BOTOX
These highlights do not include all the information needed to use BOTOX safely and effectively. See full prescribing information for BOTOX. BOTOX (onabotulinumtoxinA) for injection, for intramuscular, intradetrusor, or intradermal use Initial U.S. Approval: 1989
33d066a9-34ff-4a1a-b38b-d10983df3300
HUMAN PRESCRIPTION DRUG LABEL
Nov 15, 2023
Allergan, Inc.
DUNS: 144796497
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
onabotulinumtoxinA
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (3)
onabotulinumtoxinA
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (3)
Drug Labeling Information
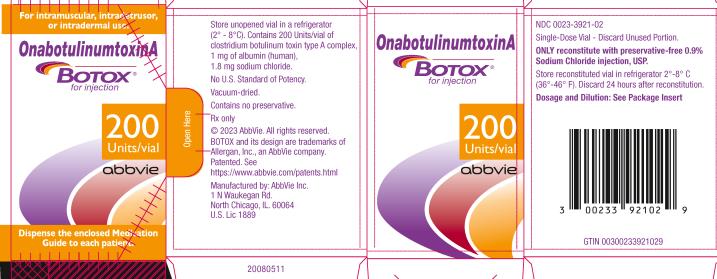
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC 0023-3921-02
OnabotulinumtoxinA
BOTOX®
for injection
200 Units/vial
abbvie
BOXED WARNING SECTION
WARNING: DISTANT SPREAD OF TOXIN EFFECT
CONTRAINDICATIONS SECTION
4****CONTRAINDICATIONS
BOTOX is contraindicated:
-
In patients who are hypersensitive to any botulinum toxin product or to any of the components in the formulation [see Warnings and Precautions (5.4)].
-
In the presence of infection at the proposed injection site(s).
-
For intradetrusor injection in patients with a urinary tract infection; or in patients with urinary retention or post-void residual (PVR) urine volume >200 mL who are not routinely performing clean intermittent self-catheterization (CIC) [see Warnings and Precautions (5.12, 5.13)].
-
Hypersensitivity to any botulinum toxin preparation or to any of the components in the formulation (4, 5.4, 6)
-
Infection at the proposed injection site (4)
-
Intradetrusor Injections: Urinary tract infection or urinary retention (4)
ADVERSE REACTIONS SECTION
6****ADVERSE REACTIONS
The following adverse reactions to BOTOX (onabotulinumtoxinA) for injection are discussed in greater detail in other sections of the labeling:
-
Spread of Toxin Effects [see Warnings and Precautions (5.1)]
-
Serious Adverse Reactions with Unapproved Use [see Warnings and Precautions (5.3)]
-
Hypersensitivity Reactions [see Contraindications (4) and Warnings and Precautions (5.4)]
-
Increased Risk of Clinically Significant Effects with Pre-Existing Neuromuscular Disorders [see Warnings and Precautions (5.5)]
-
Dysphagia and Breathing Difficulties [see Warnings and Precautions (5.6)]
-
Pulmonary Effects of BOTOX in Patients with Compromised Respiratory Status Treated for Spasticity or for Detrusor Overactivity Associated with a Neurologic Condition [see Warnings and Precautions (5.7)]
-
Corneal Exposure and Ulceration in Patients Treated with BOTOX for Blepharospasm [see Warnings and Precautions (5.8)]
-
Retrobulbar Hemorrhages in Patients Treated with BOTOX for Strabismus [see Warnings and Precautions (5.9)]
-
Bronchitis and Upper Respiratory Tract Infections in Patients Treated for Spasticity [see Warnings and Precautions (5.10)]
-
Autonomic Dysreflexia in Patients Treated for Detrusor Overactivity Associated with a Neurologic Condition [see Warnings and Precautions (5.11)]
-
Urinary Tract Infections in Patients with Overactive Bladder [see Warnings and Precautions (5.12)]
-
Urinary Retention in Patients Treated for Bladder Dysfunction [see Warnings and Precautions (5.13)]
6.1****Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
BOTOX and BOTOX Cosmetic contain the same active ingredient in the same formulation, but with different labeled Indications and Usage. Therefore, adverse reactions observed with the use of BOTOX Cosmetic also have the potential to be observed with the use of BOTOX.
In general, adverse reactions occur within the first week following injection of BOTOX and, while generally transient, may have a duration of several months or longer. Localized pain, infection, inflammation, tenderness, swelling, erythema, and/or bleeding/bruising may be associated with the injection. Symptoms associated with flu-like symptoms (e.g., nausea, fever, myalgia) have been reported after treatment. Needle-related pain and/or anxiety may result in vasovagal responses (including syncope, hypotension), which may require appropriate medical therapy.
Local weakness of the injected muscle(s) represents the expected pharmacological action of botulinum toxin. However, weakness of nearby muscles may also occur due to spread of toxin [see Warnings and Precautions (5.1)].
Overactive Bladder
Table 14 presents the most frequently reported adverse reactions in double- blind, placebo-controlled clinical trials for overactive bladder occurring within 12 weeks of the first BOTOX treatment.
Table 14: Adverse Reactions Reported by ≥2% of BOTOX Treated Patients and More Often than in Placebo-Treated Patients Within the First 12 Weeks after Intradetrusor Injection, in Double-Blind, Placebo-Controlled Clinical Trials in Patients with OAB|
Adverse Reactions |
BOTOX |
Placebo |
|
Urinary tract infection |
18 |
6 |
*Elevated PVR not requiring catheterization. Catheterization was required for PVR ≥350 mL regardless of symptoms, and for PVR ≥200 mL to <350 mL with symptoms (e.g., voiding difficulty).
A higher incidence of urinary tract infection was observed in patients with diabetes mellitus treated with BOTOX 100 Units and placebo than in patients without diabetes, as shown in Table 15.
Table 15: Proportion of Patients Experiencing Urinary Tract Infection Following an Injection in Double-Blind, Placebo-Controlled Clinical Trials in OAB According to History of Diabetes Mellitus|
Patients withDiabetes |
Patients without Diabetes | |||
|
BOTOX 100 Units |
Placebo |
BOTOX 100 Units (N=526) |
Placebo | |
|
Urinary tract infection (UTI) |
31 |
12 |
26 |
10 |
The incidence of UTI increased in patients who experienced a maximum post-void residual (PVR) urine volume ≥200 mL following BOTOX injection compared to those with a maximum PVR <200 mL following BOTOX injection, 44% versus 23%, respectively.
No change was observed in the overall safety profile with repeat dosing during an open-label, uncontrolled extension trial.
Adult Detrusor Overactivity associated with a Neurologic Condition
Table 16 presents the most frequently reported adverse reactions in the double-blind, placebo-controlled studies within 12 weeks of injection for patients with detrusor overactivity associated with a neurologic condition treated with BOTOX 200 Units.
Table 16: Adverse Reactions Reported by ≥2% of BOTOX-Treated Patients and More Frequent than in Placebo-Treated Patients Within the First 12 Weeks after Intradetrusor Injection in Double-Blind, Placebo-Controlled Clinical Trials|
Adverse Reactions |
BOTOX 200 Units |
Placebo |
|
Urinary tract infection |
24 |
17 |
The following adverse reactions with BOTOX 200 Units were reported at any time following initial injection and prior to re-injection or study exit (median duration of exposure was 44 weeks): urinary tract infections (49%), urinary retention (17%), constipation (4%), muscular weakness (4%), dysuria (4%), fall (3%), gait disturbance (3%), and muscle spasm (2%).
In the Multiple Sclerosis (MS) patients enrolled in the double-blind, placebo- controlled trials, the MS exacerbation annualized rate (i.e., number of MS exacerbation events per patient-year) was 0.23 for BOTOX and 0.20 for placebo.
No change was observed in the overall safety profile with repeat dosing.
Table 17 presents the most frequently reported adverse reactions in a placebo- controlled, double-blind post-approval 52 week study with BOTOX 100 Units (Study NDO-3) conducted in MS patients with urinary incontinence due to detrusor overactivity associated with a neurologic condition. These patients were not adequately managed with at least one anticholinergic agent and not catheterized at baseline. The table below presents the most frequently reported adverse reactions within 12 weeks of injection.
Table 17: Adverse Reactions Reported in a Post Approval Study (NDO-3) by >2% of BOTOX Treated Patients and More Frequent than in Placebo-Treated Patients Within the First 12 Weeks after Intradetrusor Injection|
Adverse Reactions |
BOTOX |
Placebo |
|
Urinary tract infection |
26 |
6 |
- Elevated PVR not requiring catheterization. Catheterization was required for PVR ≥350 mL regardless of symptoms, and for PVR ≥200 mL to <350 mL with symptoms (e.g., voiding difficulty).
The following adverse events with BOTOX 100 Units were reported at any time following initial injection and prior to re-injection or study exit (median duration of exposure was 51 weeks): urinary tract infections (39%), bacteriuria (18%), urinary retention (17%), residual urine volume* (17%), dysuria (9%), and hematuria (5%).
No difference in the MS exacerbation annualized rate (i.e., number of MS exacerbating events per patient-year) was observed (BOTOX =0, placebo =0.07).
Pediatric Detrusor Overactivity associated with a Neurologic Condition
Table 18 presents the most frequently reported adverse reactions in Study 191622-120, a double-blind, parallel-group study conducted in pediatric patients with detrusor overactivity associated with a neurologic condition. These patients were not adequately managed with at least one anticholinergic agent and were using clean intermittent catheterization at baseline [see Clinical Studies (14.3)]. The table below presents the most frequently reported adverse reactions during the 12 weeks following intradetrusor administration of BOTOX 200 Units.
Table 18: Adverse Reactions Reported by ≥ 3% of BOTOX Treated Pediatric Patients within the First 12 Weeks after Intradetrusor Injection, Study 191622-120|
Adverse Reactions |
BOTOX 200 Unit |
|
Urinary tract infection |
2 (7%) |
|
Bacteriuria |
6 (20%) |
|
Leukocyturia |
2 (7%) |
|
Hematuria |
1 (3%) |
No change was observed in the overall safety profile with repeat dosing.
The most common adverse reactions in patients who received BOTOX 6 U/kg and less than a total dose of 200 U in Study 191622-120 were urinary tract infection (UTI), bacteriuria and hematuria.
Chronic Migraine
In double-blind, placebo-controlled chronic migraine efficacy trials (Study 1 and Study 2), the discontinuation rate was 12% in the BOTOX treated group and 10% in the placebo-treated group. Discontinuations due to an adverse event were 4% in the BOTOX group and 1% in the placebo group. The most frequent adverse events leading to discontinuation in the BOTOX group were neck pain, headache, worsening migraine, muscular weakness and eyelid ptosis.
The most frequently reported adverse reactions following injection of BOTOX for chronic migraine appear in Table 19.
Table 19: Adverse Reactions Reported by ≥2% of BOTOX Treated Patients and More Frequent than in Placebo-Treated Patients in Two Chronic Migraine Double-Blind, Placebo-Controlled Clinical Trials|
Adverse Reactions |
BOTOX |
Placebo | |
|
Nervous system disorders |
5 |
3 | |
|
Eye disorders |
4 |
<1 | |
|
Infections and Infestations |
3 |
2 | |
|
Musculoskeletal and connective tissue disorders |
9 |
3 | |
|
General disorders and administration site conditions |
3 |
2 | |
|
Vascular Disorders |
2 |
1 |
Other adverse reactions that occurred more frequently in the BOTOX group compared to the placebo group at a frequency less than 1% and potentially BOTOX related include: vertigo, dry eye, eyelid edema, dysphagia, eye infection, and jaw pain. Severe worsening of migraine requiring hospitalization occurred in approximately 1% of BOTOX treated patients in Study 1 and Study 2, usually within the first week after treatment, compared to 0.3% of placebo-treated patients.
Adult Upper Limb Spasticity
The most frequently reported adverse reactions following injection of BOTOX for adult upper limb spasticity appear in Table 20.
Table 20: Adverse Reactions Reported by ≥2% of BOTOX Treated Patients and More Frequent than in Placebo-Treated Patients in Adult Upper Limb Spasticity Double-Blind, Placebo-Controlled Clinical Trials|
Adverse Reactions |
BOTOX**** |
BOTOX**** |
BOTOX******** |
Placebo |
|
Gastrointestinal disorder |
3 |
2 |
2 |
1 |
|
General disorders and administration site conditions |
3 |
2 |
2 |
0 |
|
Infections and infestations |
3 |
2 |
0 |
1 |
|
Musculoskeletal and connective tissue disorders |
6 |
5 |
9 |
4 |
Twenty-two adult patients, enrolled in double-blind placebo controlled studies, received 400 Units or higher of BOTOX for treatment of upper limb spasticity. In addition, 44 adults received 400 Units of BOTOX or higher for four consecutive treatments over approximately one year for treatment of upper limb spasticity. The type and frequency of adverse reactions observed in patients treated with 400 Units of BOTOX were similar to those reported in patients treated for upper limb spasticity with 360 Units of BOTOX.
Adult Lower Limb Spasticity
The most frequently reported adverse reactions following injection of BOTOX for adult lower limb spasticity appear in Table 21. Two hundred thirty-one patients enrolled in a double-blind placebo controlled study (Study 7) received 300 Units to 400 Units of BOTOX, and were compared with 233 patients who received placebo. Patients were followed for an average of 91 days after injection.
Table 21: Adverse Reactions Reported by ≥2% of BOTOX Treated Patients and More Frequent than in Placebo-Treated Patients in Adult Lower Limb Spasticity Double-Blind, Placebo-Controlled Clinical Trial (Study 7)|
Adverse Reactions |
B****OTOX |
Placebo |
|
Musculoskeletal and connective tissue disorders |
3 |
1 |
|
Infections and infestations |
2 |
1 |
|
General disorders and administration site conditions |
2 |
1 |
Pediatric Upper Limb Spasticity
The most frequently reported adverse reactions following injection of BOTOX in pediatric patients 2 to 17 years of age with upper limb spasticity appear in Table 22. In a double-blind, placebo-controlled trial (Study 1), 78 patients were treated with 3 Units/kg of BOTOX, and 77 patients received 6 Units/kg to a maximum dose of 200 Units of BOTOX, and were compared to 79 patients who received placebo [see Clinical Studies (14.6)]. Patients were followed for an average of 91 days after injection.
Table 22: Adverse Reactions Reported by ≥2% of BOTOX 6 Units/kg Treated Patients and More Frequent than in Placebo-Treated Patients in Pediatric Upper Limb Spasticity Double-Blind, Placebo-Controlled Clinical Trial (Study 1)|
Adverse Reactions |
BOTOX6Units/kg |
BOTOX3Units/kg |
Placebo |
|
Infections and infestations |
17 |
10 |
9 |
|
General disorders and administration site conditions |
4 |
3 |
1 |
|
Gastrointestinal disorders |
4 |
0 |
0 |
|
Respiratory, thoracic and mediastinal disorders |
4 |
0 |
1 |
|
Nervous system disorders |
5 |
1 |
0 |
*Includes upper respiratory tract infection and viral upper respiratory tract infection
**Includes seizure and partial seizure
Pediatric Lower Limb Spasticity
The most frequently reported adverse reactions following injection of BOTOX in pediatric patients 2 to 17 years of age with lower limb spasticity appear in Table 23. In a double-blind, placebo-controlled trial (Study 2), 126 patients were treated with 4 Units/kg of BOTOX, and 128 patients received 8 Units/kg to a maximum dose of 300 Units of BOTOX, and were compared to 128 patients who received placebo [see Clinical Studies (14.6)]. Patients were followed for an average of 89 days after injection.
Table 23: Adverse Reactions Reported by ≥2% of BOTOX 8 Units/kg Treated Patients and More Frequent than in Placebo-Treated Patients in Pediatric Lower Limb Spasticity Double-Blind, Placebo-Controlled Clinical Trial (Study 2)|
Adverse Reactions |
BOTOX |
BOTOX |
Placebo |
|
General disorders and administration site conditions |
2 |
0 |
0 |
|
Respiratory, thoracic and mediastinal disorders |
2 |
0 |
1 |
|
Injury, poisoning and procedural complications |
2 |
1 |
0 |
|
Metabolism and nutrition disorders |
2 |
0 |
0 |
Cervical Dystonia
In cervical dystonia patients evaluated for safety in double-blind and open- label studies following injection of BOTOX, the most frequently reported adverse reactions were dysphagia (19%), upper respiratory infection (12%), neck pain (11%), and headache (11%).
Other events reported in 2-10% of patients in any one study in decreasing order of incidence include: increased cough, flu syndrome, back pain, rhinitis, dizziness, hypertonia, soreness at injection site, asthenia, oral dryness, speech disorder, fever, nausea, and drowsiness. Stiffness, numbness, diplopia, ptosis, and dyspnea have been reported.
Dysphagia and symptomatic general weakness may be attributable to an extension of the pharmacology of BOTOX resulting from the spread of the toxin outside the injected muscles [see Warnings and Precautions (5.1, 5.6)].
The most common severe adverse reaction associated with the use of BOTOX injection in patients with cervical dystonia is dysphagia with about 20% of these cases also reporting dyspnea [see Warnings and Precautions (5.1, 5.6)]. Most dysphagia is reported as mild or moderate in severity. However, it may be associated with more severe signs and symptoms [see Warnings and Precautions (5.6)].
Additionally, reports in the literature include a case of a female patient who developed brachial plexopathy two days after injection of 120 Units of BOTOX for the treatment of cervical dystonia, and reports of dysphonia in patients who have been treated for cervical dystonia.
Primary Axillary Hyperhidrosis
The most frequently reported adverse reactions (3-10% of adult patients) following injection of BOTOX in double-blind studies included injection site pain and hemorrhage, non-axillary sweating, infection, pharyngitis, flu syndrome, headache, fever, neck or back pain, pruritus, and anxiety.
The data reflect 346 patients exposed to BOTOX 50 Units and 110 patients exposed to BOTOX 75 Units in each axilla.
Blepharospasm
In a study of blepharospasm patients who received an average dose per eye of 33 Units (injected at 3 to 5 sites) of the currently manufactured BOTOX, the most frequently reported adverse reactions were ptosis (21%), superficial punctate keratitis (6%), and eye dryness (6%).
Other events reported in prior clinical studies in decreasing order of incidence include: irritation, tearing, lagophthalmos, photophobia, ectropion, keratitis, diplopia, entropion, diffuse skin rash, and local swelling of the eyelid skin lasting for several days following eyelid injection.
In two cases of VII nerve disorder, reduced blinking from BOTOX injection of the orbicularis muscle led to serious corneal exposure, persistent epithelial defect, corneal ulceration and a case of corneal perforation. Focal facial paralysis, syncope, and exacerbation of myasthenia gravis have also been reported after treatment of blepharospasm.
Strabismus
Extraocular muscles adjacent to the injection site can be affected, causing vertical deviation, especially with higher doses of BOTOX. The incidence rates of these adverse effects in 2058 adults who received a total of 3650 injections for horizontal strabismus was 17%.
The incidence of ptosis has been reported to be dependent on the location of the injected muscles, 1% after inferior rectus injections, 16% after horizontal rectus injections and 38% after superior rectus injections.
In a series of 5587 injections, retrobulbar hemorrhage occurred in 0.3% of cases.
6.2****Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to onabotulinumtoxinA in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
In a long term, open-label study evaluating 326 cervical dystonia patients treated for an average of 9 treatment sessions with the current formulation of BOTOX, 4 (1.2%) patients had positive antibody tests. All 4 of these patients responded to BOTOX therapy at the time of the positive antibody test. However, 3 of these patients developed clinical resistance after subsequent treatment, while the fourth patient continued to respond to BOTOX therapy for the remainder of the study.
One patient among the 445 hyperhidrosis patients (0.2%), two patients among the 380 adult upper limb spasticity patients (0.5%), and no patients among 406 migraine patients with analyzed specimens developed the presence of neutralizing antibodies.
In one Phase 3 study and the open-label extension study in patients with pediatric lower limb spasticity, neutralizing antibodies developed in 2 of 264 patients (0.8%) treated with BOTOX for up to 5 treatment cycles. Both patients continued to experience clinical benefit following subsequent BOTOX treatments.
In overactive bladder patients with analyzed specimens from the two phase 3 studies and the open-label extension study, neutralizing antibodies developed in 0 of 954 patients (0.0%) while receiving BOTOX 100 Unit doses and 3 of 260 patients (1.2%) after subsequently receiving at least one 150 Unit dose. Response to subsequent BOTOX treatment was not different following seroconversion in these three patients.
In detrusor overactivity associated with neurologic condition patients with analyzable specimens in the adult drug development program (including the open-label extension study), neutralizing antibodies developed in 3 of 300 patients (1.0%) after receiving only BOTOX 200 Unit doses and 5 of 258 patients (1.9%) after receiving at least one 300 Unit dose. Following development of neutralizing antibodies in these 8 patients, 4 continued to experience clinical benefit, 2 did not experience clinical benefit, and the effect on the response to BOTOX in the remaining 2 patients is not known. In 99 pediatric patients who had a negative baseline result for binding antibodies or neutralizing antibodies and had at least one evaluable post- baseline value from one randomized double-blind study and one double-blind extension study, no patients developed neutralizing antibodies after receiving 50 Units to 200 Units of BOTOX.
The data reflect the patients whose test results were considered positive for neutralizing activity to BOTOX in a mouse protection assay or negative based on a screening ELISA assay or mouse protection assay.
Formation of neutralizing antibodies to botulinum toxin type A may reduce the effectiveness of BOTOX treatment by inactivating the biological activity of the toxin. The critical factors for neutralizing antibody formation have not been well characterized. The results from some studies suggest that BOTOX injections at more frequent intervals or at higher doses may lead to greater incidence of antibody formation. The potential for antibody formation may be minimized by injecting with the lowest effective dose given at the longest feasible intervals between injections.
6.3****Postmarketing****Experience
The following adverse reactions have been identified during post-approval use of BOTOX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions include: abdominal pain; alopecia, including madarosis; anorexia; brachial plexopathy; denervation/muscle atrophy; diarrhea; dry eye; eyelid edema (following periocular injection); hyperhidrosis; hypoacusis; hypoaesthesia; localized muscle twitching; malaise; Mephisto sign; paresthesia; peripheral neuropathy; radiculopathy; erythema multiforme, dermatitis psoriasiform, and psoriasiform eruption; strabismus; tinnitus; and visual disturbances.
There have been spontaneous reports of death, sometimes associated with dysphagia, pneumonia, and/or other significant debility or anaphylaxis, after treatment with botulinum toxin [see Warnings and Precautions (5.4, 5.6)].
There have also been reports of adverse events involving the cardiovascular system, including arrhythmia and myocardial infarction, some with fatal outcomes. Some of these patients had risk factors including cardiovascular disease. The exact relationship of these events to the botulinum toxin injection has not been established.
New onset or recurrent seizures have also been reported, typically in patients who are predisposed to experiencing these events. The exact relationship of these events to the botulinum toxin injection has not been established.
The most common adverse reactions (≥5% and >placebo, if applicable) are (6.1):
-
OAB: urinary tract infection, dysuria, urinary retention
-
Adult Detrusor Overactivity associated with a neurologic condition: urinary tract infection, urinary retention
-
Pediatric Detrusor Overactivity associated with a neurologic condition: urinary tract infection, leukocyturia, bacteriuria
-
Chronic Migraine: neck pain, headache
-
Adult Spasticity: pain in extremity
-
Pediatric Spasticity: upper respiratory tract infection
-
Cervical Dystonia: dysphagia, upper respiratory infection, neck pain, headache, increased cough, flu syndrome, back pain, rhinitis
-
Axillary Hyperhidrosis: injection site pain and hemorrhage, non-axillary sweating, pharyngitis, flu syndrome
To report SUSPECTED ADVERSE REACTIONS, contact AbbVie at 1-800-678-1605 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7****DRUG INTERACTIONS
**7.1****Aminoglycosides and Other Agents Interfering with Neuromuscular
Transmission**
Co-administration of BOTOX and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like compounds) should only be performed with caution as the effect of the toxin may be potentiated.
7.2****Anticholinergic Drugs
Use of anticholinergic drugs after administration of BOTOX may potentiate systemic anticholinergic effects.
7.3****Other Botulinum Neurotoxin Products
The effect of administering different botulinum neurotoxin products at the same time or within several months of each other is unknown. Excessive neuromuscular weakness may be exacerbated by administration of another botulinum toxin prior to the resolution of the effects of a previously administered botulinum toxin.
7.4****Muscle Relaxants
Excessive weakness may also be exaggerated by administration of a muscle relaxant before or after administration of BOTOX.
Patients receiving concomitant treatment of BOTOX and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like agents), or muscle relaxants, should be observed closely because the effect of BOTOX may be potentiated (7.1, 7.4)
DOSAGE FORMS & STRENGTHS SECTION
3****DOSAGE FORMS AND STRENGTHS
For Injection: sterile 100 Units or 200 Units vacuum-dried powder in single- dose vials for reconstitution only with sterile, preservative-free 0.9% Sodium Chloride Injection, USP prior to injection.
For Injection: 100 Units or 200 Units vacuum-dried powder in a single-dose vial (3)
USE IN SPECIFIC POPULATIONS SECTION
8****USE IN SPECIFIC POPULATIONS
8.1****Pregnancy
Risk Summary
There are no studies or adequate data from postmarketing surveillance on the developmental risk associated with use of BOTOX in pregnant women. In animal studies, administration of BOTOX during pregnancy resulted in adverse effects on fetal growth (decreased fetal weight and skeletal ossification) at clinically relevant doses, which were associated with maternal toxicity [see Data].
In the U.S. general population, the estimated background risk of major birth defects and miscarriages in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk of major birth defects and miscarriage for the indicated populations is unknown.
Data
Animal Data
When BOTOX (4, 8, or 16 Units/kg) was administered intramuscularly to pregnant mice or rats two times during the period of organogenesis (on gestation days 5 and 13), reductions in fetal body weight and decreased fetal skeletal ossification were observed at the two highest doses. The no-effect dose for developmental toxicity in these studies (4 Units/kg) is approximately equal to the human dose of 400 Units, on a body weight basis (Units/kg).
When BOTOX was administered intramuscularly to pregnant rats (0.125, 0.25, 0.5, 1, 4, or 8 Units/kg) or rabbits (0.063, 0.125, 0.25, or 0.5 Units/kg) daily during the period of organogenesis (total of 12 doses in rats, 13 doses in rabbits), reduced fetal body weights and decreased fetal skeletal ossification were observed at the two highest doses in rats and at the highest dose in rabbits. These doses were also associated with significant maternal toxicity, including abortions, early deliveries, and maternal death. The developmental no-effect doses in these studies of 1 Unit/kg in rats and 0.25 Units/kg in rabbits are less than the human dose of 400 Units, based on Units/kg.
When pregnant rats received single intramuscular injections (1, 4, or 16 Units/kg) at three different periods of development (prior to implantation, implantation, or organogenesis), no adverse effects on fetal development were observed. The developmental no-effect level for a single maternal dose in rats (16 Units/kg) is approximately 2 times the human dose of 400 Units, based on Units/kg.
8.2****Lactation
Risk Summary
There are no data on the presence of BOTOX in human or animal milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for BOTOX and any potential adverse effects on the breastfed infant from BOTOX or from the underlying maternal conditions.
8.4****Pediatric Use
Detrusor Overactivity associated with a Neurologic Condition
The safety and effectiveness of BOTOX for detrusor overactivity associated with a neurologic condition have been established in pediatric patients 5 years of age and older who have an inadequate response to or are intolerant of anticholinergic medication. Use of BOTOX in this patient population is based on the results of a randomized, double-blind, parallel group trial in 113 pediatric patients 5 to 17 years of age (inclusive) with detrusor overactivity associated with a neurologic condition (Study 191622-120) and a long-term, multicenter, double-blind, long-term extension trial (Study 191622-121) [see Clinical Studies (14.3)]. The most common adverse reactions in this population were urinary tract infection, bacteriuria, hematuria, and leukocyturia [see Adverse Reactions (6.1)].
The safety and effectiveness of BOTOX have not been established in patients with NDO younger than 5 years of age.
Overactive Bladder
The safety and effectiveness of BOTOX for the treatment of overactive bladder have not been established in pediatric patients.
Efficacy was not demonstrated in a multicenter, randomized, double-blind, parallel-group, multiple-dose clinical study which was conducted to evaluate the efficacy and safety of BOTOX in pediatric patients aged 12 to 17 years with overactive bladder. Fifty-five patients who had an inadequate response to or were intolerant of at least one anticholinergic medication were treated with BOTOX. There was not a statistically significant difference in the mean change from baseline in the daily average frequency of daytime urinary incontinence episodes (primary efficacy endpoint) at week 12 post-treatment when a medium and high dose were each compared to a low dose of BOTOX. The adverse reactions in pediatric patients treated with BOTOX were comparable with the known safety profile in adults with overactive bladder.
Prophylaxis of Headaches in Chronic Migraine
Safety and effectiveness in patients below the age of 18 years have not been established.
In a 12-week, multicenter, double-blind, placebo-controlled clinical trial, 123 adolescent patients (ages 12 to below 18 years) with chronic migraine were randomized to receive BOTOX 74 Units, BOTOX 155 Units, or placebo, for one injection cycle. This trial did not establish the efficacy of BOTOX, compared with placebo, for the prophylaxis of headaches in adolescents with chronic migraine.
Spasticity
Safety and effectiveness have been established in pediatric patients 2 to 17 years of age [see Warnings and Precautions (5.1), Adverse Reactions (6.1), and Clinical Studies (14.6)]. The safety and effectiveness of BOTOX have been established by evidence from adequate and well-controlled studies of BOTOX in patients 2 to 17 years of age with upper and lower limb spasticity.
Safety and effectiveness in pediatric patients below the age of 2 years have not been established [see Boxed Warning and Warnings and Precautions (5.1)].
Axillary Hyperhidrosis
Safety and effectiveness in patients below the age of 18 years have not been established.
Cervical Dystonia
Safety and effectiveness in pediatric patients below the age of 16 years have not been established.
Blepharospasm and Strabismus
Safety and effectiveness in pediatric patients below the age of 12 years have not been established.
Juvenile Animal Data
In a study in which juvenile rats received intramuscular injection of BOTOX (0, 8, 16, or 24 Units/kg) every other week from postnatal day 21 for 12 weeks, changes in bone size/geometry associated with decreased bone density and bone mass were observed at all doses, in association with limb disuse, decreased muscle contraction, and decreased body weight gain. Impairment of fertility and male reproductive organ histopathology (degeneration of seminiferous tubules of the testis) were observed at the mid and high doses. Bone and male reproductive organ effects showed evidence of reversibility after dosing cessation. The no-effect dose for adverse developmental effects in juvenile animals (8 Units/kg) is similar to the human dose (400 Units) on a body weight (kg) basis.
8.5****Geriatric Use
Of the 2145 adult patients in placebo-controlled clinical studies of BOTOX for the treatment of spasticity, 33.5% were 65 or older, and 7.7% were 75 years of age or older. No overall differences in safety were observed between elderly patients and adult patients younger than 65 years of age.
In clinical studies of BOTOX across other indications, no overall differences in safety were observed between elderly patients and younger adult patients, with the exception of Overactive Bladder (see below). Other reported clinical experience has not identified differences in responses between the elderly and younger adult patients, but greater sensitivity of some older individuals cannot be ruled out.
Overactive Bladder
Of 1242 overactive bladder patients in placebo-controlled clinical studies of BOTOX, 41.4% were 65 years of age or older, and 14.7% were 75 years of age or older. Adverse reactions of UTI and urinary retention were more common in patients 65 years of age or older in both placebo and BOTOX groups compared to younger patients (see Table 24). Otherwise, there were no overall differences in the safety profile following BOTOX treatment between patients aged 65 years and older compared to adult patients younger than 65 years of age in these studies.
Table 24: Incidence of Urinary Tract Infection and Urinary Retention according to Age Group during First Placebo-Controlled Treatment, Placebo- Controlled Clinical Trials in Patients with OAB|
<65 Years |
65 to 74 Years |
**≥**75 Years | ||||
|
Adverse Reaction****s |
B****OTOX |
Placebo |
B****OTOX |
Placebo |
B****OTOX |
Placebo |
|
Urinary tract infection |
21 |
7 |
30 |
13 |
38 |
19 |
|
Urinary retention |
6 |
0.6 |
8 |
0 |
9 |
1 |
Observed effectiveness was comparable between these age groups in placebo- controlled clinical studies.
- Pregnancy: Based on animal data, may cause fetal harm. (8.1)
DESCRIPTION SECTION
11****DESCRIPTION
OnabotulinumtoxinA is a sterile, vacuum-dried purified botulinum toxin type A, produced from fermentation of Hall strain Clostridium botulinum type A, and intended for intramuscular, intradetrusor and intradermal use. It is purified from the culture solution by dialysis and a series of acid precipitations to a complex consisting of the neurotoxin, and several accessory proteins. The complex is dissolved in sterile sodium chloride solution containing Albumin Human and is sterile filtered (0.2 microns) prior to filling and vacuum- drying.
The primary release procedure for BOTOX uses a cell-based potency assay to determine the potency relative to a reference standard. The assay is specific to AbbVie’s products BOTOX and BOTOX Cosmetic. One Unit of BOTOX corresponds to the calculated median intraperitoneal lethal dose (LD50) in mice. Due to specific details of this assay such as the vehicle, dilution scheme, and laboratory protocols, Units of biological activity of BOTOX cannot be compared to nor converted into Units of any other botulinum toxin or any toxin assessed with any other specific assay method. The specific activity of BOTOX is approximately 20 Units/nanogram of neurotoxin protein complex.
Each vial of BOTOX (onabotulinumtoxinA) for injection contains either 100 Units of Clostridium botulinum type A neurotoxin complex, 0.5 mg of Albumin Human, and 0.9 mg of sodium chloride; or 200 Units of Clostridium botulinum type A neurotoxin complex, 1 mg of Albumin Human, and 1.8 mg of sodium chloride in a sterile, vacuum-dried form without a preservative.
CLINICAL PHARMACOLOGY SECTION
12****CLINICAL PHARMACOLOGY
12.1****Mechanism of Action
BOTOX blocks neuromuscular transmission by binding to acceptor sites on motor or autonomic nerve terminals, entering the nerve terminals, and inhibiting the release of acetylcholine. This inhibition occurs as the neurotoxin cleaves SNAP-25, a protein integral to the successful docking and release of acetylcholine from vesicles situated within nerve endings. When injected intramuscularly at therapeutic doses, BOTOX produces partial chemical denervation of the muscle resulting in a localized reduction in muscle activity. In addition, the muscle may atrophy, axonal sprouting may occur, and extrajunctional acetylcholine receptors may develop. There is evidence that reinnervation of the muscle may occur, thus slowly reversing muscle denervation produced by BOTOX.
When injected intradermally, BOTOX produces temporary chemical denervation of the sweat gland resulting in local reduction in sweating.
Following intradetrusor injection, BOTOX affects the efferent pathways of detrusor activity via inhibition of acetylcholine release.
12.3****Pharmacokinetics
Using currently available analytical technology, it is not possible to detect BOTOX in the peripheral blood following intramuscular injection at the recommended doses.
SPL MEDGUIDE SECTION
|
MEDICATION GUIDE |
|
What is the most important information I should know about BOTOX****and
BOTOX Cosmetic? *Problems breathing or swallowing *Spread of toxin effects These problems can happen hours, days, to weeks after an injection of BOTOX or BOTOX Cosmetic.****Call your doctor or get medical help right away if you have any of these problems after treatment with BOTOX****or BOTOX** **Cosmetic: Problems swallowing, speaking, or breathing.These problems can happen hours, days, to weeks after an injection of BOTOX or BOTOX Cosmetic usually because the muscles that you use to breathe and swallow can become weak after the injection. Death can happen as a complication if you have severe problems with swallowing or breathing after treatment withBOTOX orBOTOXCosmetic. * People with certain breathing problems may need to use muscles in their neck to help them breathe. These people may be at greater risk for serious breathing problems withBOTOX or**BOTOX*Cosmetic. *Spread of toxin effects. In some cases, the effect of botulinum toxin may affect areas of the body away from the injection site and cause symptoms of a serious condition called botulism. The symptoms of botulism include: These symptoms can happen hours, days, to weeks after you receive an injection
ofBOTOX orBOTOX****Cosmetic. |
|
What are BOTOX and BOTOX Cosmetic?
BOTOX****is also injected into the skin to treat the symptoms of severe underarm sweating (severe primary axillary hyperhidrosis) when medicines used on the skin (topical) do not work well enough. |
|
BOTOX****Cosmetic is a prescription medicine for adults that is injected into muscles and used for a short period of time (temporary) to improve the look of:
You may receive treatment for frown lines, crow’s feet lines, and forehead lines at the same time. |
|
It is not known whetherBOTOX is safe and effective in people younger than:
BOTOX****Cosmetic is not recommended for use in children younger than 18
years of age. |
|
Who should notreceive BOTOXor BOTOX Cosmetic?
|
|
What should I tell my doctor beforereceiving BOTOX or BOTOX
Cosmetic?
Tell your doctor about all the medicines you take, including prescription
and over-the-counter medicines, vitamins and herbal supplements. Using
BOTOX orBOTOX****Cosmetic with certain other medicines may cause
serious side effects.Do not start any new medicines until you have told
your doctor that you have received BOTOX or BOTOX Cosmetic in the past.
Ask your doctor if you are not sure if your medicine is one that is listed
above. |
|
HowwillIreceiveBOTOX or BOTOX Cosmetic? BOTOX orBOTOX***Cosmetic is an injection that your doctor will give you. *BOTOX is injected into your affected muscles, skin, or bladder. *BOTOXCosmeticis injected into your affected muscles.
*Your doctor will tell you how often you will receive your dose of BOTOX or BOTOX Cosmetic injections. |
|
What should I avoid whilereceivingBOTOX or BOTOX Cosmetic? |
|
What are the possible side effects of BOTOX and BOTOX Cosmetic?
Tell your doctor if you have any side effect that bothers you or that does not
go away. |
|
General information aboutthe safe and effective use ofBOTOX and
BOTOX Cosmetic: |
|
What are the ingredients in BOTOX and BOTOX Cosmetic? |
|
Manufactured by: AbbVie Inc. |
|
|
|
v7.0MG1145 |
This Medication Guide has been approved by the U.S. Food and Drug Administration.Revised:11/202****3
OVERDOSAGE SECTION
10****OVERDOSAGE
Excessive doses of BOTOX (onabotulinumtoxinA) for injection may be expected to produce neuromuscular weakness with a variety of symptoms.
Symptoms of overdose are likely not to be present immediately following injection. Should accidental injection or oral ingestion occur or overdose be suspected, the person should be medically supervised for several weeks for signs and symptoms of systemic muscular weakness which could be local, or distant from the site of injection [see Boxed Warning and Warnings and Precautions (5.1, 5.6)]. These patients should be considered for further medical evaluation and appropriate medical therapy immediately instituted, which may include hospitalization.
If the musculature of the oropharynx and esophagus are affected, aspiration may occur which may lead to development of aspiration pneumonia. If the respiratory muscles become paralyzed or sufficiently weakened, intubation and assisted respiration may be necessary until recovery takes place. Supportive care could involve the need for a tracheostomy and/or prolonged mechanical ventilation, in addition to other general supportive care.
In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin- induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. If you do not receive a response within 30 minutes, please contact the CDC directly at 1-770-488-7100. More information can be obtained at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5232a8.htm.
NONCLINICAL TOXICOLOGY SECTION
13****NONCLINICAL TOXICOLOGY
13.1****Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long term studies in animals have not been performed to evaluate the carcinogenic potential of BOTOX.
Mutagenesis
BOTOX was negative in a battery of in vitro (microbial reverse mutation assay, mammalian cell mutation assay, and chromosomal aberration assay) and in vivo (micronucleus assay) genetic toxicology assays.
Impairment of Fertility
In fertility studies of BOTOX (4, 8, or 16 Units/kg) in which either male or female rats were injected intramuscularly prior to mating and on the day of mating (3 doses, 2 weeks apart for males: 2 doses, 2 weeks apart for females) to untreated animals, reduced fertility was observed in males at the intermediate and high doses and in females at the high dose. The no-effect doses for reproductive toxicity (4 Units/kg in males, 8 Units/kg in females) are approximately equal to the human dose of 400 Units, on a body weight basis (Units/kg).
13.2Animal Toxicology and/or Pharmacology
In a study to evaluate inadvertent peribladder administration, bladder stones were observed in 1 of 4 male monkeys that were injected with a total of 6.8 Units/kg divided into the prostatic urethra and proximal rectum (single administration). No bladder stones were observed in male or female monkeys following injection of up to 36 Units/kg (~12X the highest human bladder dose) directly to the bladder as either single or 4 repeat dose injections or in female rats for single injections up to 100 Units/kg (~33X the highest human bladder dose [200 Units], based on Units/kg).
HOW SUPPLIED SECTION
16****HOW SUPPLIED/STORAGE AND HANDLING
16**.1****How Supplied**
BOTOX (onabotulinumtoxinA) for injection is a sterile, vacuum-dried powder supplied in a single-dose vial in the following sizes:
100 Units NDC 0023-1145-01
200 Units NDC 0023-3921-02
BOTOX cartons have features to alert users if contents may have been compromised. Each BOTOX vial label and carton also contains the U.S. License number: 1889 [see Dosage and Administration (2.1)].
Do not use the product and contact AbbVie for additional information at 1-800-678-1605 if the labeling is not described as above.
16.2**Storage and Handling**
Unopened vials of BOTOX should be stored in a refrigerator between 2° to 8°C (36º to 46ºF) for up to 36 months. Do not use after the expiration date on the vial. Reconstituted BOTOX may be stored in a refrigerator (2° to 8°C) for up to 24 hours until time of use [see Dosage and Administration (2.2)].
INFORMATION FOR PATIENTS SECTION
17****PATIENT COUNSELING INFORMATION
Advise the patient or caretaker to read the FDA-approved patient labeling (Medication Guide).
Swallowing, Speaking or Breathing Difficulties, or Other Unusual Symptoms
Advise patients or their caretaker(s) to inform their doctor or pharmacist if they develop any unusual symptoms (including difficulty with swallowing, speaking, or breathing), or if any existing symptom worsens [see Boxed Warning and Warnings and Precautions (5.1, 5.6)].
Ability to Operate Machinery or Vehicles
Advise patients or their caretaker(s) that if loss of strength, muscle weakness, blurred vision, dizziness, or drooping eyelids occur, they should avoid driving a car or engaging in other potentially hazardous activities.
Voiding Symptoms after Bladder Injections
After bladder injections for urinary incontinence, advise patients to contact their physician if they experience difficulties in voiding or burning sensation upon voiding.****
Manufactured by: AbbVie Inc.
1 N Waukegan Rd. North Chicago, IL. 60064
U.S. License Number 1889
© 2023 AbbVie.
All rights reserved.
BOTOX and its design are trademarks of Allergan Inc., an AbbVie company
Patented. See: https://www.abbvie.com/patents.html

v11.0USPI1145

