DIMETHYL FUMARATE
These highlights do not include all the information needed to use DIMETHYL FUMARATE DELAYED-RELEASE CAPSULES safely and effectively. See full prescribing information for DIMETHYL FUMARATE DELAYED-RELEASE CAPSULES. DIMETHYL FUMARATE delayed-release capsules, for oral use Initial U.S. Approval: 2013
b856ac70-71cd-477b-95b1-0a6132c260e8
HUMAN PRESCRIPTION DRUG LABEL
Feb 19, 2024
Camber Pharmaceuticals, Inc.
DUNS: 826774775
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
DIMETHYL FUMARATE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (23)
DIMETHYL FUMARATE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (23)
dimethyl fumarate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Dimethyl Fumarate Delayed-Release Capsules - 30-Day Starter Pack
****
**Dimethyl Fumarate Delayed-Release Capsules - 120 mg (14 capsules container)
**
****
** Dimethyl Fumarate Delayed-Release Capsules - 120 mg (14 capsules carton)**

Dimethyl Fumarate Delayed-Release Capsules - 240 mg (60 capsules
container)
****
Dimethyl Fumarate Delayed-Release Capsules - 240 mg (60 capsules carton)

Dimethyl Fumarate Delayed-Release Capsules - 240 mg (46 capsules
container)
****
Dimethyl Fumarate Delayed-Release Capsules - 240 mg (46 capsules carton)

INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Dimethyl fumarate delayed-release capsules are indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Dimethyl fumarate delayed-release capsules are indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. ( 1)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Dimethyl fumarate delayed-release capsules are contraindicated in patients with known hypersensitivity to dimethyl fumarate or to any of the excipients of dimethyl fumarate delayed-release capsules. Reactions have included anaphylaxis and angioedema [see Warnings and Precautions ( 5.1)].
Known hypersensitivity to dimethyl fumarate or any of the excipients of dimethyl fumarate delayed-release capsules. ( 4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis and Angioedema
Dimethyl fumarate delayed-release capsules can cause anaphylaxis and angioedema after the first dose or at any time during treatment. Signs and symptoms have included difficulty breathing, urticaria, and swelling of the throat and tongue. Patients should be instructed to discontinue dimethyl fumarate delayed-release capsules and seek immediate medical care should they experience signs and symptoms of anaphylaxis or angioedema.
5.2 Progressive Multifocal Leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) has occurred in patients with
MS treated with dimethyl fumarate delayed-release capsules. PML is an
opportunistic viral infection of the brain caused by the JC virus (JCV) that
typically only occurs in patients who are immunocompromised, and that usually
leads to death or severe disability. A fatal case of PML occurred in a patient
who received dimethyl fumarate delayed-release capsules for 4 years while
enrolled in a clinical trial. During the clinical trial, the patient
experienced prolonged lymphopenia (lymphocyte counts predominantly <0.5x10 9/L
for 3.5 years) while taking dimethyl fumarate delayed-release capsules [see Warnings and Precautions (5.4)]. The patient had no other identified systemic
medical conditions resulting in compromised immune system function and had not
previously been treated with natalizumab, which has a known association with
PML. The patient was also not taking any immunosuppressive or immunomodulatory
medications concomitantly.
PML has also occurred in the postmarketing setting in the presence of
lymphopenia (<0.9x10 9/L). While the role of lymphopenia in these cases is
uncertain, the PML cases have occurred predominantly in patients with
lymphocyte counts <0.8x10 9/L persisting for more than 6 months.
At the first sign or symptom suggestive of PML, withhold dimethyl fumarate
delayed-release capsules and perform an appropriate diagnostic evaluation.
Typical symptoms associated with PML are diverse, progress over days to weeks,
and include progressive weakness on one side of the body or clumsiness of
limbs, disturbance of vision, and changes in thinking, memory, and orientation
leading to confusion and personality changes.
MRI findings may be apparent before clinical signs or symptoms. Cases of PML,
diagnosed based on MRI findings and the detection of JCV DNA in the
cerebrospinal fluid in the absence of clinical signs or symptoms specific to
PML, have been reported in patients treated with other MS medications
associated with PML. Many of these patients subsequently became symptomatic
with PML. Therefore, monitoring with MRI for signs that may be consistent with
PML may be useful, and any suspicious findings should lead to further
investigation to allow for an early diagnosis of PML, if present. Lower PML-
related mortality and morbidity have been reported following discontinuation
of another MS medication associated with PML in patients with PML who were
initially asymptomatic compared to patients with PML who had characteristic
clinical signs and symptoms at diagnosis. It is not known whether these
differences are due to early detection and discontinuation of MS treatment or
due to differences in disease in these patients.
5.3 Herpes Zoster and Other Serious Opportunistic Infections
Serious cases of herpes zoster have occurred with dimethyl fumarate delayed-
release capsules, including disseminated herpes zoster, herpes zoster
ophthalmicus, herpes zoster meningoencephalitis, and herpes zoster
meningomyelitis. These events may occur at any time during treatment. Monitor
patients on dimethyl fumarate delayed-release capsules for signs and symptoms
of herpes zoster. If herpes zoster occurs, appropriate treatment for herpes
zoster should be administered.
Other serious opportunistic infections have occurred with dimethyl fumarate
delayed-release capsules, including cases of serious viral (herpes simplex
virus, West Nile virus, cytomegalovirus), fungal (Candida and Aspergillus),
and bacterial (Nocardia, Listeria monocytogenes, Mycobacterium tuberculosis)
infections. These infections have been reported in patients with reduced
absolute lymphocyte counts (ALC) as well as in patients with normal ALC. These
infections have affected the brain, meninges, spinal cord, gastrointestinal
tract, lungs, skin, eye, and ear. Patients with symptoms and signs consistent
with any of these infections should undergo prompt diagnostic evaluation and
receive appropriate treatment.
Consider withholding dimethyl fumarate delayed-release capsules treatment in
patients with herpes zoster or other serious infections until the infection
has resolved [see Adverse Reactions ( 6.2)].
5.4 Lymphopenia
Dimethyl fumarate delayed-release capsules may decrease lymphocyte counts. In the MS placebo-controlled trials, mean lymphocyte counts decreased by approximately 30% during the first year of treatment with dimethyl fumarate delayed-release capsules and then remained stable. Four weeks after stopping dimethyl fumarate delayed-release capsules, mean lymphocyte counts increased but did not return to baseline. Six percent (6%) of dimethyl fumarate delayed- release capsules patients and <1% of placebo patients experienced lymphocyte counts <0.5x10 9/L (lower limit of normal 0.91x10 9/L). The incidence of infections (60% vs 58%) and serious infections (2% vs 2%) was similar in patients treated with dimethyl fumarate delayed-release capsules or placebo, respectively. There was no increased incidence of serious infections observed in patients with lymphocyte counts <0.8x10 9/L or <0.5x10 9/L in controlled trials, although one patient in an extension study developed PML in the setting of prolonged lymphopenia (lymphocyte counts predominantly <0.5x10 9/L for 3.5 years) [see Warnings and Precautions ( 5.2)].
Incontrolledand uncontrolled clinical trials, 2% of patients experienced prolonged, severe lymphopenia, (defined as lymphocyte counts <0.5 x 10 9/L for at least six months); in this group of patients, themajorityof lymphocyte counts remained <0.5x10 9/L with continued therapy. In these patients with prolonged,severelymphopenia, the median time for lymphocyte counts to return to normal after discontinuing dimethyl fumarate delayed-releasecapsuleswas 96.0 weeks.
In thesecontrolledand uncontrolled clinical studies, among patients who did not experience prolonged, severe lymphopenia during treatment, the median times forlymphocytecounts to return to normal after discontinuing dimethyl fumarate delayed-release capsules were as follows:
• 4.3weeksin patients with mild lymphopenia (lymphocyte count ≥0.8x10 9/L) at
discontinuation,
• 10.0 weeks in patients with moderate lymphopenia (lymphocyte count 0.5 to
<0.8x10 9/L) at discontinuation, and
• 16.7weeksin patients with severe lymphopenia (lymphocyte count <0.5x10 9/L)
at discontinuation.
Dimethyl fumarate delayed-release capsules have not been studied in patients
with pre-existing low lymphocyte counts.
Obtain a CBC, including lymphocyte count, before initiating treatment with
dimethyl fumarate delayed-release capsules, 6 months after starting treatment,
and then every 6 to 12 months thereafter, and as clinically indicated.
Consider interruption of dimethyl fumarate delayed-release capsules in
patients with lymphocyte counts less than 0.5 x 10 9/L persisting for more
than six months. Given the potential for delayed recovery of lymphocyte
counts, continue to obtain lymphocyte counts until their recovery if dimethyl
fumarate delayed-release capsules are discontinued or interrupted due to
lymphopenia. Consider withholding treatment from patients with serious
infections until resolution. Decisions about whether or not to restart
dimethyl fumarate delayed-release capsules should be individualized based on
clinical circumstances.
5.5 Liver Injury
Clinically significant cases of liver injury have been reported in patients
treated with dimethyl fumarate delayed-release capsules in the postmarketing
setting. The onset has ranged from a few days to several months after
initiation of treatment with dimethyl fumarate delayed-release capsules. Signs
and symptoms of liver injury, including elevation of serum aminotransferases
to greater than 5-fold the upper limit of normal and elevation of total
bilirubin to greater than 2-fold the upper limit of normal have been observed.
These abnormalities resolved upon treatment discontinuation. Some cases
required hospitalization. None of the reported cases resulted in liver
failure, liver transplant, or death. However, the combination of new serum
aminotransferase elevations with increased levels of bilirubin caused by drug-
induced hepatocellular injury is an important predictor of serious liver
injury that may lead to acute liver failure, liver transplant, or death in
some patients.
Elevations of hepatic transaminases (most no greater than 3 times the upper
limit of normal) were observed during controlled trials [see Adverse Reactions ( 6.1)].
Obtain serum aminotransferase, alkaline phosphatase (ALP), and total bilirubin
levels prior to treatment with dimethyl fumarate delayed-release capsules and
during treatment, as clinically indicated. Discontinue dimethyl fumarate
delayed-release capsules if clinically significant liver injury induced by
dimethyl fumarate delayed-release capsules is suspected.
5.6 Flushing
Dimethyl fumarate delayed-release capsules may cause flushing (e.g., warmth, redness, itching, and/or burning sensation). In clinical trials, 40% of dimethyl fumarate delayed-release capsules treated patients experienced flushing. Flushing symptoms generally began soon after initiating dimethyl fumarate delayed-release capsules and usually improved or resolved over time. In the majority of patients who experienced flushing, it was mild or moderate in severity. Three percent (3%) of patients discontinued dimethyl fumarate delayed-release capsules for flushing and <1% had serious flushing symptoms that were not life-threatening but led to hospitalization. Administration of dimethyl fumarate delayed-release capsules with food may reduce the incidence of flushing. Alternatively, administration of non-enteric coated aspirin (up to a dose of 325 mg) 30 minutes prior to dimethyl fumarate delayed-release capsules dosing may reduce the incidence or severity of flushing [see Dosing and Administration ( 2.1) and Clinical Pharmacology ( 12.3)].
5.7 Serious Gastrointestinal Reactions
Seriousgastrointestinal reactions, including perforation, ulceration,
hemorrhage, and obstruction, some with fatal outcomes, have been reported in
the postmarketing setting with the use of fumaric acid esters, including
dimethyl fumarate delayed-release capsules, with or without concomitant
aspirin use. The majority of these events have occurred within 6 months of
fumaric acid ester treatment initiation. In controlled clinical trials, the
incidence of serious gastrointestinal adverse events was 1% in patients
treated with dimethyl fumarate delayed-release capsules; these events, none of
which were fatal, included vomiting (0.3%) and abdominal pain (0.3%) [see Adverse Reactions ( 6.1)] .
Monitor patients, promptly evaluate, and discontinue dimethyl fumarate
delayed-release capsules for new or worsening severe gastrointestinal signs
and symptoms.
• Anaphylaxis and Angioedema: Discontinue and do not restart dimethyl fumarate
delayed-release capsules if these occur. ( 5.1)
• Progressive Multifocal Leukoencephalopathy (PML): Withhold dimethyl fumarate
delayed-release capsules at the first sign or symptom suggestive of PML. (
5.2)
• Herpes Zoster and Other Serious Opportunistic Infections: Consider
withholding dimethyl fumarate delayed-release capsules in cases of serious
infection until the infection has resolved. ( 5.3)
• Lymphopenia: Obtain a CBC including lymphocyte count before initiating
dimethyl fumarate delayed-release capsules, after 6 months, and every 6 to 12
months thereafter. Consider interruption of dimethyl fumarate delayed-release
capsules if lymphocyte counts <0.5 x 10 9/L persist for more than 6 months. (
5.4)
• Liver Injury: Obtain serum aminotransferase, alkaline phosphatase, and total
bilirubin levels before initiating dimethyl fumarate delayed-release capsules
and during treatment, as clinically indicated. Discontinue dimethyl fumarate
delayed-release capsules if clinically significant liver injury induced by
dimethyl fumarate delayed-release capsules is suspected. ( 5.5)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following important adverse reactions are described elsewhere in labeling:
• Anaphylaxis and Angioedema [see Warnings and Precautions ( 5.1)]
• Progressive multifocal leukoencephalopathy [see Warnings and Precautions ( 5.2)]
• Herpes Zoster and Other Serious Opportunistic Infections [see Warnings and Precautions ( 5.3)]
• Lymphopenia [see Warnings and Precautions ( 5.4)]
• Liver Injury [see Warnings and Precautions ( 5.5)]
• Flushing [see Warnings and Precautions ( 5.6)]
• Serious Gastrointestinal Reactions [see Warnings and Precautions ( 5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse
reaction rates observed in clinical trials of a drug cannot be directly
compared to rates in the clinical trials of another drug and may not reflect
the rates observed in clinical practice.
In placebo-controlled and uncontrolled clinical studies, a total of 2513
patients have received dimethyl fumarate delayed-release capsules and been
followed for periods up to 13 years with an overall exposure of 11,318 person-
years. Approximately 1169 patients have received more than 5 years of
treatment with dimethyl fumarate delayed-release capsules, and 426 patients
have received at least 10 years of treatment with dimethyl fumarate delayed-
release capsules.
Adverse Reactions in Placebo-Controlled Trials
In the two well-controlled studies demonstrating effectiveness, 1529 patients
received dimethyl fumarate delayed-release capsules with an overall exposure
of 2244 person-years [see Clinical Studies ( 14)].
The adverse reactions presented in the table below are based on safety
information from 769 patients treated with dimethyl fumarate delayed-release
capsules 240 mg twice a day and 771 placebo-treated patients.
The most common adverse reactions (incidence ≥10% and ≥2% more than placebo)
for dimethyl fumarate delayed-release capsules were flushing, abdominal pain,
diarrhea, and nausea.****
** Table 1: Adverse Reactions in Study 1 and 2 reported for Dimethyl Fumarate
Delayed-Release Capsules 240 mg BID at ≥ 2% higher incidence than placebo**
|
Dimethyl Fumarate Delayed-Release**Capsules** |
Placebo | |
|
Flushing |
40 |
6 |
|
Abdominal pain |
18 |
10 |
|
Diarrhea |
14 |
11 |
|
Nausea |
12 |
9 |
|
Vomiting |
9 |
5 |
|
Pruritus |
8 |
4 |
|
Rash |
8 |
3 |
|
Albumin urine present |
6 |
4 |
|
Erythema |
5 |
1 |
|
Dyspepsia |
5 |
3 |
|
Aspartate aminotransferase increased |
4 |
2 |
|
Lymphopenia |
2 |
<1 |
Gastrointestinal
Dimethyl fumarate delayed-release capsules caused GI events (e.g., nausea,
vomiting, diarrhea, abdominal pain, and dyspepsia). The incidence of GI events
was higher early in the course of treatment (primarily in month 1) and usually
decreased over time in patients treated with dimethyl fumarate delayed-release
capsules compared with placebo. Four percent (4%) of patients treated with
dimethyl fumarate delayed-release capsules and less than 1% of placebo
patients discontinued due to gastrointestinal events. The incidence of serious
GI events was 1% in clinical trial patients treated with dimethyl fumarate
delayed-release capsules; these events, none of which were fatal, included
vomiting (0.3%) and abdominal pain (0.3%).
Hepatic Transaminases
An increased incidence of elevations of hepatic transaminases in patients
treated with dimethyl fumarate delayed-release capsules was seen primarily
during the first six months of treatment, and most patients with elevations
had levels < 3 times the upper limit of normal (ULN) during controlled trials.
Elevations of alanine aminotransferase and aspartate aminotransferase to ≥ 3
times the ULN occurred in a small number of patients treated with both
dimethyl fumarate delayed-release capsules and placebo and were balanced
between groups. There were no elevations in transaminases ≥ 3 times the ULN
with concomitant elevations in total bilirubin > 2 times the ULN.
Discontinuations due to elevated hepatic transaminases were < 1% and were
similar in patients treated with dimethyl fumarate delayed-release capsules or
placebo.
Eosinophilia
A transient increase in mean eosinophil counts was seen during the first 2
months of therapy.
6.2 Post Marketing Experience
The following adverse reactions have been identified during post-approval use
of dimethyl fumarate delayed-release capsules. Because these reactions are
reported voluntarily from a population of uncertain size, it is not always
possible to reliably estimate their frequency or establish a causal
relationship to drug exposure.
Gastrointestinal Disorders: Acute Pancreatitis; Gastrointestinal perforation,
ulceration, obstruction, and hemorrhage [see Warnings and Precautions ( 5.7)]
Hepatobiliary Disorders: Liver function abnormalities (elevations in
transaminases ≥ 3 times ULN with concomitant elevations in total bilirubin > 2
times ULN) [see Warnings and Precautions ( 5.5)]
Infections and Infestations: Herpes zoster infection and other serious
opportunistic infections [see Warnings and Precautions ( 5.3)]
Respiratory, Thoracic, and Mediastinal Disorders: Rhinorrhea
Skin and Subcutaneous: Alopecia
Most common adverse reactions (incidence ≥10% and ≥2% placebo) were flushing,
abdominal pain, diarrhea, and nausea. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Hetero Labs Limited at
1-866-495-1995 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient
Information).
Dosage
Inform patients that they will be provided two strengths of dimethyl fumarate
delayed-release capsules when starting treatment: 120 mg capsules for the
7-day starter dose and 240 mg capsules for the maintenance dose, both to be
taken twice daily. Inform patients to swallow dimethyl fumarate delayed-
release capsules whole and intact. Inform patients to not crush, chew, or
sprinkle capsule contents on food. Inform patients that dimethyl fumarate
delayed-release capsules can be taken with or without food [see Dosage and Administration ( 2.1)] .
Anaphylaxis and Angioedema
Advise patients to discontinue dimethyl fumarate delayed-release capsules and
seek medical care if they develop signs and symptoms of anaphylaxis or
angioedema [see Warnings and Precautions ( 5.1)].
Progressive Multifocal Leukoencephalopathy
Inform patients that progressive multifocal leukoencephalopathy (PML) has
occurred in patients who received dimethyl fumarate delayed-release capsules.
Inform the patient that PML is characterized by a progression of deficits and
usually leads to death or severe disability over weeks or months. Instruct the
patient of the importance of contacting their doctor if they develop any
symptoms suggestive of PML. Inform the patient that typical symptoms
associated with PML are diverse, progress over days to weeks, and include
progressive weakness on one side of the body or clumsiness of limbs,
disturbance of vision, and changes in thinking, memory, and orientation
leading to confusion and personality changes [see Warnings and Precautions ( 5.2)] .
Herpes Zoster and Other Serious Opportunistic Infections
Inform patients that herpes zoster and other serious opportunistic infections
have occurred in patients who received dimethyl fumarate delayed-release
capsules. Instruct the patient of the importance of contacting their doctor if
they develop any signs or symptoms associated with herpes zoster or other
serious opportunistic infections [see Warnings and Precautions ( 5.3)].
Lymphocyte Counts
Inform patients that dimethyl fumarate delayed-release capsules may decrease
lymphocyte counts. A blood test should be obtained before they start therapy.
Blood tests are also recommended after 6 months of treatment, every 6 to 12
months thereafter, and as clinically indicated [see Warnings and Precautions (5.4), Adverse Reactions ( 6.1)].
Liver Injury
Inform patients that dimethyl fumarate delayed-release capsules may cause
liver injury. Instruct patients treated with dimethyl fumarate delayed-release
capsules to report promptly any symptoms that may indicate liver injury,
including fatigue, anorexia, right upper abdominal discomfort, dark urine, or
jaundice. A blood test should be obtained before patients start therapy and
during treatment, as clinically indicated [see Warnings and Precautions ( 5.5)].
Flushing
Inform patients that flushing is one of the most common reactions, especially
at the initiation of therapy, and may decrease over time. Advise patients to
contact their healthcare provider if they experience persistent and/or severe
flushing. Advise patients experiencing flushing that taking dimethyl fumarate
delayed-release capsules with food or taking a non-enteric coated aspirin
prior to taking dimethyl fumarate delayed-release capsules may help [see Adverse Reactions ( 6.1)] .
Gastrointestinal (GI) Events
Inform patients that GI events (abdominal pain, diarrhea, and nausea) are some
of the most common adverse reactions, especially at the initiation of therapy,
and may decrease over time. Some patients may experience more severe GI
events. Advise patients to immediately contact their healthcare provider and
discontinue dimethyl fumarate delayed-release capsules if they experience
gastrointestinal bleeding (e.g., rectal bleeding, bloody diarrhea,
hematemesis) or other serious gastrointestinal adverse events (e.g., severe
abdominal pain, severe vomiting and/or diarrhea) [see Warnings and Precautions ( 5.7)] .
Pregnancy
Instruct patients that if they are pregnant or plan to become pregnant while
taking dimethyl fumarate delayed-release capsules they should inform their
physician.

Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854
By:HETERO****TM
HETERO LABS LIMITED
22-110, I.D.A., Jeedimetla,
Hyderabad - 500055, India.
Revised: 01/2024
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
Warnings and Precautions, Lymphopenia ( 5.4) 02/2023
Warnings and Precautions, Serious Gastrointestinal Reactions ( 5.7) 12/2023
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism by which dimethyl fumarate (DMF) exerts its therapeutic effect in multiple sclerosis is unknown. DMF and the metabolite, monomethyl fumarate (MMF), have been shown to activate the Nuclear factor (erythroid-derived 2)-like 2 (Nrf2) pathway in vitroand in vivoin animals and humans. The Nrf2 pathway is involved in the cellular response to oxidative stress. MMF has been identified as a nicotinic acid receptor agonist in vitro.
12.2 Pharmacodynamics
Potential to prolong the QT interval
In a placebo controlled thorough QT study performed in healthy subjects, there
was no evidence that dimethyl fumarate caused QT interval prolongation of
clinical significance (i.e., the upper bound of the 90% confidence interval
for the largest placebo-adjusted, baseline-corrected QTc was below 10 ms).
12.3 Pharmacokinetics
After oral administration of dimethyl fumarate delayed-release capsules,
dimethyl fumarate undergoes rapid presystemic hydrolysis by esterases and is
converted to its active metabolite, monomethyl fumarate (MMF). Dimethyl
fumarate is not quantifiable in plasma following oral administration of
dimethyl fumarate delayed-release capsules. Therefore, all pharmacokinetic
analyses related to dimethyl fumarate delayed-release capsules were performed
with plasma MMF concentrations. Pharmacokinetic data were obtained in subjects
with multiple sclerosis and healthy volunteers.
Absorption
The median T maxof MMF is 2 to 2.5 hours. The peak plasma concentration (C
max) and overall exposure (AUC) increased approximately dose proportionally in
the dose range studied (120 mg to 360 mg). Following administration of
dimethyl fumarate delayed-release capsules 240 mg twice a day with food, the
mean C maxof MMF was 1.87 mg/L and AUC was 8.21 mg.hr/L in MS patients.
A high-fat, high-calorie meal did not affect the AUC of MMF but decreased its
C maxby 40%. The T maxwas delayed from 2.0 hours to 5.5 hours. In this study,
the incidence of flushing was reduced by approximately 25% in the fed state.
Distribution
The apparent volume of distribution of MMF varies between 53 and 73 L in
healthy subjects. Human plasma protein binding of MMF is 27 to 45% and
independent of concentration.
Metabolism
In humans, dimethyl fumarate is extensively metabolized by esterases, which
are ubiquitous in the gastrointestinal tract, blood, and tissues, before it
reaches the systemic circulation. Further metabolism of MMF occurs through the
tricarboxylic acid (TCA) cycle, with no involvement of the cytochrome P450
(CYP) system. MMF, fumaric and citric acid, and glucose are the major
metabolites in plasma.
Elimination
Exhalation of CO 2is the primary route of elimination, accounting for
approximately 60% of the dimethyl fumarate delayed-release capsules dose.
Renal and fecal elimination are minor routes of elimination, accounting for
16% and 1% of the dose respectively. Trace amounts of unchanged MMF were
present in urine.
The terminal half-life of MMF is approximately 1 hour and no circulating MMF
is present at 24 hours in the majority of individuals. Accumulation of MMF
does not occur with multiple doses of dimethyl fumarate delayed-release
capsules.
Specific Populations
Body weight, gender, and age do not require dosage adjustment.
No studies have been conducted in subjects with hepatic or renal impairment.
However, neither condition would be expected to affect exposure to MMF and
therefore no dosage adjustment is necessary.
Drug Interaction Studies
No potential drug interactions with dimethyl fumarate or MMF were identified
in in vitroCYP inhibition and induction studies, or in P-glycoprotein studies.
Single doses of interferon beta-1a or glatiramer acetate did not alter the
pharmacokinetics of MMF. Aspirin, when administered approximately 30 minutes
before dimethyl fumarate delayed-release capsules, did not alter the
pharmacokinetics of MMF.
Oral Contraceptives
The coadministration of dimethyl fumarate with a combined oral contraceptive
(norelgestromin and ethinyl estradiol) did not elicit any relevant effects in
oral contraceptives exposure. No interaction studies have been performed with
oral contraceptives containing other progestogens.
Vaccines
A randomized, open-label study examined the concomitant use of dimethyl
fumarate delayed-release capsules and several non-live vaccines in adults 27
to 55 years of age with relapsing forms of MS (38 subjects undergoing
treatment with dimethyl fumarate delayed-release capsules at the time of
vaccination and 33 subjects undergoing treatment with non-pegylated interferon
at the time of vaccination). Concomitant exposure to dimethyl fumarate
delayed-release capsules did not attenuate antibody responses to tetanus
toxoid-containing vaccine, pneumococcal polysaccharide, and meningococcal
vaccines relative to antibody responses in interferon-treated patients. The
impact of these findings on vaccine effectiveness in this patient population
is unknown. The safety and effectiveness of live or live-attenuated vaccines
administered concomitantly with dimethyl fumarate delayed-release capsules
have not been assessed.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies of dimethyl fumarate (DMF) were conducted in mice and
rats. In mice, oral administration of DMF (25, 75, 200, and 400 mg/kg/day) for
up to two years resulted in an increase in nonglandular stomach (forestomach)
and kidney tumors: squamous cell carcinomas and papillomas of the forestomach
in males and females at 200 and 400 mg/kg/day; leiomyosarcomas of the
forestomach at 400 mg/kg/day in males and females; renal tubular adenomas and
carcinomas at 200 and 400 mg/kg/day in males; and renal tubule adenomas at 400
mg/kg/day in females. Plasma MMF exposure (AUC) at the highest dose not
associated with tumors in mice (75 mg/kg/day) was similar to that in humans at
the recommended human dose (RHD) of 480 mg/day.
In rats, oral administration of DMF (25, 50, 100, and 150 mg/kg/day) for up to
two years resulted in increases in squamous cell carcinomas and papillomas of
the forestomach at all doses tested in males and females, and in testicular
interstitial (Leydig) cell adenomas at 100 and 150 mg/kg/day. Plasma MMF AUC
at the lowest dose tested was lower than that in humans at the RHD.
Mutagenesis
Dimethyl fumarate (DMF) and monomethyl fumarate (MMF) were not mutagenic in
the in vitrobacterial reverse mutation (Ames) assay. DMF and MMF were
clastogenic in the in vitrochromosomal aberration assay in human peripheral
blood lymphocytes in the absence of metabolic activation. DMF was not
clastogenic in the in vivomicronucleus assay in the rat.
Impairment of Fertility
In male rats, oral administration of DMF (75, 250, and 375 mg/kg/day) prior to
and throughout the mating period had no effect on fertility; however,
increases in non-motile sperm were observed at the mid and high doses. The no-
effect dose for adverse effects on sperm is similar to the recommended human
dose (RHD) of 480 mg/day on a body surface area (mg/m 2) basis.
In female rats, oral administration of DMF (20, 100, and 250 mg/kg/day) prior
to and during mating and continuing to gestation day 7 caused disruption of
the estrous cycle and increases in embryolethality at the highest dose tested.
The highest dose not associated with adverse effects (100 mg/kg/day) is twice
the RHD on a mg/m 2basis.
Testicular toxicity (germinal epithelial degeneration, atrophy, hypospermia,
and/or hyperplasia) was observed at clinically relevant doses in mice, rats,
and dogs in subchronic and chronic oral toxicity studies of DMF, and in a
chronic oral toxicity study evaluating a combination of four fumaric acid
esters (including DMF) in rats.
13.2 Animal Toxicology and/or Pharmacology
Kidney toxicity was observed after repeated oral administration of dimethyl
fumarate (DMF) in mice, rats, dogs, and monkeys. Renal tubule epithelia
regeneration, suggestive of tubule epithelial injury, was observed in all
species. Renal tubular hyperplasia was observed in rats with dosing for up to
two years. Cortical atrophy and interstitial fibrosis were observed in dogs
and monkeys at doses above 5 mg/kg/day. In monkeys, the highest dose tested
(75 mg/kg/day) was associated with single cell necrosis and multifocal and
diffuse interstitial fibrosis, indicating irreversible loss of renal tissue
and function. In dogs and monkeys, the 5 mg/kg/day dose was associated with
plasma MMF exposures less than or similar to that in humans at the recommended
human dose (RHD).
A dose-related increase in incidence and severity of retinal degeneration was
observed in mice following oral administration of DMF for up to two years at
doses above 75 mg/kg/day, a dose associated with plasma MMF exposure (AUC)
similar to that in humans at the RHD.
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Dimethyl fumarate is available as hard gelatin delayed-release capsules containing 120 mg or 240 mg of dimethyl fumarate. The 120 mg capsules are light blue opaque size '0' hard gelatin capsules imprinted with 'H' on cap and 'D12' on body filled with white to off white tablets. The 240 mg capsules are white opaque size '0el' hard gelatin capsules imprinted with 'H' on cap and 'D15' on body filled with white to off white tablets.
Delayed-release capsules:120 mg and 240 mg ( 3)
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
The efficacy and safety of dimethyl fumarate delayed-release capsules were
demonstrated in two studies (Studies 1 and 2) that evaluated dimethyl fumarate
delayed-release capsules taken either twice or three times a day in patients
with relapsing-remitting multiple sclerosis (RRMS). The starting dose for
dimethyl fumarate delayed-release capsules was 120 mg twice or three times a
day for the first 7 days, followed by an increase to 240 mg twice or three
times a day. Both studies included patients who had experienced at least 1
relapse over the year preceding the trial or had a brain Magnetic Resonance
Imaging (MRI) scan demonstrating at least one gadolinium-enhancing (Gd+)
lesion within 6 weeks of randomization. The Expanded Disability Status Scale
(EDSS) was also assessed and patients could have scores ranging from 0 to 5.
Neurological evaluations were performed at baseline, every 3 months, and at
the time of suspected relapse. MRI evaluations were performed at baseline,
month 6, and year 1 and 2 in a subset of patients (44% in Study 1 and 48% in
Study 2).
Study 1: Placebo-Controlled Trial in RRMS
Study 1 was a 2-year randomized, double-blind, placebo-controlled study in
1234 patients with RRMS. The primary endpoint was the proportion of patients
relapsed at 2 years. Additional endpoints at 2 years included the number of
new or newly enlarging T2 hyperintense lesions, number of new T1 hypointense
lesions, number of Gd+ lesions, annualized relapse rate (ARR), and time to
confirmed disability progression. Confirmed disability progression was defined
as at least a 1 point increase from baseline EDSS (1.5 point increase for
patients with baseline EDSS of 0) sustained for 12 weeks.
Patients were randomized to receive dimethyl fumarate delayed-release capsules
240 mg twice a day (n=410), dimethyl fumarate delayed-release capsules 240 mg
three times a day (n=416), or placebo (n=408) for up to 2 years. The median
age was 39 years, median time since diagnosis was 4 years, and median EDSS
score at baseline was 2. The median time on study drug for all treatment arms
was 96 weeks. The percentages of patients who completed 96 weeks on study drug
per treatment group were 69% for patients assigned to dimethyl fumarate
delayed-release capsules 240 mg twice a day, 69% for patients assigned to
dimethyl fumarate delayed-release capsules 240 mg three times a day and 65%
for patients assigned to placebo groups.
Dimethyl fumarate delayed-release capsules had a statistically significant
effect on all of the endpoints described above and the 240 mg three times
daily dose showed no additional benefit over the dimethyl fumarate delayed-
release capsules 240 mg twice daily dose. The results for this study (240 mg
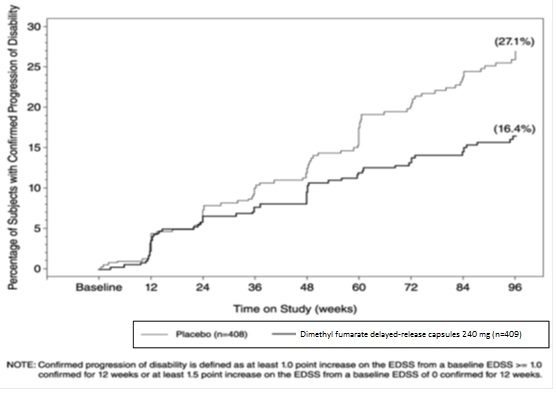
twice a day vs. placebo) are shown in Table 2 and Figure 1.
Table 2: Clinical and MRI Results of Study 1
|
Dimethyl Fumarate Delayed-Release****Capsules |
Placebo |
P-value | |
|
Clinical Endpoints |
N=410 |
N=408 | |
|
Proportion relapsing (primary endpoint) Relative risk reduction |
27% |
46% |
<0.0001 |
|
Annualized relapse rate |
0.172 |
0.364 |
<0.0001 |
|
Proportion with disability progression |
16% |
27% |
0.0050 |
|
Relative risk reduction |
38% | ||
|
MRI Endpoints |
N=152 |
N=165 | |
|
Mean number of new or newly enlarging T2 lesions over 2 years |
2.6 45% |
17 27% |
<0.0001 |
|
Number of Gd+ lesions at 2 years |
0.1 (0) |
1.8 (0) | |
|
Percentage of subjects with |
93% |
62% | |
|
Relative odds reduction (percentage) |
90% |
<0.0001 | |
|
Mean number of new T1 hypointense |
1.5 |
5.6 |
<0.0001 |
Figure 1: Time to 12-Week Confirmed Progression of Disability (Study 1)
Study 2: Placebo-Controlled Trial in RRMS
Study 2 was a 2-year multicenter, randomized, double-blind, placebo-controlled
study that also included an open-label comparator arm in patients with RRMS.
The primary endpoint was the annualized relapse rate at 2 years. Additional
endpoints at 2 years included the number of new or newly enlarging T2
hyperintense lesions, number of T1 hypointense lesions, number of Gd+ lesions,
proportion of patients relapsed, and time to confirmed disability progression
as defined in Study 1.
Patients were randomized to receive dimethyl fumarate delayed-release capsules
240 mg twice a day (n=359), dimethyl fumarate delayed-release capsules 240 mg
three times a day (n=345), an open-label comparator (n=350), or placebo
(n=363) for up to 2 years. The median age was 37 years, median time since
diagnosis was 3 years, and median EDSS score at baseline was 2.5. The median
time on study drug for all treatment arms was 96 weeks. The percentages of
patients who completed 96 weeks on study drug per treatment group were 70% for
patients assigned to dimethyl fumarate delayed-release capsules 240 mg twice a
day, 72% for patients assigned to dimethyl fumarate delayed-release capsules
240 mg three times a day and 64% for patients assigned to placebo groups.
Dimethyl fumarate delayed-release capsules had a statistically significant
effect on the relapse and MRI endpoints described above. There was no
statistically significant effect on disability progression. The dimethyl
fumarate delayed-release capsules 240 mg three times daily dose resulted in no
additional benefit over the dimethyl fumarate delayed-release capsules 240 mg
twice daily dose. The results for this study (240 mg twice a day vs. placebo)
are shown in Table 3.
Table 3: Clinical and MRI Results of Study 2
|
Dimethyl Fumarate Delayed-Release**Capsules** |
Placebo |
P-value | |
|
Clinical Endpoints |
N=359 |
N=363 | |
|
Annualized relapse rate |
0.224 |
0.401 |
<0.0001 |
|
Proportion relapsing |
29% |
41% |
0.0020 |
|
Proportion with disability progression |
13% |
17% |
0.25 |
|
MRI Endpoints |
N=147 |
N=144 | |
|
Mean number of new or newly enlarging T2 lesions over 2 years |
5.1 27% |
17.4 12% |
<0.0001 |
|
Number of Gd+ lesions at 2 years |
0.5 (0.0) |
2.0 (0.0) | |
|
Percentage of subjects with |
80% |
61% | |
|
Relative odds reduction (percentage) |
74% |
<0.0001 | |
|
Mean number of new T1 hypointense lesions over 2 years |
3.0 |
7.0 |
<0.0001 |
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Dimethyl fumarate is available as hard gelatin delayed-release capsules in two
strengths containing either 120 mg or 240 mg of dimethyl fumarate. The 120 mg
capsules are light blue opaque size '0' hard gelatin capsules imprinted with
'H' on cap and 'D12' on body filled with white to off white tablets. They are
available as follows:
30-day Starter Pack NDC 31722-680-60
7-day bottle 120 mg capsules, quantity 14
23-day bottle 240 mg capsules, quantity 46
120 mg capsules:
7-day bottle of 14 capsules NDC 31722-657-31
Blister Pack of 100 (10x10) unit dose capsules NDC 31722-657-32
The 240 mg capsules are white opaque size '0el' hard gelatin capsules
imprinted with 'H' on cap and 'D15' on body filled with white to off white
tablets. They are available as follows:
240 mg capsules:
23-day bottle of 46 capsules NDC 31722-658-31
30-day bottle of 60 capsules NDC 31722-658-32
Blister Pack of 100 (10x10) unit dose capsules NDC 31722-658-33
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Protect the capsules from light. Store in original container.
OVERDOSAGE SECTION
10 OVERDOSE
Cases of overdose with dimethyl fumarate delayed-release capsules have been
reported. The symptoms described in these cases were consistent with the known
adverse event profile of dimethyl fumarate delayed-release capsules.
There are no known therapeutic interventions to enhance elimination of
dimethyl fumarate nor is there a known antidote. In the event of overdose,
initiate symptomatic supportive treatment as clinically indicated.
DESCRIPTION SECTION
11 DESCRIPTION
Dimethyl fumarate delayed-release capsules contain dimethyl fumarate which is also known by its chemical name, dimethyl (E) butenedioate, (C 6H 8O 4). It has the following structure:
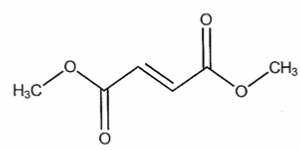
Dimethyl fumarate is a white to off white powder that is slightly soluble in
dimethylformamide with a molecular mass of 144.13.
Dimethyl fumarate is provided as hard gelatin delayed-release capsules for
oral administration, containing 120 mg or 240 mg of dimethyl fumarate
consisting of the following inactive ingredients: calcium silicate, colloidal
silicon dioxide, croscarmellose sodium, gelatin, magnesium stearate,
methacrylic acid and ethyl acrylate copolymer, methacrylic acid and methyl
methacrylate copolymer, poloxamer, polysorbate 80, silicified microcrystalline
cellulose, sodium bicarbonate, sodium lauryl sulfate, talc, titanium dioxide
and triethyl citrate. In addition, the 120 mg capsules also contain FD&C Blue
1, iron oxide black and iron oxide yellow.
The imprinting ink contains the following inactive ingredients: black iron
oxide, potassium hydroxide, propylene glycol, shellac and strong ammonia
solution.
SPL UNCLASSIFIED SECTION
Patient Information
|
Dimethyl Fumarate(dye meth il FYOO ma rate) Delayed-Release Capsules |
|
What are dimethyl fumarate delayed-release****capsules?
|
|
Who should not take dimethyl fumarate delayed-release****capsules?
|
|
Before taking and while you take dimethyl fumarate delayed- release****capsules, tell your doctor if you have or have had:
|
|
How should I take dimethyl fumarate delayed-release****capsules?
|
|
What are the possible side effects of dimethyl fumarate delayed- release****capsules? Dimethyl fumarate delayed-release****capsules may cause serious side effects
including:
***herpes zoster infections (shingles),**including central nervous system infections
*other serious infections
***serious gastrointestinal problems,**including bleeding, ulcers, blockage, and tears (perforation) of the stomach or intestines. Tell your healthcare provider right away if you have any of these symptoms during treatment: The most common side effects of dimethyl fumarate delayed- release****capsules include:
These are not all the possible side effects of dimethyl fumarate delayed- release capsules. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.For more information go to dailymed.nlm.nih.gov. |
|
General Information about the safe and effective use of dimethyl fumarate delayed-release****capsules
|
|
What are the ingredients in dimethyl fumarate delayed-release capsules?
By:HETERO****TM |
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 01/2024
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
The starting dose for dimethyl fumarate delayed-release capsules is 120 mg
twice a day orally. After 7 days, the dose should be increased to the
maintenance dose of 240 mg twice a day orally. Temporary dose reductions to
120 mg twice a day may be considered for individuals who do not tolerate the
maintenance dose. Within 4 weeks, the recommended dose of 240 mg twice a day
should be resumed. Discontinuation of dimethyl fumarate delayed-release
capsules should be considered for patients unable to tolerate return to the
maintenance dose. The incidence of flushing may be reduced by administration
of dimethyl fumarate delayed-release capsules with food. Alternatively,
administration of non-enteric coated aspirin (up to a dose of 325 mg) 30
minutes prior to dimethyl fumarate delayed-release capsules dosing may reduce
the incidence or severity of flushing [see Clinical Pharmacology ( 12.3)] .
Dimethyl fumarate delayed-release capsules should be swallowed whole and
intact. Dimethyl fumarate delayed-release capsules should not be crushed or
chewed, and the capsule contents should not be sprinkled on food. Dimethyl
fumarate delayed-release capsules can be taken with or without food.
2.2 Blood Tests Prior to Initiation of Therapy
Obtain a complete blood cell count (CBC) including lymphocyte count before
initiation of therapy [see Warnings and Precautions ( 5.4)].
Obtain serum aminotransferase, alkaline phosphatase, and total bilirubin
levels prior to treatment with dimethyl fumarate delayed-release capsules [see Warnings and Precautions ( 5.5)].
• Starting dose: 120 mg twice a day, orally, for 7 days ( 2.1)
• Maintenance dose after 7 days: 240 mg twice a day, orally ( 2.1)
• Swallow dimethyl fumarate delayed-release capsules whole and intact. Do not
crush, chew, or sprinkle capsule contents on food ( 2.1)
• Take dimethyl fumarate delayed-release capsules with or without food ( 2.1)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate data on the developmental risk associated with the use
of dimethyl fumarate delayed-release capsules in pregnant women. In animals,
adverse effects on offspring survival, growth, sexual maturation, and
neurobehavioral function were observed when dimethyl fumarate (DMF) was
administered during pregnancy and lactation at clinically relevant doses [see Data].
In the U.S. general population, the estimated background risk of major birth
defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15
to 20%, respectively. The background risk of major birth defects and
miscarriage for the indicated population is unknown.
Data
Animal Data
In rats administered DMF orally (25, 100, 250 mg/kg/day) throughout
organogenesis, embryofetal toxicity (reduced fetal body weight and delayed
ossification) were observed at the highest dose tested. This dose also
produced evidence of maternal toxicity (reduced body weight). Plasma exposure
(AUC) for monomethyl fumarate (MMF), the major circulating metabolite, at the
no-effect dose is approximately three times that in humans at the recommended
human dose (RHD) of 480 mg/day. In rabbits administered DMF orally (25, 75,
and 150 mg/kg/day) throughout organogenesis, embryolethality and decreased
maternal body weight were observed at the highest dose tested. The plasma AUC
for MMF at the no-effect dose is approximately 5 times that in humans at the
RHD.
Oral administration of DMF (25, 100, and 250 mg/kg/day) to rats throughout
organogenesis and lactation resulted in increased lethality, persistent
reductions in body weight, delayed sexual maturation (male and female pups),
and reduced testicular weight at the highest dose tested. Neurobehavioral
impairment was observed at all doses. A no-effect dose for developmental
toxicity was not identified. The lowest dose tested was associated with plasma
AUC for MMF lower than that in humans at the RHD.
8.2 Lactation
Risk Summary
There are no data on the presence of DMF or MMF in human milk. The effects on
the breastfed infant and on milk production are unknown.
The developmental and health benefits of breastfeeding should be considered
along with the mother’s clinical need for dimethyl fumarate delayed-release
capsules and any potential adverse effects on the breastfed infant from the
drug or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Clinical studies of dimethyl fumarate delayed-release capsules did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients.
Pregnancy: Based on animal data, may cause fetal harm. ( 8.1)
