibitors as a possible cause for severe joint pain and discontinue drug if appropriate.
5.7 Bullous Pemphigoid
Postmarketing cases of bullous pemphigoid requiring hospitalization have been reported with DPP-4 inhibitor use. In reported cases, patients typically recovered with topical or systemic immunosuppressive treatment and discontinuation of the DPP-4 inhibitor. Tell patients to report development of blisters or erosions while receiving JANUVIA. If bullous pemphigoid is suspected, JANUVIA should be discontinued and referral to a dermatologist should be considered for diagnosis and appropriate treatment.
- Pancreatitis: There have been postmarketing reports of acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis. If pancreatitis is suspected, promptly discontinue JANUVIA. (5.1)
- Heart failure: Heart failure has been observed with two other members of the DPP-4 inhibitor class. Consider risks and benefits of JANUVIA in patients who have known risk factors for heart failure. Monitor patients for signs and symptoms. (5.2)
- Acute Renal Failure: Has been reported postmarketing, sometimes requiring dialysis. Assessment of renal function is recommended prior to initiating JANUVIA and periodically thereafter. (5.3)
- Hypoglycemia with Concomitant Use with Insulin or Insulin Secretagogues: Increased risk of hypoglycemia when used in combination with insulin and/or an insulin secretagogue. Lower dose of insulin or insulin secretagogue may be required. (5.4, 7.1)
- Hypersensitivity Reactions: There have been postmarketing reports of serious allergic and hypersensitivity reactions in patients treated with JANUVIA such as anaphylaxis, angioedema, and exfoliative skin conditions including Stevens-Johnson syndrome. Promptly stop JANUVIA, assess for other potential causes, institute appropriate monitoring and treatment. (5.5, 6.2)
- Severe and Disabling Arthralgia: Has been reported in patients taking DPP-4 inhibitors. Consider as a possible cause for severe joint pain and discontinue drug if appropriate. (5.6)
- Bullous Pemphigoid: There have been postmarketing reports requiring hospitalization in patients taking DPP-4 inhibitors. Tell patients to report development of blisters or erosions. If bullous pemphigoid is suspected, discontinue JANUVIA. (5.7)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosing
The recommended dose of JANUVIA is 100 mg once daily. JANUVIA can be taken with or without food.
2.2 Recommendations for Use in Renal Impairment
Assess renal function prior to initiation of JANUVIA and periodically thereafter.
For patients with an estimated glomerular filtration rate [eGFR] greater than or equal to 45 mL/min/1.73 m2 to less than 90 mL/min/1.73 m2, no dosage adjustment for JANUVIA is required.
For patients with moderate renal impairment (eGFR greater than or equal to 30 mL/min/1.73 m2 to less than 45 mL/min/1.73 m2), the dose of JANUVIA is 50 mg once daily.
For patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2) or with end-stage renal disease (ESRD) requiring hemodialysis or peritoneal dialysis, the dose of JANUVIA is 25 mg once daily. JANUVIA may be administered without regard to the timing of dialysis.
The recommended dose of JANUVIA is 100 mg once daily. JANUVIA can be taken with or without food. (2.1)
Dosage adjustment is recommended for patients with eGFR less than 45 mL/min/1.73 m2. (2.2)
Dosage Adjustment in Patients with Renal Impairment (2.2)|
eGFR greater than or equal to 30 mL/min/1.73 m2 to less than 45 mL/min/1.73 m2 |
eGFR less than 30 mL/min/1.73 m2 (including patients with end stage renal disease [ESRD] on dialysis) |
|
50 mg once daily |
25 mg once daily |
DESCRIPTION SECTION
11 DESCRIPTION
JANUVIA Tablets contain sitagliptin phosphate, an orally-active inhibitor of the dipeptidyl peptidase-4 (DPP-4) enzyme.
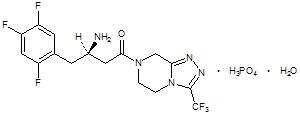
Sitagliptin phosphate monohydrate is described chemically as 7-[(3R)-3-amino-1-oxo-4-(2,4,5-trifluorophenyl)butyl]-5,6,7,8-tetrahydro-3-(trifluoromethyl)-1,2,4-triazolo[4,3-a]pyrazine phosphate (1:1) monohydrate.
The empirical formula is C16H15F6N5O•H3PO4•H2O and the molecular weight is 523.32. The structural formula is:
|
|
Sitagliptin phosphate monohydrate is a white to off-white, crystalline, non- hygroscopic powder. It is soluble in water and N,N-dimethyl formamide; slightly soluble in methanol; very slightly soluble in ethanol, acetone, and acetonitrile; and insoluble in isopropanol and isopropyl acetate.
Each film-coated tablet of JANUVIA contains 32.13, 64.25, or 128.5 mg of sitagliptin phosphate monohydrate, which is equivalent to 25, 50, or 100 mg, respectively, of free base and the following inactive ingredients: microcrystalline cellulose, anhydrous dibasic calcium phosphate, croscarmellose sodium, magnesium stearate, and sodium stearyl fumarate. In addition, the film coating contains the following inactive ingredients: polyvinyl alcohol, polyethylene glycol, talc, titanium dioxide, red iron oxide, and yellow iron oxide.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Sitagliptin is a DPP-4 inhibitor, which is believed to exert its actions in patients with type 2 diabetes mellitus by slowing the inactivation of incretin hormones. Concentrations of the active intact hormones are increased by sitagliptin, thereby increasing and prolonging the action of these hormones. Incretin hormones, including glucagon-like peptide-1 (GLP-1) and glucose- dependent insulinotropic polypeptide (GIP), are released by the intestine throughout the day, and levels are increased in response to a meal. These hormones are rapidly inactivated by the enzyme, DPP-4. The incretins are part of an endogenous system involved in the physiologic regulation of glucose homeostasis. When blood glucose concentrations are normal or elevated, GLP-1 and GIP increase insulin synthesis and release from pancreatic beta cells by intracellular signaling pathways involving cyclic AMP. GLP-1 also lowers glucagon secretion from pancreatic alpha cells, leading to reduced hepatic glucose production. By increasing and prolonging active incretin levels, sitagliptin increases insulin release and decreases glucagon levels in the circulation in a glucose-dependent manner. Sitagliptin demonstrates selectivity for DPP-4 and does not inhibit DPP-8 or DPP-9 activity in vitro at concentrations approximating those from therapeutic doses.
12.2 Pharmacodynamics
General
In patients with type 2 diabetes mellitus, administration of sitagliptin led to inhibition of DPP-4 enzyme activity for a 24-hour period. After an oral glucose load or a meal, this DPP-4 inhibition resulted in a 2- to 3-fold increase in circulating levels of active GLP-1 and GIP, decreased glucagon concentrations, and increased responsiveness of insulin release to glucose, resulting in higher C-peptide and insulin concentrations. The rise in insulin with the decrease in glucagon was associated with lower fasting glucose concentrations and reduced glucose excursion following an oral glucose load or a meal.
In studies with healthy subjects, sitagliptin did not lower blood glucose or cause hypoglycemia.
Sitagliptin and Metformin hydrochloride Coadministration
In a two-day study in healthy subjects, sitagliptin alone increased active GLP-1 concentrations, whereas metformin alone increased active and total GLP-1 concentrations to similar extents. Coadministration of sitagliptin and metformin had an additive effect on active GLP-1 concentrations. Sitagliptin, but not metformin, increased active GIP concentrations. It is unclear how these findings relate to changes in glycemic control in patients with type 2 diabetes mellitus.
Cardiac Electrophysiology
In a randomized, placebo-controlled crossover study, 79 healthy subjects were administered a single oral dose of sitagliptin 100 mg, sitagliptin 800 mg (8 times the recommended dose), and placebo. At the recommended dose of 100 mg, there was no effect on the QTc interval obtained at the peak plasma concentration, or at any other time during the study. Following the 800 mg dose, the maximum increase in the placebo-corrected mean change in QTc from baseline was observed at 3 hours postdose and was 8.0 msec. This increase is not considered to be clinically significant. At the 800 mg dose, peak sitagliptin plasma concentrations were approximately 11 times higher than the peak concentrations following a 100-mg dose.
In patients with type 2 diabetes mellitus administered sitagliptin 100 mg (N=81) or sitagliptin 200 mg (N=63) daily, there were no meaningful changes in QTc interval based on ECG data obtained at the time of expected peak plasma concentration.
12.3 Pharmacokinetics
The pharmacokinetics of sitagliptin have been extensively characterized in healthy subjects and patients with type 2 diabetes mellitus. Following a single oral 100-mg dose to healthy volunteers, mean plasma AUC of sitagliptin was 8.52 μM•hr, Cmax was 950 nM, and apparent terminal half-life (t1/2) was 12.4 hours. Plasma AUC of sitagliptin increased in a dose-proportional manner and increased approximately 14% following 100 mg doses at steady-state compared to the first dose. The intra-subject and inter-subject coefficients of variation for sitagliptin AUC were small (5.8% and 15.1%). The pharmacokinetics of sitagliptin was generally similar in healthy subjects and in patients with type 2 diabetes mellitus.
Absorption
After oral administration of a 100 mg dose to healthy subjects, sitagliptin was rapidly absorbed with peak plasma concentrations (median Tmax) occurring 1 to 4 hours postdose. The absolute bioavailability of sitagliptin is approximately 87%.
Effect of Food
Coadministration of a high-fat meal with sitagliptin had no effect on the pharmacokinetics of sitagliptin.
Distribution
The mean volume of distribution at steady state following a single 100-mg intravenous dose of sitagliptin to healthy subjects is approximately 198 liters. The fraction of sitagliptin reversibly bound to plasma proteins is low (38%).
Elimination
Approximately 79% of sitagliptin is excreted unchanged in the urine with metabolism being a minor pathway of elimination. The apparent terminal t1/2 following a 100 mg oral dose of sitagliptin was approximately 12.4 hours and renal clearance was approximately 350 mL/min.
Metabolism
Following a [14C]sitagliptin oral dose, approximately 16% of the radioactivity was excreted as metabolites of sitagliptin. Six metabolites were detected at trace levels and are not expected to contribute to the plasma DPP-4 inhibitory activity of sitagliptin. In vitro studies indicated that the primary enzyme responsible for the limited metabolism of sitagliptin was CYP3A4, with contribution from CYP2C8.
Excretion
Following administration of an oral [14C]sitagliptin dose to healthy subjects, approximately 100% of the administered radioactivity was eliminated in feces (13%) or urine (87%) within one week of dosing.
Elimination of sitagliptin occurs primarily via renal excretion and involves active tubular secretion. Sitagliptin is a substrate for human organic anion transporter-3 (hOAT-3), which may be involved in the renal elimination of sitagliptin. The clinical relevance of hOAT-3 in sitagliptin transport has not been established. Sitagliptin is also a substrate of P-glycoprotein (P-gp), which may also be involved in mediating the renal elimination of sitagliptin. However, cyclosporine, a P-gp inhibitor, did not reduce the renal clearance of sitagliptin.
Specific Populations
Patients with Renal Impairment
An approximately 2-fold increase in the plasma AUC of sitagliptin was observed in patients with moderate renal impairment with eGFR of 30 to less than 45 mL/min/1.73 m2, and an approximately 4-fold increase was observed in patients with severe renal impairment, including patients with ESRD on hemodialysis, as compared to normal healthy control subjects.
Patients with Hepatic Impairment
In patients with moderate hepatic impairment (Child-Pugh score 7 to 9), mean AUC and Cmax of sitagliptin increased approximately 21% and 13%, respectively, compared to healthy matched controls following administration of a single 100-mg dose of sitagliptin. These differences are not considered to be clinically meaningful.
There is no clinical experience in patients with severe hepatic impairment (Child-Pugh score >9).
Effects of Age, Body Mass Index (BMI), Gender, and Race
Based on a population pharmacokinetic analysis or a composite analysis of available pharmacokinetic data, BMI, gender, and race do not have a clinically meaningful effect on the pharmacokinetics of sitagliptin. When the effects of age on renal function are taken into account, age alone did not have a clinically meaningful impact on the pharmacokinetics of sitagliptin based on a population pharmacokinetic analysis. Elderly subjects (65 to 80 years) had approximately 19% higher plasma concentrations of sitagliptin compared to younger subjects.
Drug Interaction Studies
In Vitro Assessment of Drug Interactions
Sitagliptin is not an inhibitor of CYP isozymes CYP3A4, 2C8, 2C9, 2D6, 1A2, 2C19 or 2B6, and is not an inducer of CYP3A4. Sitagliptin is a P-gp substrate, but does not inhibit P-gp mediated transport of digoxin. Based on these results, sitagliptin is considered unlikely to cause interactions with other drugs that utilize these pathways.
Sitagliptin is not extensively bound to plasma proteins. Therefore, the propensity of sitagliptin to be involved in clinically meaningful drug-drug interactions mediated by plasma protein binding displacement is very low.
In Vivo Assessment of Drug Interactions
Effects of Sitagliptin on Other Drugs
In clinical studies, sitagliptin did not meaningfully alter the pharmacokinetics of metformin, glyburide, simvastatin, rosiglitazone, digoxin, warfarin, or an oral contraceptive (ethinyl estradiol and norethindrone) (Table 4), providing in vivo evidence of a low propensity for causing drug interactions with substrates of CYP3A4, CYP2C8, CYP2C9, P-gp, and organic cationic transporter (OCT).
Table 4: Effect of Sitagliptin on Systemic Exposure of Coadministered Drugs|
Coadministered Drug |
Dose of Coadministered Drug* |
Dose of Sitagliptin* |
Geometric Mean Ratio | ||
|---|---|---|---|---|---|
|
AUC† |
Cmax | ||||
| |||||
|
Digoxin |
0.25 mg‡ once daily for 10 days |
100 mg‡ once daily for 10 days |
Digoxin |
1.11§ |
1.18 |
|
Glyburide |
1.25 mg |
200 mg‡ once daily for 6 days |
Glyburide |
1.09 |
1.01 |
|
Simvastatin |
20 mg |
200 mg‡ once daily for 5 days |
Simvastatin |
0.85¶ |
0.80 |
|
Simvastatin Acid |
1.12¶ |
1.06 | |||
|
Rosiglitazone |
4 mg |
200 mg‡ once daily for 5 days |
Rosiglitazone |
0.98 |
0.99 |
|
Warfarin |
30 mg single dose on day 5 |
200 mg‡ once daily for 11 days |
S(-) Warfarin |
0.95 |
0.89 |
|
R(+) Warfarin |
0.99 |
0.89 | |||
|
Ethinyl estradiol and norethindrone |
21 days once daily of 35 µg ethinyl estradiol with norethindrone 0.5 mg × 7 days, 0.75 mg × 7 days, 1.0 mg × 7 days |
200 mg‡ once daily for 21 days |
Ethinyl estradiol |
0.99 |
0.97 |
|
Norethindrone |
1.03 |
0.98 | |||
|
Metformin HCl |
1000 mg‡ twice daily for 14 days |
50 mg‡ twice daily for 7 days |
Metformin |
1.02# |
0.97 |
Effects of Other Drugs on Sitagliptin
Clinical data described below suggest that sitagliptin is not susceptible to clinically meaningful interactions by coadministered medications (Table 5).
Table 5: Effect of Coadministered Drugs on Systemic Exposure of Sitagliptin|
Coadministered Drug |
Dose of Coadministered Drug* |
Dose of Sitagliptin* |
Geometric Mean Ratio | ||
|---|---|---|---|---|---|
|
AUC† |
Cmax | ||||
| |||||
|
Cyclosporine |
600 mg once daily |
100 mg once daily |
Sitagliptin |
1.29 |
1.68 |
|
Metformin HCl |
1000 mg‡ twice daily for 14 days |
50 mg‡ twice daily for 7 days |
Sitagliptin |
1.02§ |
1.05 |
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A two-year carcinogenicity study was conducted in male and female rats given oral doses of sitagliptin of 50, 150, and 500 mg/kg/day. There was an increased incidence of combined liver adenoma/carcinoma in males and females and of liver carcinoma in females at 500 mg/kg. This dose results in exposures approximately 60 times the human exposure at the maximum recommended daily adult human dose (MRHD) of 100 mg/day based on AUC comparisons. Liver tumors were not observed at 150 mg/kg, approximately 20 times the human exposure at the MRHD. A two-year carcinogenicity study was conducted in male and female mice given oral doses of sitagliptin of 50, 125, 250, and 500 mg/kg/day. There was no increase in the incidence of tumors in any organ up to 500 mg/kg, approximately 70 times human exposure at the MRHD. Sitagliptin was not mutagenic or clastogenic with or without metabolic activation in the Ames bacterial mutagenicity assay, a Chinese hamster ovary (CHO) chromosome aberration assay, an in vitro cytogenetics assay in CHO, an in vitro rat hepatocyte DNA alkaline elution assay, and an in vivo micronucleus assay.
In rat fertility studies with oral gavage doses of 125, 250, and 1000 mg/kg, males were treated for 4 weeks prior to mating, during mating, up to scheduled termination (approximately 8 weeks total) and females were treated 2 weeks prior to mating through gestation day 7. No adverse effect on fertility was observed at 125 mg/kg (approximately 12 times human exposure at the MRHD of 100 mg/day based on AUC comparisons). At higher doses, nondose-related increased resorptions in females were observed (approximately 25 and 100 times human exposure at the MRHD based on AUC comparison).
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
There were approximately 5200 patients with type 2 diabetes randomized in nine double-blind, placebo-controlled clinical safety and efficacy studies conducted to evaluate the effects of sitagliptin on glycemic control. In a pooled analysis of seven of these studies, the ethnic/racial distribution was approximately 59% white, 20% Hispanic, 10% Asian, 6% black, and 6% other groups. Patients had an overall mean age of approximately 55 years (range 18 to 87 years). In addition, an active (glipizide)-controlled study of 52-weeks duration was conducted in 1172 patients with type 2 diabetes who had inadequate glycemic control on metformin.
In patients with type 2 diabetes, treatment with JANUVIA produced clinically significant improvements in hemoglobin A1C, fasting plasma glucose (FPG) and 2-hour post-prandial glucose (PPG) compared to placebo.
14.1 Monotherapy
A total of 1262 patients with type 2 diabetes participated in two double- blind, placebo-controlled studies, one of 18-week and another of 24-week duration, to evaluate the efficacy and safety of JANUVIA monotherapy. In both monotherapy studies, patients currently on an antihyperglycemic agent discontinued the agent, and underwent a diet, exercise, and drug washout period of about 7 weeks. Patients with inadequate glycemic control (A1C 7% to 10%) after the washout period were randomized after completing a 2-week single-blind placebo run-in period; patients not currently on antihyperglycemic agents (off therapy for at least 8 weeks) with inadequate glycemic control (A1C 7% to 10%) were randomized after completing the 2-week single-blind placebo run-in period. In the 18-week study, 521 patients were randomized to placebo, JANUVIA 100 mg, or JANUVIA 200 mg, and in the 24-week study 741 patients were randomized to placebo, JANUVIA 100 mg, or JANUVIA 200 mg. Patients who failed to meet specific glycemic goals during the studies were treated with metformin rescue, added on to placebo or JANUVIA.
Treatment with JANUVIA at 100 mg daily provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo (Table 6). In the 18-week study, 9% of patients receiving JANUVIA 100 mg and 17% who received placebo required rescue therapy. In the 24-week study, 9% of patients receiving JANUVIA 100 mg and 21% of patients receiving placebo required rescue therapy. The improvement in A1C compared to placebo was not affected by gender, age, race, prior antihyperglycemic therapy, or baseline BMI. As is typical for trials of agents to treat type 2 diabetes, the mean reduction in A1C with JANUVIA appears to be related to the degree of A1C elevation at baseline. In these 18- and 24-week studies, among patients who were not on an antihyperglycemic agent at study entry, the reductions from baseline in A1C were -0.7% and -0.8%, respectively, for those given JANUVIA, and -0.1% and -0.2%, respectively, for those given placebo. Overall, the 200 mg daily dose did not provide greater glycemic efficacy than the 100 mg daily dose. The effect of JANUVIA on lipid endpoints was similar to placebo. Body weight did not increase from baseline with JANUVIA therapy in either study, compared to a small reduction in patients given placebo.
Table 6: Glycemic Parameters in 18- and 24-Week Placebo-Controlled Studies of JANUVIA in Patients with Type 2 Diabetes*|
18-Week Study |
24-Week Study | |||
|
JANUVIA 100 mg |
Placebo |
JANUVIA 100 mg |
Placebo | |
| ||||
|
A1C (%) |
N = 193 |
N = 103 |
N = 229 |
N = 244 |
|
Baseline (mean) |
8.0 |
8.1 |
8.0 |
8.0 |
|
Change from baseline (adjusted mean†) |
-0.5 |
0.1 |
-0.6 |
0.2 |
|
Difference from placebo (adjusted mean†) |
-0.6‡ |
-0.8‡ | ||
|
Patients (%) achieving A1C <7% |
69 (36%) |
16 (16%) |
93 (41%) |
41 (17%) |
|
FPG (mg/dL) |
N = 201 |
N = 107 |
N = 234 |
N = 247 |
|
Baseline (mean) |
180 |
184 |
170 |
176 |
|
Change from baseline (adjusted mean†) |
-13 |
7 |
-12 |
5 |
|
Difference from placebo (adjusted mean†) |
-20‡ |
-17‡ | ||
|
2-hour PPG (mg/dL) |
§ |
§ |
N = 201 |
N = 204 |
|
Baseline (mean) |
257 |
271 | ||
|
Change from baseline (adjusted mean†) |
-49 |
-2 | ||
|
Difference from placebo (adjusted mean†) |
-47‡ |
Additional Monotherapy Study
A multinational, randomized, double-blind, placebo-controlled study was also conducted to assess the safety and tolerability of JANUVIA in 91 patients with type 2 diabetes and chronic renal insufficiency (creatinine clearance <50 mL/min). Patients with moderate renal insufficiency received 50 mg daily of JANUVIA and those with severe renal insufficiency or with ESRD on hemodialysis or peritoneal dialysis received 25 mg daily. In this study, the safety and tolerability of JANUVIA were generally similar to placebo. A small increase in serum creatinine was reported in patients with moderate renal insufficiency treated with JANUVIA relative to those on placebo. In addition, the reductions in A1C and FPG with JANUVIA compared to placebo were generally similar to those observed in other monotherapy studies. [See Clinical Pharmacology (12.3).]
14.2 Combination Therapy
Add-on Combination Therapy with Metformin
A total of 701 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of JANUVIA in combination with metformin. Patients already on metformin HCl (N=431) at a dose of at least 1500 mg per day were randomized after completing a 2-week single-blind placebo run-in period. Patients on metformin and another antihyperglycemic agent (N=229) and patients not on any antihyperglycemic agents (off therapy for at least 8 weeks, N=41) were randomized after a run-in period of approximately 10 weeks on metformin HCl (at a dose of at least 1500 mg per day) in monotherapy. Patients with inadequate glycemic control (A1C 7% to 10%) were randomized to the addition of either 100 mg of JANUVIA or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with pioglitazone rescue.
In combination with metformin, JANUVIA provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo with metformin (Table 7). Rescue glycemic therapy was used in 5% of patients treated with JANUVIA 100 mg and 14% of patients treated with placebo. A similar decrease in body weight was observed for both treatment groups.
Table 7: Glycemic Parameters at Final Visit (24-Week Study) for JANUVIA in Add-on Combination Therapy with Metformin*|
JANUVIA 100 mg + Metformin |
Placebo + Metformin | |
| ||
|
A1C (%) |
N = 453 |
N = 224 |
|
Baseline (mean) |
8.0 |
8.0 |
|
Change from baseline (adjusted mean†) |
-0.7 |
-0.0 |
|
Difference from placebo + metformin (adjusted mean†) |
-0.7‡ | |
|
Patients (%) achieving A1C <7% |
213 (47%) |
41 (18%) |
|
FPG (mg/dL) |
N = 454 |
N = 226 |
|
Baseline (mean) |
170 |
174 |
|
Change from baseline (adjusted mean†) |
-17 |
9 |
|
Difference from placebo + metformin (adjusted mean†) |
-25‡ | |
|
2-hour PPG (mg/dL) |
N = 387 |
N = 182 |
|
Baseline (mean) |
275 |
272 |
|
Change from baseline (adjusted mean†) |
-62 |
-11 |
|
Difference from placebo + metformin (adjusted mean†) |
-51‡ |
Initial Combination Therapy with Metformin
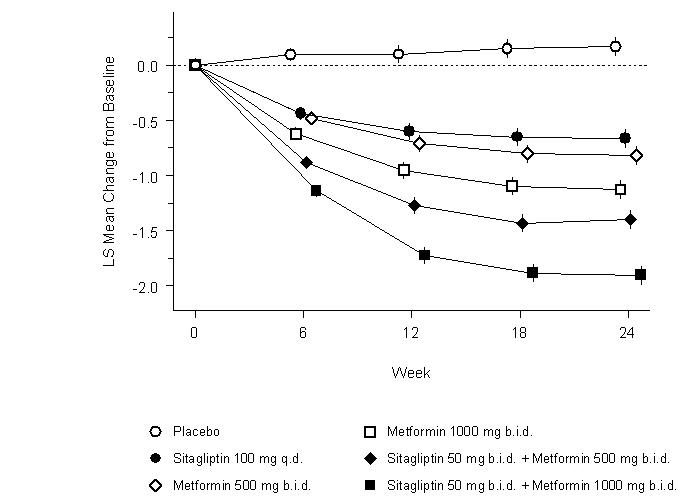
A total of 1091 patients with type 2 diabetes and inadequate glycemic control on diet and exercise participated in a 24-week, randomized, double-blind, placebo-controlled factorial study designed to assess the efficacy of sitagliptin as initial therapy in combination with metformin. Patients on an antihyperglycemic agent (N=541) discontinued the agent, and underwent a diet, exercise, and drug washout period of up to 12 weeks duration. After the washout period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized after completing a 2-week single-blind placebo run-in period. Patients not on antihyperglycemic agents at study entry (N=550) with inadequate glycemic control (A1C 7.5% to 11%) immediately entered the 2-week single-blind placebo run-in period and then were randomized. Approximately equal numbers of patients were randomized to receive initial therapy with placebo, 100 mg of JANUVIA once daily, 500 mg or 1000 mg of metformin HCl twice daily, or 50 mg of sitagliptin twice daily in combination with 500 mg or 1000 mg of metformin HCl twice daily. Patients who failed to meet specific glycemic goals during the study were treated with glyburide (glibenclamide) rescue.
Initial therapy with the combination of JANUVIA and metformin provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo, to metformin alone, and to JANUVIA alone (Table 8, Figure 1). Mean reductions from baseline in A1C were generally greater for patients with higher baseline A1C values. For patients not on an antihyperglycemic agent at study entry, mean reductions from baseline in A1C were: JANUVIA 100 mg once daily, -1.1%; metformin HCl 500 mg bid, -1.1%; metformin HCl 1000 mg bid, -1.2%; sitagliptin 50 mg bid with metformin HCl 500 mg bid, -1.6%; sitagliptin 50 mg bid with metformin HCl 1000 mg bid, -1.9%; and for patients receiving placebo, -0.2%. Lipid effects were generally neutral. The decrease in body weight in the groups given sitagliptin in combination with metformin was similar to that in the groups given metformin alone or placebo.
Table 8: Glycemic Parameters at Final Visit (24-Week Study) for Sitagliptin and Metformin, Alone and in Combination as Initial Therapy*|
Placebo |
Sitagliptin (JANUVIA) 100 mg QD |
Metformin |
Metformin |
Sitagliptin |
Sitagliptin | |
| ||||||
|
A1C (%) |
N = 165 |
N = 175 |
N = 178 |
N = 177 |
N = 183 |
N = 178 |
|
Baseline (mean) |
8.7 |
8.9 |
8.9 |
8.7 |
8.8 |
8.8 |
|
Change from baseline (adjusted mean†) |
0.2 |
-0.7 |
-0.8 |
-1.1 |
-1.4 |
-1.9 |
|
Difference from placebo (adjusted mean†) (95% CI) |
-0.8‡ |
-1.0‡ |
-1.3‡ |
-1.6‡ |
-2.1‡ | |
|
Patients (%) achieving A1C <7% |
15 (9%) |
35 (20%) |
41 (23%) |
68 (38%) |
79 (43%) |
118 (66%) |
|
% Patients receiving rescue medication |
32 |
21 |
17 |
12 |
8 |
2 |
|
FPG (mg/dL) |
N = 169 |
N = 178 |
N = 179 |
N = 179 |
N = 183 |
N = 180 |
|
Baseline (mean) |
196 |
201 |
205 |
197 |
204 |
197 |
|
Change from baseline (adjusted mean†) |
6 |
-17 |
-27 |
-29 |
-47 |
-64 |
|
Difference from placebo (adjusted mean†) (95% CI) |
-23‡ |
-33‡ |
-35‡ |
-53‡ |
-70‡ | |
|
2-hour PPG (mg/dL) |
N = 129 |
N = 136 |
N = 141 |
N = 138 |
N = 147 |
N = 152 |
|
Baseline (mean) |
277 |
285 |
293 |
283 |
292 |
287 |
|
Change from baseline (adjusted mean†) |
0 |
-52 |
-53 |
-78 |
-93 |
-117 |
|
Difference from placebo (adjusted mean†) (95% CI) |
-52‡ |
-54‡ |
-78‡ |
-93‡ |
-117‡ |
|
|
|
Initial combination therapy or maintenance of combination therapy may not be appropriate for all patients. These management options are left to the discretion of the health care provider.
Active-Controlled Study vs Glipizide in Combination with Metformin
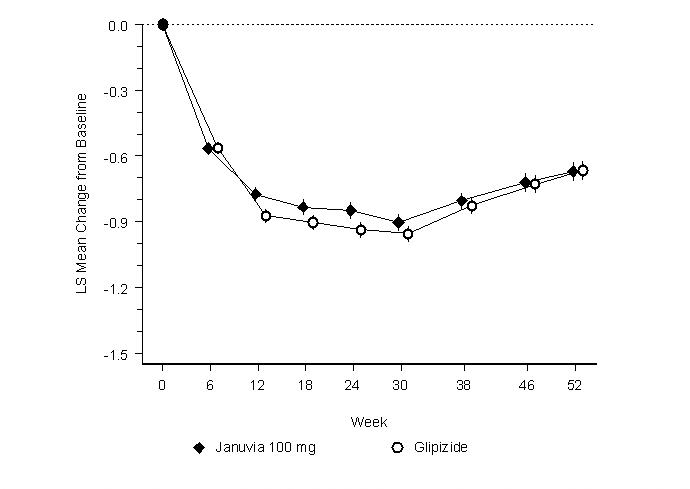
The efficacy of JANUVIA was evaluated in a 52-week, double-blind, glipizide- controlled noninferiority trial in patients with type 2 diabetes. Patients not on treatment or on other antihyperglycemic agents entered a run-in treatment period of up to 12 weeks duration with metformin HCl monotherapy (dose of ≥1500 mg per day) which included washout of medications other than metformin, if applicable. After the run-in period, those with inadequate glycemic control (A1C 6.5% to 10%) were randomized 1:1 to the addition of JANUVIA 100 mg once daily or glipizide for 52 weeks. Patients receiving glipizide were given an initial dosage of 5 mg/day and then electively titrated over the next 18 weeks to a maximum dosage of 20 mg/day as needed to optimize glycemic control. Thereafter, the glipizide dose was to be kept constant, except for down- titration to prevent hypoglycemia. The mean dose of glipizide after the titration period was 10 mg.
After 52 weeks, JANUVIA and glipizide had similar mean reductions from baseline in A1C in the intent-to-treat analysis (Table 9). These results were consistent with the per protocol analysis (Figure 2). A conclusion in favor of the non-inferiority of JANUVIA to glipizide may be limited to patients with baseline A1C comparable to those included in the study (over 70% of patients had baseline A1C <8% and over 90% had A1C <9%).
Table 9: Glycemic Parameters in a 52-Week Study Comparing JANUVIA to Glipizide as Add-On Therapy in Patients Inadequately Controlled on Metformin (Intent-to-Treat Population)*|
JANUVIA 100 mg |
Glipizide | |
| ||
|
A1C (%) |
N = 576 |
N = 559 |
|
Baseline (mean) |
7.7 |
7.6 |
|
Change from baseline (adjusted mean†) |
-0.5 |
-0.6 |
|
FPG (mg/dL) |
N = 583 |
N = 568 |
|
Baseline (mean) |
166 |
164 |
|
Change from baseline (adjusted mean†) |
-8 |
-8 |
|
|
|
The incidence of hypoglycemia in the JANUVIA group (4.9%) was significantly (p<0.001) lower than that in the glipizide group (32.0%). Patients treated with JANUVIA exhibited a significant mean decrease from baseline in body weight compared to a significant weight gain in patients administered glipizide (-1.5 kg vs +1.1 kg).
Add-on Combination Therapy with Pioglitazone
A total of 353 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of JANUVIA in combination with pioglitazone. Patients on any oral antihyperglycemic agent in monotherapy (N=212) or on a PPARγ agent in combination therapy (N=106) or not on an antihyperglycemic agent (off therapy for at least 8 weeks, N=34) were switched to monotherapy with pioglitazone (at a dose of 30-45 mg per day), and completed a run-in period of approximately 12 weeks in duration. After the run-in period on pioglitazone monotherapy, patients with inadequate glycemic control (A1C 7% to 10%) were randomized to the addition of either 100 mg of JANUVIA or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with metformin rescue. Glycemic endpoints measured were A1C and fasting glucose.
In combination with pioglitazone, JANUVIA provided significant improvements in A1C and FPG compared to placebo with pioglitazone (Table 10). Rescue therapy was used in 7% of patients treated with JANUVIA 100 mg and 14% of patients treated with placebo. There was no significant difference between JANUVIA and placebo in body weight change.
Table 10: Glycemic Parameters at Final Visit (24-Week Study) for JANUVIA in Add-on Combination Therapy with Pioglitazone*|
JANUVIA 100 mg + Pioglitazone |
Placebo + Pioglitazone | |
| ||
|
A1C (%) |
N = 163 |
N = 174 |
|
Baseline (mean) |
8.1 |
8.0 |
|
Change from baseline (adjusted mean†) |
-0.9 |
-0.2 |
|
Difference from placebo + pioglitazone (adjusted mean†) |
-0.7‡ | |
|
Patients (%) achieving A1C <7% |
74 (45%) |
40 (23%) |
|
FPG (mg/dL) |
N = 163 |
N = 174 |
|
Baseline (mean) |
168 |
166 |
|
Change from baseline (adjusted mean†) |
-17 |
1 |
|
Difference from placebo + pioglitazone (adjusted mean†) |
-18‡ |
Initial Combination Therapy with Pioglitazone
A total of 520 patients with type 2 diabetes and inadequate glycemic control on diet and exercise participated in a 24-week, randomized, double-blind study designed to assess the efficacy of JANUVIA as initial therapy in combination with pioglitazone. Patients not on antihyperglycemic agents at study entry (<4 weeks cumulative therapy over the past 2 years, and with no treatment over the prior 4 months) with inadequate glycemic control (A1C 8% to 12%) immediately entered the 2-week single-blind placebo run-in period and then were randomized. Approximately equal numbers of patients were randomized to receive initial therapy with 100 mg of JANUVIA in combination with 30 mg of pioglitazone once daily or 30 mg of pioglitazone once daily as monotherapy. There was no glycemic rescue therapy in this study.
Initial therapy with the combination of JANUVIA and pioglitazone provided significant improvements in A1C, FPG, and 2-hour PPG compared to pioglitazone monotherapy (Table 11). The improvement in A1C was generally consistent across subgroups defined by gender, age, race, baseline BMI, baseline A1C, or duration of disease. In this study, patients treated with JANUVIA in combination with pioglitazone had a mean increase in body weight of 1.1 kg compared to pioglitazone alone (3.0 kg vs. 1.9 kg). Lipid effects were generally neutral.
Table 11: Glycemic Parameters at Final Visit (24-Week Study) for JANUVIA in Combination with Pioglitazone as Initial Therapy*|
JANUVIA 100 mg + Pioglitazone |
Pioglitazone | |
| ||
|
A1C (%) |
N = 251 |
N = 246 |
|
Baseline (mean) |
9.5 |
9.4 |
|
Change from baseline (adjusted mean†) |
-2.4 |
-1.5 |
|
Difference from pioglitazone (adjusted mean†) (95% CI) |
-0.9‡ | |
|
Patients (%) achieving A1C <7% |
151 (60%) |
68 (28%) |
|
FPG (mg/dL) |
N = 256 |
N = 253 |
|
Baseline (mean) |
203 |
201 |
|
Change from baseline (adjusted mean†) |
-63 |
-40 |
|
Difference from pioglitazone (adjusted mean†) (95% CI) |
-23‡ | |
|
2-hour PPG (mg/dL) |
N = 216 |
N = 211 |
|
Baseline (mean) |
283 |
284 |
|
Change from baseline (adjusted mean†) |
-114 |
-69 |
|
Difference from pioglitazone (adjusted mean†) (95% CI) |
-45‡ |
Add-on Combination Therapy with Metformin and Rosiglitazone
A total of 278 patients with type 2 diabetes participated in a 54-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of JANUVIA in combination with metformin and rosiglitazone. Patients on dual therapy with metformin HCl ≥1500 mg/day and rosiglitazone ≥4 mg/day or with metformin HCl ≥1500 mg/day and pioglitazone ≥30 mg/day (switched to rosiglitazone ≥4 mg/day) entered a dose-stable run-in period of 6 weeks. Patients on other dual therapy were switched to metformin HCl ≥1500 mg/day and rosiglitazone ≥4 mg/day in a dose titration/stabilization run-in period of up to 20 weeks in duration. After the run-in period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized 2:1 to the addition of either 100 mg of JANUVIA or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the study were treated with glipizide (or other sulfonylurea) rescue. The primary time point for evaluation of glycemic parameters was Week 18.
In combination with metformin and rosiglitazone, JANUVIA provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo with metformin and rosiglitazone (Table 12) at Week 18. At Week 54, mean reduction in A1C was -1.0% for patients treated with JANUVIA and -0.3% for patients treated with placebo in an analysis based on the intent-to-treat population. Rescue therapy was used in 18% of patients treated with JANUVIA 100 mg and 40% of patients treated with placebo. There was no significant difference between JANUVIA and placebo in body weight change.
Table 12: Glycemic Parameters at Week 18 for JANUVIA in Add-on Combination Therapy with Metformin and Rosiglitazone*|
JANUVIA 100 mg + Metformin + Rosiglitazone |
Placebo + Metformin + Rosiglitazone | |
| ||
|
A1C (%) |
N = 176 |
N = 93 |
|
Baseline (mean) |
8.8 |
8.7 |
|
Change from baseline (adjusted mean†) |
-1.0 |
-0.4 |
|
Difference from placebo + rosiglitazone + metformin (adjusted mean†) (95% CI) |
-0.7‡ | |
|
Patients (%) achieving A1C <7% |
39 (22%) |
9 (10%) |
|
FPG (mg/dL) |
N = 179 |
N = 94 |
|
Baseline (mean) |
181 |
182 |
|
Change from baseline (adjusted mean†) |
-30 |
-11 |
|
Difference from placebo + rosiglitazone + metformin (adjusted mean†) (95% CI) |
-18‡ | |
|
2-hour PPG (mg/dL) |
N = 152 |
N = 80 |
|
Baseline (mean) |
256 |
248 |
|
Change from baseline (adjusted mean†) |
-59 |
-21 |
|
Difference from placebo + rosiglitazone + metformin (adjusted mean†) (95% CI) |
-39‡ |
Add-on Combination Therapy with Glimepiride, with or without Metformin
A total of 441 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of JANUVIA in combination with glimepiride, with or without metformin. Patients entered a run-in treatment period on glimepiride (≥4 mg per day) alone or glimepiride in combination with metformin HCl (≥1500 mg per day). After a dose-titration and dose-stable run-in period of up to 16 weeks and a 2-week placebo run-in period, patients with inadequate glycemic control (A1C 7.5% to 10.5%) were randomized to the addition of either 100 mg of JANUVIA or placebo, administered once daily. Patients who failed to meet specific glycemic goals during the studies were treated with pioglitazone rescue.
In combination with glimepiride, with or without metformin, JANUVIA provided significant improvements in A1C and FPG compared to placebo (Table 13). In the entire study population (patients on JANUVIA in combination with glimepiride and patients on JANUVIA in combination with glimepiride and metformin), a mean reduction from baseline relative to placebo in A1C of -0.7% and in FPG of -20 mg/dL was seen. Rescue therapy was used in 12% of patients treated with JANUVIA 100 mg and 27% of patients treated with placebo. In this study, patients treated with JANUVIA had a mean increase in body weight of 1.1 kg vs. placebo (+0.8 kg vs. -0.4 kg). In addition, there was an increased rate of hypoglycemia. [See Warnings and Precautions (5.4); Adverse Reactions (6.1).]
Table 13: Glycemic Parameters at Final Visit (24-Week Study) for JANUVIA as Add-On Combination Therapy with Glimepiride, with or without Metformin*|
JANUVIA 100 mg |
Placebo + |
JANUVIA 100 mg |
Placebo | |
| ||||
|
A1C (%) |
N = 102 |
N = 103 |
N = 115 |
N = 105 |
|
Baseline (mean) |
8.4 |
8.5 |
8.3 |
8.3 |
|
Change from baseline (adjusted mean†) |
-0.3 |
0.3 |
-0.6 |
0.3 |
|
Difference from placebo (adjusted mean†) |
-0.6‡ |
-0.9‡ | ||
|
Patients (%) achieving A1C <7% |
11 (11%) |
9 (9%) |
26 (23%) |
1 (1%) |
|
FPG (mg/dL) |
N = 104 |
N = 104 |
N = 115 |
N = 109 |
|
Baseline (mean) |
183 |
185 |
179 |
179 |
|
Change from baseline (adjusted mean†) |
-1 |
18 |
-8 |
13 |
|
Difference from placebo (adjusted mean†) |
-19§ |
-21‡ |
Add-on Combination Therapy with Insulin (with or without Metformin)
A total of 641 patients with type 2 diabetes participated in a 24-week, randomized, double-blind, placebo-controlled study designed to assess the efficacy of JANUVIA as add-on to insulin therapy (with or without metformin). The racial distribution in this study was approximately 70% white, 18% Asian, 7% black, and 5% other groups. Approximately 14% of the patients in this study were Hispanic. Patients entered a 2-week, single-blind run-in treatment period on pre-mixed, long-acting, or intermediate-acting insulin, with or without metformin HCl (≥1500 mg per day). Patients using short-acting insulins were excluded unless the short-acting insulin was administered as part of a pre- mixed insulin. After the run-in period, patients with inadequate glycemic control (A1C 7.5% to 11%) were randomized to the addition of either 100 mg of JANUVIA or placebo, administered once daily. Patients were on a stable dose of insulin prior to enrollment with no changes in insulin dose permitted during the run-in period. Patients who failed to meet specific glycemic goals during the double-blind treatment period were to have uptitration of the background insulin dose as rescue therapy.
The median daily insulin dose at baseline was 42 units in the patients treated with JANUVIA and 45 units in the placebo-treated patients. The median change from baseline in daily dose of insulin was zero for both groups at the end of the study. In combination with insulin (with or without metformin), JANUVIA provided significant improvements in A1C, FPG, and 2-hour PPG compared to placebo (Table 14). Both treatment groups had an adjusted mean increase in body weight of 0.1 kg from baseline to Week 24. There was an increased rate of hypoglycemia in patients treated with JANUVIA. [See Warnings and Precautions (5.4); Adverse Reactions (6.1).]
Table 14: Glycemic Parameters at Final Visit (24-Week Study) for JANUVIA as Add-on Combination Therapy with Insulin*|
JANUVIA 100 mg + Insulin (+/- Metformin) |
Placebo + Insulin (+/- Metformin) | |
| ||
|
A1C (%) |
N = 305 |
N = 312 |
|
Baseline (mean) |
8.7 |
8.6 |
|
Change from baseline (adjusted mean†) |
-0.6 |
-0.1 |
|
Difference from placebo (adjusted mean†,‡) (95% CI) |
-0.6§ (-0.7, -0.4) | |
|
Patients (%) achieving A1C <7% |
39 (12.8%) |
16 (5.1%) |
|
FPG (mg/dL) |
N = 310 |
N = 313 |
|
Baseline (mean) |
176 |
179 |
|
Change from baseline (adjusted mean†) |
-18 |
-4 |
|
Difference from placebo (adjusted mean†) (95% CI) |
-15§ (-23, -7) | |
|
2-hour PPG (mg/dL) |
N = 240 |
N = 257 |
|
Baseline (mean) |
291 |
292 |
|
Change from baseline (adjusted mean†) |
-31 |
5 |
|
Difference from placebo (adjusted mean†) (95% CI) |
-36§ (-47, -25) |
Maintenance of JANUVIA During Initiation and Titration of Insulin Glargine
A total of 746 patients with type 2 diabetes (mean baseline HbA1C 8.8%, disease duration 10.8 years) participated in a 30-week, randomized, double- blind, placebo-controlled study to assess the efficacy and safety of continuing JANUVIA during the initiation and uptitration of insulin glargine. Patients who were on a stable dose of metformin HCl (≥1500 mg/day) in combination with a DPP-4 inhibitor and/or sulfonylurea but with inadequate glycemic control (A1C 7.5% to 11%) were enrolled in the study. Those on metformin and JANUVIA (100 mg/day) directly entered the double-blind treatment period; those on another DPP-4 inhibitor and/or on a sulfonylurea entered a 4-8 week run-in period in which they were maintained on metformin and switched to JANUVIA (100 mg); other DPP-4 inhibitors and sulfonylureas were discontinued. At randomization patients were randomized either to continue JANUVIA or to discontinue JANUVIA and switch to a matching placebo. On the day of randomization, insulin glargine was initiated at a dose of 10 units subcutaneously in the evening. Patients were instructed to uptitrate their insulin dose in the evening based on fasting blood glucose measurements to achieve a target of 72-100 mg/dL.
At 30 weeks, the mean reduction in A1C was greater in the sitagliptin group than in the placebo group (Table 15). At the end of the trial, 27.3% of patients in the sitagliptin group and 27.3% in the placebo group had a fasting plasma glucose (FPG) in the target range; there was no significant difference in insulin dose between arms.
Table 15: Change from Baseline in A1C and FPG at Week 30 in the Maintenance of JANUVIA During Initiation and Titration of Insulin Glargine Study|
Sitagliptin 100 mg |
Placebo | |
|---|---|---|
| ||
|
A1C (%) |
N = 373* |
N = 370* |
|
Baseline (mean) |
8.8 |
8.8 |
|
Week 30 (mean) |
6.9 |
7.3 |
|
Change from baseline (adjusted mean)† |
-1.9 |
-1.4 |
|
Difference from placebo (adjusted mean) (95% CI)† |
-0.4 (-0.6, -0.3)‡ | |
|
Patients (%) with A1C <7% |
202 (54.2%) |
131 (35.4%) |
|
FPG (mg/dL) |
N = 373* |
N = 370* |
|
Baseline (mean) |
199 |
201 |
|
Week 30 (mean) |
118 |
123 |
|
Change from baseline (adjusted mean)† |
-81 |
-76 |
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Pancreatitis
Inform patients that acute pancreatitis has been reported during postmarketing use of JANUVIA. Inform patients that persistent severe abdominal pain, sometimes radiating to the back, which may or may not be accompanied by vomiting, is the hallmark symptom of acute pancreatitis. Instruct patients to promptly discontinue JANUVIA and contact their physician if persistent severe abdominal pain occurs [see Warnings and Precautions (5.1)].
Heart Failure
Inform patients of the signs and symptoms of heart failure. Before initiating JANUVIA, ask patients about a history of heart failure or other risk factors for heart failure including moderate to severe renal impairment. Instruct patients to contact their health care provider as soon as possible if they experience symptoms of heart failure, including increasing shortness of breath, rapid increase in weight or swelling of the feet [see Warnings and Precautions (5.2)].
Hypoglycemia
Inform patients that the incidence of hypoglycemia is increased when JANUVIA is added to a sulfonylurea or insulin. Explain to patients receiving JANUVIA in combination with these medications the risks of hypoglycemia, its symptoms and treatment, and conditions that predispose to its development [see Warnings and Precautions (5.4)].
Hypersensitivity Reactions
Inform patients that allergic reactions have been reported during postmarketing use of JANUVIA. If symptoms of allergic reactions (including rash, hives, and swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing) occur, patients must stop taking JANUVIA and seek medical advice promptly [see Warnings and Precautions (5.5)].
Severe and Disabling Arthralgia
Inform patients that severe and disabling joint pain may occur with this class of drugs. The time to onset of symptoms can range from one day to years. Instruct patients to seek medical advice if severe joint pain occurs [see Warnings and Precautions (5.6)].
Bullous Pemphigoid
Inform patients that bullous pemphigoid may occur with this class of drugs. Instruct patients to seek medical advice if blisters or erosions occur [see Warnings and Precautions (5.7)].
SPL MEDGUIDE SECTION
|
Medication Guide | ||||||
|---|---|---|---|---|---|---|
|
This Medication Guide has been approved by the U.S. Food and Drug Administration. |
Revised: 07/2022 | |||||
|
Read this Medication Guide carefully before you start taking JANUVIA and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about JANUVIA, ask your doctor or pharmacist. | ||||||
|
What is the most important information I should know about JANUVIA? *Inflammation of the pancreas (pancreatitis) which may be severe and lead to death. Certain medical problems make you more likely to get pancreatitis. | ||||||
|
|
| ||||
|
Stop taking JANUVIA and call your doctor right away if you have pain in your stomach area (abdomen) that is severe and will not go away. The pain may be felt going from your abdomen through to your back. The pain may happen with or without vomiting. These may be symptoms of pancreatitis. | ||||||
|
*Heart failure. Heart failure means your heart does not pump blood well enough. | ||||||
These may be symptoms of heart failure. | ||||||
|
What is JANUVIA?
| ||||||
|
Who should not take JANUVIA?
Symptoms of a serious allergic reaction to JANUVIA may include rash, raised red patches on your skin (hives), or swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing. | ||||||
|
What should I tell my doctor before taking JANUVIA?
Tell your doctor about all the medicines you take, including prescription
and over-the-counter medicines, vitamins, and herbal supplements. | ||||||
|
How should I take JANUVIA?
| ||||||
|
What are the possible side effects of JANUVIA?
| ||||||
|
|
|
|
| ||
|
*Serious allergic reactions. If you have any symptoms of a serious allergic reaction, stop taking JANUVIA and call your doctor right away or get emergency medical help. See "Who should not take JANUVIA?". Your doctor may give you a medicine for your allergic reaction and prescribe a different medicine for your diabetes. *Joint pain. Some people who take medicines called DPP-4 inhibitors like JANUVIA, may develop joint pain that can be severe. Call your doctor if you have severe joint pain. *Skin reaction. Some people who take medicines called DPP-4 inhibitors like JANUVIA may develop a skin reaction called bullous pemphigoid that can require treatment in a hospital. Tell your doctor right away if you develop blisters or the breakdown of the outer layer of your skin (erosion). Your doctor may tell you to stop taking JANUVIA. The most common side effects of JANUVIA include upper respiratory infection,
stuffy or runny nose and sore throat, and headache. | ||||||
|
How should I store JANUVIA? | ||||||
|
General information about the safe and effective use of JANUVIA. | ||||||
|
What are the ingredients in JANUVIA? | ||||||
|
Distributed by: Merck Sharp & Dohme LLC |