Cisatracurium Besylate
These highlights do not include all the information needed to use CISATRACURIUM BESYLATE INJECTION safely and effectively. See full prescribing information for CISATRACURIUM BESYLATE INJECTION.CISATRACURIUM BESYLATE injection, for intravenous useInitial U.S. Approval: 1995
7c8c41b6-d07c-4740-84b7-603289104c59
HUMAN PRESCRIPTION DRUG LABEL
Jan 19, 2023
Meitheal Pharmaceuticals Inc.
DUNS: 080548348
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Cisatracurium Besylate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (3)
Cisatracurium Besylate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
Cisatracurium Besylate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (2)
Drug Labeling Information
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The 10 mL cisatracurium besylate injection multi-dose vials contain the preservative benzyl alcohol. Therefore, if cisatracurium besylate is needed during pregnancy, consider using a benzyl alcohol-free formulation (i.e., 5 mL and 20 mL cisatracurium besylate injection single-dose vials). Because benzyl alcohol is rapidly metabolized by a pregnant woman, benzyl alcohol exposure in the fetus is unlikely. However, adverse reactions have occurred in premature neonates and low birth weight infants who received intravenously administered benzyl alcohol-containing drugs [see Contraindications (4), Warnings and Precautions (5.2), and Use in Specific Populations (8.4)].
There are no available clinical trial data on cisatracurium use in pregnancy to evaluate a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Animal studies conducted in rats administered cisatracurium besylate during organogenesis (Gestational Day 6 to 15) found no evidence of fetal harm at 0.8 times (ventilated rats) the exposure from a human starting IV bolus dose of 0.2 mg/kg (see Data).
The estimated background risk for major birth defects and miscarriage in the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Labor or Delivery
The action of neuromuscular blocking agents may be enhanced by magnesium salts administered for the management of preeclampsia or eclampsia of pregnancy.
Data
Animal Data
Two embryofetal developmental reproductive toxicity studies were conducted in rats. In a non-ventilated rat study, pregnant animals were treated with cisatracurium besylate subcutaneously twice per day from Gestational Day 6 to 15 using subparalyzing doses (2 and 4 mg/kg daily; equivalent to 6- and 12-times, respectively, the AUC exposure in humans following a bolus dose of 0.2 mg/kg IV). In the ventilated rat study, pregnant animals were treated with cisatracurium besylate intravenously once a day between Gestational Day 6 to 15 using paralyzing doses (0.5 and 1 mg/kg; equivalent to 0.4- and 0.8-times, respectively, the exposure in humans following a bolus dose of 0.2 mg/kg IV based on mg/m2 comparison). Neither of these studies revealed maternal or fetal toxicity or malformations.
8.2 Lactation
Risk Summary
The 10 mL cisatracurium besylate injection multi-dose vials contains the preservative benzyl alcohol. Therefore, if cisatracurium besylate is needed during lactation, consider using a benzyl alcohol-free formulation (i.e., 5 mL and 20 mL cisatracurium besylate injection single-dose vials). Because benzyl alcohol is rapidly metabolized by a lactating woman, benzyl alcohol exposure in the breastfed infant is unlikely. However, adverse reactions have occurred in premature neonates and low birth weight infants who received intravenously administered benzyl alcohol-containing drugs [see Contraindications (4), Warnings and Precautions (5.2) and Use in Specific Populations (8.4)].
There are no data on the presence of cisatracurium besylate in human milk, the effects on the breastfed child, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for cisatracurium besylate and any potential adverse effects on the breastfed child from cisatracurium besylate or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of cisatracurium besylate as an adjunct to general anesthesia to facilitate tracheal intubation, and to provide skeletal muscle relaxation during surgery in pediatric patients 1 month through 12 years of age were established from three studies in pediatric patients [see Dosing and Administration (2.2, 2.5) and Clinical Studies (14.2)]. The three open-label studies are summarized below.
The safety and effectiveness of cisatracurium besylate have not been established in pediatric patients less than 1 month of age.
Tracheal Intubation
A study of 0.15 mg/kg cisatracurium besylate evaluated 230 pediatric patients (ages 1 month to 12 years). Excellent or good intubating conditions were produced 120 seconds following 0.15 mg/kg of cisatracurium besylate in 88 of 90 of patients induced with halothane and in 85 of 90 of patients induced with thiopentone and fentanyl. The study also evaluated 50 pediatric patients during opioid anesthesia, with maximum neuromuscular blockade achieved in an average of about 3 minutes and a clinically effective block for 36 minutes in patients ages 2 to 12 years, and maximum neuromuscular block in about 2 minutes and a clinically effective block for about 43 minutes in infants 1 to 23 months [see Clinical Studies (14.2)].
In a study of 0.1 mg/kg cisatracurium besylate administered in 16 pediatric patients (ages 2 to 12 years) during opioid/nitrous oxide/oxygen anesthesia, maximum neuromuscular blockade was achieved in an average of 2.8 minutes with a clinically effective block for 28 minutes [see Clinical Studies (14.2)].
Skeletal Muscle Relaxation During Surgery
In a study of cisatracurium besylate administered during halothane/nitrous oxide/oxygen anesthesia, 18 pediatric patients (ages 2 to 12 years) were scheduled for surgical procedures that required neuromuscular block for 60 minutes or longer. The average duration of continuous infusion was 62.8 minutes (range: 17 to 145 minutes). The overall mean infusion rate for 9 patients whose infusion was 45 minutes or longer was 1.7 mcg/kg/minute (range: 1.19 to 2.14 mcg/kg/minute).
Serious Adverse Reactions in Infants Due to Benzyl Alcohol Preservative in 10 mL Multi-Dose Vials
Serious adverse reactions including fatal reactions and the “gasping syndrome” occurred in premature neonates and infants in the neonatal intensive care unit who received drugs containing benzyl alcohol as a preservative. In these cases, benzyl alcohol dosages of 99 to 234 mg/kg/day produced high levels of benzyl alcohol and its metabolites in the blood and urine (blood levels of benzyl alcohol were 0.61 to 1.378 mmol/L). Additional adverse reactions included gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Preterm, low- birth weight infants may be more likely to develop these reactions because they may be less able to metabolize benzyl alcohol.
When prescribing the 10 mL multi-dose cisatracurium besylate vials in infants consider the combined daily metabolic load of benzyl alcohol from all sources including cisatracurium besylate (multi-dose vials contain 9 mg of benzyl alcohol per mL) and other drugs containing benzyl alcohol. The minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known [see Warnings and Precautions (5.2)]. This warning is not applicable to the 5 mL and 20 mL cisatracurium besylate single-dose vials because these vials do not contain benzyl alcohol.
The use of 10 mL cisatracurium besylate multi-dose vials is contraindicated in pediatric patients less than 1 month of age and low birth-weight infants because these patients are more likely to develop benzyl alcohol toxicity.
8.5 Geriatric Use
Of the total number of subjects (135) in clinical studies of cisatracurium besylate, 57, 63, and 15 subjects were 65-70 years old, 70-80 years old, and greater than 80 years old, respectively. The geriatric population included a subset of patients with significant cardiovascular disease [see Clinical Pharmacology (12.3)].
Because the time to maximum neuromuscular blockade is approximately 1 minute slower in geriatric patients compared to younger patients, consider extending the interval between administering cisatracurium besylate and attempting intubation by at least 1 minute to achieve adequate intubation conditions [see Dosage and Administration (2.2) and Clinical Pharmacology (12.2)].
The time to maximum neuromuscular blockade is approximately 1 minute slower in geriatric patients, a difference that should be taken into account when selecting a neuromuscular blocking agent (e.g., the need to rapidly secure the airway) and when initiating laryngoscopy [see Clinical Pharmacology (12.3)]. Minor differences in the pharmacokinetics of cisatracurium between elderly and young adult patients were not associated with clinically significant differences in the recovery profile of cisatracurium besylate following a single 0.1 mg/kg dose.
Besides the differences noted above, no overall differences in safety or effectiveness were observed between geriatric and younger subjects, and other reported clinical experience has not identified differences in responses between geriatric and younger subjects, but greater sensitivity of some older individuals to cisatracurium besylate cannot be ruled out.
8.6 Patients with Renal Impairment
The time to 90% neuromuscular blockade was 1 minute slower in patients with end-stage renal disease than in patients with normal renal function. Therefore, consider extending the interval between administering cisatracurium besylate and attempting intubation by at least 1 minute to achieve adequate intubation conditions [see Dosage and Administration (2.2) and Clinical Pharmacology (12.2)].
There was no clinically significant alteration in the recovery profile of cisatracurium besylate in patients with end-stage renal disease following a 0.1 mg/kg dose of cisatracurium besylate. The recovery profile of cisatracurium besylate is unchanged in patients with renal impairment, which is consistent with predominantly organ-independent elimination [see Clinical Pharmacology (12.3)].
8.7 Patients with Hepatic Impairment
The pharmacokinetic study analysis in patients with end-stage liver disease undergoing liver transplantation and healthy subjects undergoing elective surgery indicated slightly larger volumes of distribution in liver transplant patients with slightly higher plasma clearances of cisatracurium. The times to maximum neuromuscular blockade were approximately one minute faster in liver transplant patients than in healthy adult patients receiving 0.1 mg/kg cisatracurium besylate. These minor differences in pharmacokinetics were not associated with clinically significant differences in the recovery profile of cisatracurium besylate [see Clinical Pharmacology (12.3)].
8.8 Burn Patients
Patients with burns have been shown to develop resistance to nondepolarizing neuromuscular blocking agents. The extent of altered response depends upon the size of the burn and the time elapsed since the burn injury. Cisatracurium besylate has not been studied in patients with burns. However, based on its structural similarity to another neuromuscular blocking agent, consider the possibility of increased dosage requirements and shortened duration of action if cisatracurium besylate is administered to burn patients.
8.9 Patients with Hemiparesis or Paraparesis
Patients with hemiparesis or paraparesis may demonstrate resistance to nondepolarizing neuromuscular blocking agents in the affected limbs. To avoid inaccurate dosing, perform neuromuscular monitoring on a non-paretic limb.
8.10 Patients with Neuromuscular Disease
Profound and prolonged neuromuscular blockade may occur in patients with neuromuscular diseases (e.g., myasthenia gravis and myasthenic syndrome) and carcinomatosis. Therefore, a lower maximum initial bolus is recommended in these patients [see Dosage and Administration (2.2)].
- Patients with Hemiparesis or Paraparesis: Perform neuromuscular monitoring on non-paretic limb (8.9)
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cisatracurium besylate binds competitively to cholinergic receptors on the motor end-plate to antagonize the action of acetylcholine, resulting in blockade of neuromuscular transmission. This action is antagonized by acetylcholinesterase inhibitors such as neostigmine.
12.2 Pharmacodynamics
The average ED95 (dose required to produce 95% suppression of the adductor pollicis muscle twitch response to ulnar nerve stimulation) of cisatracurium is 0.05 mg/kg (range: 0.048 to 0.053) in adults receiving opioid/nitrous oxide/oxygen anesthesia.
The pharmacodynamics of various cisatracurium besylate doses administered over 5 to 10 seconds during opioid/nitrous oxide/oxygen anesthesia are summarized in Table 5. When the cisatracurium besylate dose is doubled, the clinically effective duration of blockade increases by approximately 25 minutes. Once recovery begins, the rate of recovery is independent of dose.
Isoflurane or enflurane administered with nitrous oxide/oxygen to achieve 1.25 MAC (Minimum Alveolar Concentration) prolonged the clinically effective duration of action of initial and maintenance cisatracurium besylate doses, and decreased the average infusion rate requirement of cisatracurium besylate. The magnitude of these effects depended on the duration of administration of the volatile agents:
- Fifteen to 30 minutes of exposure to 1.25 MAC isoflurane or enflurane had minimal effects on the duration of action of initial doses of cisatracurium besylate.
- In surgical procedures during enflurane or isoflurane anesthesia greater than 30 minutes, less frequent maintenance dosing, lower maintenance doses, or reduced infusion rates of cisatracurium besylate were required. The average infusion rate requirement was decreased by as much as 30% to 40% [see Drug Interactions (7.1)].
The onset, duration of action, and recovery profiles of cisatracurium besylate during propofol/oxygen or propofol/nitrous oxide/oxygen anesthesia were similar to those during opioid/nitrous oxide/oxygen anesthesia (see Table 5).
Repeated administration of maintenance cisatracurium besylate doses or a continuous cisatracurium besylate infusion for up to 3 hours was not associated with development of tachyphylaxis or cumulative neuromuscular blocking effects. The time needed to recover from successive maintenance doses did not change with the number of doses administered when partial recovery occurred between doses. The rate of spontaneous recovery of neuromuscular function after cisatracurium besylate infusion was independent of the duration of infusion and comparable to the rate of recovery following initial doses (see Table 5).
Pediatric patients including infants generally had a shorter time to maximum neuromuscular blockade and a faster recovery from neuromuscular blockade compared to adults treated with the same weight-based doses (see Table 5).
Table 5. Pharmacodynamic Dose Response* of Cisatracurium Besylate During Opioid/Nitrous Oxide/Oxygen Anesthesia
| |||||||
|
† Clinically effective duration of block | |||||||
|
‡ Train-of-four ratio | |||||||
|
§ n=the number of patients with Time to Maximum Block data | |||||||
|
|| Propofol anesthesia | |||||||
|
¶ Halothane anesthesia | |||||||
|
** Thiopentone, alfentanil, N2O/O2 anesthesia | |||||||
|
Cisatracurium Besylate |
Time to 90% |
Time to Maximum Block in minutes |
5% |
25% |
95% |
T4:T****1 |
25%-75% |
|
Adults | |||||||
|
0.1 mg/kg |
3.3 |
5.0 |
33 |
42 |
64 |
64 |
13 |
|
(2 × ED95) |
(1.0-8.7) |
(1.2-17.2) |
(15-51) |
(22-63) |
(25-93) |
(32-91) |
(5-30) |
|
0.15|| mg/kg |
2.6 |
3.5 |
46 |
55 |
76 |
75 |
13 |
|
(3 × ED95) |
(1.0-4.4) |
(1.6-6.8) |
(28-65) |
(44-74) |
(60-103) |
(63-98) |
(11-16) |
|
(n = 39) | |||||||
|
0.2 mg/kg |
2.4 |
2.9 |
59 |
65 |
81 |
85 |
12 |
|
(4 × ED95) |
(1.5-4.5) |
(1.9-5.2) |
(31-103) |
(43-103) |
(53-114) |
(55-114) |
(2-30) |
|
(n = 30) | |||||||
|
0.25 mg/kg |
1.6 |
2.0 |
70 |
78 |
91 |
97 |
8 |
|
(5 × ED95) |
(0.8-3.3) |
(1.2-3.7) |
(58-85) |
(66-86) |
(76-109) |
(82-113) |
(5-12) |
|
(n = 15) | |||||||
|
0.4 mg/kg |
1.5 |
1.9 |
83 |
91 |
121 |
126 |
14 |
|
(8 × ED95) |
(1.3-1.8) |
(1.4-2.3) |
(37-103) |
(59-107) |
(110-134) |
(115-137) |
(10-18) |
|
(n = 15) | |||||||
|
Infants (1-23 months of age) | |||||||
|
0.15 mg/kg** |
1.5 |
2.0 |
36 |
43 |
64 |
59 |
11.3 |
|
(n = 18-26) |
(0.7-3.2) |
(1.3-4.3) |
(28-50) |
(34-58) |
(54-84) |
(49-76) |
(7.3-18.3) |
|
Pediatric Patients 2-12 years | |||||||
|
0.08 mg/kg¶ (2 × ED95) |
2.2 |
3.3 |
22 |
29 |
52 |
50 |
11 |
|
(n = 60) | |||||||
|
0.1 mg/kg |
1.7 |
2.8 |
21 |
28 |
46 |
44 |
10 |
|
(n = 16) |
(1.3-2.7) |
(1.8-6.7) |
(13-31) |
(21-38) |
(37-58) |
(36-58) |
(7-12) |
|
0.15 mg/kg** |
2.1 |
3.0 |
29 |
36 |
55 |
54 |
10.6 |
|
(n = 23-24) |
(1.3-2.8) |
(1.5-8.0) |
(19-38) |
(29-46) |
(45-72) |
(44-66) |
(8.5-17.7) |
Hemodynamics Profile
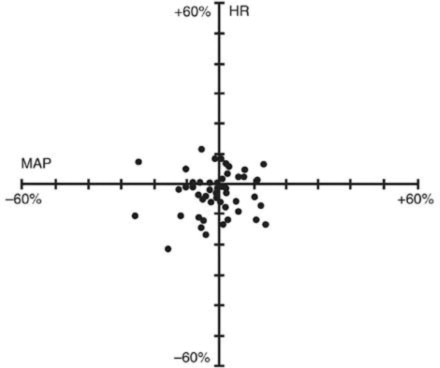
Cisatracurium besylate had no dose-related effects on mean arterial blood pressure (MAP) or heart rate (HR) following doses ranging from 0.1 mg/kg to 0.4 mg/kg, administered over 5 to 10 seconds, in healthy adult patients (see Figure 1) or in patients with serious cardiovascular disease (see Figure 2).
A total of 141 patients undergoing coronary artery bypass graft (CABG) surgery were administered cisatracurium besylate in three active-controlled clinical trials and received doses ranging from 0.1 mg/kg to 0.4 mg/kg. While the hemodynamic profile was comparable in both the cisatracurium besylate and active control groups, data for doses above 0.3 mg/kg in this population are limited.
Figure 1. Maximum Percent Change from Preinjection in HR and MAP During First 5Minutes after Initial 4 × ED95to 8 × ED95** Cisatracurium Besylate Doses in Healthy Adults Who Received Opioid/Nitrous Oxide/Oxygen Anesthesia (n = 44)**
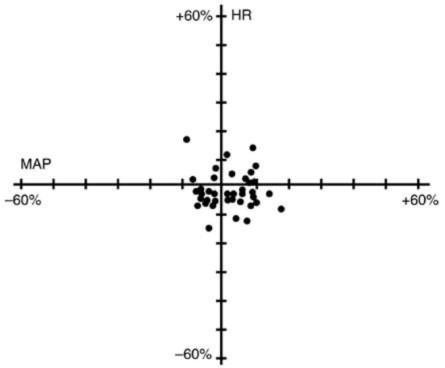
Figure 2. Percent Change from Preinjection in HR and MAP 10 Minutes After an Initial 4**× ED95 to 8 × ED95 Cisatracurium Besylate Dose in Patients Undergoing CABG Surgery Receiving Oxygen/Fentanyl/Midazolam/Anesthesia (n = 54)**
No clinically significant changes in MAP or HR were observed following administration of doses up to 0.1 mg/kg cisatracurium besylate over 5 to 10 seconds in 2- to 12-year-old pediatric patients who received either halothane/nitrous oxide/oxygen or opioid/nitrous oxide/oxygen anesthesia. Doses of 0.15 mg/kg cisatracurium besylate administered over 5 seconds were not consistently associated with changes in HR and MAP in pediatric patients aged 1 month to 12 years who received opioid/nitrous oxide/oxygen or halothane/nitrous oxide/oxygen anesthesia.
12.3 Pharmacokinetics
The neuromuscular blocking activity of cisatracurium besylate is due to parent drug. Cisatracurium plasma concentration-time data following IV bolus administration are best described by a two- compartment open model (with elimination from both compartments) with an elimination half-life (t½β) of 22 minutes, a plasma clearance (CL) of 4.57 mL/min/kg, and a volume of distribution at steady state (Vss) of 145 mL/kg.
Results from population pharmacokinetic/pharmacodynamic (PK/PD) analyses from 241 healthy surgical patients are summarized in Table 6.
Table 6. Key Population PK/PD Parameter Estimates for Cisatracurium in Healthy Surgical Patients* Following 0.1 (2 × ED95) to 0.4 mg/kg (8 × ED95) of Cisatracurium Besylate
| ||
|
† The percent standard error of the mean (%SEM) ranged from 3% to 12% indicating good precision for the PK/PD estimates. | ||
|
‡ Expressed as a coefficient of variation; the %SEM ranged from 20% to 35% indicating adequate precision for the estimates of interpatient variability. | ||
|
§ Vss is the volume of distribution at steady state estimated using a two- compartment model with elimination from both compartments. Vss is equal to the sum of the volume in the central compartment (Vc) and the volume in the peripheral compartment (Vp); interpatient variability could only be estimated for Vc. | ||
|
ll Rate constant describing the equilibration between plasma concentrations and neuromuscular | ||
|
block | ||
|
¶ Concentration required to produce 50% T1 suppression; an index of patient sensitivity. | ||
|
Parameter |
Estimate**†** |
Magnitude of Interpatient Variability (CV)****‡ |
|
CL (mL/min/kg) |
4.57 |
16% |
|
Vss (mL/kg)§ |
145 |
27% |
|
keo (min-1)ll |
0.0575 |
61% |
|
EC50 (ng/mL)¶ |
141 |
52% |
The magnitude of interpatient variability in CL was low (16%), as expected based on the importance of Hofmann elimination. The magnitudes of interpatient variability in CL and volume of distribution were low in comparison to those for keo and EC50. This suggests that any alterations in the time course of cisatracurium besylate-induced neuromuscular blockade were more likely to be due to variability in the PD parameters than in the PK parameters. Parameter estimates from the population PK analyses were supported by noncompartmental PK analyses on data from healthy patients and from specific populations.
Conventional PK analyses have shown that the PK of cisatracurium are proportional to dose between 0.1 (2 × ED95) and 0.2 (4 × ED95) mg/kg cisatracurium. In addition, population PK analyses revealed no statistically significant effect of initial dose on CL for doses between 0.1 (2 × ED95) and 0.4 (8 × ED95) mg/kg cisatracurium.
Distribution
The volume of distribution of cisatracurium is limited by its large molecular weight and high polarity. The Vss was equal to 145 mL/kg (Table 6) in healthy 19- to 64-year-old surgical patients receiving opioid anesthesia. The Vss was 21% larger in similar patients receiving inhalation anesthesia.
The binding of cisatracurium to plasma proteins has not been successfully studied due to its rapid degradation at physiologic pH. Inhibition of degradation requires nonphysiological conditions of temperature and pH which are associated with changes in protein binding.
Elimination
Organ-independent Hofmann elimination (a chemical process dependent on pH and temperature) is the predominant pathway for the elimination of cisatracurium. The liver and kidney play a minor role in the elimination of cisatracurium but are primary pathways for the elimination of metabolites. Therefore, the t½β values of metabolites (including laudanosine) are longer in patients with renal or hepatic impairment and metabolite concentrations may be higher after long-term administration [see Warnings and Precautions (5.3)].
The mean CL values for cisatracurium ranged from 4.5 to 5.7 mL/min/kg in studies of healthy surgical patients. The compartmental PK modeling suggests that approximately 80% of the cisatracurium CL is accounted for by Hofmann elimination and the remaining 20% by renal and hepatic elimination. These findings are consistent with the low magnitude of interpatient variability in CL (16%) estimated as part of the population PK/PD analyses and with the recovery of parent and metabolites in urine.
In studies of healthy surgical patients, mean t½β values of cisatracurium ranged from 22 to 29 minutes and were consistent with the t½β of cisatracurium in vitro (29 minutes). The mean ± SD t½β values of laudanosine were 3.1 ± 0.4 hours in healthy surgical patients receiving cisatracurium besylate (n = 10).
Metabolism
The degradation of cisatracurium was largely independent of liver metabolism. Results from in vitro experiments suggest that cisatracurium undergoes Hofmann elimination (a pH and temperature-dependent chemical process) to form laudanosine [see Warnings and Precautions (5.3)] and the monoquaternary acrylate metabolite, neither of which has any neuromuscular blocking activity. The monoquaternary acrylate undergoes hydrolysis by non-specific plasma esterases to form the monoquaternary alcohol (MQA) metabolite. The MQA metabolite can also undergo Hofmann elimination but at a much slower rate than cisatracurium. Laudanosine is further metabolized to desmethyl metabolites which are conjugated with glucuronic acid and excreted in the urine.
The laudanosine metabolite of cisatracurium has been noted to cause transient hypotension and, in higher doses, cerebral excitatory effects when administered to several animal species. The relationship between CNS excitation and laudanosine concentrations in humans has not been established [see Warnings and Precautions (5.3)].
During IV infusions of cisatracurium besylate, peak plasma concentrations (Cmax) of laudanosine and the MQA metabolite were approximately 6% and 11% of the parent compound, respectively. The Cmax values of laudanosine in healthy surgical patients receiving infusions of cisatracurium besylate were mean ± SD Cmax: 60 ± 52 ng/mL.
Excretion
Following 14C-cisatracurium administration to 6 healthy male patients, 95% of the dose was recovered in the urine (mostly as conjugated metabolites) and 4% in the feces; less than 10% of the dose was excreted as unchanged parent drug in the urine. In 12 healthy surgical patients receiving non-radiolabeled cisatracurium who had Foley catheters placed for surgical management, approximately 15% of the dose was excreted unchanged in the urine.
Special Populations
Geriatric Patients
The results of conventional PK analysis from a study of 12 healthy elderly patients and 12 healthy young adult patients who received a single IV cisatracurium besylate dose of 0.1 mg/kg are summarized in Table 7. Plasma clearances of cisatracurium were not affected by age; however, the volumes of distribution were slightly larger in elderly patients than in young patients resulting in slightly longer t½β values for cisatracurium.
The rate of equilibration between plasma cisatracurium concentrations and neuromuscular blockade was slower in elderly patients than in young patients (mean ± SD keo: 0.071 ± 0.036 and 0.105 ± 0.021 minutes-1, respectively); there was no difference in the patient sensitivity to cisatracurium-induced block, as indicated by EC50 values (mean ± SD EC50: 91 ± 22 and 89 ± 23 ng/mL, respectively). These changes were consistent with the 1-minute slower times to maximum block in elderly patients receiving 0.1 mg/kg cisatracurium besylate, when compared to young patients receiving the same dose. The minor differences in PK/PD parameters of cisatracurium between elderly patients and young patients were not associated with clinically significant differences in the recovery profile of cisatracurium besylate.
Table 7. Pharmacokinetic Parameters* of Cisatracurium in Healthy Elderly and Young Adult Patients Following 0.1 mg/kg (2 × ED95) of Cisatracurium Besylate (Isoflurane/Nitrous Oxide/Oxygen Anesthesia)
| ||
|
† P < 0.05 for comparisons between healthy elderly and healthy young adult patients | ||
|
‡ Volume of distribution is underestimated because elimination from the peripheral compartment is ignored. | ||
|
Parameter |
Healthy Elderly Patients |
Healthy Young Adult Patients |
|
Elimination Half-Life (t½β, min) |
25.8 ± 3.6**†** |
22.1 ± 2.5 |
|
Volume of Distribution at Steady State**‡** (mL/kg) |
156 ± 17**†** |
133 ± 15 |
|
Plasma Clearance (mL/min/kg) |
5.7 ± 1.0 |
5.3 ± 0.9 |
Patients with Hepatic Impairment
Table 8 summarizes the conventional PK analysis from a study of cisatracurium besylate in 13 patients with end-stage liver disease undergoing liver transplantation and 11 healthy adult patients undergoing elective surgery. The slightly larger volumes of distribution in liver transplant patients were associated with slightly higher plasma clearances of cisatracurium. The parallel changes in these parameters resulted in no difference in t½β values. There were no differences in keo or EC50 between patient groups. The times to maximum neuromuscular blockade were approximately one minute faster in liver transplant patients than in healthy adult patients receiving 0.1 mg/kg cisatracurium besylate. These minor PK differences were not associated with clinically significant differences in the recovery profile of cisatracurium besylate.
The t½β values of metabolites are longer in patients with hepatic disease and concentrations may be higher after long-term administration.
Table 8. Pharmacokinetic Parameters* of Cisatracurium in Healthy Adult Patients and in Patients Undergoing Liver Transplantation Following 0.1 mg/kg (2 × ED95) of Cisatracurium Besylate (Isoflurane/Nitrous Oxide/Oxygen Anesthesia)
| ||
|
† P < 0.05 for comparisons between liver transplant patients and healthy adult patients | ||
|
‡ Volume of distribution is underestimated because elimination from the peripheral compartment is ignored. | ||
|
Parameter |
Liver Transplant Patients |
Healthy Adult Patients |
|
Elimination Half-Life (t½β, min) |
24.4 ± 2.9 |
23.5 ± 3.5 |
|
Volume of Distribution at Steady State**‡** (mL/kg) |
195 ± 38**†** |
161 ± 23 |
|
Plasma Clearance (mL/min/kg) |
6.6 ± 1.1**†** |
5.7 ± 0.8 |
Patients with Renal Impairment
Results from a conventional PK study of cisatracurium besylate in 13 healthy adult patients and 15 patients with end-stage renal disease (ESRD) who had elective surgery are summarized in Table 9. The PK/PD parameters of cisatracurium were similar in healthy adult patients and ESRD patients. The times to 90% neuromuscular blockade were approximately one minute slower in ESRD patients following 0.1 mg/kg cisatracurium besylate. There were no differences in the durations or rates of recovery of cisatracurium besylate between ESRD and healthy adult patients.
The t½β values of metabolites are longer in patients with ESRD and concentrations may be higher after long-term administration.
Population PK analyses showed that patients with creatinine clearances ≤ 70 mL/min had a slower rate of equilibration between plasma concentrations and neuromuscular block than patients with normal renal function; this change was associated with a slightly slower (~ 40 seconds) predicted time to 90% T1 suppression in patients with renal impairment following 0.1 mg/kg cisatracurium besylate. There was no clinically significant alteration in the recovery profile of cisatracurium besylate in patients with renal impairment. The recovery profile of cisatracurium besylate is unchanged in the presence of renal or hepatic failure, which is consistent with predominantly organ- independent elimination.
Table 9. Pharmacokinetic Parameters* for Cisatracurium in Healthy Adult Patients and in Patients With End-Stage Renal Disease (ESRD) Who Received 0.1 mg/kg (2 × ED95) of Cisatracurium Besylate (Opioid/Nitrous Oxide/Oxygen Anesthesia)
| ||
|
† Volume of distribution is underestimated because elimination from the peripheral compartment is ignored. | ||
|
Parameter |
Healthy Adult Patients |
ESRD Patients |
|
Elimination Half-Life (t½β, min) |
29.4 ± 4.1 |
32.3 ± 6.3 |
|
Volume of Distribution at Steady State**†** (mL/kg) |
149 ± 35 |
160 ± 32 |
|
Plasma Clearance (mL/min/kg) |
4.66 ± 0.86 |
4.26 ± 0.62 |
Intensive Care Unit (ICU) Patients
The PK of cisatracurium and its metabolites were determined in six ICU patients who received cisatracurium besylate and are presented in Table 10. The relationships between plasma cisatracurium concentrations and neuromuscular blockade have not been evaluated in ICU patients.
Limited PK data are available for ICU patients with hepatic or renal impairment who received cisatracurium besylate. Relative to cisatracurium besylate-treated ICU patients with normal renal and hepatic function, metabolite concentrations (plasma and tissues) may be higher in cisatracurium besylate-treated ICU patients with renal or hepatic impairment [see Warnings and Precautions (5.3)].
Table 10. Parameter Estimates* for Cisatracurium and Metabolites in ICU Patients After Long-Term (24-48 Hour) Administration of Cisatracurium Besylate
| ||
|
† Volume of distribution during the terminal elimination phase, an underestimate because elimination from the peripheral compartment is ignored. | ||
|
‡ n = 2, range presented | ||
|
Parameter |
Cisatracurium (n = 6) | |
|
Parent Compound |
CL (mL/min/kg) |
7.45 ± 1.02 |
|
t½ β(min) |
26.8 ± 11.1 | |
|
Vβ (mL/kg)† |
280 ± 103 | |
|
Laudanosine |
Cmax (ng/mL) |
707 ± 360 |
|
t½β (hrs) |
6.6 ± 4.1 | |
|
MQA metabolite |
Cmax (ng/mL) |
152-181**‡** |
|
t½β (min) |
26-31**‡** |
Pediatric Population
The population PK/PD of cisatracurium were described in 20 healthy pediatric patients ages 2 to 12 years during halothane anesthesia, using the same model developed for healthy adult patients. The CL was higher in healthy pediatric patients (5.89 mL/min/kg) than in healthy adult patients (4.57 mL/min/kg) during opioid anesthesia. The rate of equilibration between plasma concentrations and neuromuscular blockade, as indicated by keo, was faster in healthy pediatric patients receiving halothane anesthesia (0.1330 minutes-1) than in healthy adult patients receiving opioid anesthesia (0.0575 minutes-1). The EC50 in healthy pediatric patients (125 ng/mL) was similar to the value in healthy adult patients (141 ng/mL) during opioid anesthesia. The minor differences in the PK/PD parameters of cisatracurium were associated with a faster time to onset and a shorter duration of cisatracurium-induced neuromuscular blockade in pediatric patients.
Sex and Obesity
Although population PK/PD analyses revealed that sex and obesity were associated with effects on the PK and/or PD of cisatracurium; these PK/PD changes were not associated with clinically significant alterations in the predicted onset or recovery profile of cisatracurium besylate.
Use of Inhalation Agents
The use of inhalation agents was associated with a 21% larger Vss, a 78% larger keo, and a 15% lower EC50 for cisatracurium. These changes resulted in a slightly faster (~ 45 seconds) predicted time to 90% T1 suppression in patients who received 0.1 mg/kg cisatracurium during inhalation anesthesia than in patients who received the same dose of cisatracurium during opioid anesthesia; however, there were no clinically significant differences in the predicted recovery profile of cisatracurium besylate between patient groups.
Drug Interaction Studies
Carbamazepine and phenytoin
The systemic clearance of cisatracurium was higher in patients who were on prior chronic anticonvulsant therapy of carbamazepine or phenytoin [see Warning and Precautions (5.9) and Drug Interactions (7.1)].
