VONVENDI
These highlights do not include all the information needed to use VONVENDI safely and effectively. See full prescribing information for VONVENDI. VONVENDI [von Willebrand factor (recombinant)] lyophilized powder for solution, for intravenous injection Initial U.S. Approval: 2015
53b6d198-6175-4a26-8606-dc0d2a0f12d6
PLASMA DERIVATIVE
Sep 10, 2025
Takeda Pharmaceuticals America, Inc.
DUNS: 039997266
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
von Willebrand Factor (Recombinant)
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
von Willebrand Factor (Recombinant)
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Drug Labeling Information
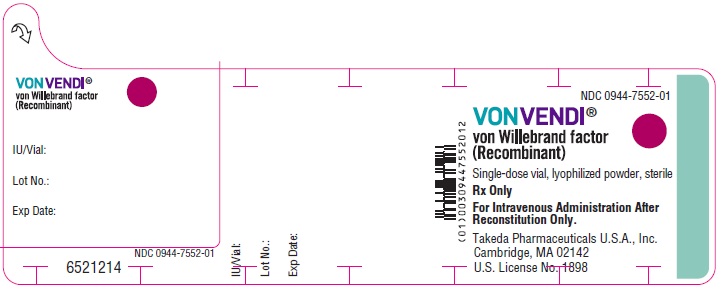
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 1300 IU Vial Label
NDC 0944-7552-01
VONVENDI**®******
von Willebrand factor
(Recombinant)
Single-dose vial, lyophilized powder, sterile
Rx Only
For Intravenous Administration After
Reconstitution Only.
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142
U.S. License No. 1898
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
VONVENDI® is indicated in adult and pediatric patients with von Willebrand disease (VWD) for:
- On-demand treatment and control of bleeding episodes.
- Perioperative management of bleeding.
For adult patients only:
- Routine prophylaxis to reduce the frequency of bleeding episodes.,
VONVENDI [von Willebrand factor (recombinant)] is a recombinant von Willebrand factor (rVWF) indicated in adult and pediatric patients with von Willebrand disease (VWD) for:
- On-demand treatment and control of bleeding episodes. (1)
- Perioperative management of bleeding. (1)
For adult patients only:
- Routine prophylaxis to reduce the frequency of bleeding episodes. (1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
VONVENDI is contraindicated in patients who have had life-threatening hypersensitivity reactions to VONVENDI or constituents of the product (tri- sodium citrate-dihydrate, glycine, mannitol, trehalose-dihydrate, polysorbate 80, and hamster or mouse proteins) [see Warning and Precautions (5.2) and Description (11)].
Do not use in patients who have had life-threatening hypersensitivity reactions to VONVENDI or its components (tri-sodium citrate-dihydrate, glycine, mannitol, trehalose-dihydrate polysorbate 80, and hamster or mouse proteins). (4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Thromboembolic Events
Thromboembolic events have occurred with VONVENDI [see Adverse Reactions (6.1)]. These events can include disseminated intravascular coagulation (DIC), venous thrombosis, pulmonary embolism, myocardial infarction, and stroke. Patients with known risk factors for thrombosis, including low ADAMTS13 levels, are at a higher risk [see Description (11)]. Monitor patients for signs and symptoms of thrombosis such as pain, swelling, discoloration, dyspnea, cough, hemoptysis, and syncope. Institute prophylaxis measures against thromboembolism according to current clinical practice and standard of care.
In patients requiring frequent doses of VONVENDI in combination with rFVIII, monitor plasma levels for FVIII:C activity because sustained excessive factor VIII plasma levels can increase the risk of thromboembolic complications.
5.2 Hypersensitivity and Infusion-Related Reactions
Hypersensitivity reactions and infusion-related reactions have occurred with VONVENDI [see Adverse Reactions (6.1). These reactions can include anaphylactic shock, generalized urticaria, angioedema, chest tightness, hypotension, shock, lethargy, nausea, vomiting, paresthesia, pruritus, restlessness, blurred vision, wheezing and/or acute respiratory distress. If signs and symptoms of severe allergic reactions occur, immediately discontinue administration of VONVENDI and provide appropriate supportive care.
VONVENDI contains trace amounts of mouse immunoglobulin G (MuIgG) and hamster proteins less than or equal to 2 ng/IU VONVENDI. Patients treated with this product may develop hypersensitivity reactions to non-human mammalian proteins.
5.3 Neutralizing Antibodies
Neutralizing antibodies to VWF and/or factor VIII can occur with VONVENDI. If the expected plasma levels of VWF activity (VWF:RCo) are not attained, perform an appropriate assay to determine if anti-VWF or anti-factor VIII inhibitors are present. Consider other therapeutic options and direct the patient to a physician with experience in the care of either VWD or hemophilia A.
In patients with high levels of inhibitors to VWF or factor VIII, VONVENDI therapy may not be effective, and infusion of this protein may lead to severe hypersensitivity reactions. Since inhibitor antibodies can occur concomitantly with anaphylactic reactions, evaluate patients experiencing an anaphylactic reaction for the presence of inhibitors.
5.4 Monitoring Laboratory Tests
Monitor plasma levels of VWF:RCo and factor VIII activities in patients receiving VONVENDI to avoid sustained excessive VWF and/or factor VIII activity levels, which may increase the risk of thrombotic events, particularly in patients with known clinical or laboratory risk factors.
Monitor for development of VWF and/or factor VIII inhibitors when suspected. Perform appropriate inhibitor assays to determine if VWF and/or factor VIII inhibitors are present if bleeding is not controlled with the expected dose of VONVENDI.
- Thromboembolic events have occurred with VONVENDI. Patients with known risk factors for thrombosis are at higher risk. Monitor for early signs of thrombosis and have prophylaxis measures against thromboembolism instituted according to current recommendations. In patients requiring frequent doses of VONVENDI in combination with recombinant factor VIII, monitor plasma levels for FVIII:C because sustained excessive factor VIII plasma levels can increase the risk for thromboembolic events. (5.1)
- Hypersensitivity and infusion-related reactions, including anaphylaxis, may occur. Discontinue VONVENDI if hypersensitivity symptoms occur and administer appropriate emergency treatment. (5.2)
- Neutralizing antibodies to von Willebrand factor (VWF) and/or factor VIII can occur with VONVENDI. If the expected plasma levels of VWF activity (VWF:RCo) are not attained, or if bleeding is not controlled with an appropriate dose, perform an appropriate assay to determine if an anti-VWF or anti-factor VIII inhibitors are present. (5.3)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety data described in this section reflects exposure of VONVENDI in six clinical studies (Study 1, Study 2, Study 3, Study 4, Study 5 and Study 6) in patients with von Willebrand Disease (VWD). A total of 103 adult and 29 pediatric patients received intravenous infusion of VONVENDI with or without rFVIII with a median dose of 311 IU/kg per patient (range of 2 to 29593 IU/kg). The patients were followed for up to 4.6 years.
The most common adverse reactions observed in greater than or equal to 2% of patients in clinical trials with VONVENDI (n=132) were headache, vomiting, nausea, dizziness and generalized pruritus.
Table 5 lists the adverse reactions reported with VONVENDI from pooled safety population from six clinical studies.
Table 5: Adverse Reactions|
System Organ Class (SOC) |
Adverse Reaction |
Total (N=132) |
|---|---|---|
| ||
|
Cardiac Disorders |
Tachycardia |
1 (0.8%) |
|
Gastrointestinal Disorders |
Vomiting |
9 (7%) |
|
Nausea |
7 (5%) | |
|
General Disorders and Administration Site Conditions |
Infusion site paresthesia |
1 (0.8%) |
|
Infusion-related reaction* |
1 (0.8%) | |
|
Skin and Subcutaneous Tissues Disorders |
Generalized pruritus |
3 (2%) |
|
Vascular Disorders |
Hypertension |
2 (2%) |
|
Hot flush |
1 (0.8%) | |
|
Deep vein thrombosis |
1 (0.8%) | |
|
Nervous System Disorders |
Headache |
18 (14%) |
|
Dizziness |
4 (3%) | |
|
Vertigo |
2 (2%) | |
|
Dysgeusia |
1 (0.8%) | |
|
Tremor |
1 (0.8%) | |
|
Investigations |
Electrocardiogram T wave inversions |
1 (0.8%) |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of VONVENDI. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System Disorders: Hypersensitivity including anaphylactic reaction; Infusion related reaction.
The most common adverse reactions observed (≥2% of patients) were headache, vomiting, nausea, dizziness and generalized pruritus. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals U.S.A., Inc. at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
SPL PATIENT PACKAGE INSERT SECTION
|
Patient Information |
|---|
|
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 9/2025 |
|
This leaflet summarizes important information about VONVENDI. Please read it
carefully before using this medicine. This information does not take the place
of talking with your healthcare provider, and it does not include all of the
important information about VONVENDI. If you have any questions after reading
this, ask your healthcare provider. |
|
What is VONVENDI?
For adult patients only:
|
|
Who should not use VONVENDI?
Tell your healthcare provider if you are pregnant or breastfeeding because VONVENDI may not be right for you. |
|
What should I tell my healthcare provider before I use VONVENDI?
|
|
How should I use VONVENDI? |
|
What are the possible side effects of VONVENDI? |
|
What are the VONVENDI dosage strengths? |
|
Green: Dosage strength of approximately 650 International Units (450–850 IU) (reconstituted with 5 mL of sterile water). |
|
Dark Red: Dosage strength of approximately 1300 International Units (900–1700 IU) (reconstituted with 10 mL of sterile water). |
|
|
How do I store VONVENDI?
|
|
What else should I know about VONVENDI and von Willebrand Disease? |
|
Resources at Takeda available to the patients: |
INSTRUCTIONS FOR USE SECTION
|
Instructions for Use |
This Instructions for Use contains information on how to inject VONVENDI.
For first dose for each bleeding episode, use with recombinant factor VIII as instructed by your physician.
- Always follow the specific instructions given by your healthcare provider. The steps listed below are general guidelines for using VONVENDI. If you are unsure of the procedures, please call your healthcare provider before using.
- Call your healthcare provider right away if bleeding is not controlled after using VONVENDI.
- Your healthcare provider will prescribe the VONVENDI dose that you should take. If this is your first infusion to control a new bleeding episode, and if recombinant factor VIII in needed, be sure you also have the correct dose of recombinant factor VIII as instructed by your physician.
- Your healthcare provider may need to take blood tests from time to time.
- Talk to your healthcare provider before traveling. Plan to bring enough VONVENDI for your treatment during this time.
- Dispose of all materials, including any leftover reconstituted VONVENDI product, in an appropriate container.
See below for step-by-step instructions for reconstituting and administrating VONVENDI:
Reconstitution
Prepare a clean flat surface and gather all the materials you will need for the infusion. Check the expiration date, and let the VONVENDI warm up to room temperature. Wash your hands and put on clean exam gloves. If infusing yourself at home, the use of gloves is optional.
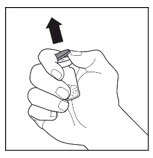
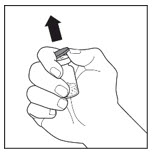
Remove the caps from the VONVENDI concentrate and diluent vials to expose the center of the rubber stoppers.
|
|
Disinfect each stopper with a separate sterile alcohol swab (or other suitable sterile solution suggested by your healthcare provider or hemophilia center) by rubbing the stopper for several seconds and allow it to dry prior to use. Place the vials on a flat surface.
|
|
Open the Mix2Vial device package by completely peeling away the lid, without touching the inside of the package. Do not remove the Mix2Vial device from the package.
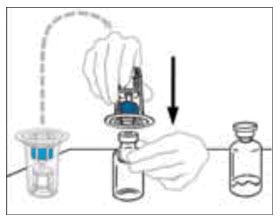
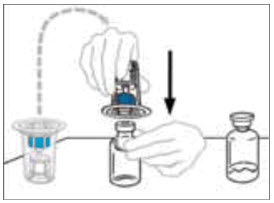
Turn the package with the Mix2Vial device upside down and place it over the top of the diluent vial. Firmly insert the blue plastic spike of the device into the center of the diluent vial stopper by pushing straight down. Grip the package at its edge and lift it off the Mix2Vial device. Be careful not to touch the clear plastic spike. The diluent vial now has the Mix2Vial device connected to it and is ready to be connected to the VONVENDI vial.
|
|
To connect the diluent vial to the VONVENDI vial, turn the diluent vial over and place it on top of the vial containing VONVENDI concentrate. Fully insert the clear plastic spike into the VONVENDI vial stopper by firmly pushing straight down. This should be done right away to keep the liquid free of germs. The diluent will flow into the VONVENDI vial by vacuum. Verify that diluent transfer is complete. Do not use if vacuum has been lost.
|
|
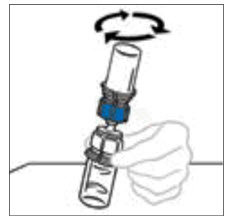
Gently and continuously swirl the connected vials or allow the reconstituted product to sit for 5 minutes then gently swirl to ensure the powder is completely dissolved. Do not shake. Shaking will adversely affect the product. Do not refrigerate after reconstitution.
Note: Some flakes or particles may remain in the reconstituted vial. The filter included in the Mix2Vial device will remove extraneous flakes or particles, and the resulting solution in the syringe should be clear and colorless. Do not use the solution in the syringe if it is cloudy or contains flakes or particles after filtration from the vial into the syringe.
|
|
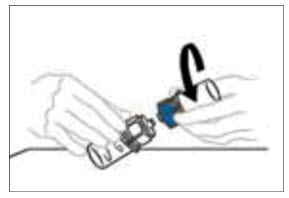
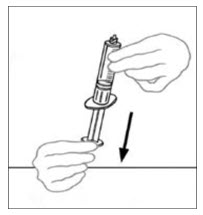
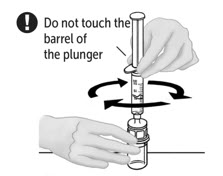
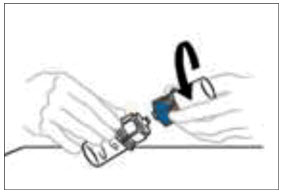
Disconnect the two sides of the Mix2Vial from each other by holding the clear plastic side of the Mix2Vial device attached to the VONVENDI vial with one hand and the blue plastic side of the Mix2Vial device attached to the diluent vial with the other hand. Turn the blue plastic side counterclockwise and gently pull the two vials apart. Do not touch the end of the plastic connector attached to the VONVENDI vial containing the dissolved product. Place the VONVENDI vial on a flat work surface. Discard the empty diluent vial.
|
|
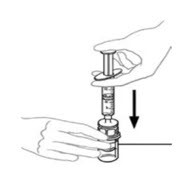
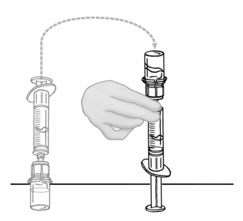
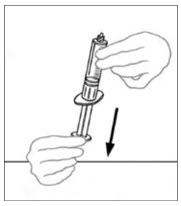
Draw air into the empty, sterile disposable plastic syringe by pulling back on the plunger. The amount of air should equal the amount of reconstituted VONVENDI that you will withdraw from the vial.
|
|
Leaving the VONVENDI vial (containing the dissolved product) on your flat work surface, connect the syringe to the clear plastic connector by attaching and turning the syringe clockwise (Figure A). Hold the vial with one hand and use the other hand to push the entire amount of air from the syringe into the vial (Figure B). The required amount of product will not be drawn into the syringe if all the air is not pushed into the vial.
|
Figure A |
Figure B |
|
|
|
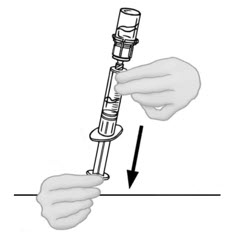
Flip connected syringe and VONVENDI vial so the vial is on top. Be sure to keep the syringe plunger pressed in. Draw the VONVENDI into the syringe by pulling plunger back slowly. Do not push and pull solution back and forth between syringe and vial. Doing so may harm the integrity of the product. Inspect syringe visually for particulate matter; the solution should be clear and colorless in appearance. If flakes or particles are seen, do not use the solution and notify your healthcare provider.
|
|
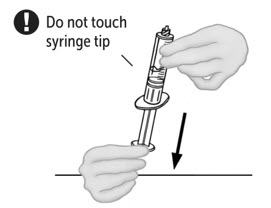
When ready to infuse, disconnect the syringe by turning it counterclockwise.
|
|
If your dose requires more than one vial of VONVENDI, reconstitute each vial using a separate Mix2Vial device following the reconstitution steps above (2 to 8).
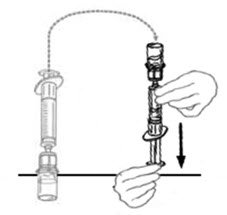
Up to two vials of VONVENDI may be pooled into a single syringe. If you have a second vial of reconstituted VONVENDI:
a.
Disconnect the syringe with reconstituted solution carefully from the first vial of VONVENDI by turning the syringe counterclockwise. Do not touch exposed connector.
|
|
b.
Pull the plunger back to draw air into the syringe containing the first vial of reconstituted VONVENDI. The amount of air added should equal the amount of reconstituted VONVENDI you will withdraw from the second vial. Do not touch exposed connector.
|
|
c.
Leave second vial of VONVENDI on flat surface and connect syringe by attaching to plastic connector and turning syringe clockwise.
|
|
d.
Flip connected syringe and second vial of VONVENDI so vial is on top (Figure C). Hold the vial with one hand and use the other hand to slowly push air into vial by pressing the syringe plunger (Figure D). Do not push any fluid from the syringe into the vial.
|
Figure C |
Figure D |
|
|
|
e.
Draw reconstituted VONVENDI from second vial of VONVENDI into syringe by slowly pulling back the plunger. Do not push any fluid from the syringe into the vial.
|
|
f.
Leave syringe attached to vial until ready to infuse to reduce risk of contamination. If your dose requires more than two vials of reconstituted VONVENDI, go back to Step 9 to draw your third vial into a NEW plastic syringe. No more than two vials of VONVENDI may be pooled into a single syringe. Pooling of more than two vials into a syringe may result in formation of filaments, which requires discarding of the solution in the syringe.
15.
If you need to infuse recombinant factor VIII, reconstitute recombinant factor VIII as instructed in the package insert for that product. Do not administer your recombinant factor VIII until you have infused your complete dose of VONVENDI. Always follow your healthcare provider’s specific directions.
Administration
1.
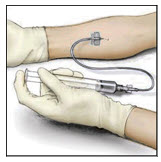
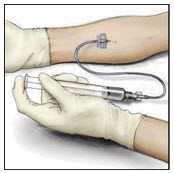
Attach the infusion needle to a syringe containing VONVENDI solution. For comfort, a winged (butterfly) infusion set is preferred. Point the needle up and remove any air bubbles by gently tapping the syringe with your finger and slowly and carefully pushing air out of the syringe and needle.
2.
Apply a tourniquet and get the injection site ready by wiping the skin well with a sterile alcohol swab (or other suitable sterile solution suggested by your healthcare provider or hemophilia center).
|
|
3.
Insert the needle into the vein and remove the tourniquet. Slowly infuse the VONVENDI. Do not infuse any faster than 4 mL per minute.
4.
Disconnect the empty syringe. If your dose requires multiple syringes, attach and administer each additional syringe of VONVENDI one at a time.
5.
Do not remove butterfly needle until all syringes have been infused and do not touch the Luer port that connects to the syringe.
6.
If your healthcare provider has prescribed recombinant factor VIII, administer recombinant factor VIII within 10 minutes after you have infused your complete dose of VONVENDI.
|
|
7.
Take the needle out of the vein and use sterile gauze to put pressure on the infusion site for several minutes.
8.
**Do not recap the needle.** Place the needle, syringe, and empty VONVENDI and diluent vial(s) in a hard-walled sharps container for proper disposal. Do not dispose of these supplies in ordinary household trash.
Important: Contact your healthcare provider or local hemophilia treatment center if you experience any problems.
Manufactured by:
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142
U.S. License No. 1898
VONVENDI is a registered trademark of Baxalta Incorporated.
Takeda and  are
registered trademarks of Takeda Pharmaceutical Company Limited.
are
registered trademarks of Takeda Pharmaceutical Company Limited.
Mix2Vial® is a registered trademark of West Pharma. Services IL, Ltd., a subsidiary of West Pharmaceutical Services, Inc.
Patented: see [www.takeda.com/en-us/patents](http://www.takeda.com/en- us/patents)
©2025 Takeda Pharmaceutical Company Limited. All rights reserved.
VON355
This Instructions for Use has been approved by the U.S. Food and Drug
Administration.
Revised: 9/2025
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Indications and Usage (1) |
9/2025 |
|
Dosage and Administration (2.1, 2.2) |
9/2025 |
|
Warnings and Precautions (5.1, 5.2, 5.3) |
9/2025 |
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosing Information
For intravenous use after reconstitution only.
- Each vial of VONVENDI is labeled with the actual amount of rVWF activity in International Units (IU), as measured with the Ristocetin cofactor assay (VWF:RCo).
- Individualize dosage and frequency according to the patient’s weight, type, location, and severity of the bleeding episodes/surgical intervention and monitoring of appropriate clinical and laboratory measures [see Warnings and Precautions (5.2, 5.3)].
- If the patient's baseline plasma FVIII:C level is below 40%, or is unknown, administer an approved recombinant (non-von Willebrand factor containing) factor VIII (rFVIII) with the first infusion of VONVENDI to achieve a hemostatic plasma level of FVIII:C.
- If an immediate rise in FVIII:C is not necessary, administer VONVENDI without rFVIII. Depending on the patient’s baseline FVIII:C level, a single infusion of VONVENDI is expected to increase endogenous FVIII:C activity above 40% within 6 hours.
- See rFVIII package insert for reconstitution and administration instructions.
- When repeated infusions are required, monitor factor VIII levels to determine if rFVIII is required with subsequent infusions.
2.2 Recommended Dosage
On-Demand Treatment and Control of Bleeding Episodes
- The recommended dose of VONVENDI is based on the type of bleeding episodes. Dosing guidelines for treatment of minor and major bleeds in adult and pediatric patients are provided in Table 1.
|
Bleeding Episodes |
Initial Dose |
Subsequent Dose |
|---|---|---|
| ||
|
Minor (e.g., readily managed epistaxis, oral bleeding, menorrhagia) |
40 to 50 IU/kg |
40 to 50 IU/kg every 8 to 24 hours |
|
Major***** (e.g., severe or refractory epistaxis, menorrhagia, GI bleeding, CNS trauma, hemarthrosis, or traumatic hemorrhage) |
50 to 80 IU/kg |
40 to 60 IU/kg every 8 to 24 hours for approximately 2 to 3 days |
- The initial dose of VONVENDI should achieve greater than 60% of von Willebrand factor (VWF) levels (based on VWF:RCo greater than 60 IU/dL) and an infusion of rFVIII should achieve factor VIII levels greater than 40% (FVIII:C greater than 40 IU/dL). In major bleeding episodes, maintain trough levels of VWF:RCo greater than 50% for as long as deemed necessary.
- Administer VONVENDI with rFVIII if the FVIII:C level is less than 40%, or is unknown, to control bleeding. The rFVIII dose should be calculated according to the difference between the patient’s baseline plasma FVIII:C level, and the desired peak FVIII:C level to achieve an appropriate plasma FVIII:C level based on the approximate mean recovery of 2 (IU/dL)/(IU/kg).
- Administer the complete dose of VONVENDI followed by rFVIII within 10 minutes.
Calculating Dose
VONVENDI dose [IU] = dose in [IU/kg] x body weight [kg]
In a major bleeding episode when baseline factor VIII level is unknown, rFVIII should be administered to achieve a target peak level of FVIII:C 80 to100 IU/dL, based on the approximate mean recovery of 2 (IU/dL)/(IU/kg). Refer to label for weight-based dose calculation of rFVIII that is used.
If expected VWF activity plasma levels are not attained, or if bleeding episode is not controlled with an appropriate dose, perform an assay that measures the presence of VWF or factor VIII inhibitors [see Warnings and Precautions (5.3)].
Perioperative Management of Bleeding
Elective Surgical Procedures
- A preoperative dose of VONVENDI may be administered 12 to 24 hours prior to surgery to allow the endogenous factor VIII levels to increase to at least 30 IU/dL (minor surgery) or 60 IU/dL (major surgery) before the loading dose (1 hour preoperative dose) of VONVENDI with or without rFVIII. Ensure baseline FVIII:C level is available prior to determining the need for 12 to 24 hour preoperative dose.
- FVIII:C level should also be assessed within 3 hours prior to initiating the surgical procedure. If the level is at the recommended minimum target levels (30 IU/dL for minor surgery and 60 IU/dL for major surgery), administer a dose of VONVENDI alone (without factor VIII treatment) within 1 hour prior to the procedure. If the FVIII:C level is below the recommended minimum target level, administer complete dose of VONVENDI followed by rFVIII within 10 minutes to raise VWF:RCo and FVIII:C.
- Refer to Table 2 for recommended VWF:RCo and FVIII:C target peak plasma levels and dosing guidelines for perioperative management of bleeding in adult and pediatric patients. When possible, measure incremental recovery (IR) for VONVENDI before surgery. For calculation of IR, measure baseline plasma VWF:RCo. Then infuse a dose of 50 IU/kg of VONVENDI. Measure VWF:RCo, 30 minutes after infusion of VONVENDI.
Use the following formula to calculate IR:
IR = [Plasma VWF:RCo at 30 minutes (IU/dL) – Plasma VWF:RCo at baseline (IU/dL)]/Dose (IU/kg)
Emergency Surgery
- A 12 to 24 hour preoperative dose may not be feasible in patients requiring emergency surgery. Baseline VWF:RCo and FVIII:C levels should be assessed within 3 hours prior to initiating the surgical procedure if it is feasible. If baseline VWF:RCo and FVIII:C are available, the loading dose (1 hour preoperative dose) can be calculated as the difference in the target peak and baseline plasma VWF:RCo levels divided by the IR. If the IR is not available, assume an IR of 2.0 IU/dL per IU/kg.
- If baseline VWF:RCo and FVIII:C are not available, as a general guidance a loading dose (1 hour preoperative dose) of VONVENDI, 40 to 60 IU/kg VWF:RCo, should be administered. Additionally, rFVIII at a dose of 30 to 45 IU/kg may be infused sequentially, preferably within 10 minutes after the VONVENDI infusion in patients whose factor VIII plasma levels already are (or are highly likely to be) less than 40 to 50 IU/dL for minor surgery or 80 to 100 IU/dL for major surgery.
Refer to Table 2 for recommended VWF:RCo and FVIII:C target peak plasma levels and dosing guidelines for perioperative management of bleeding.
Table 2: Recommended VWF:RCo and FVIII:C Target Peak Plasma Levels for the Perioperative Management of Bleeding|
Type of Surgery |
VWF:RCo Target Peak Plasma Level |
FVIII:C Target Peak Plasma Level* |
Calculation of rVWF Dose |
|---|---|---|---|
† ‡ ** Baseline plasma VWF:RCo is VWF:RCo activity level assessed within 3 hours prior to administration of 12 to 24 hours preoperative dose of VONVENDI. If no dose is administered 12 to 24 hours preoperatively, it’s recommended to use the VWF:RCo levels prior to surgery. | |||
|
Minor |
50 to 60 IU/dL |
40 to 50 IU/dL |
∆† VWF:RCo x BW (kg) /IR‡ |
|
Major |
100 IU/dL |
80 to 100 IU/dL |
∆† VWF:RCo x BW (kg) /IR‡ |
In the absence of available baseline FVIII:C, VWF:RCo and IR, it is recommended to use body weight-based dosing as outlined below in Table 3.
Table 3: Recommended Body Weight (BW) Based Dosing for the Perioperative Management of Bleeding|
Type of Surgery |
VWF:RCo (IU VWF:RCo/kg BW) |
VWF:RCo Target Peak Plasma Level |
FVIII:C (IU FVIII:C/ |
FVIII:C Target Peak Plasma Level |
|---|---|---|---|---|
|
Minor |
25 to 30 IU/kg |
50 to 60 IU/dL |
20 to 25 IU/kg |
40 to 50 IU/dL |
|
Major |
50 ± 10 IU/kg |
100 IU/dL |
40 to 50 IU/kg |
80 to 100 IU/dL |
- Monitor VWF:RCo and FVIII:C plasma levels starting 12 to 24 hours after surgery and at least every 24 hours in the perioperative period to adjust the dosing of VONVENDI or rFVIII levels. VWF:RCo and FVIII:C plasma levels should be monitored and the intra- and postoperative maintenance regimen should be individualized according to the pharmacokinetic (PK) results and intensity and duration of the hemostatic challenge.
- Refer to Table 4 for recommended VWF:RCo and FVIII:C target trough plasma levels and minimum duration of treatment for subsequent maintenance doses after surgery.
|
Type of Surgery |
VWF:RCo |
FVIII:C |
Minimum Duration of Treatment |
Frequency of Dosing | ||
|---|---|---|---|---|---|---|
|
up to 72 Hours Post-Surgery |
after 72 Hours Post-Surgery |
up to 72 Hours Post-Surgery |
after 72 Hours Post-Surgery | |||
|
Minor |
≥30 IU/dL |
|
|
|
48 hours |
Every 12 to 24 hours to every other day |
|
Major |
|
|
|
|
72 hours |
Every 12 to 24 hours to every other day |
Routine Prophylaxis in Adults
For initiation of prophylactic treatment, administer 40 to 60 IU of VONVENDI per kg of body weight twice weekly. Treat breakthrough bleeding as per the dosing guidelines in Table 1.
2.3 Preparation and Reconstitution
- Allow VONVENDI and Sterile Water for Injection (diluent) to reach room temperature.
- If the patient requires more than one vial of VONVENDI per injection, reconstitute each vial according to the following instructions.
- Some flakes or particles may remain in the reconstituted vial. The filter included in the Mix2Vial device will remove extraneous flakes or particles, and the resulting solution in the syringe should be clear and colorless. Do not use the solution in the syringe if it is cloudy or contains flakes or particles after filtration from the vial into the syringe.
Reconstitution
Remove the plastic caps from the VONVENDI and water for injection vials.
|
|
Clean the rubber stoppers with a sterile alcohol swab.
|
|
Peel back the cover of the Mix2Vial transfer device. To maintain sterility, leave the Mix2Vial device in the clear plastic packaging.
While firmly holding the diluent vial on a level surface, take the Mix2Vial in its plastic package and invert it over the diluent vial. Push the blue plastic cannula of the Mix2Vial firmly straight down through the rubber stopper. Carefully remove the plastic package leaving the Mix2Vial attached firmly to the diluent vial.
|
|
Hold the VONVENDI vial firmly on a level surface, quickly invert the diluent vial with the Mix2Vial attached and push the transparent plastic cannula end of the Mix2Vial firmly straight down through the stopper of the VONVENDI vial. The diluent will be drawn into the VONVENDI vial by the vacuum.
|
|
Verify that diluent transfer is complete. Do not use if vacuum has been lost.
With both vials still attached, gently swirl the vials or allow the reconstituted product to sit for 5 minutes then gently swirl to ensure the powder is completely dissolved.
Do not shake. Shaking will adversely affect the integrity of the product.
Note: Some flakes or particles may remain in the reconstituted vial. The
filter included in the Mix2Vial device will remove extraneous flakes or
particles, and the resulting solution in the syringe should be clear and
colorless. Do not use the solution in the syringe if it is cloudy or contains
flakes or particles after filtration from the vial into the syringe.
|
|
Once the content is completely dissolved, firmly hold both the transparent and blue parts of the Mix2Vial. Unscrew the Mix2Vial into two separate pieces and discard the empty diluent vial and the blue part of the Mix2Vial. Note: The Mix2Vial is intended for one-time use with a single vial of VONVENDI and diluent only. If the dose requires more than one vial of VONVENDI, reconstitute each vial separately.
Do not refrigerate after reconstitution.
|
|
2.4 Administration
For intravenous administration only.
- Administer VONVENDI immediately after reconstitution. If not, store at room temperature not to exceed 25°C (77°F) for up to 3 hours. Discard after 3 hours.
- No more than two vials of VONVENDI may be pooled into a single syringe. Pooling of more than two vials into a syringe may result in formation of filaments, which requires discarding of the solution in the syringe. If a patient is to receive more than one vial of VONVENDI, leave syringe attached to the vial or cover syringe tip with a suitable sterile cap until ready to infuse to reduce risk of contamination.
- Use plastic syringes with this product because proteins in the product tend to stick to the surface of glass syringes.
- Do not mix VONVENDI with other medicinal products.
Administration
Draw air into an empty, sterile disposable plastic syringe. The amount of air should equal the amount of reconstituted VONVENDI to be withdrawn from the vial.
|
|
Leaving the VONVENDI vial (containing the dissolved product) on your flat work surface, connect the syringe to the clear plastic connector by attaching and turning the syringe clockwise (Figure A). Hold the vial with one hand and use the other hand to push the entire amount of air from the syringe into the vial (Figure B). The required amount of product will not be drawn into the syringe if all the air is not pushed into the vial.
|
Figure A |
Figure B |
|
|
|
Flip connected syringe and VONVENDI vial so the vial is on top. Be sure to keep the syringe plunger pressed in. Draw the VONVENDI into the syringe by pulling plunger back slowly. Do not push and pull solution back and forth between syringe and vial. Doing so may harm the integrity of the product.
|
|
Inspect VONVENDI after filtration/withdrawal into the syringe for discoloration and particulate matter prior to administration. The solution should be clear or slightly opalescent in appearance. Do not administer if particulate matter, discoloration, or cloudiness is observed and notify Takeda Medical Information 1-877-TAKEDA-7 (1-877-825-3327).
When ready to infuse, firmly hold the barrel of the syringe (keeping the syringe plunger facing down) and detach the Mix2Vial from the syringe. Discard the Mix2Vial (transparent plastic part) and the empty VONVENDI vial. If a patient is to receive more than one vial of VONVENDI, the contents of up to two vials may be drawn into a single syringe. When pushing air into a second vial of VONVENDI to be pooled into a syringe, position the vial and connected syringe so that the vial is on top.
|
|
Clean the intended injection site with a sterile alcohol swab.
|
|
Attach a suitable infusion needle to the syringe. Infuse intravenously at a rate slow enough that ensures the comfort of the patient, up to a maximum of 4 mL per minute.
|
|
If tachycardia occurs, the injection speed must be reduced or the administration must be interrupted.
Dispose of any unused product or waste material in accordance with local requirements.
For intravenous use after reconstitution only.
On-Demand Treatment and Control of Bleeding Episodes
- For each bleeding episode, administer the first dose of VONVENDI with an approved recombinant (non-von Willebrand factor containing) factor VIII, if factor VIII baseline levels are below 40% or are unknown. (2.2)
- Initial dose is 40 to 80 International Units (IU) per kg body weight (BW). Adjust the dosage based on the extent and location of bleeding. (2.2)
|
Bleeding Episode |
Initial Dose |
Subsequent Dose |
|---|---|---|
|
Minor |
40 to 50 IU/kg |
40 to 50 IU/kg every 8 to 24 hours |
|
Major |
50 to 80 IU/kg |
40 to 60 IU/kg every 8 to 24 hours for approximately 2 to 3 days |
Perioperative Management of Bleeding
For Elective Surgical Procedure
- A dose of VONVENDI may be given 12 to 24 hours prior to surgery to allow the endogenous factor VIII levels to increase to at least 30 IU/dL (minor surgery) or 60 IU/dL (major surgery). (2.2)
- Assess FVIII:C levels within 3 hours prior to surgery. If the FVIII:C levels are at or above the recommended minimum target levels, administer a dose of VONVENDI alone within 1 hour prior to the procedure. If the FVIII:C levels are below the recommended minimum target levels, administer recombinant factor VIII in addition to VONVENDI to raise VWF:RCo and FVIII:C. (2.2)
For Emergency Surgery
- Assess baseline VWF:RCo and FVIII:C levels within 3 hours prior to surgery. If not available, use weight-based dosing calculation. (2.2)
- Administer VONVENDI 1 hour before surgery with or without recombinant factor VIII and adjust the dose to raise VWF:RCo and FVIII:C to adequate level. (2.2)
|
Type of Surgery |
Target Peak Plasma Level |
Calculation of rVWF Dose | |
|---|---|---|---|
|
VWF:RCo |
FVIII:C | ||
|
Minor |
50 to 60 IU/dL |
40 to 50 IU/dL |
∆ VWF:RCo x BW (kg)/IR |
|
Major |
100 IU/dL |
80 to 100 IU/dL |
∆ VWF:RCo x BW (kg)/IR |
- Continue to monitor the VWF:RCo and FVIII:C plasma levels after surgical procedure. (2.2)
Routine Prophylaxis in Adults
Initial dosage of VONVENDI is 40 to 60 IU/kg body weight to be administered twice weekly. Treat breakthrough bleeding as per dosing guidelines. (2.2)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
VONVENDI is available as a non-pyrogenic, white to off-white, lyophilized powder for reconstitution in single-dose vials containing nominally 650 or 1300 IU VWF:RCo/vial.
Each VONVENDI vial is labeled with the number of units of VWF:RCo expressed in IU, which are based on the current World Health Organization (WHO) standard for VWF concentrate.
VONVENDI is available as a lyophilized powder in single-dose vials containing nominally 650 or 1300 international units VWF:RCo. (3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Adequate and well-controlled studies with VONVENDI have not been conducted in pregnant women. Animal developmental and reproductive toxicity studies have not been conducted with VONVENDI. It is not known whether VONVENDI can cause fetal harm when administered to a pregnant woman or whether it can affect reproduction capacity.
The background risk of major birth defects and miscarriage in the indicated population is unknown; however, in the US population, the estimated background risk of major birth defects and miscarriage is 2 to 4% and 15 to 20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of VONVENDI in human milk, the effects on the breastfed infant, or the effects on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for VONVENDI and any potential adverse effects on the breastfed infant from VONVENDI or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of VONVENDI for on-demand treatment of bleeding episodes and perioperative management of bleeding have been established in pediatric patients. The use of VONVENDI was supported by evidence from Study 3 and Study 6 which included 26 pediatric patients 1 to 16 years of age [see Adverse Reactions (6.1) and Clinical Studies (14)].
8.5 Geriatric Use
Clinical studies with VONVENDI included 4 (3%) patients aged 65 years and above. No overall differences in safety or effectiveness were observed between these and younger patients.
DESCRIPTION SECTION
11 DESCRIPTION
VONVENDI is a purified rVWF expressed in Chinese Hamster Ovary (CHO) cells. VONVENDI is produced and formulated without the addition of any exogenous raw materials of human or animal origin in the cell culture, purification, or formulation of the final product. Proteins present in the final container product other than rVWF are trace quantities of mouse immunoglobulin (IgG, from the immunoaffinity purification), host cell (i.e., CHO) protein, rFurin (used to further process rVWF), and recombinant factor VIII (rFVIII).
Von Willebrand factor is a large multimeric glycoprotein that is normally found in plasma, and stored as ultra-large multimers in alpha-granules of platelets and intracellular organelles known as Weibel-Palade bodies, prior to secretion into the blood.1 Once the VWF is released to the blood stream and in contact with ADAMTS13 (a proteolytic enzyme in blood), it is cleaved to smaller sizes that can be detected with SDS agarose gels as multimer bands, representing the various species of VWF within the circulation. VONVENDI is rVWF that contains ultra-large multimers in addition to all of the multimers found in plasma as it is not exposed to proteolysis by ADAMTS13 during the manufacturing process.
VONVENDI is formulated as a sterile, non-pyrogenic, white to off-white friable powder for intravenous injection after reconstitution. VONVENDI in a single- dose vial contains nominally 650 or 1300 IU VWF:RCo.
The product contains no preservative. When reconstituted with the provided Sterile Water for Injection the final solution contains the following stabilizers and excipients (Table 6) in targeted amounts:
Table 6: Concentration of Stabilizer and Excipient after Reconstitution|
Stabilizer and Excipient |
Targeted Concentration for Nominal Strengths (650, 1300 IU) |
|---|---|
|
Tri-Sodium Citrate-dihydrate |
15 mM |
|
Glycine |
15 mM |
|
Mannitol |
20 g/L |
|
Trehalose-dihydrate |
10 g/L |
|
Polysorbate 80 |
0.1 g/L |
Each vial of VONVENDI is labeled with the specific number of units of VWF:RCo expressed in IU, which are based on the current World Health Organization (WHO) standard for VWF concentrate. After reconstitution of the lyophilized powder and filtration/withdrawal into a syringe, all dosage strengths yield a clear, colorless solution, free from particles.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
In VWD patients, VONVENDI acts 1) to promote hemostasis by mediating platelet adhesion to damaged vascular sub-endothelial matrix (e.g., collagen) and platelet aggregation, and 2) as a carrier protein for factor VIII, protecting it from rapid proteolysis. The adhesive activity of VWF depends on the size of its multimers, with larger multimers being the most effective in supporting interactions with collagen and platelet receptors.1 The binding capacity and affinity of VONVENDI to factor VIII in plasma is comparable to that of endogenous VWF, allowing for VONVENDI to reduce factor VIII clearance.
12.2 Pharmacodynamics
The PD of VWF following prophylactic treatment with VONVENDI in adults were investigated in a clinical trial (Study 5). In Prior OD adult patients, a single infusion of VONVENDI led to an increase of FVIII:C with peak levels observed approximately 24 hours post-infusion (mean [SD] dose: 50.1 [3.03] IU/kg). After 1-year repeat infusions of 50 ± 10 IU/kg VONVENDI twice weekly, the median (range) pre-dose FVIII:C increased from 2.0 (2.0 to 45.0) IU/dL (baseline after wash-out, N=12) to 11.0 (6.0 to 81.0) IU/dL (Month 12, N=9). The pre-dose FVIII:C (median [range] ≥11.0 [10.0 to 81.0] IU/dL) were observed over the prophylactic visits at Months 1, 2, 3, 6, 9 and 12. At Month 12, the median [range] Cmax and AUC(0-96 hours) of FVIII:C were 97.0 [63.0, 169.0] IU/dL and 5752 [2870, 11400] IU*h/dL (N=9), respectively.
The PD of VWF in 20 pediatric patients (aged less than 17 years) receiving on- demand therapy for bleeding episodes and treatment for surgical bleeds were evaluated using sparse sampling across three age groups (less than 6 years old, 6 years to less than 12 years old, and 12 years to less than 17 years old). Following a single infusion of VONVENDI at 50 (±5) IU/kg in pediatric patients, the median baseline corrected Cmax and AUC0-96 of FVIII:C were 64.5 IU/dL and 3379 IU*h/dL.
12.3 Pharmacokinetics
The PK profile of VONVENDI was determined based on data analyses from two clinical trials in adults (Studies 1 and 2) by assessment of VWF:RCo, VWF:Ag, and VWF:CB following a single dose. Patients were evaluated in the non- bleeding state.
Table 7 below summarizes the PK parameters of VONVENDI after infusions of 50 IU/kg (PK50) or 80 IU/kg VWF:RCo (PK80) VONVENDI in adult patients.
Table 7: Pharmacokinetic Assessment of VWF:RCo Following Single-Dose Infusion in Adults|
Parameter (unit) |
PK50 VONVENDI with ADVATE* |
PK50 VONVENDI |
PK80 VONVENDI |
|---|---|---|---|
|
Mean (SD) |
Mean (SD) |
Mean (SD) | |
|
AUC(0-inf) = area under plasma concentration-time curve from time 0 hour to infinite time post-infusion; IR = incremental recovery; CL = clearance; t1/2 = half-life. | |||
| |||
|
T1/2 |
19.3 (10.99) |
22.6 (5.34) |
19.1 (4.32) |
|
(h) |
10.8; 51.2 |
17.0; 37.2 |
11.8; 28.0 |
|
CL |
0.04 (0.028) |
0.02 (0.005) |
0.03 (0.009) |
|
([dL/kg]/h) |
0.01; 0.16 |
0.02; 0.04 |
0.02; 0.05 |
|
IR |
1.7 (0.62) |
1.9 (0.41) |
2.0 (0.39) |
|
([IU/dL]/([IU/kg]) |
1.0; 3.6 |
1.2; 2.7 |
1.4; 2.9 |
|
AUC0-inf |
1541.4 (554.31) |
2105.4 (427.51) |
2939.0 (732.72) |
|
(IU*h/dL) |
173.8; 2862.0 |
1334.0; 2813.3 |
1507.8; 4121.1 |
|
AUC0-inf/Dose |
33.4 (13.87) |
42.1 (8.31) |
36.8 (8.97) |
|
([IU*h/dL]/[IU/kg]) |
6.4; 70.4 |
27.8; 54.8 |
18.8; 50.4 |
The PK of VWF following prophylactic treatment with VONVENDI in adults were investigated in a clinical trial (Study 5). Steady state PK parameters of VWF:RCo are presented in Table 8 for patients who were previously treated on- demand (OD) with any VWF product prior to study entry (Prior OD group) and patients who were previously treated prophylactically with a plasma derived VWF product (Switch group) prior to study enrollment. The pharmacokinetics of VWF following single and multiple dosing (at Month 12) were similar in the Prior OD group. The PK of VWF following multiple dosing (at 12 months) were similar between Prior OD and Switch groups.
Table 8: Steady State Pharmacokinetic Assessment of VWF:RCo (Month 12; All Patients)|
Parameter |
Prior OD Group |
Switch Group |
|---|---|---|
|
AUC(0-96 hours) = area under plasma concentration-time curve from time 0 to 96 hours post-infusion; Cmax = maximum plasma concentration; IR = incremental recovery; CL = clearance; t1/2 = half-life; dose regimens for patients with VWD in Prior OD group were 41 to 56 IU/kg and for patients with VWD in Switch group were 24 to 77 IU/kg. | ||
| ||
|
T1/2 |
16.5 (4.13)* |
15.1 (5.78)† |
|
(h) |
10.9; 22.4 |
9.4; 22.9 |
|
CL |
0.04 (0.012)* |
0.04 (0.014)† |
|
([dL/kg]/h) |
0.02; 0.05 |
0.02; 0.06 |
|
IR at Cmax |
1.8 (0.5) |
1.9 (0.29) |
|
([IU/dL] / [IU/kg]) |
0.9; 2.7 |
1.6; 2.3 |
|
Cmax |
92.6 (37.1) |
102.9 (44.7) |
|
(IU/dL) |
41.6; 148.7 |
46.7; 176.6 |
|
Cmax/Dose |
1.9 (0.6) |
1.9 (0.3) |
|
([IU/dL]/[IU/kg]) |
0.9; 2.7 |
1.6; 2.3 |
|
AUC(0-96 hours) |
1561 (1298) |
1662 (675)‡ |
|
(IU*h/dL) |
460; 4460 |
1230; 2440 |
|
AUC(0- 96 hours)/Dose |
30.9 (23.4) |
27.5 (9.7)‡ |
|
([IU*h/dL]/[IU/kg]) |
9.8; 83.4 |
21.7; 38.7 |
The pharmacokinetics of VWF in pediatric patients with VWD were estimated based on PK modeling using sparse PK samples collected during a pediatric clinical trial (Study 3) across three age groups (less than 6 years old [N=5], 6 years to less than 12 years old [N=10], and 12 years to less than 17 years old [N=6]) receiving 50 ± 5 IU/kg rVWF:RCo VONVENDI (Table 9).
Table 9: Pharmacokinetic Assessment of VWF:RCo Following Single-Dose Infusion in Pediatric Patients|
Parameter (unit) |
PK50 VONVENDI | |||
|---|---|---|---|---|
|
Age Range |
<6 yrs |
6 yrs to <12 yrs |
12 yrs to <17 yrs |
Total |
|
AUC(0-inf) = area under plasma concentration-time curve from time 0 hour to infinite time post-infusion; IR = incremental recovery; CL = clearance; t1/2 = half-life. | ||||
|
T1/2 |
12.4 (2.90) |
14.5 (1.47) |
14.5 (1.27) |
14.0 (1.96) |
|
(h) |
8.96; 15.7 |
12.3; 16.7 |
13.0; 16.4 |
8.96; 16.7 |
|
CL |
0.08 (0.041) |
0.05 (0.016) |
0.05 (0.008) |
0.06 (0.026) |
|
([dL/kg]/h) |
0.048; 0.141 |
0.032; 0.077 |
0.034; 0.055 |
0.032; 0.141 |
|
Cmax |
69.4 (18.8) |
82.6 (20.8) |
80.8 (19.7) |
79.0 (19.9) |
|
(IU/dL) |
51.0; 90.3 |
53.7; 122 |
65.7; 115 |
51.0; 122 |
|
IR at Cmax |
1.25 (0.378) |
1.54 (0.378) |
1.57 (0.279) |
1.48 (0.360) |
|
([IU/dL]/[(IU/kg]) |
0.828; 1.78 |
1.06; 2.13 |
1.29; 2.06 |
0.828; 2.13 |
|
AUC0-inf |
1260 (654) |
1630 (882) |
1600 (867) |
1530 (805) |
|
(IU*h/dL) |
811; 2390 |
697; 3360 |
961; 2760 |
697; 3360 |
|
AUC0-inf/Dose |
25.6 (12.8) |
32.5 (18.1) |
33.1 (17.6) |
31.0 (16.3) |
|
([IU*h/dL]/[IU/kg]) |
16.1; 47.9 |
13.5; 68.5 |
19.0; 55.6 |
13.5; 68.5 |
12.6 Immunogenicity
The immunogenicity of VONVENDI was assessed in clinical trials by assessing the development of neutralizing antibodies against VWF and FVIII, as well as binding antibodies against VWF, Furin, Chinese hamster ovary (CHO) protein and mouse IgG. Of the 132 patients who received VONVENDI in the clinical trials, one patient who was treated with VONVENDI perioperatively developed treatment- emergent binding antibodies against VWF following a surgery, for whom no adverse events or lack of hemostatic efficacy was reported. No binding antibodies against potential impurities such as rFurin, CHO-protein or mouse IgG developed after treatment with VONVENDI.
Two patients included in the surgery study had pre-existing high-titer specific binding antibodies against VWF. The high-titer binding anti-VWF antibodies were associated with a significantly decreased VWF:Ag activity post-infusion of either plasma derived VWF (pdVWF) or rVWF and consequently, the decreased activity of VWF:RCo, VWF:CB and FVIII:C. This finding indicates the potential clinical significance of pre-existing binding (non-neutralizing) antibodies: VWD patients previously treated with pdVWF concentrates may be at risk to express a pre-existing binding antibody against VWF prior to first exposure to rVWF which could potentially result in a decreased hemostatic response to rVWF. Such patients could be managed clinically by administration of higher doses of rVWF based on the PK data for each individual patient.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In vitro and in vivo genotoxicity studies indicated no mutagenic potential for VONVENDI. Long-term animal studies to assess the carcinogenic potential of VONVENDI were not performed. Animal studies evaluating the developmental and reproductive toxicity of VONVENDI were not conducted.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
The efficacy of VONVENDI was evaluated in Study 1 (NCT00816660), Study 2 (NCT01410227), Study 3 (NCT02932618), Study 4 (NCT02283268), Study 5 (NCT02973087), and Study 6 (NCT03879135), as described below.
Study 1
This was a multicenter, single-blind, randomized, controlled, dose escalation study to evaluate the pharmacokinetics (PK), safety and tolerability of VONVENDI in patients with severe von Willebrand disease (VWD). The study enrolled patients with type 3 or severe type 1 VWD (VWF:RCo ≤10% and FVIII<20%), and who had a history of ≥25 days of exposure to VWF/FVIII factor concentrates.
A total of 31 patients received a single infusion of VONVENDI and rFVIII in a ratio of 1.3:1. VONVENDI was administered at a dose of either 2, 7.5, 20, or 50 IU/kg. The major outcome measures were PK parameters as described in section 12 above [see Clinical pharmacology (12.3)].
On-Demand Treatment and Control of Bleeding Episodes
Study 2 (Adults)
Hemostatic efficacy of VONVENDI was assessed in a multicenter, open-label trial investigating different dosing strategies with and without rFVIII (ADVATE) for on-demand treatment and control of bleeding episodes in adults diagnosed with von Willebrand disease. The study enrolled 37 patients who received treatment for on-demand treatment and control of bleeding episodes.
The demographic of the population were as follows: median age of 37 years (range 18 to 64), 20 patients (54%) were female, 32 patients (86%) were White, 5 patients (14%) were Asian and 2 patients (5%) were of Hispanic or Latino ethnicity. The types of VWD were as follows: Type 1 (n=2; 5%), Type 2A (n=5; 14%), Type 2N (n=1; 3%). and Type 3 (n=29; 78%).
Bleeding episodes were treated initially with an infusion of VONVENDI and ADVATE at a ratio of 1.3:1 respectively (i.e., 30% more VONVENDI than ADVATE), and subsequently with VONVENDI with or without ADVATE. ADVATE was given based on FVIII:C levels with a goal to achieve target plasma levels of greater than 40 IU/dL (40%) of FVIII:C.
A total of 192 bleeding episodes were treated with VONVENDI in 22/37 adult patients. The median cumulative dose of VONVENDI administered per bleeding episode (with or without ADVATE) was 48.2 IU/kg (90% CI, 43.9 to 50.2) IU/kg. The median number of VONVENDI infusions was 2 for major/severe (range: 1 to 3), 1 for moderate (range: 1 to 4), and 1 for minor bleeding episodes (range: 1 to 3). The median cumulative dose based on bleeding severity was 100 IU/kg (range, 57.5 to 135 IU/kg) for major (n=7), 52.7 IU/kg (range, 23.8 to 184.9 IU/kg) for moderate (n=61), and 43.3 IU/kg (range: 25.2 to 158.2 IU/kg) for minor bleeding episodes (n=122).
The primary efficacy endpoint was the number of patients with treatment success for control of bleeding episodes. Treatment success was defined as a mean efficacy rating score of less than 2.5 for all bleeding episodes treated with VONVENDI (with or without ADVATE) during the trial period, using a pre- specified 4-point rating scale comparing the prospectively estimated number of infusions needed to treat the bleeding episodes as assessed by the investigator to the actual number of infusions administered. The definitions for each of the 4-point rating scales are provided in Table 10.
Table 10: Definitions of 4-Point Rating Scales|
Rating |
Minor and Moderate Bleeding Events |
Major Bleeding Events |
|---|---|---|
|
Excellent |
Actual number of infusions ≤ estimated number of infusions required to treat
that bleeding episode. |
Actual number of infusions ≤ estimated number of infusions required to treat
that bleeding episode. |
|
Good |
1 to 2 infusions greater than estimated required to control that bleeding
episode. |
<1.5x infusions greater than estimated required to control that bleeding
episode. |
|
Moderate |
3 or more infusions greater than estimated used to control that bleeding
event. |
≥1.5x more infusions greater than estimated used to control that bleeding
event. |
|
None |
Severe uncontrolled bleeding or intensity of bleeding not changed. |
Severe uncontrolled bleeding or intensity of bleeding not changed. |
Secondary efficacy measures were the number of treated bleeding episodes with an efficacy rating of “excellent” or “good”, the number of infusions and number of units of VONVENDI, administered with or without ADVATE, per bleeding episode.
The primary efficacy assessment excluded patients with GI bleeds (n=2), and patients in whom the number of infusions required per bleeding episode was estimated retrospectively (n=2). The rate of patients (n=18) with treatment success was 100% (95% CI, 81.5 to 100). Sensitivity analyses of treatment success for bleeding episodes including GI bleeds and those bleeding episodes for which the investigator had to make retrospective assessment of the number of infusions required (n=22: 17 with type 3 VWD, 4 with type 2A VWD and 1 with type 2N VWD) confirmed the primary analysis, with a 100% treatment success rate for each scenario.
All bleeding episodes treated with VONVENDI and ADVATE or VONVENDI alone received an efficacy rating of excellent (97%) or good (3%). This was consistent across all degrees of severity.
Table 11 summarizes data obtained for number of infusions and efficacy rating per bleeding episode by location. Bleeding episodes of “Other” location (n=37) are not included in the table.
Table 11: Efficacy by Bleeding Episode Location (Adults)|
Bleeding Episodes by Location (n)* |
Median Number of Infusions (Range) |
Rating (%) |
|---|---|---|
| ||
|
Joint (n=59) |
1 (1 to 3) |
Excellent (97%) |
|
GI (n=6) |
1 (1 to 2) |
Excellent (83%) |
|
Mucosal: Genital Tract Female (n=32) |
1 (1 to 2) |
Excellent (97%) |
|
Mucosal: Nasopharyngeal (n=42) |
1 (1 to 2) |
Excellent (98%) |
|
Mucosal: Mouth and Oral Cavity (n=26) |
1 (1 to 4) |
Excellent (100%) |
Study 3 (Pediatrics)
Hemostatic efficacy of VONVENDI with or without ADVATE for on-demand treatment of non-surgical bleeding episodes was assessed in a multicenter, open-label trial in pediatric patients diagnosed with severe VWD. The study enrolled 18 patients who received treatment for on-demand bleeding episodes, including 3 patients who were 17 years old. The patients were followed for a duration of at least 12 months.
The demographics of the population were as follows: the median age was 11 years (range 1 to 17 years), 11 patients (61%) were female, 15 patients (94%) were White, 1 patient (6%) was of multiple races, and 1 patient (6%) was Hispanic or Latino. The types of VWD were as follows: Type 1 (n=2; 11%), Type 2A (n=3; 17%), Type 2B (n=2; 11%), and Type 3 (n=11; 61%).
A total of 28 bleeding episodes in 7 patients were treated with an initial dose of 40 to 60 IU/kg VONVENDI (median dose of 48 IU/kg; range 18 to 63 IU/kg) along with 30 to 45 IU/kg ADVATE (median dose of 33 IU/kg; range 9 to 45 IU/kg). A total of 76 bleeding episodes in 15 patients received an initial dose of 40 to 60 IU/kg VONVENDI (median dose 49 IU/kg; range 18 to 86 IU/kg) without ADVATE due to baseline FVIII level of at least 30%. In 8 patients, at least one additional dose of VONVENDI without ADVATE was administered in 18 bleeding episodes every 8 to 24 hours to maintain VWF:RCo and FVIII levels.
The primary efficacy endpoint was the number of patients with treatment success. Treatment success was defined as a mean efficacy rating score of less than 2.5 for all bleeding episodes using the pre-specified 4-point efficacy rating scale. Secondary efficacy outcome measures were assessed for each bleeding episode and included the number of treated nonsurgical bleeding episodes with an efficacy rating of “excellent” or “good”, the number of infusions, and VONVENDI and ADVATE consumption.
Table 12 summarizes efficacy rating and VONVENDI consumption by bleeding episode severity.
Table 12: Efficacy by Severity of Bleeding Episodes (Pediatric On- Demand)|
Severity of Bleeding Episodes | |||||
|---|---|---|---|---|---|
|
Mild |
Moderate |
Major/Severe |
Unknown |
Total | |
| |||||
|
Number of Patients with Bleeding Episodes |
13 |
13 |
2 |
3 |
18 |
|
Number of Treated Nonsurgical Bleeding Episodes (n)***** |
48 |
31 |
2 |
23 |
104 |
|
Hemostatic Efficacy Rating |
Excellent |
Excellent |
Excellent |
Excellent |
Excellent |
Table 13 summarizes efficacy rating by location of the bleeding episode.
Table 13: Efficacy by Bleeding Episode Location (Pediatric On-Demand)|
Bleeding Episodes by Location (n) |
Median Number of Infusions of rVWF (Range) |
Median Number of Infusions of ADVATE (Range) |
Rating (%) |
|---|---|---|---|
|
Joint |
1 (1 to 9) |
1 (1 to 1) |
Excellent (100%) |
|
Mucosal: Nasopharyngeal |
1 (1 to 3) |
1 (1 to 1) |
Excellent (100%) |
|
Mucosal: Mouth and Oral Cavity (n=14) |
1 (1 to 3) |
NA |
Excellent (93%) |
|
Mucosal: Genital Tract Female (n=12) |
1 (1 to 1) |
1 (1 to 1) |
Excellent (100%) |
|
Muscle/Skin/Soft Tissue (n=14) |
1 (1 to 3) |
1 (1 to 1) |
Excellent (100%) |
|
Multiple/Other |
1 (1 to 2) |
1 (1 to 1) |
Excellent (100%) |
Perioperative Management of Bleeding
Study 4 (Adults)
Hemostatic efficacy of VONVENDI was assessed in a prospective, open-label, multicenter trial to evaluate efficacy and safety of VONVENDI with or without ADVATE in elective surgical procedures in adults diagnosed with severe VWD and the patients were followed for 14 days after surgery. A total of 15 VWD patients completed the trial. Out of 15 patients, 10 underwent major surgeries and five underwent minor surgeries.
The demographics of the population were as follows: Median age was 40 (range, 20 to 70 years), 8 patients (53%) were female, 12 patients (80%) were White, 3 patients (20%) were Asian and 1 patient (7%) was Hispanic or Latino. The types of VWD were as follows: Type 1 (n=3; 20%), Type 2A (n=2; 13%), Type 2B (n=1; 7%), Type 2M (n=1; 7%) and Type 3 (n=8; 53%).
Major surgeries included orthopedic surgeries: total hip replacement, total knee replacement, knee endoprosthesis, ankle prosthesis, anterior cruciate ligament surgery and meniscectomy. Other major surgeries included laparoscopic cholecystectomy, laparoscopic cystectomy and complex dental extractions. Minor surgeries/procedures included nasopharyngoscopy, dental extractions, colonoscopy and radioisotope synovectomy.
All patients were administered a 12 to 24 hour preoperative dose of 40 to 60 IU/kg of VONVENDI to increase the factor VIII levels to target levels. Within 3 hours prior to surgery, the patients’ FVIII:C levels were assessed to ensure that target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries was achieved. Within 1 hour prior to surgery, patients received a dose of VONVENDI. ADVATE (recombinant Factor VIII) was administered based on FVIII:C levels performed 3 hours prior to surgery. VWF and factor VIII IR were used to guide the initial and subsequent doses.
The primary outcome measure was the overall hemostatic efficacy assessed 24 hours after the last perioperative VONVENDI infusion or at completion of study visit whichever occurred earlier using a 4-point ordinal efficacy scale outlined in Table 14 (“excellent”, “good”, “moderate” and “none”) based on estimated expected versus actual blood loss, transfusion requirements and postoperative bleeding and oozing. A rating of excellent or good was required to declare the outcome a success.
Table 14: Primary Efficacy Assessment|
Rating |
Overall Assessment of Hemostatic Efficacy 24 Hours after Last Perioperative IP Infusion or at Day 14 Completion Visit (Whatever Occurs Earlier) |
|---|---|
|
Excellent (1) |
Intra- and postoperative hemostasis achieved with rVWF with or without ADVATE was as good or better than that expected for the type of surgical procedure performed in a hemostatically normal patient. |
|
Good (2) |
Intra- and postoperative hemostasis achieved with rVWF with or without ADVATE was probably as good as that expected for the type of surgical procedure performed in a hemostatically normal patient. |
|
Moderate (3) |
Intra- and postoperative hemostasis with rVWF with or without ADVATE was clearly less than optimal for the type of procedure performed but was maintained without the need to change the rVWF concentrate. |
|
None (4) |
Patient experienced uncontrolled bleeding that was the result of inadequate therapeutic response despite proper dosing, necessitating a change of rVWF concentrate. |
Overall hemostatic efficacy for major and minor surgeries was 100% (15/15) with a 90% confidence interval of 81.9% to 100%. It was excellent for 60% of surgeries and good for 40% of surgeries.
Intraoperative hemostatic efficacy was a secondary endpoint. For major and minor surgeries, it was 100% with a 90% confidence interval of 81.9% to 100%. It was excellent for 73% of surgeries and good for 27% of surgeries.
For details regarding hemostatic efficacy for minor and major surgery, see Table 15.
Table 15: Overall Hemostatic Efficacy (Adults)|
Type of Surgery |
Excellent |
Good |
Moderate |
Total |
|---|---|---|---|---|
|
Minor |
4 |
1 |
0 |
5 |
|
Major |
5 |
5 |
0 |
10 |
Dosing was individualized based on IR results performed before surgery.
Mean total 12 to 24 preoperative dose was 50.9 IU/kg (median 55.0 IU/kg; range, 36.1 to 59.9 IU/kg).
Mean total loading dose (1 hour preoperative dose) per infusion was 38.6 IU/kg (median 35.8 IU/kg; range, 8.0 to 82.7 IU/kg). Major surgeries required a mean loading dose of 42.8 IU/kg (median 37.6 IU/kg; range, 15.7 to 82.7 IU/kg) in comparison with a mean loading dose of 30.2 IU/kg (median 34.2 IU/kg; range, 8.0 to 46.4 IU/kg) for minor surgeries.
For patients treated with VONVENDI (with or without ADVATE), the median total postoperative dose within the first 7 days after surgery was 114.2 IU/kg with a range of 23.8 to 318.9 IU/kg (n=13) and 76.2 IU/kg with a range of 23.8 to 214.4 IU/kg for the next 7 postoperative days (n=8).
Study 3 (Pediatrics)
The multicenter, open-label pediatric trial (Study 3) also assessed the efficacy of VONVENDI with or without ADVATE in the management of surgical bleeding from elective and emergency surgeries in pediatric patients diagnosed with severe von Willebrand disease. A total of 4 patients completed the study. Four minor (three elective and one emergency) surgeries were treated with VONVENDI in these four patients, aged 6 to 12 years.
Of the 4 patients who underwent surgeries, 2 were 12 to <17 years, and 2 were 6 to <12 years, and no subjects were <6 years. Three were male subjects with one female undergoing emergency surgery. All patients were White and /non- Hispanic or Latino and 1 had Type 1 VWD and 3 had Type 3 VWD.
Minor surgeries included second stage buccal mucosa hypospadias reconstruction, tunneled central venous catheter with subcutaneous port removal (emergency surgery), and circumcision.
The mean dose of VONVENDI administered preoperatively and postoperatively during the 4 surgeries was 94 IU/kg (mean, 1.8 preoperative infusions) and 117 IU/kg (mean, 2.3 postoperative infusions), respectively. A total of 5 infusions of ADVATE were administered for one surgery in one patient. This patient received one preoperative infusion and 4 postoperative infusions.
All 4 surgeries had overall and intraoperative hemostatic efficacy ratings of “Excellent” (95% CI [39.8, 100.0]). The blood loss rating (actual versus predicted blood loss) was “Excellent” for all 4 surgeries.
Routine Prophylaxis to Reduce the Frequency of Bleeding Episodes
Study 5 (Adults)
VONVENDI was assessed in a prospective, single arm, open-label, international multicenter study (Study 5) to evaluate efficacy, safety, PK and PD of prophylactic treatment in reducing the frequency of bleeding episodes in adult patients (age 18 years and older) diagnosed with VWD. Patients were enrolled into two treatment arms based on the treatment they received for management of bleeding prior to study entry consisting of a Prior on-demand (OD) group in which patients received on-demand treatment only and the Switch group in which patients had received prophylactic treatment with pdVWF. Efficacy was assessed based on the annualized bleeding rate for all bleeds, spontaneous bleeds and joint bleeds and was based on descriptive statistics.
The study enrolled 23 patients who received prophylactic treatment. Twenty-two efficacy evaluable patients received a median of 92.5 doses, 12 of these patients had previously received on demand treatment (Prior OD group) and 10 patients previously received prophylactic treatment with pdVWF (Switch group) prior to enrolling into this study. Nine patients in the Prior OD group and 8 patients in the Switch group completed the study which required 12 months of treatment.
The demographic of the population is as follows: Median age of patients in the study was 34 years (18 - 77 years), 12 patients (55%) were male, 21 patients (95%) were White and 19 patients (86%) were non-Hispanic or Latino. Of the 12 patients in the Prior OD group, one had severe Type 1, one had severe Type 2 VWD, and ten had severe Type 3 VWD. Of the 10 patients in the Switch group, one had severe Type 1, one had severe Type 2 VWD, and eight had severe Type 3 VWD.
Patients in the Prior OD group began treatment at 50 ± 10 IU/kg per infusion twice weekly and in the Switch group, the initial VONVENDI prophylactic treatment was based on matching (±10%) VWF content of the patient’s prior pdVWF prophylaxis regimen. The initial prophylactic regimen for 80% of Switch patients was also twice weekly, except for 2 patients; one started with a once weekly regimen of 80 IU/kg/infusion and the other started with 3-times-per- week regimen of 60 IU/kg/infusion. Dose adjustments up to 80 IU/kg per infusion and/or higher frequency up to 3 infusions per week were allowed in cases of breakthrough bleeding episodes.
The mean (SD) [range] average weight-adjusted VONVENDI prophylaxis dose per infusion was 52.2 (3.8) [44.8, 58.8] IU/kg for Prior OD patients and 52.2 (16.2) [24.4, 79.4] IU/kg for Switch patients. The mean (SD) number of prophylaxis infusions per week were 1.88 (0.7) for Prior OD and 1.85 (0.4) for Switch patients.
For the Prior OD group, treatment success was defined as at least 25% reduction in the ABR for spontaneous bleeding episodes requiring factor treatment from the patient’s historical to the on-study period (reduction success). A total of 11/12 (91.7%) Prior OD patients achieved ABR reduction success.
For the Switch group, treatment success was defined as achieving an on-study ABR for spontaneous bleeding episodes requiring factor treatment that was no greater than the patient’s historical ABR for treated bleeding episodes (preservation success). A total of 9/10 (90%) Switch patients achieved preservation success.
The efficacy parameters of VONVENDI as prophylactic treatment in adult patients are provided in Table 16.
Table 16: Efficacy of Routine Prophylaxis with VONVENDI|
Bleeding Event |
Pre-Study ABR*,† |
On-Study ABR* |
|---|---|---|
|
Median |
Median | |
| ||
|
Prior OD Patients (N = 12) | ||
|
Treated Spontaneous and Traumatic Bleeds |
4.0 |
0.0 |
|
All Spontaneous and Traumatic Bleeds‡ |
4.5 |
0.5 |
|
All Joint Bleeds‡,§ |
1.5 |
0.0 |
|
Switch Patients (N=10) | ||
|
Treated Spontaneous and Traumatic Bleeds |
0.0 |
0.0 |
|
All Spontaneous and Traumatic Bleeds‡ |
1.0 |
3.6 |
|
All Joint Bleeds‡ |
0.0 |
0.0 |
REFERENCES SECTION
15 REFERENCES
1
Stockschlaeder M, Schneppenheim R, Budde U, Update on von Willebrand factor multimers: focus on high-molecular-weight multimers and their role in hemostasis. Blood Coagul Fibrinolysis 2014, 25:206-216.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
VONVENDI is packaged with Sterile Water for Injection (sWFI), one Mix2Vial reconstitution device, one full prescribing physician insert, and one patient insert.
VONVENDI is available in single-dose vials that contain the following product strengths:
|
Color Code |
VWF:RCo Potency Range |
Carton NDC |
sWFI fill size |
|---|---|---|---|
|
Green |
450–850 IU per vial |
0944-7551-02 |
5 mL |
|
Dark Red |
900–1700 IU per vial |
0944-7553-02 |
10 mL |
The actual von Willebrand factor activity in international units is printed on the label of each VONVENDI vial and carton.
Components are not made with natural rubber latex.
Storage and Handling
- Store at refrigerated temperature 2°C to 8°C (36°F to 46°F) or room temperature not to exceed 30°C (86°F).
- Do not freeze.
- Store in the original box and protect from extreme exposure to light.
- Do not use beyond the expiration date printed on the VONVENDI vial label or carton.
- Do not use if the solution in the syringe is cloudy or contains flakes or particles after filtration from the vial into the syringe.
- Use reconstituted product immediately or within 3 hours after reconstitution.
- Discard any unused reconstituted product after 3 hours.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient and/or caregiver:
- To read the FDA-approved patient labeling (Patient Information and Instructions for Use).
- About early signs of hypersensitivity and infusion-related reactions, including anaphylactic shock, generalized urticaria, angioedema, chest tightness, hypotension, shock, lethargy, nausea, vomiting, paresthesia, pruritus, restlessness, wheezing and/or acute respiratory distress. Advise patients and/or caregivers to discontinue use of the product if these symptoms occur and seek immediate emergency treatment with resuscitative measures.
- To contact their physician or treatment center for further treatment and/or assessment if they experience a lack of clinical response to von Willebrand factor therapy, as this may be a manifestation of an inhibitor.
- To consult with their physicians or healthcare provider prior to travel. While traveling, advise patients and/or caregivers to bring an adequate supply of VONVENDI based on their current regimen of treatment.
SPL UNCLASSIFIED SECTION
Manufactured by:
Takeda Pharmaceuticals U.S.A., Inc.
Cambridge, MA 02142
U.S. License No. 1898
VONVENDI is a registered trademark of Baxalta Incorporated.
Takeda and  are
registered trademarks of Takeda Pharmaceutical Company Limited.
are
registered trademarks of Takeda Pharmaceutical Company Limited.
Mix2Vial® is a registered trademark of West Pharma. Services IL, Ltd., a subsidiary of West Pharmaceutical Services, Inc.
Patented: see [www.takeda.com/en-us/patents](http://www.takeda.com/en- us/patents)
©2025 Takeda Pharmaceutical Company Limited. All rights reserved.
VON355