Alkindi
These highlights do not include all the information needed to use ALKINDI SPRINKLE safely and effectively. See full prescribing information for ALKINDI SPRINKLE. ALKINDI SPRINKLE (hydrocortisone) oral granules Initial U.S. Approval: 1952
26c13a5f-7119-4c6a-bf10-fda4e07d7682
HUMAN PRESCRIPTION DRUG LABEL
Feb 28, 2024
Eton Pharmaceuticals, Inc.
DUNS: 080870465
Products 6
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Hydrocortisone
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Drug Labeling Information
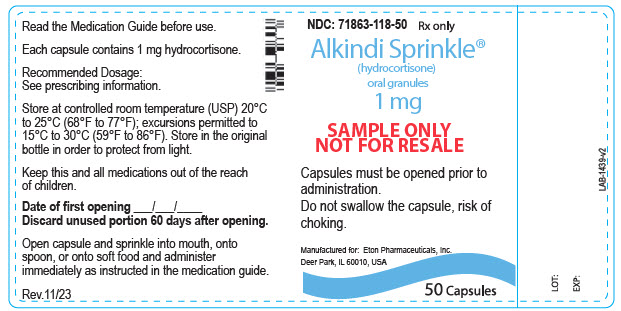
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - 1 mg Capsule Bottle Label
NDC: 71863-118-50
Rx only
Alkindi Sprinkle®
(hydrocortisone)
oral granules
1 mg
SAMPLE ONLY
NOT FOR RESALE
Capsules must be opened prior to
administration.
Do not swallow the capsule, risk of
choking.
Manufactured for: Eton Pharmaceuticals, Inc.
Deer Park, IL 60010, USA
50 Capsules
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
ALKINDI SPRINKLE is indicated as replacement therapy in pediatric patients with adrenocortical insufficiency.
ALKINDI SPRINKLE is a corticosteroid indicated as replacement therapy in pediatric patients with adrenocortical insufficiency. (1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
ALKINDI SPRINKLE is contraindicated in patients with hypersensitivity to hydrocortisone or to any of the ingredients in ALKINDI SPRINKLE. Anaphylactic reactions have occurred in patients receiving corticosteroids [see Adverse Reactions (6.2)].
- Hypersensitivity to hydrocortisone or to any of the ingredients in ALKINDI SPRINKLE. (4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following serious adverse reactions are described here and elsewhere in the label:
- Adrenal Crisis [see Warnings and Precautions (5.1)]
- Immunosuppression and Increased Risk of Infection with Use of a Dosage Greater Than Replacement [see Warnings and Precautions (5.2)]
- Growth Retardation [see Warnings and Precautions (5.3)]
- Cushing's Syndrome Due to Use of Excessive Doses of Corticosteroids [see Warnings and Precautions (5.4)]
- Decrease in Bone Mineral Density [see Warnings and Precautions (5.5)]
- Psychiatric Adverse Reactions [see Warnings and Precautions (5.6)]
- Ophthalmic Adverse Reactions [see Warnings and Precautions (5.7)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.8)]
- Risk of Kaposi's Sarcoma with Use of Dosage Greater Than Replacement [see Warnings and Precautions (5.9)]
- Vaccinations [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
ALKINDI SPRINKLE was evaluated in an uncontrolled, open-label, single-arm clinical study in 18 pediatric patients with adrenocortical insufficiency. Adrenocortical insufficiency was due to congenital adrenal hyperplasia in 17 patients and to hypopituitarism in one patient. All patients received at least one dose of ALKINDI SPRINKLE. The age ranged from 36 days to 5.7 years at start of treatment; 8 patients were female and 10 were male; 100% were White. Adverse reactions that were reported in two or more patients (≥ 11%) are shown in Table 1.
Table 1. Adverse Reactions Occurring in ≥11% of Pediatric Patients with Adrenocortical Insufficiency Treated with ALKINDI SPRINKLE for up to 29 Months|
Adverse Reactions |
N=18 n (%) |
|---|---|
|
Pyrexia |
10 (56) |
|
Gastroenteritis |
9 (50) |
|
Viral upper respiratory tract infection |
8 (44) |
|
Vomiting |
7 (39) |
|
Viral infection |
6 (33) |
|
Conjunctivitis |
5 (28) |
|
Otitis media viral |
3 (17) |
|
Tonsillitis |
3 (17) |
|
Body temperature increased |
2 (11) |
|
Bronchitis |
2 (11) |
|
Dental caries |
2 (11) |
|
Diarrhea |
2 (11) |
|
Genitourinary operation |
2 (11) |
|
Pharyngitis |
2 (11) |
|
Respiratory tract infection |
2 (11) |
|
Rhinitis |
2 (11) |
6.2 Postmarketing Experience
The following adverse reactions seen in pediatric and adult patients associated with the use of corticosteroids were identified in the literature and from postmarketing reports. Because some of these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Common adverse reactions for corticosteroids include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite and weight gain.
Allergic Reactions: Anaphylaxis, angioedema
Cardiovascular: Bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction, pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis
Dermatologic: Acne, allergic dermatitis, cutaneous and subcutaneous atrophy, dry scalp, edema, facial erythema, hyper or hypo-pigmentation, impaired wound healing, increased sweating, petechiae and ecchymoses, rash, sterile abscess, striae, suppressed reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria
Endocrine: Abnormal fat deposits, decreased carbohydrate tolerance, development of Cushingoid state, hirsutism, manifestations of latent diabetes mellitus and increased requirements for insulin or oral hypoglycemic agents in diabetics, menstrual irregularities, moon faces, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery or illness), suppression of growth in pediatric patients
Fluid and Electrolyte Disturbances: Fluid retention, potassium loss, hypertension, hypokalemic alkalosis, sodium retention
Gastrointestinal: Abdominal distention, elevation in serum liver enzymes levels (usually reversible upon discontinuation), hepatomegaly, hiccups, malaise, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, ulcerative esophagitis
General: Increased appetite and weight gain
Metabolic: Negative nitrogen balance due to protein catabolism
Musculoskeletal: Osteonecrosis of femoral and humeral heads, Charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, steroid myopathy, tendon rupture, vertebral compression fractures
Neurological: Arachnoiditis, convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudo- tumor cerebri) usually following discontinuation of treatment, insomnia, meningitis, mood swings, neuritis, neuropathy, paraparesis/paraplegia, paresthesia, personality changes, sensory disturbances, vertigo
Ophthalmic: Exophthalmos, glaucoma, increased intraocular pressure, posterior subcapsular cataracts, and central serous chorioretinopathy
Reproductive: Alteration in motility and number of spermatozoa
Common adverse reactions for corticosteroids include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite, and weight gain. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Eton Pharmaceuticals, Inc. at 1-855-224-0233 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Table 2. Drug Interactions with ALKINDI SPRINKLE|
CYP3A4 Inhibitors | |
|
Clinical Impact: |
Hydrocortisone is metabolized by cytochrome P450 3A4 (CYP3A4). Concomitant administration of inhibitors of CYP3A4 may lead to increases in serum concentrations of ALKINDI SPRINKLE and increase the risk of adverse reactions associated with the use of excessive doses. |
|
Intervention: |
Concomitant use of CYP3A4 inhibitors may require a decrease in the ALKINDI SPRINKLE dose. |
|
Examples: |
Anti-fungals: itraconazole, posaconazole, voriconazole |
|
CYP3A4 Inducers | |
|
Clinical Impact: |
Hydrocortisone is metabolized by cytochrome P450 3A4 (CYP3A4). Concomitant administration of inducers of CYP3A4 may lead to decreases in serum concentrations of ALKINDI SPRINKLE and increase the risk of adverse reactions, including adrenal crisis. |
|
Intervention: |
Concomitant use of CYP3A4 inducers may require an increase in the ALKINDI SPRINKLE dose. |
|
Examples: |
Anticonvulsants: phenytoin, carbamazepine and oxcarbazepine |
|
Estrogen and Estrogen Containing Products | |
|
Clinical Impact: |
Oral estrogen and estrogen-containing oral contraceptives may interact with hydrocortisone by increasing serum cortisol-binding globulin (CBG) concentration. Concomitant use may reduce the efficacy of ALKINDI SPRINKLE by binding and delaying or preventing absorption. |
|
Intervention: |
Concomitant use of estrogen/estrogen containing products may require an increase in the ALKINDI SPRINKLE dose. |
|
Antidiabetic Agents | |
|
Clinical Impact: |
Corticosteroids in supraphysiologic doses may increase blood glucose concentrations. |
|
Intervention: |
Use of ALKINDI SPRINKLE in supraphysiologic doses may require a dose adjustment of antidiabetic agents. |
|
Anticoagulant Agents | |
|
Clinical Impact: |
Concomitant use of warfarin and corticosteroids usually results in inhibition of response to warfarin, although there have been some conflicting reports. |
|
Intervention: |
Monitor coagulation indices in patients receiving ALKINDI SPRINKLE and concomitant warfarin to maintain the desired anticoagulant effect. |
|
Cyclosporine | |
|
Clinical Impact: |
Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with concurrent use. |
|
Intervention: |
Monitor patients receiving ALKINDI SPRINKLE and concomitant cyclosporine. |
|
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | |
|
Clinical Impact: |
Concomitant use of NSAIDs and corticosteroids increases the risk of gastrointestinal adverse reactions. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids; this could lead to decreased salicylate serum levels or increase the risk of salicylate toxicity when corticosteroid is withdrawn. |
|
Intervention: |
Monitor patients receiving ALKINDI SPRINKLE and concomitant NSAIDs. |
- CYP3A4 Inhibitors: concomitant administration may require a decrease in the ALKINDI SPRINKLE dose. (7)
- CYP3A4 Inducers: concomitant administration may require an increase in the ALKINDI SPRINKLE dose. (7)
- Estrogen and Estrogen Containing Products: concomitant administration may require an increase in the ALKINDI SPRINKLE dose. (7)
- Antidiabetic agents: excessive doses may increase blood glucose concentrations. Dose adjustment of antidiabetic agents may be required. (7)
- NSAIDs: concomitant administration increases risk of gastrointestinal adverse reactions. (7)
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Warnings and Precautions (5.2, 5.9, 5.10) |
02/2024 |
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
ALKINDI SPRINKLE oral granules are white to off-white granules contained within transparent capsules and are available as follows:
|
Strength |
Imprint on Capsules |
|---|---|
|
0.5 mg |
"INF-0.5" in red ink |
|
1 mg |
"INF-1.0" in blue ink |
|
2 mg |
"INF-2.0" in green ink |
|
5 mg |
"INF-5.0" in gray ink |
- Oral granules: 0.5 mg, 1 mg, 2 mg, 5 mg contained in capsules. (3)
OVERDOSAGE SECTION
10 OVERDOSAGE
Treatment of acute overdosage is by supportive and symptomatic therapy.
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Untreated adrenocortical insufficiency in pregnancy can result in a high rate of complications, including maternal mortality. The use of physiologic doses of hydrocortisone is not expected to cause major birth defects, miscarriage and adverse maternal and fetal outcomes. Available data from observational studies with hydrocortisone use in pregnancy have not identified a clear drug- associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
Data
Human Data
Available data from observational studies with hydrocortisone use in pregnant women have not identified a clear drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Evidence from published epidemiologic studies suggest that there may be a small increased risk of cleft lip with or without cleft palate associated with first trimester systemic corticosteroid use in pregnant patients. However, the data are limited and report inconsistent findings, and studies have important methodological limitations, including non-randomized design, retrospective data collection, lack of dose-response data and the inability to control for confounders, such as underlying maternal disease and use of concomitant medications. In addition, unlike other corticosteroids, hydrocortisone is enzymatically deactivated by the placenta and therefore, limits fetal exposure.
Animal Data
Corticosteroids have been shown to be teratogenic in many species when given in doses equivalent to the human dose. Animal studies in which corticosteroids have been given to pregnant mice, rats and rabbits without adrenocortical insufficiency have yielded an increased incidence of cleft palate in the offspring.
8.2 Lactation
Risk Summary
Cortisol is present in human milk. The use of hydrocortisone at a physiologic dose for adrenocortical insufficiency is not expected to adversely affect the breastfed infant or milk production. There are no data on the presence of hydrocortisone in breast milk, the effect on the breastfed infant or on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ALKINDI SPRINKLE and any potential adverse effects on the breastfed infant from ALKINDI SPRINKLE or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of ALKINDI SPRINKLE have been established in pediatric patients for replacement therapy of adrenocortical insufficiency and the information on this use is discussed throughout the labeling. Use of ALKINDI SPRINKLE in pediatric patients is supported by use in pediatric patients for adrenocortical insufficiency with another hydrocortisone product, along with supportive pharmacokinetic and safety data in 24 pediatric patients with adrenocortical insufficiency. No new adverse reactions were identified [see Adverse Reactions (6) and Clinical Pharmacology (12.3)]. ALKINDI SPRINKLE are oral granules contained within capsules that must be opened and not swallowed whole to administer the granules. Additionally, ALKINDI SPRINKLE granules should not be administered via nasogastric or gastric tubes as they may cause tube blockage [see Dosage and Administration (2.2)].
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Hydrocortisone is a glucocorticoid. Glucocorticoids, adrenocortical steroids, cause varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli.
12.2 Pharmacodynamics
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states.
12.3 Pharmacokinetics
Absorption
Following oral administration, a dose of ALKINDI SPRINKLE 4×5 mg was approximately 87% bioavailable when compared to intravenous hydrocortisone in dexamethasone-suppressed healthy adult male volunteers. The median time to peak serum concentration (Tmax) was 0.75 hours post-dose following oral administration.
In an open label, single dose study in 24 pediatric patients with adrenocortical insufficiency, ALKINDI SPRINKLE (1-4 mg based on body surface area) increased cortisol levels from baseline to median cortisol level 19.4 mcg/dL (range 12.5 – 52.4 mcg/dL) at Cmax (60 minutes post-dose).
Effect of Food
The coadministration of ALKINDI SPRINKLE with soft food (yogurt and fruit puree) has been studied in healthy adult male volunteers, where it was shown to be bioequivalent to administration of dry granules directly to the back of the tongue.
Distribution
90% or more of circulating hydrocortisone is reversibly bound to protein.
The binding is accounted for by two protein fractions. One, corticosteroid- binding globulin is a glycoprotein; the other is albumin.
Elimination
Hydrocortisone is metabolized in the liver and most body tissues to hydrogenated and degraded forms such as tetrahydrocortisone and tetrahydrocortisol which are excreted in the urine, mainly conjugated as glucuronides, together with a very small proportion of unchanged hydrocortisone.
The terminal half-life of hydrocortisone is about 1.5 hours following intravenous and oral dosing of hydrocortisone tablets and ALKINDI SPRINKLE in dexamethasone-suppressed healthy adult male volunteers.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No adequate studies in animals have been conducted with hydrocortisone to evaluate carcinogenic or mutagenic potential. Corticosteroids have been shown to impair fertility in male rats.
SPL UNCLASSIFIED SECTION
ALKINDI SPRINKLE is manufactured for Eton Pharmaceuticals, Inc. by Glatt Pharmaceutical Services GmbH & Co. KG Werner-Glatt-Strasse 1, Binzen, Baden- Wuerttemberg, 79589, Germany.
ALKINDI SPRINKLE**®** is a registered trademark of Diurnal Limited.
ALKINDI is covered by the following US patents: 9,649,280; 9,675,559; 9,717,740; and other patents in other countries internationally.
ALKINDI SPRINKLE is distributed in the USA by Eton Pharmaceuticals, Inc. under license from Diurnal Limited.
LAB-1413-v3
SPL MEDGUIDE SECTION
|
provider needs to change your child's dose of ALKINDI SPRINKLE. Especially tell your healthcare provider if your child:
Know the medicines your child takes. Keep a list of them to show your healthcare provider and pharmacist when your child gets a new medicine. |
|
How should I give ALKINDI SPRINKLE?
|
|
What are the possible side effects of ALKINDI SPRINKLE? ALKINDI SPRINKLE may cause serious side effects, including: *See "What is the most important information I should know about ALKINDI SPRINKLE?" ***Infections.**Taking too much ALKINDI SPRINKLE can increase the risk of infections. Tell your healthcare provider if your child has any of these symptoms: * fever o stomach area (abdominal) pain * cough o diarrhea * flu-like symptoms ***Slowed growth in children.**Taking too much ALKINDI SPRINKLE and taking it for long periods of time can affect your child's growth. Tell your healthcare provider if you are worried about your child's growth. Your healthcare provider will change the dose depending on your child's size. ***Cushing's syndrome.**Taking too much ALKINDI SPRINKLE and taking it for long periods of time can cause Cushing's syndrome. Tell your healthcare provider if your child has any of these symptoms: * weight gain o high blood o swelling o muscle o feeling sugar weakness depressed * slowed o high blood o bruising o red, round o mood swings growth in pressure easily face height ***Weak, brittle, or soft bones.**ALKINDI SPRINKLE can affect your child's bones. Your healthcare provider will change the dose depending on your child's size and will monitor your child's growth and bones. ***Changes in behavior.**Your child's behavior may change after starting or during treatment with ALKINDI SPRINKLE. Tell your healthcare provider right away if your child develops any changes inbehavior including: |
***Vision problems.**Tell your healthcare provider if your child develops blurred vision or other vision problems during treatment with ALKINDI SPRINKLE. Your healthcare provider may have your child see an eye doctor. ***Gastrointestinal problems.**ALKINDI SPRINKLE can affect your child's stomach or intestine. Tell your healthcare provider if your child has gastrointestinal illnesses such as stomach or intestinal ulcers, infections, or gastrointestinal surgery. The most common side effects of ALKINDI SPRINKLE include:
These are not all the possible side effects of ALKINDI SPRINKLE. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store ALKINDI SPRINKLE?
Keep ALKINDI SPRINKLE and all medicines out of the reach of children. |
|
General information about the safe and effective use of ALKINDI SPRINKLE. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ALKINDI SPRINKLE for a condition for which it was not prescribed. Do not give ALKINDI SPRINKLE to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about ALKINDI SPRINKLE that is written for health professionals. |
|
**What are the ingredients in ALKINDI SPRINKLE? Active ingredient: **hydrocortisone Inactive ingredients: granules: microcrystalline cellulose, hypromellose, magnesium stearate, ethyl cellulose. capsule: hypromellose printing ink: shellac, propylene glycol, concentrated ammonia solution. ALKINDI SPRINKLE is manufactured for Eton Pharmaceuticals, Inc. by Glatt Pharmaceutical Services GmbH & Co. KG Werner-Glatt-Strasse 1, Binzen, Baden- Wuerttemberg, 79589, Germany ALKINDI SPRINKLE**®**is a registered trademark of Diurnal Limited. ALKINDI is covered by the following US patents: 9,649,280; 9,675,559; 9,717,740; and other patents in other countries internationally. For more information, go to www.alkindisprinkle.com or call1-833-343-2500. |
DESCRIPTION SECTION
11 DESCRIPTION
ALKINDI SPRINKLE contains hydrocortisone, a corticosteroid, also known as cortisol. The chemical name of hydrocortisone is 11β,17α,21-trihydroxy- pregn-4-ene-3,20-dione and it has the chemical formula of C21H30O5, and molecular weight of 362 g∙mol−1. Hydrocortisone is a white or almost white powder soluble in the pH range of 1-7.
Structural formula of hydrocortisone:
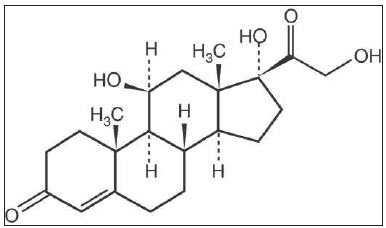
ALKINDI SPRINKLE are oral granules contained within hard capsules. The inactive ingredients in the granules are microcrystalline cellulose, hypromellose, magnesium stearate and ethyl cellulose and the capsule shell contains hypromellose. The printing ink contains shellac, propylene glycol and concentrated ammonia solution. The printing ink also contains red iron oxide, potassium hydroxide for 0.5 mg (red), indigotine for 1 mg (blue), indigotine, yellow iron oxide, titanium dioxide for 2 mg (green) and titanium dioxide, black iron oxide, potassium hydroxide for 5 mg (gray).
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
ALKINDI SPRINKLE oral granules are supplied as white to off-white granules in transparent capsules as follows:
|
Strength |
Imprint on Capsules |
Amount in Bottle |
NDC |
|---|---|---|---|
|
0.5 mg |
"INF-0.5" in red ink |
50 capsules |
71863-109-50 |
|
1 mg |
"INF-1.0" in blue ink |
50 capsules |
71863-110-50 |
|
2 mg |
"INF-2.0" in green ink |
50 capsules |
71863-111-50 |
|
5 mg |
"INF-5.0" in gray ink |
50 capsules |
71863-112-50 |
Store at controlled room temperature (USP) 20°C to 25°C (68°F to 77°F). Excursions permitted to 15°C to 30°C (59°F to 86°F). Store in the original bottle in order to protect from light.
Once the bottle has been opened, use the capsules within 60 days.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise patients and/or caregivers to read the FDA-approved patient labeling (Medication Guide).
Administration Information
Advise patients and/or caregivers that ALKINDI SPRINKLE is a granule formulation contained in a capsule. Do not swallow the capsule. Do not chew or crush the granules. Open the capsule and give the granules directly into the patient's mouth. Alternatively, sprinkle the granules onto soft food and give immediately as the taste masking cover can dissolve in as little as 5 minutes. Avoid wetting the capsule as this may cause some granules to stick to the capsule. Immediately following administration, take a sip of fluids to ensure all granules have been swallowed. Advise patients and/or caregivers to contact their healthcare provider if the full dose was not administered due to regurgitation or vomiting of granules as a repeat dose may be required [see Dosage and Administration (2.3)].
Adrenal Crisis
Inform patients and/or caregivers that undertreatment or sudden discontinuation of ALKINDI SPRINKLE or switching to ALKINDI SPRINKLE from another oral hydrocortisone formulation, may lead to adrenocortical insufficiency, adrenal crisis, and death. Inform the caregiver that potential dosing inaccuracy of the manipulated oral hydrocortisone formulation (e.g., split or crushed tablets, compounded formulations) may result in dosing differences when switching to ALKINDI SPRINKLE which may require dose adjustments. Advise caregivers to watch the patient for symptoms of adrenocortical insufficiency during the days after the switching to ALKINDI SPRINKLE. Inform patient and/or caregiver to contact their healthcare provider if they have symptoms of adrenocortical insufficiency, prolonged vomiting, are severely ill or are unable to take oral medications [see Warnings and Precautions (5.1)].
Immunosuppression and Increased Risk of Infections
Advise patients and/or caregivers that greater than replacement dosage of corticosteroids can suppress the immune system and increase the risk of infections. Instruct patients and/or caregivers to contact their healthcare provider if they develop any infections [see Warnings and Precautions (5.2)].
Growth Retardation
Discuss with caregivers that long-term use of corticosteroids in excessive doses may cause growth retardation in pediatric patients [see Warnings and Precautions (5.3)].
Cushing's Syndrome
Inform patients and/or caregivers that prolonged use of corticosteroids in supraphysiologic doses may cause Cushing's syndrome and that symptoms and signs include weight gain, decreased height velocity, hyperglycemia, hypertension, edema, easy bruising, muscle weakness, red round face, depression or mood swings [see Warnings and Precautions (5.4)].
Decrease in Bone Mineral Density
Inform patients and/or caregivers that corticosteroids decrease bone formation and increase bone resorption that may lead to osteoporosis [see Warnings and Precautions (5.5)].
Psychiatric Adverse Reactions
Advise patients and/or caregivers that corticosteroid use may be associated with severe psychiatric adverse reactions such as euphoria, mania, psychosis with hallucinations or depression. Instruct caregivers and/or patients to seek medical advice if psychiatric symptoms develop [see Warnings and Precautions (5.6)].
Ophthalmic Adverse Reactions
Inform patients and/or caregivers that ophthalmic effects such as cataract, glaucoma or central serous chorioretinopathy have been reported with prolonged use of high-dose corticosteroids. Instruct patients or caregivers to report any blurred vision or visual disturbances to their healthcare provider [see Warnings and Precautions (5.7)].
Gastrointestinal Adverse Reactions
Discuss with patients and/or caregivers that use of corticosteroids may increase risk of gastrointestinal perforation in certain gastrointestinal disorders [see Warnings and Precautions (5.8)].
Vaccination
Inform patients and/or caregivers that administration of live vaccine may be acceptable [see Warnings and Precautions (5.10)].
Excretion of Granules
ALKINDI SPRINKLE granules may sometimes be seen in stools since the center of the granule is not absorbed in the gut after the active substance has been released. Inform patients or caregivers that this does not mean the product is ineffective and they should not take another dose.
INSTRUCTIONS FOR USE SECTION
Instructions for Use
ALKINDI® SPRINKLE(ælˈkɪndi spr-en-kle)
(hydrocortisone) oral granules
Read this Instructions for Use before you start using ALKINDI SPRINKLE, and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your child's medical condition or treatment.
Important information you need to know before giving ALKINDI SPRINKLE
- ALKINDI SPRINKLE comes in a capsule that must be opened before use. *Do not let your child swallow the capsule. Small children may choke. *Do not let your child chew or crush the granules in the capsule. *Do not let the capsules get wet as this may make some of the granules stick to the capsule.
- Your healthcare provider will decide the right dose of ALKINDI SPRINKLE for your child. Follow your healthcare provider's instructions for the dose of ALKINDI SPRINKLE to give your child.
- Ask your healthcare provider or pharmacist if you are not sure how to prepare or give the prescribed dose of ALKINDI SPRINKLE to your child.
- Call your healthcare provider if granules come back up into your child's mouth (regurgitation) or your child has vomiting after swallowing ALKINDI SPRINKLE. Your child may not have received the full dose of ALKINDI SPRINKLE and another dose of ALKINDI SPRINKLE may be needed.
- Your child may sometimes pass the ALKINDI SPRINKLE granules in their stools (bowel movement). It does not mean that ALKINDI SPRINKLE is not working. Do not give your child another dose of ALKINDI SPRINKLE.
Supplies needed to give ALKINDI SPRINKLE:
- ALKINDI SPRINKLE capsule(s) for prescribed dose
- 1 spoon
- soft food such as yogurt or pureed fruit or sip of fluids such as water, milk, breastmilk or formula
Preparing and giving ALKINDI SPRINKLE:
Step 1: Check the expiration date on the ALKINDI SPRINKLE bottle. Do not use ALKINDI SPRINKLE after the expiration date on the bottle has passed.
Step 2: Remove the prescribed dose of ALKINDI SPRINKLE capsules from the bottle.
|
Step 3: Hold and Tap
Hold the capsule with the writing at the top. Tap the capsule to make sure the granules fall to the bottom. |
Step 4: Squeeze
Gently squeeze the bottom of the capsule to loosen the top of the capsule from the bottom. |
**Step 5:**Twist
|
Step 6: Giving ALKINDI SPRINKLE
ALKINDI SPRINKLE can be given (a) with food onto a spoon, (b) without food onto a spoon, or (c) directly into the child's mouth.
Do not add the granules to a fluid before giving ALKINDI SPRINKLE because it can result in less than the full dose given and it may leave a bitter taste in the mouth.
|
(a) With food onto a spoon
Pourall granules from each capsule directly onto a spoonful of cold or room temperature soft food (such as yogurt or fruit puree) and give right away. |
(b) Without food onto a spoon
Pourall granules directly onto a spoon and place them in the child's mouth. |
(c) Directly onto the child's tongue.
Pourall granules that make up the prescribed dose directly onto the child's tongue. |
Tap the capsule to make sure all granules are removed.
The ALKINDI SPRINKLE granules should be given and swallowed within 5 minutes to avoid a bitter taste.
Step 7: Give Fluids
After giving ALKINDI SPRINKLE, give a sip of fluids such as water, milk, breastmilk or formula right away to make sure all granules are swallowed.
Throwing Away (disposal of) ALKINDI SPRINKLE:
Ask your pharmacist how to throw away medicines you no longer use.
How should I store ALKINDI SPRINKLE?
- Store ALKINDI SPRINKLE at room temperature between 68°F to 77°F (20°C to 25°C).
- Store in the original bottle to protect from light.
- After the bottle has been opened, use the ALKINDI SPRINKLE capsules within 60 days.
Keep ALKINDI SPRINKLE and all medicines out of the reach of children.
ALKINDI SPRINKLE is manufactured for Eton Pharmaceuticals, Inc. by Glatt Pharmaceutical Services GmbH & Co. KG Werner-Glatt-Strasse 1, Binzen, Baden- Wuerttemberg, 79589, Germany
ALKINDI® is a registered trademark of Diurnal Limited.
ALKINDI is covered by the following US patents: 9,649,280; 9,675,559; 9,717,740; and other patents in other countries internationally.
For more information, go to www.alkindisprinkle.com or call 1-833-343-2500.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Revised: 12/2022



 Carefully twist off
the top of the capsule.
Carefully twist off
the top of the capsule.

