Fluoxetine
These highlights do not include all the information needed to use FLUOXETINE CAPSULES safely and effectively. See full prescribing information for FLUOXETINE CAPSULES. FLUOXETINE capsules, for oral use Initial U.S. Approval: 1987
8e822937-9431-446f-88c4-330a25d12439
HUMAN PRESCRIPTION DRUG LABEL
Sep 26, 2023
MARKSANS PHARMA LIMITED
DUNS: 925822975
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Fluoxetine Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Fluoxetine Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Fluoxetine Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (11)
Drug Labeling Information
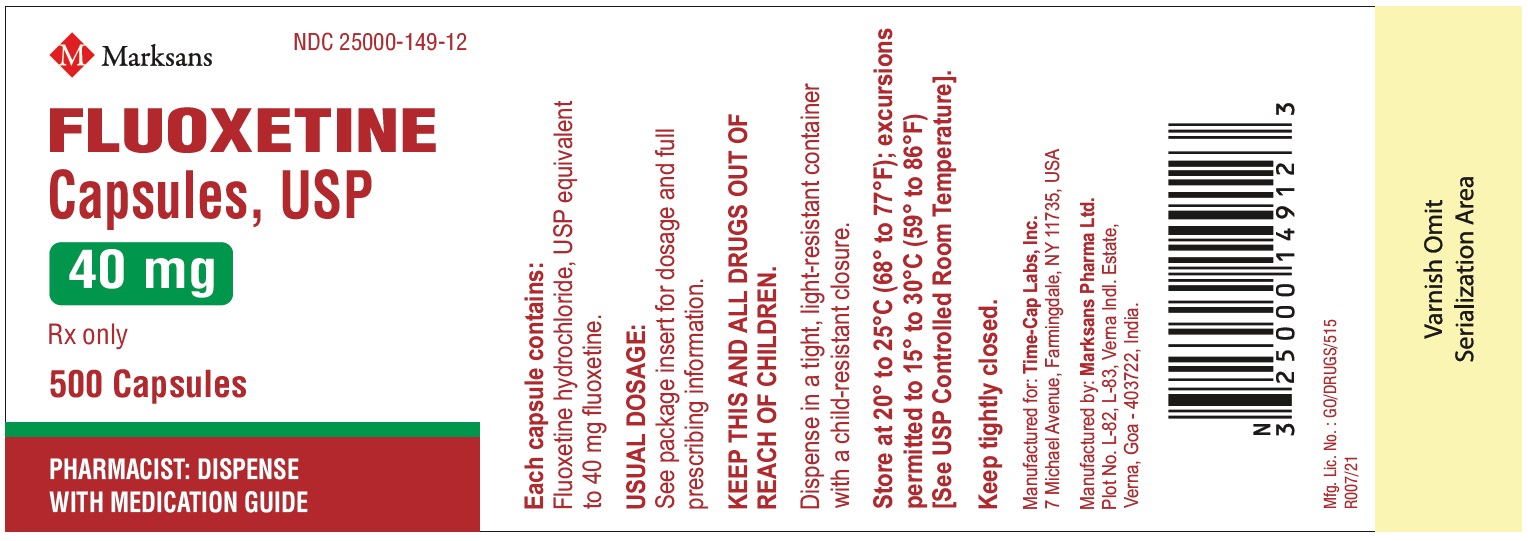
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
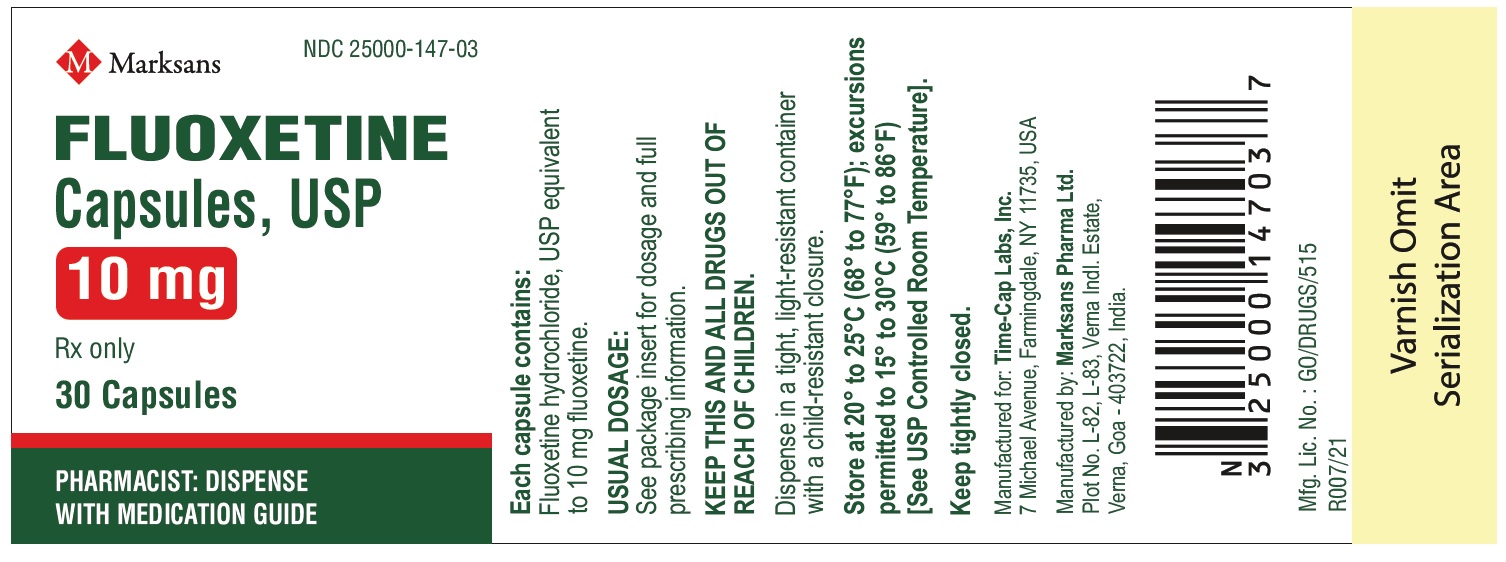
NDC 25000-147-03
Fluoxetine Capsules, USP 10 mg
30 count bottle label
NDC 25000-147-08
Fluoxetine Capsules, USP 10 mg
100 count bottle label

NDC 25000-147-14
Fluoxetine Capsules, USP 10 mg
1000 count bottle label

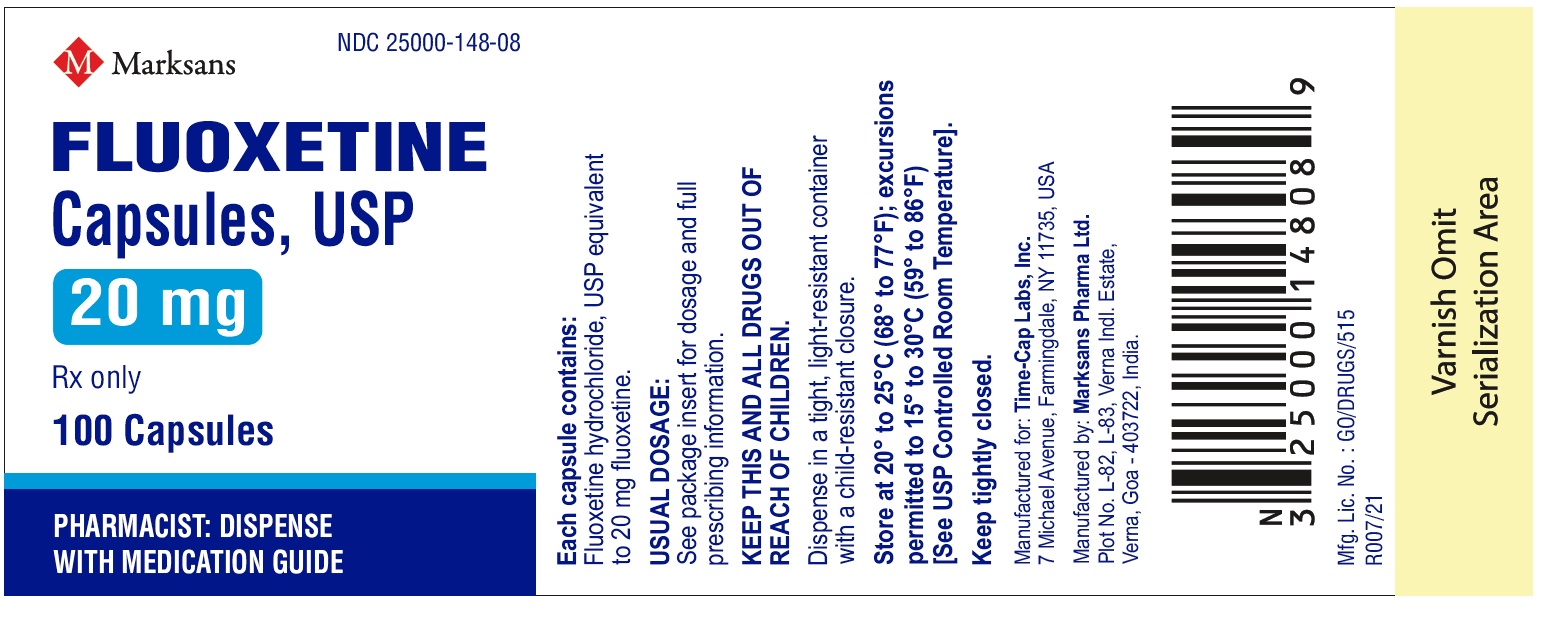
NDC 25000-148-08
Fluoxetine Capsules, USP 20 mg
100 count bottle label
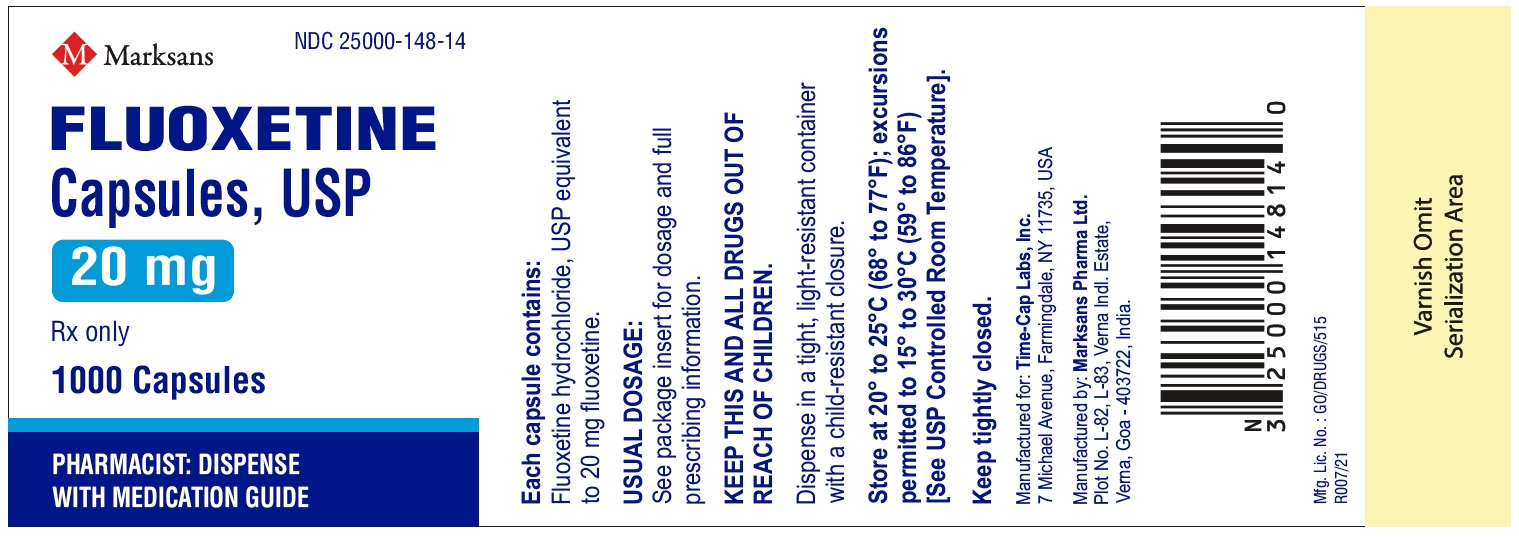
NDC 25000-148-14
Fluoxetine Capsules, USP 20 mg
1000 count bottle label
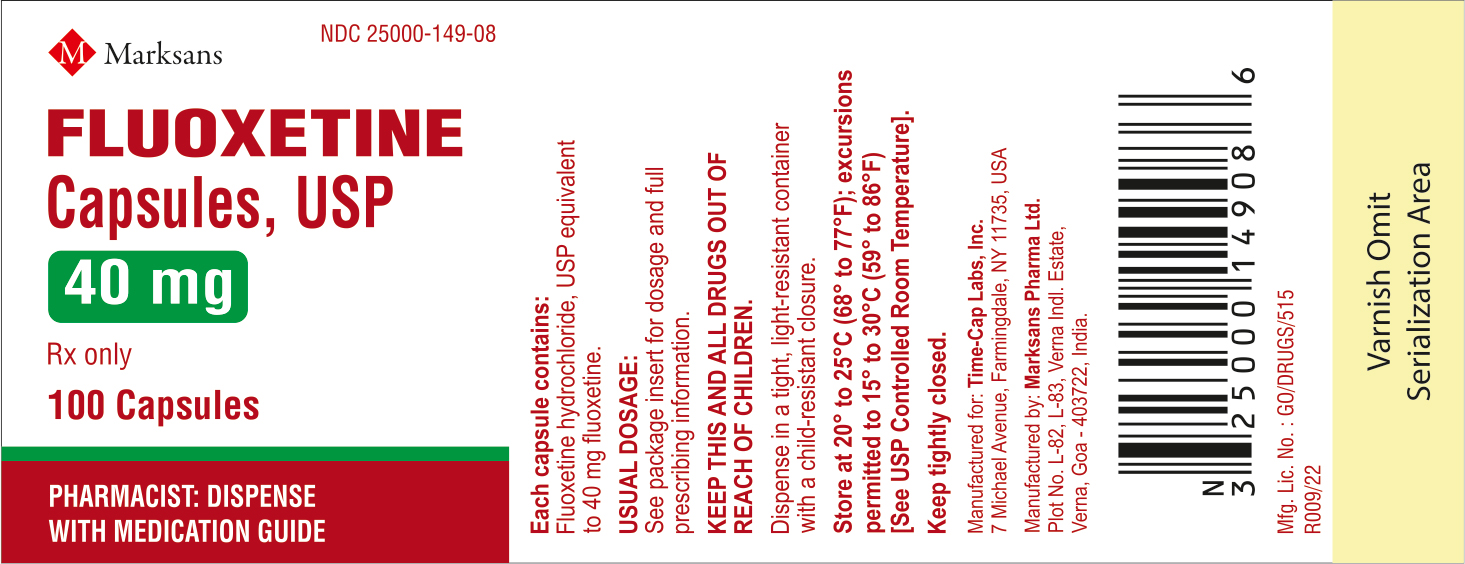
NDC 25000-149-08
Fluoxetine Capsules, USP 40 mg
100 count bottle label
NDC 25000-149-12
Fluoxetine Capsules, USP 40 mg
500 count bottle label
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
When using fluoxetine and olanzapine in combination, also refer to the Contraindications section of the package insert for Symbyax.
4.1 Monoamine Oxidase Inhibitors (MAOIs)
The use of MAOIs intended to treat psychiatric disorders with fluoxetine or
within 5 weeks of stopping treatment with fluoxetine is contraindicated
because of an increased risk of serotonin syndrome. The use of fluoxetine
within 14 days of stopping an MAOI intended to treat psychiatric disorders is
also contraindicated [see Dosage and Administration (2.9) and Warnings and Precautions (5.2)].
Starting fluoxetine in a patient who is being treated with MAOIs such as
linezolid or intravenous methylene blue is also contraindicated because of an
increased risk of serotonin syndrome [see Dosage and Administration (2.10) and Warnings and Precautions (5.2)].
4.2 Other Contraindications
The use of fluoxetine is contraindicated with the following:
• Pimozide [see Warnings and Precautions (5.11) and Drug Interactions (7.7, 7.8)]
• Thioridazine [see Warnings and Precautions (5.11) and Drug Interactions (7.7, 7.8)]
Pimozide and thioridazine prolong the QT interval. Fluoxetine can increase the
levels of pimozide and thioridazine through inhibition of CYP2D6. Fluoxetine
can also prolong the QT interval.
• Serotonin Syndrome and MAOIs: Do not use MAOIs intended to treat psychiatric
disorders with fluoxetine or within 5 weeks of stopping treatment with
fluoxetine. Do not use fluoxetine within 14 days of stopping an MAOI intended
to treat psychiatric disorders. In addition, do not start fluoxetine in a
patient who is being treated with linezolid or intravenous methylene blue
(4.1)
• Pimozide: Do not use. Risk of QT prolongation and drug interaction (4.2,
5.11, 7.7, 7.8)
• Thioridazine: Do not use. Risk of QT interval prolongation and elevated
thioridazine plasma levels. Do not use thioridazine within 5 weeks of
discontinuing fluoxetine. Do not use thioridazine within 5 weeks of
discontinuing fluoxetine (4.2, 5.11, 7.7,7.8)
• When using fluoxetine and olanzapine in combination, also refer to the
Contraindications section of the package insert for Symbyax (4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
When using fluoxetine and olanzapine in combination, also refer to the Warnings and Precautions section of the package insert for Symbyax.
5.1 Suicidal Thoughts and Behaviors in Children, Adolescents, and Young
Adults
Patients with Major Depressive Disorder (MDD), both adult and pediatric, may
experience worsening of their depression and/or the emergence of suicidal
ideation and behavior (suicidality) or unusual changes in behavior, whether or
not they are taking antidepressant medications, and this risk may persist
until significant remission occurs. Suicide is a known risk of depression and
certain other psychiatric disorders, and these disorders themselves are the
strongest predictors of suicide. There has been a long-standing concern,
however, that antidepressants may have a role in inducing worsening of
depression and the emergence of suicidality in certain patients during the
early phases of treatment. Pooled analyses of short-term placebo-controlled
trials of antidepressant drugs (SSRIs and others) showed that these drugs
increase the risk of suicidal thinking and behavior (suicidality) in children,
adolescents, and young adults (ages 18-24) with Major Depressive Disorder
(MDD) and other psychiatric disorders. Short-term studies did not show an
increase in the risk of suicidality with antidepressants compared to placebo
in adults beyond age 24; there was a reduction with antidepressants compared
to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents
with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders
included a total of 24 short-term trials of 9 antidepressant drugs in over
4400 patients. The pooled analyses of placebo-controlled trials in adults with
MDD or other psychiatric disorders included a total of 295 short-term trials
(median duration of 2 months) of 11 antidepressant drugs in over 77,000
patients. There was considerable variation in risk of suicidality among drugs,
but a tendency toward an increase in the younger patients for almost all drugs
studied. There were differences in absolute risk of suicidality across the
different indications, with the highest incidence in MDD. The risk differences
(drug versus placebo), however, were relatively stable within age strata and
across indications. These risk differences (drug-placebo difference in the
number of cases of suicidality per 1000 patients treated) are provided in
Table 2.
Table 2: Suicidality per 1000 Patients Treated
|
Age Range |
Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|
Increases Compared to Placebo | |
|
<18 |
14 additional cases |
|
18 - 24 |
5 additional cases |
|
Decreases Compared to Placebo | |
|
25 - 64 |
1 fewer case |
|
≥65 |
6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in
the adult trials, but the number was not sufficient to reach any conclusion
about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e.,
beyond several months. However, there is substantial evidence from placebo-
controlled maintenance trials in adults with depression that the use of
antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be
monitored appropriately and observed closely for clinical worsening,
suicidality, and unusual changes in behavior, especially during the initial
few months of a course of drug therapy, or at times of dose changes, either
increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia,
irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor
restlessness), hypomania, and mania, have been reported in adult and pediatric
patients being treated with antidepressants for Major Depressive Disorder as
well as for other indications, both psychiatric and nonpsychiatric. Although a
causal link between the emergence of such symptoms and either the worsening of
depression and/or the emergence of suicidal impulses has not been established,
there is concern that such symptoms may represent precursors to emerging
suicidality.
Consideration should be given to changing the therapeutic regimen, including
possibly discontinuing the medication, in patients whose depression is
persistently worse, or who are experiencing emergent suicidality or symptoms
that might be precursors to worsening depression or suicidality, especially if
these symptoms are severe, abrupt in onset, or were not part of the patient’s
presenting symptoms.
If the decision has been made to discontinue treatment, medication should be
tapered, as rapidly as is feasible, but with recognition that abrupt
discontinuation can be associated with certain symptoms [see Warnings and Precautions (5.15)].
Families and caregivers of patients being treated with antidepressants for
Major Depressive Disorder or other indications, both psychiatric and
nonpsychiatric, should be alerted about the need to monitor patients for the
emergence of agitation, irritability, unusual changes in behavior, and the
other symptoms described above, as well as the emergence of suicidality, and
to report such symptoms immediately to health care providers. Such monitoring
should include daily observation by families and caregivers. Prescriptions
for fluoxetine should be written for the smallest quantity of capsules
consistent with good patient management, in order to reduce the risk of
overdose.
It should be noted that fluoxetine is approved in the pediatric population for
Major Depressive Disorder and Obsessive Compulsive Disorder; and fluoxetine in
combination with olanzapine for the acute treatment of depressive episodes
associated with Bipolar I Disorder.
5.2 Serotonin Syndrome
Selective serotonin reuptake inhibitors (SSRIs), including Fluoxetine, can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, meperidine, methadone, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e., MAOIs [see Contraindications (4), Drug Interactions (7.1)]. Serotonin syndrome can also occur when these drugs are used alone.
Serotonin syndrome signs and symptoms may include mental status changes (e.g.,
agitation, hallucinations, delirium, and coma), autonomic instability (e.g.,
tachycardia, labile blood pressure, dizziness, diaphoresis, flushing,
hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus,
hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms
(e.g., nausea, vomiting, diarrhea).
The concomitant use of fluoxetine with MAOIs is contraindicated. In addition,
do not initiate Fluoxetine in a patient being treated with MAOIs such as
linezolid or intravenous methylene blue. No reports involved the
administration of methylene blue by other routes (such as oral tablets or
local tissue injection). If it is necessary to initiate treatment with an MAOI
such as linezolid or intravenous methylene blue in a patient taking
fluoxetine, discontinue fluoxetine before initiating treatment with the MAOI
[see Contraindications (4)and Drug Interactions (7.1)].
Monitor all patients taking fluoxetine for the emergence of serotonin
syndrome. Discontinue treatment with fluoxetine and any concomitant
serotonergic agents immediately if the above symptoms occur, and initiate
supportive symptomatic treatment. If concomitant use of fluoxetine with other
serotonergic drugs is clinically warranted, inform patients of the increased
risk for serotonin syndrome and monitor for symptoms
5.3 Allergic Reactions and Rash
In US fluoxetine clinical trials, 7% of 10,782 patients developed various
types of rashes and/or urticaria. Among the cases of rash and/or urticaria
reported in premarketing clinical trials, almost a third were withdrawn from
treatment because of the rash and/or systemic signs or symptoms associated
with the rash. Clinical findings reported in association with rash include
fever, leukocytosis, arthralgias, edema, carpal tunnel syndrome, respiratory
distress, lymphadenopathy, proteinuria, and mild transaminase elevation. Most
patients improved promptly with discontinuation of fluoxetine and/or
adjunctive treatment with antihistamines or steroids, and all patients
experiencing these reactions were reported to recover completely.
In premarketing clinical trials, 2 patients are known to have developed a
serious cutaneous systemic illness. In neither patient was there an
unequivocal diagnosis, but one was considered to have a leukocytoclastic
vasculitis, and the other, a severe desquamating syndrome that was considered
variously to be a vasculitis or erythema multiforme. Other patients have had
systemic syndromes suggestive of serum sickness.
Since the introduction of fluoxetine, systemic reactions, possibly related to
vasculitis and including lupus-like syndrome, have developed in patients with
rash. Although these reactions are rare, they may be serious, involving the
lung, kidney, or liver. Death has been reported to occur in association with
these systemic reactions.
Anaphylactoid reactions, including bronchospasm, angioedema, laryngospasm, and
urticaria alone and in combination, have been reported.
Pulmonary reactions, including inflammatory processes of varying
histopathology and/or fibrosis, have been reported rarely. These reactions
have occurred with dyspnea as the only preceding symptom.
Whether these systemic reactions and rash have a common underlying cause or
are due to different etiologies or pathogenic processes is not known.
Furthermore, a specific underlying immunologic basis for these reactions has
not been identified. Upon the appearance of rash or of other possibly allergic
phenomena for which an alternative etiology cannot be identified, fluoxetine
should be discontinued.
5.4 Screening Patients for Bipolar Disorder and Monitoring for
Mania/Hypomania
A major depressive episode may be the initial presentation of Bipolar
Disorder. It is generally believed (though not established in controlled
trials) that treating such an episode with an antidepressant alone may
increase the likelihood of precipitation of a mixed/manic episode in patients
at risk for Bipolar Disorder. Whether any of the symptoms described for
clinical worsening and suicide risk represent such a conversion is unknown.
However, prior to initiating treatment with an antidepressant, patients with
depressive symptoms should be adequately screened to determine if they are at
risk for Bipolar Disorder; such screening should include a detailed
psychiatric history, including a family history of suicide, Bipolar Disorder,
and depression. It should be noted that fluoxetine and olanzapine in
combination is approved for the acute treatment of depressive episodes
associated with Bipolar I Disorder [see Warnings and Precautions section of the package insert for Symbyax]. Fluoxetine monotherapy is not indicated for
the treatment of depressive episodes associated with Bipolar I Disorder.
In US placebo-controlled clinical trials for Major Depressive Disorder,
mania/hypomania was reported in 0.1% of patients treated with fluoxetine and
0.1% of patients treated with placebo. Activation of mania/hypomania has also
been reported in a small proportion of patients with Major Affective Disorder
treated with other marketed drugs effective in the treatment of Major
Depressive Disorder [see Use in Specific Populations (8.4)].
In US placebo-controlled clinical trials for OCD, mania/hypomania was reported
in 0.8% of patients treated with fluoxetine and no patients treated with
placebo. No patients reported mania/hypomania in US placebo-controlled
clinical trials for bulimia. In US fluoxetine clinical trials, 0.7% of 10,782
patients reported mania/hypomania [see Use in Specific Populations (8.4)].
5.5 Seizures
In US placebo-controlled clinical trials for Major Depressive Disorder, convulsions (or reactions described as possibly having been seizures) were reported in 0.1% of patients treated with fluoxetine and 0.2% of patients treated with placebo. No patients reported convulsions in US placebo- controlled clinical trials for either OCD or bulimia. In US fluoxetine clinical trials, 0.2% of 10,782 patients reported convulsions. The percentage appears to be similar to that associated with other marketed drugs effective in the treatment of Major Depressive Disorder. Fluoxetine should be introduced with care in patients with a history of seizures.
5.6 Altered Appetite and Weight
Significant weight loss, especially in underweight depressed or bulimic
patients, may be an undesirable result of treatment with fluoxetine.
In US placebo-controlled clinical trials for Major Depressive Disorder, 11% of
patients treated with fluoxetine and 2% of patients treated with placebo
reported anorexia (decreased appetite). Weight loss was reported in 1.4% of
patients treated with fluoxetine and in 0.5% of patients treated with placebo.
However, only rarely have patients discontinued treatment with fluoxetine
because of anorexia or weight loss [see Use in Specific Populations (8.4)].
In US placebo-controlled clinical trials for OCD, 17% of patients treated with
fluoxetine and 10% of patients treated with placebo reported anorexia
(decreased appetite). One patient discontinued treatment with fluoxetine
because of anorexia [see Use in Specific Populations (8.4)].
In US placebo-controlled clinical trials for Bulimia Nervosa, 8% of patients
treated with fluoxetine 60 mg and 4% of patients treated with placebo reported
anorexia (decreased appetite). Patients treated with fluoxetine 60 mg on
average lost 0.45 kg compared with a gain of 0.16 kg by patients treated with
placebo in the 16-week double-blind trial. Weight change should be monitored
during therapy.
5.7 Increased Risk of Bleeding
SNRIs and SSRIs, including fluoxetine, may increase the risk of bleeding
reactions. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs,
warfarin, and other anti-coagulants may add to this risk. Case reports and
epidemiological studies (case-control and cohort design) have demonstrated an
association between use of drugs that interfere with serotonin reuptake and
the occurrence of gastrointestinal bleeding. Bleeding reactions related to
SNRIs and SSRIs use have ranged from ecchymoses, hematomas, epistaxis, and
petechiae to life-threatening hemorrhages.
Patients should be cautioned about the risk of bleeding associated with the
concomitant use of fluoxetine and NSAIDs, aspirin, warfarin, or other drugs
that affect coagulation [see Drug Interactions (7.4)].
5.8 Angle-Closure Glaucoma
Angle-Closure Glaucoma — The pupillary dilation that occurs following use of many antidepressant drugs including fluoxetine may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.9 Hyponatremia
Hyponatremia has been reported during treatment with SNRIs and SSRIs,
including fluoxetine. In many cases, this hyponatremia appears to be the
result of the syndrome of inappropriate antidiuretic hormone secretion
(SIADH). Cases with serum sodium lower than 110 mmol/L have been reported and
appeared to be reversible when fluoxetine was discontinued. Elderly patients
may be at greater risk of developing hyponatremia with SNRIs and SSRIs. Also,
patients taking diuretics or who are otherwise volume depleted may be at
greater risk [see Use in Specific Populations (8.5)].
Discontinuation of fluoxetine should be considered in patients with
symptomatic hyponatremia and appropriate medical intervention should be
instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating,
memory impairment, confusion, weakness, and unsteadiness, which may lead to
falls. More severe and/or acute cases have been associated with hallucination,
syncope, seizure, coma, respiratory arrest, and death.
5.10 Anxiety and Insomnia
In US placebo-controlled clinical trials for Major Depressive Disorder, 12% to
16% of patients treated with fluoxetine and 7% to 9% of patients treated with
placebo reported anxiety, nervousness, or insomnia.
In US placebo-controlled clinical trials for OCD, insomnia was reported in 28%
of patients treated with fluoxetine and in 22% of patients treated with
placebo. Anxiety was reported in 14% of patients treated with fluoxetine and
in 7% of patients treated with placebo.
In US placebo-controlled clinical trials for Bulimia Nervosa, insomnia was
reported in 33% of patients treated with fluoxetine 60 mg, and 13% of patients
treated with placebo. Anxiety and nervousness were reported, respectively, in
15% and 11% of patients treated with fluoxetine 60 mg and in 9% and 5% of
patients treated with placebo.
Among the most common adverse reactions associated with discontinuation
(incidence at least twice that for placebo and at least 1% for fluoxetine in
clinical trials collecting only a primary reaction associated with
discontinuation) in US placebo-controlled fluoxetine clinical trials were
anxiety (2% in OCD), insomnia (1% in combined indications and 2% in bulimia),
and nervousness (1% in Major Depressive Disorder) [see Table 5].
5.11 QT Prolongation
Post-marketing cases of QT interval prolongation and ventricular arrhythmia
including Torsades de Pointes have been reported in patients treated with
fluoxetine. Fluoxetine should be used with caution in patients with congenital
long QT syndrome; a previous history of QT prolongation; a family history of
long QT syndrome or sudden cardiac death; and other conditions that predispose
to QT prolongation and ventricular arrhythmia. Such conditions include
concomitant use of drugs that prolong the QT interval; hypokalemia or
hypomagnesemia; recent myocardial infarction, uncompensated heart failure,
bradyarrhythmias, and other significant arrhythmias; and conditions that
predispose to increased fluoxetine exposure (overdose, hepatic impairment, use
of CYP2D6 inhibitors, CYP2D6 poor metabolizer status, or use of other highly
protein-bound drugs). Fluoxetine is primarily metabolized by CYP2D6 [see Contraindications (4.2), Adverse Reactions (6.2), Drug Interactions (7.7, 7.8), Overdosage (10),and Clinical Pharmacology (12.3)].
Pimozide and thioridazine are contraindicated for use with fluoxetine. Avoid
the concomitant use of drugs known to prolong the QT interval. These include
specific antipsychotics (e.g., ziprasidone, iloperidone, chlorpromazine,
mesoridazine, droperidol,); specific antibiotics (e.g., erythromycin,
gatifloxacin, moxifloxacin, sparfloxacin); Class 1A antiarrhythmic medications
(e.g., quinidine, procainamide); Class III antiarrhythmics (e.g., amiodarone,
sotalol); and others (e.g., pentamidine, levomethadyl acetate, methadone,
halofantrine, mefloquine, dolasetron mesylate, probucol or tacrolimus) [see Drug Interactions (7.7, 7.8) and Clinical Pharmacology (12.3)].
Consider ECG assessment and periodic ECG monitoring if initiating treatment
with fluoxetine in patients with risk factors for QT prolongation and
ventricular arrhythmia. Consider discontinuing fluoxetine and obtaining a
cardiac evaluation if patients develop signs or symptoms consistent with
ventricular arrhythmia.
5.12 Use in Patients with Concomitant Illness
Clinical experience with fluoxetine in patients with concomitant systemic
illness is limited. Caution is advisable in using fluoxetine in patients with
diseases or conditions that could affect metabolism or hemodynamic responses.
Cardiovascular — Fluoxetine has not been evaluated or used to any appreciable
extent in patients with a recent history of myocardial infarction or unstable
heart disease. Patients with these diagnoses were systematically excluded from
clinical studies during the product’s premarket testing. However, the
electrocardiograms of 312 patients who received fluoxetine in double-blind
trials were retrospectively evaluated; no conduction abnormalities that
resulted in heart block were observed. The mean heart rate was reduced by
approximately 3 beats/min.
Glycemic Control — In patients with diabetes, fluoxetine may alter glycemic
control. Hypoglycemia has occurred during therapy with fluoxetine, and
hyperglycemia has developed following discontinuation of the drug. As is true
with many other types of medication when taken concurrently by patients with
diabetes, insulin and/or oral hypoglycemic, dosage may need to be adjusted
when therapy with fluoxetine is instituted or discontinued.
5.13 Potential for Cognitive and Motor Impairment
As with any CNS-active drug, fluoxetine has the potential to impair judgment, thinking, or motor skills. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that the drug treatment does not affect them adversely.
5.14 Long Elimination Half-Life
Because of the long elimination half-lives of the parent drug and its major active metabolite, changes in dose will not be fully reflected in plasma for several weeks, affecting both strategies for titration to final dose and withdrawal from treatment. This is of potential consequence when drug discontinuation is required or when drugs are prescribed that might interact with fluoxetine and norfluoxetine following the discontinuation of fluoxetine [see Clinical Pharmacology (12.3)].
5.15 Discontinuation Adverse Reactions
During marketing of fluoxetine, SNRIs, and SSRIs, there have been spontaneous reports of adverse reactions occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, and hypomania. While these reactions are generally self-limiting, there have been reports of serious discontinuation symptoms. Patients should be monitored for these symptoms when discontinuing treatment with fluoxetine. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the healthcare provider may continue decreasing the dose but at a more gradual rate. Plasma fluoxetine and norfluoxetine concentration decrease gradually at the conclusion of therapy which may minimize the risk of discontinuation symptoms with this drug.
5.16 Fluoxetine and Olanzapine in Combination
When using fluoxetine and olanzapine in combination, also refer to the Warnings and Precautions section of the package insert for Symbyax.
5.17 Sexual Dysfunction
Use of SSRIs, including fluoxetine, may cause symptoms of sexual dysfunction
[see Adverse Reactions (6.1)]. In male patients, SSRI use may result in
ejaculatory delay or failure, decreased libido, and erectile dysfunction. In
female patients, SSRI use may result in decreased libido and delayed or absent
orgasm.
It is important for prescribers to inquire about sexual function prior to
initiation of fluoxetine and to inquire specifically about changes in sexual
function during treatment, because sexual function may not be spontaneously
reported. When evaluating changes in sexual function, obtaining a detailed
history (including timing of symptom onset) is important because sexual
symptoms may have other causes, including the underlying psychiatric disorder.
Discuss potential management strategies to support patients in making informed
decisions about treatment.
• Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults:
Monitor for clinical worsening and suicidal thinking and behavior (5.1)
• Serotonin Syndrome: Serotonin syndrome has been reported with SSRIs and
SNRIs, including fluoxetine, both when taken alone, but especially when co-
administered with other serotonergic agents. If such symptoms occur,
discontinue Fluoxetine capsules and serotonergic agents and initiate
supportive treatment. If concomitant use of Fluoxetine capsules with other
serotonergic drugs is clinically warranted, patients should be made aware of a
potential increased risk for serotonin syndrome, particularly during treatment
initiation and dose increases (5.2)
• Allergic Reactions and Rash: Discontinue upon appearance of rash or allergic
phenomena (5.3)
• Activation of Mania/Hypomania: Screen for Bipolar Disorder and monitor for
mania/hypomania (5.4)
• Seizures: Use cautiously in patients with a history of seizures or with
conditions that potentially lower the seizure threshold (5.5)
• Altered Appetite and Weight: Significant weight loss has occurred (5.6)
• Increased Risk of Bleeding: May increase the risk of bleeding. Use with
NSAIDs, aspirin, warfarin, or other drugs that affect coagulation may
potentiate the risk of gastrointestinal or other bleeding(5.7)
• Angle-Closure Glaucoma: Angle-closure glaucoma has occurred in patients with
untreated anatomically narrow angles treated with antidepressants (5.8)
• Hyponatremia: Has been reported with fluoxetine in association with syndrome
of inappropriate antidiuretic hormone (SIADH). Consider discontinuing if
symptomatic hyponatremia occurs (5.9)
• Anxiety and Insomnia: May occur (5.10)
• QT Prolongation: QT prolongation and ventricular arrhythmia including
Torsades de Pointes have been reported with fluoxetine use. Use with caution
in conditions that predispose to arrhythmias or increased fluoxetine exposure.
Use cautiously in patients with risk factors for QT prolongation (4.2, 5.11)
• Potential for Cognitive and Motor Impairment: Has potential to impair
judgment, thinking, and motor skills. Use caution when operating machinery
(5.13)
• Long Half-Life: Changes in dose will not be fully reflected in plasma for
several weeks(5.14)
• Fluoxetine and Olanzapine in Combination: When using fluoxetine and
olanzapine in combination, also refer to the Warnings and Precautions section
of the package insert for Symbyax (5.16)
• Sexual Dysfunction: Fluoxetine may cause symptoms of sexual dysfunction (5.17)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections
of the labeling:
• Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
[see Boxed Warningand Warnings and Precautions (5.1)]
• Serotonin Syndrome [see Warnings and Precautions (5.2)]
• Allergic Reactions and Rash [see Warnings and Precautions (5.3)]
• Screening Patients for Bipolar Disorder and Monitoring for Mania/Hypomania
[see Warnings and Precautions (5.4)]
• Seizures [see Warnings and Precautions (5.5)]
• Altered Appetite and Weight [see Warnings and Precautions (5.6)]
• Increased Risk of Bleeding [see Warnings and Precautions (5.7)]
• Angle-Closure Glaucoma [see Warnings and Precautions (5.8)]
• Hyponatremia [see Warnings and Precautions (5.9)]
• Anxiety and Insomnia [see Warnings and Precautions (5.10)]
• QT Prolongation [see Warnings and Precautions (5.11)]
• Potential for Cognitive and Motor Impairment [see Warnings and Precautions (5.13)]
• Discontinuation Adverse Reactions [see Warnings and Precautions (5.15)]
• Sexual Dysfunction [see Warnings and Precautions (5.17)]
When using fluoxetine and olanzapine in combination, also refer to the Adverse
Reactions section of the package insert for Symbyax.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse
reaction rates observed in the clinical trials of a drug cannot be directly
compared to rates in the clinical trials of another drug and may not reflect
or predict the rates observed in practice.
Multiple doses of fluoxetine have been administered to 10,782 patients with
various diagnoses in US clinical trials. In addition, there have been 425
patients administered fluoxetine in panic clinical trials. The stated
frequencies represent the proportion of individuals who experienced, at least
once, a treatment-emergent adverse reaction of the type listed. A reaction was
considered treatment-emergent if it occurred for the first time or worsened
while receiving therapy following baseline evaluation.
Incidence in Major Depressive Disorder, OCD, bulimia, and Panic Disorder
placebo-controlled clinical trials (excluding data from extensions of trials)
— Table 3 enumerates the most common treatment-emergent adverse reactions
associated with the use of fluoxetine (incidence of at least 5% for fluoxetine
and at least twice that for placebo within at least 1 of the indications) for
the treatment of Major Depressive Disorder, OCD, and bulimia in US controlled
clinical trials and Panic Disorder in US plus non-US controlled trials. Table
5 enumerates treatment-emergent adverse reactions that occurred in 2% or more
patients treated with fluoxetine and with incidence greater than placebo who
participated in US Major Depressive Disorder, OCD, and bulimia controlled
clinical trials and US plus non-US Panic Disorder controlled clinical trials.
Table 4 provides combined data for the pool of studies that are provided
separately by indication in Table 3.
Table 3: Most Common Treatment-Emergent Adverse Reactions: Incidence in
Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled
Clinical Trials****1,2
|
Percentage of Patients Reporting Event | ||||||||
|
Major Depressive Disorder |
OCD |
Bulimia |
Panic Disorder | |||||
|
Body System/ Adverse Reaction |
Fluoxetine (N=1728) |
Placebo (N=975) |
Fluoxetine (N=266) |
Placebo (N=89) |
Fluoxetine (N=450) |
Placebo (N=267) |
Fluoxetine (N=425) |
Placebo (N=342) |
|
Body as a Whole | ||||||||
|
Asthenia |
9 |
5 |
15 |
11 |
21 |
9 |
7 |
7 |
|
Flu syndrome |
3 |
4 |
10 |
7 |
8 |
3 |
5 |
5 |
|
Cardiovascular System | ||||||||
|
Vasodilatation |
3 |
2 |
5 |
-- |
2 |
1 |
1 |
-- |
|
Digestive System | ||||||||
|
Nausea |
21 |
9 |
26 |
13 |
29 |
11 |
12 |
7 |
|
Diarrhea |
12 |
8 |
18 |
13 |
8 |
6 |
9 |
4 |
|
Anorexia |
11 |
2 |
17 |
10 |
8 |
4 |
4 |
1 |
|
Dry mouth |
10 |
7 |
12 |
3 |
9 |
6 |
4 |
4 |
|
Dyspepsia |
7 |
5 |
10 |
4 |
10 |
6 |
6 |
2 |
|
Nervous System | ||||||||
|
Insomnia |
16 |
9 |
28 |
22 |
33 |
13 |
10 |
7 |
|
Anxiety |
12 |
7 |
14 |
7 |
15 |
9 |
6 |
2 |
|
Nervousness |
14 |
9 |
14 |
15 |
11 |
5 |
8 |
6 |
|
Somnolence |
13 |
6 |
17 |
7 |
13 |
5 |
5 |
2 |
|
Tremor |
10 |
3 |
9 |
1 |
13 |
1 |
3 |
1 |
|
Libido decreased |
3 |
-- |
11 |
2 |
5 |
1 |
1 |
2 |
|
Abnormal |
1 |
1 |
5 |
2 |
5 |
3 |
1 |
1 |
|
Respiratory System | ||||||||
|
Pharyngitis |
3 |
3 |
11 |
9 |
10 |
5 |
3 |
3 |
|
Sinusitis |
1 |
4 |
5 |
2 |
6 |
4 |
2 |
3 |
|
Yawn |
-- |
-- |
7 |
-- |
11 |
-- |
1 |
-- |
|
Skin and Appendages | ||||||||
|
Sweating |
8 |
3 |
7 |
-- |
8 |
3 |
2 |
2 |
|
Rash |
4 |
3 |
6 |
3 |
4 |
4 |
2 |
2 |
|
Urogenital System | ||||||||
|
Impotence3 |
2 |
-- |
-- |
-- |
7 |
-- |
1 |
-- |
|
Abnormal ejaculation3 |
-- |
-- |
7 |
-- |
7 |
-- |
2 |
1 |
1 Incidence less than 1%.
2 Includes US data for Major Depressive Disorder, OCD, Bulimia, and Panic
Disorder clinical trials, plus non-US data for Panic Disorder clinical trials.
3 Denominator used was for males only (N=690 Fluoxetine Major Depressive
Disorder; N=410 Placebo Major Depressive Disorder; N=116 Fluoxetine OCD; N=43
Placebo OCD; N=14 Fluoxetine Bulimia; N=1 Placebo Bulimia; N=162 Fluoxetine
Panic; N=121 Placebo Panic).
**Table 4: Treatment-Emergent Adverse Reactions: Incidence in Major Depressive
Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled Clinical Trials
**1,2
|
Percentage of Patients Reporting Event | ||
|
Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Combined | ||
|
Body System/ |
Fluoxetine (N=2869) |
Placebo (N=1673) |
|
Body as a Whole | ||
|
Headache |
21 |
19 |
|
Asthenia |
11 |
6 |
|
Flu syndrome |
5 |
4 |
|
Fever |
2 |
1 |
|
Cardiovascular System | ||
|
Vasodilatation |
2 |
1 |
|
Digestive System | ||
|
Nausea |
22 |
9 |
|
Diarrhea |
11 |
7 |
|
Anorexia |
10 |
3 |
|
Dry mouth |
9 |
6 |
|
Dyspepsia |
8 |
4 |
|
Constipation |
5 |
4 |
|
Flatulence |
3 |
2 |
|
Vomiting |
3 |
2 |
|
Metabolic and Nutritional Disorders | ||
|
Weight loss |
2 |
1 |
|
Nervous System | ||
|
Insomnia |
19 |
10 |
|
Nervousness |
13 |
8 |
|
Anxiety |
12 |
6 |
|
Somnolence |
12 |
5 |
|
Dizziness |
9 |
6 |
|
Tremor |
9 |
2 |
|
Libido decreased |
4 |
1 |
|
Thinking abnormal |
2 |
1 |
|
Respiratory System | ||
|
Yawn |
3 |
-- |
|
Skin and Appendages | ||
|
Sweating |
7 |
3 |
|
Rash |
4 |
3 |
|
Pruritus |
3 |
2 |
|
Special Senses | ||
|
Abnormal vision |
2 |
1 |
1 Incidence less than 1%.
2 Includes US data for Major Depressive Disorder, OCD, bulimia, and Panic
Disorder clinical trials, plus non-US data for Panic Disorder clinical trials.
Associated with discontinuation in Major Depressive Disorder, OCD, bulimia, and Panic Disorder placebo-controlled clinical trials (excluding data from extensions of trials) — Table 5 lists the adverse reactions associated with discontinuation of fluoxetine treatment (incidence at least twice that for placebo and at least 1% for fluoxetine in clinical trials collecting only a primary reaction associated with discontinuation) in Major Depressive Disorder, OCD, bulimia, and Panic Disorder clinical trials, plus non-US Panic Disorder clinical trials.
Table 5: Most Common Adverse Reactions Associated with Discontinuation in Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Placebo-Controlled Clinical Trials****1
|
Major Depressive Disorder, OCD, Bulimia, and Panic Disorder Combined (N=1533) |
Major Depressive Disorder (N=392) |
OCD (N=266) |
Bulimia (N=450) |
Panic Disorder (N=425) |
|
Anxiety (1%) |
-- |
Anxiety (2%) |
-- |
Anxiety (2%) |
|
-- |
-- |
-- |
Insomnia (2%) |
-- |
|
-- |
Nervousness (1%) |
-- |
-- |
Nervousness (1%) |
|
-- |
-- |
Rash (1%) |
-- |
-- |
1 Includes US Major Depressive Disorder, OCD, Bulimia, and Panic Disorder clinical trials, plus non-US Panic Disorder clinical trials.
Other adverse reactions in pediatric patients (children and adolescents) —
Treatment-emergent adverse reactions were collected in 322 pediatric patients
(180 fluoxetine-treated, 142 placebo-treated). The overall profile of adverse
reactions was generally similar to that seen in adult studies, as shown in
Tables 4 and 5. However, the following adverse reactions (excluding those
which appear in the body or footnotes of Tables 4 and 5 and those for which
the COSTART terms were uninformative or misleading) were reported at an
incidence of at least 2% for fluoxetine and greater than placebo: thirst,
hyperkinesia, agitation, personality disorder, epistaxis, urinary frequency,
and menorrhagia.
The most common adverse reaction (incidence at least 1% for fluoxetine and
greater than placebo) associated with discontinuation in 3 pediatric placebo-
controlled trials (N=418 randomized; 228 fluoxetine-treated; 190 placebo-
treated) was mania/hypomania (1.8% for fluoxetine-treated, 0% for placebo-
treated). In these clinical trials, only a primary reaction associated with
discontinuation was collected.
Male and female sexual dysfunction with SSRIs — Although changes in sexual
desire, sexual performance, and sexual satisfaction often occur as
manifestations of a psychiatric disorder, they may also be a consequence of
pharmacologic treatment. In particular, some evidence suggests that SSRIs can
cause such untoward sexual experiences. Reliable estimates of the incidence
and severity of untoward experiences involving sexual desire, performance, and
satisfaction are difficult to obtain, however, in part because patients and
healthcare providers may be reluctant to discuss them. Accordingly, estimates
of the incidence of untoward sexual experience and performance, cited in
product labeling, are likely to underestimate their actual incidence. In
patients enrolled in US Major Depressive Disorder, OCD, and bulimia placebo-
controlled clinical trials, decreased libido was the only sexual side effect
reported by at least 2% of patients taking fluoxetine (4% fluoxetine, <1%
placebo). There have been spontaneous reports in women taking fluoxetine of
orgasmic dysfunction, including anorgasmia.
There are no adequate and well-controlled studies examining sexual dysfunction
with fluoxetine treatment.
Symptoms of sexual dysfunction occasionally persist after discontinuation of
fluoxetine treatment.
Priapism has been reported with all SSRIs.
While it is difficult to know the precise risk of sexual dysfunction
associated with the use of SSRIs, healthcare providers should routinely
inquire about such possible side effects.
Other Reactions
Following is a list of treatment-emergent adverse reactions reported by
patients treated with fluoxetine in clinical trials. This listing is not
intended to include reactions (1) already listed in previous tables or
elsewhere in labeling, (2) for which a drug cause was remote, (3) which were
so general as to be uninformative, (4) which were not considered to have
significant clinical implications, or (5) which occurred at a rate equal to or
less than placebo.
Reactions are classified by body system using the following definitions:
frequent adverse reactions are those occurring in at least 1/100 patients;
infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients;
rare reactions are those occurring in fewer than 1/1000 patients.
Body as a Whole — Frequent: chills; Infrequent: suicide attempt; Rare:
acute abdominal syndrome, photosensitivity reaction.
Cardiovascular System — Frequent: palpitation; Infrequent: arrhythmia,
hypotension1.
Digestive System— Infrequent: dysphagia, gastritis, gastroenteritis,
melena, stomach ulcer; Rare: bloody diarrhea, duodenal ulcer, esophageal
ulcer, gastrointestinal hemorrhage, hematemesis, hepatitis, peptic ulcer,
stomach ulcer hemorrhage.
Hemic and Lymphatic System — Infrequent: ecchymosis; Rare: petechia,
purpura.
Investigations— Frequent: QT interval prolongation (QTcF ≥450 msec)3.
Nervous System — Frequent: emotional lability; Infrequent: akathisia,
ataxia, balance disorder1, bruxism1, buccoglossal syndrome, depersonalization,
euphoria, hypertonia, libido increased, myoclonus, paranoid reaction; Rare:
delusions.
Respiratory System — Rare: larynx edema.
Skin and Appendages — Infrequent: alopecia; Rare: purpuric rash.
Special Senses— Frequent: taste perversion; Infrequent: mydriasis.
Urogenital System — Frequent: micturition disorder; Infrequent: dysuria,
gynecological bleeding2.
1 MedDRA dictionary term from integrated database of placebo controlled trials
of 15870 patients, of which 9673 patients received fluoxetine.
2 Group term that includes individual MedDRA terms: cervix hemorrhage uterine,
dysfunctional uterine bleeding, genital hemorrhage, menometrorrhagia,
menorrhagia, metrorrhagia, polymenorrhea, postmenopausal hemorrhage, uterine
hemorrhage, vaginal hemorrhage. Adjusted for gender.
3 QT prolongation data are based on routine ECG measurements in clinical
trials.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use
of fluoxetine. Because these reactions are reported voluntarily from a
population of uncertain size, it is not always possible to reliably estimate
their frequency or evaluate a causal relationship to drug exposure.
Voluntary reports of adverse reactions temporally associated with fluoxetine
that have been received since market introduction and that may have no causal
relationship with the drug include the following: anosmia, aplastic anemia,
atrial fibrillation1, cataract, cerebrovascular accident1, cholestatic
jaundice, drug reaction with eosinophilia and systemic symptoms (DRESS),
dyskinesia (including, for example, a case of buccal-lingual-masticatory
syndrome with involuntary tongue protrusion reported to develop in a 77-year-
old female after 5 weeks of fluoxetine therapy and which completely resolved
over the next few months following drug discontinuation), eosinophilic
pneumonia 1, epidermal necrolysis, erythema multiforme, erythema nodosum,
exfoliative dermatitis, galactorrhea, gynecomastia, heart arrest 1, hepatic
failure/necrosis, hyperprolactinemia, hypoglycemia, hyposmia, immune-related
hemolytic anemia, kidney failure, memory impairment, movement disorders
developing in patients with risk factors including drugs associated with such
reactions and worsening of pre-existing movement disorders, optic neuritis,
pancreatitis 1, pancytopenia, pulmonary embolism, pulmonary hypertension, QT
prolongation, Stevens-Johnson syndrome, thrombocytopenia 1, thrombocytopenic
purpura, ventricular tachycardia (including Torsades de Pointes–type
arrhythmias), vaginal bleeding, and violent behaviors 1.
1 These terms represent serious adverse events, but do not meet the definition
for adverse drug reactions. They are included here because of their
seriousness.
Most common adverse reactions (≥5% and at least twice that for placebo)
associated with:
Major Depressive Disorder, Obsessive Compulsive Disorder, Bulimia, and Panic
Disorder: abnormal dreams, abnormal ejaculation, anorexia, anxiety, asthenia,
diarrhea, dry mouth, dyspepsia, flu syndrome, impotence, insomnia, libido
decreased, nausea, nervousness, pharyngitis, rash, sinusitis, somnolence,
sweating, tremor, vasodilatation, and yawn (6.1)
Fluoxetine and olanzapine in combination – Also refer to the Adverse Reactions
section of the package insert for Symbyax (6)
To report SUSPECTED ADVERSE REACTIONS, contact Marksans at 1-877-376-4271 or FDA at 1-800-FDA-1088 or****www.fda.gov/medwatch
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity — The dietary administration of fluoxetine to rats and mice
for 2 years at doses of up to 10 and 12 mg/kg/day, respectively [approximately 2.4 and 1.44 times, respectively, the maximum recommended human dose (MRHD) of 20 mg given to children on a mg/m2 basis], produced no evidence of
carcinogenicity.
Mutagenicity — Fluoxetine and norfluoxetine have been shown to have no
genotoxic effects based on the following assays: bacterial mutation assay, DNA
repair assay in cultured rat hepatocytes, mouse lymphoma assay, and in vivo
sister chromatid exchange assay in Chinese hamster bone marrow cells.
Impairment of Fertility — Two fertility studies conducted in adult rats at
doses of up to 7.5 and 12.5 mg/kg/day (approximately 0.97 and 1.6 times,
respectively, the MRHD of 60 mg given to adolescents on a mg/m2 basis)
indicated that fluoxetine had no adverse effects on fertility. However,
adverse effects on fertility were seen when juvenile rats were treated with
fluoxetine [see Use in Specific Populations (8.4)].
13.2 Animal Toxicology and/or Pharmacology
Phospholipids are increased in some tissues of mice, rats, and dogs given fluoxetine chronically. This effect is reversible after cessation of fluoxetine treatment. Phospholipid accumulation in animals has been observed with many cationic amphiphilic drugs, including fenfluramine, imipramine, and ranitidine. The significance of this effect in humans is unknown.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
Efficacy for fluoxetine was established for the:
• Acute and maintenance treatment of Major Depressive Disorder in adults, and
children and adolescents (8 to 18 years) in 7 short-term and 2 long-term,
placebo-controlled trials [see Clinical Studies 14.1].
• Acute treatment of obsessions and compulsions in adults, and children and
adolescents (7 to 17 years) with Obsessive Compulsive Disorder (OCD) in 3
short-term placebo-controlled trials [see Clinical Studies (14.2)].
• Acute and maintenance treatment of binge-eating and vomiting behaviors in
adult patients with moderate to severe Bulimia Nervosa in 3 short-term and 1
long-term, placebo-controlled trials [see Clinical Studies (14.3)].
• Acute treatment of Panic Disorder, with or without agoraphobia, in adult
patients in 2 short-term, placebo- controlled trials [see Clinical Studies (14.4)].
Efficacy for fluoxetine and olanzapine in combination was established for the:
• Acute treatment of depressive episodes in Bipolar I Disorder in adults, and
children and adolescents (10 to 17 years) in 3 short-term, placebo-controlled
trials.
• Acute and maintenance treatment of treatment resistant depression in adults
(18 to 85 years) in 3 short-term, placebo-controlled trials and 1 randomized
withdrawal study with an active control.
When using fluoxetine and olanzapine in combination, also refer to the
Clinical Studies section of the package insert for Symbyax.
14.1 Major Depressive Disorder
Daily Dosing
Adult — The efficacy of fluoxetine was studied in 5- and 6-week placebo-
controlled trials with depressed adult and geriatric outpatients (≥18 years of
age) whose diagnoses corresponded most closely to the DSM-III (currently DSM-
IV) category of Major Depressive Disorder. Fluoxetine was shown to be
significantly more effective than placebo as measured by the Hamilton
Depression Rating Scale (HAM-D). Fluoxetine was also significantly more
effective than placebo on the HAM-D subscores for depressed mood, sleep
disturbance, and the anxiety subfactor.
Two 6-week controlled studies (N=671, randomized) comparing fluoxetine 20 mg
and placebo have shown fluoxetine 20 mg daily to be effective in the treatment
of elderly patients (≥60 years of age) with Major Depressive Disorder. In
these studies, fluoxetine produced a significantly higher rate of response and
remission as defined, respectively, by a 50% decrease in the HAM-D score and a
total endpoint HAM-D score of ≤8. Fluoxetine was well tolerated and the rate
of treatment discontinuations due to adverse reactions did not differ between
fluoxetine (12%) and placebo (9%).
Pediatric (children and adolescents) — The efficacy of fluoxetine 20 mg/day in
children and adolescents (N=315 randomized; 170 children ages 8 to <13, 145
adolescents ages 13 to ≤18) was studied in two 8- to 9-week placebo-controlled
clinical trials in depressed outpatients whose diagnoses corresponded most
closely to the DSM-III-R or DSM-IV category of Major Depressive Disorder.
In both studies independently, fluoxetine produced a statistically
significantly greater mean change on the Childhood Depression Rating Scale-
Revised (CDRS-R) total score from baseline to endpoint than did placebo.
Subgroup analyses on the CDRS-R total score did not suggest any differential
responsiveness on the basis of age or gender.
Maintenance Treatment
A study was conducted involving depressed outpatients who had responded
(modified HAMD-17 score of ≤7 during each of the last 3 weeks of open-label
treatment and absence of Major Depressive Disorder by DSM-III-R criteria) by
the end of an initial 12-week open-treatment phase on fluoxetine 20 mg/day.
These patients (N=298) were randomized to continuation on double-blind
fluoxetine 20 mg/day or placebo. At 38 weeks (50 weeks total), a statistically
significantly lower relapse rate (defined as symptoms sufficient to meet a
diagnosis of Major Depressive Disorder for 2 weeks or a modified HAMD-17 score
of ≥14 for 3 weeks) was observed for patients taking fluoxetine compared with
those on placebo.
An additional maintenance study was conducted involving adult outpatients
meeting DSM-IV criteria for Major Depressive Disorder who had responded
(defined as having a modified HAMD-17 score of ≤9, a CGI-Severity rating of
≤2, and no longer meeting criteria for Major Depressive Disorder) for 3
consecutive weeks at the end of 13 weeks of open-label treatment with
fluoxetine 20 mg once daily. These patients were randomized to double-blind,
once-weekly continuation treatment with fluoxetine delayed-release capsules 90
mg once weekly, fluoxetine 20 mg once daily, or placebo. Fluoxetine 20 mg once
daily demonstrated superior efficacy (having a significantly longer time to
relapse of depressive symptoms) compared with placebo for a period of 25
weeks.
14.2 Obsessive Compulsive Disorder
Adult — The effectiveness of fluoxetine for the treatment of Obsessive
Compulsive Disorder (OCD) was demonstrated in two 13-week, multicenter,
parallel group studies (Studies 1 and 2) of adult outpatients who received
fixed fluoxetine doses of 20, 40, or 60 mg/day (on a once-a-day schedule, in
the morning) or placebo. Patients in both studies had moderate to severe OCD
(DSM-III-R), with mean baseline ratings on the Yale-Brown Obsessive Compulsive
Scale (YBOCS, total score) ranging from 22 to 26. In Study 1, patients
receiving fluoxetine experienced mean reductions of approximately 4 to 6 units
on the YBOCS total score, compared with a 1-unit reduction for placebo
patients. In Study 2, patients receiving fluoxetine experienced mean
reductions of approximately 4 to 9 units on the YBOCS total score, compared
with a 1-unit reduction for placebo patients. While there was no indication of
a dose-response relationship for effectiveness in Study 1, a dose-response
relationship was observed in Study 2, with numerically better responses in the
2 higher dose groups. The following table provides the outcome classification
by treatment group on the Clinical Global Impression (CGI) improvement scale
for Studies 1 and 2 combined:
Table 6
|
Outcome Classification (%) on CGI Improvement Scale for Completers in Pool of Two OCD Studies | ||||
|
Fluoxetine | ||||
|
Outcome Classification |
Placebo |
20 mg |
40 mg |
60 mg |
|
Worse |
8% |
0% |
0% |
0% |
|
No change |
64% |
41% |
33% |
29% |
|
Minimally improved |
17% |
23% |
28% |
24% |
|
Much improved |
8% |
28% |
27% |
28% |
|
Very much improved |
3% |
8% |
12% |
19% |
Exploratory analyses for age and gender effects on outcome did not suggest any
differential responsiveness on the basis of age or sex.
Pediatric (children and adolescents) — In one 13-week clinical trial in
pediatric patients (N=103 randomized; 75 children ages 7 to <13, 28
adolescents ages 13 to <18) with OCD (DSM-IV), patients received fluoxetine 10
mg/day for 2 weeks, followed by 20 mg/day for 2 weeks. The dose was then
adjusted in the range of 20 to 60 mg/day on the basis of clinical response and
tolerability. Fluoxetine produced a statistically significantly greater mean
change from baseline to endpoint than did placebo as measured by the
Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS).
Subgroup analyses on outcome did not suggest any differential responsiveness
on the basis of age or gender.
14.3 Bulimia Nervosa
The effectiveness of fluoxetine for the treatment of bulimia was demonstrated
in two 8-week and one 16-week, multicenter, parallel group studies of adult
outpatients meeting DSM-III-R criteria for bulimia. Patients in the 8-week
studies received either 20 or 60 mg/day of fluoxetine or placebo in the
morning. Patients in the 16-week study received a fixed fluoxetine dose of 60
mg/day (once a day) or placebo. Patients in these 3 studies had moderate to
severe bulimia with median binge-eating and vomiting frequencies ranging from
7 to 10 per week and 5 to 9 per week, respectively. In these 3 studies,
fluoxetine 60 mg, but not 20 mg, was statistically significantly superior to
placebo in reducing the number of binge-eating and vomiting episodes per week.
The statistically significantly superior effect of 60 mg versus placebo was
present as early as Week 1 and persisted throughout each study. The fluoxetine
-related reduction in bulimic episodes appeared to be independent of baseline
depression as assessed by the Hamilton Depression Rating Scale. In each of
these 3 studies, the treatment effect, as measured by differences between
fluoxetine 60 mg and placebo on median reduction from baseline in frequency of
bulimic behaviors at endpoint, ranged from 1 to 2 episodes per week for binge-
eating and 2 to 4 episodes per week for vomiting. The size of the effect was
related to baseline frequency, with greater reductions seen in patients with
higher baseline frequencies. Although some patients achieved freedom from
binge-eating and purging as a result of treatment, for the majority, the
benefit was a partial reduction in the frequency of binge-eating and purging.
In a longer-term trial, 150 patients meeting DSM-IV criteria for Bulimia
Nervosa, purging subtype, who had responded during a single-blind, 8-week
acute treatment phase with fluoxetine 60 mg/day, were randomized to
continuation of fluoxetine 60 mg/day or placebo, for up to 52 weeks of
observation for relapse. Response during the single-blind phase was defined by
having achieved at least a 50% decrease in vomiting frequency compared with
baseline. Relapse during the double-blind phase was defined as a persistent
return to baseline vomiting frequency or healthcare provider judgment that the
patient had relapsed. Patients receiving continued fluoxetine 60 mg/day
experienced a significantly longer time to relapse over the subsequent 52
weeks compared with those receiving placebo.
14.4 Panic Disorder
The effectiveness of fluoxetine in the treatment of Panic Disorder was
demonstrated in 2 double-blind, randomized, placebo-controlled, multicenter
studies of adult outpatients who had a primary diagnosis of Panic Disorder
(DSM-IV), with or without agoraphobia.
Study 1 (N=180 randomized) was a 12-week flexible-dose study. Fluoxetine was
initiated at 10 mg/day for the first week, after which patients were dosed in
the range of 20 to 60 mg/day on the basis of clinical response and
tolerability. A statistically significantly greater percentage of fluoxetine
-treated patients were free from panic attacks at endpoint than placebo-
treated patients, 42% versus 28%, respectively.
Study 2 (N=214 randomized) was a 12-week flexible-dose study. Fluoxetine was
initiated at 10 mg/day for the first week, after which patients were dosed in
a range of 20 to 60 mg/day on the basis of clinical response and tolerability.
A statistically significantly greater percentage of fluoxetine -treated
patients were free from panic attacks at endpoint than placebo-treated
patients, 62% versus 44%, respectively.
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
When using fluoxetine and olanzapine in combination, also refer to the Use in Specific Populations section of the package insert for Symbyax.
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in
women exposed to antidepressants during pregnancy. Healthcare providers are
encouraged to register patients by calling the National Pregnancy Registry for
Antidepressants at 1-844-405-6185 or visiting online at
https://womensmentalhealth.org/clinical-and-research- programs/pregnancy
registry/antidepressants/.
Risk Summary
Based on data from published observational studies, exposure to SSRIs,
particularly in the month before delivery, has been associated with a less
than 2-fold increase in the risk of postpartum hemorrhage [see Warnings and Precautions (5.7) and Clinical Considerations].
Available data from published epidemiologic studies and postmarketing reports
over several decades have not established an increased risk of major birth
defects or miscarriage. Some studies have reported an increased incidence of
cardiovascular malformations; however, these studies results do not establish
a causal relationship (see Data). There are risks associated with untreated
depression in pregnancy and risks of persistent pulmonary hypertension of the
newborn (PPHN) (see Data) and poor neonatal adaptation with exposure to
selective serotonin reuptake inhibitors (SSRIs), including fluoxetine, during
pregnancy (see Clinical Considerations).
In rats and rabbits treated with fluoxetine during the period of
organogenesis, there was no evidence of developmental effects at doses up to
1.6 and 3.9 times, respectively, the maximum recommended human dose (MRHD) of
60 mg/day given to adolescents on a mg/m2 basis. However, in other
reproductive studies in rats, an increase in stillborn pups, a decrease in pup
weight, and an increase in pup deaths early after birth occurred at doses that
are 1.5 times (during gestation) and 0.97 time (during gestation and
lactation) the MRHD given to adolescents on a mg/m2 basis.
The estimated background risk of major birth defects and miscarriage for the
indicated population is unknown. All pregnancies have a background risk of
birth defect, loss, or other adverse outcomes. In the US general population,
the estimated background risk of major birth defects and miscarriage in
clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Women who discontinue antidepressants during pregnancy are more likely to
experience a relapse of major depression than women who continue
antidepressants. This finding is from a prospective, longitudinal study that
followed 201 pregnant women with a history of major depressive disorder who
were euthymic and taking antidepressants at the beginning of pregnancy.
Consider the risk of untreated depression when discontinuing or changing
treatment with antidepressant medication during pregnancy and postpartum.
Maternal Adverse Reactions
Use of fluoxetine in the month before delivery may be associated with an
increased risk of postpartum hemorrhage [see Warnings and Precautions (5.7)].
Fetal/Neonatal adverse reactions Neonates exposed to fluoxetine and other SSRI
or SNRIs late in the third trimester have developed complications requiring
prolonged hospitalization, respiratory support, and tube feeding. Such
complications can arise immediately upon delivery. Reported clinical findings
have included respiratory distress, cyanosis, apnea, seizures, temperature
instability, feeding difficulty, vomiting, hypoglycemia, hypotonia,
hypertonia, hyperreflexia, tremors, jitteriness, irritability, and constant
crying. These findings are consistent with either a direct toxic effect of
SSRIs and SNRIs or possibly a drug discontinuation syndrome. It should be
noted that, in some cases, the clinical picture is consistent with serotonin
syndrome [see Warnings and Precautions (5.2)].
Data
Human Data — It has been shown that SSRIs (including fluoxetine) can cross the
placenta. Published epidemiological studies of pregnant women exposed to
fluoxetine have not established an increased risk of major birth defects,
miscarriage, and other adverse developmental outcomes. Several publications
reported an increased incidence of cardiovascular malformations in children
with in utero exposure to fluoxetine. However, these studies results do not
establish a causal relationship. Methodologic limitations of these
observational studies include possible exposure and outcome misclassification,
lack of adequate controls, adjustment for confounders and confirmatory
studies. However, these studies cannot definitely establish or exclude any
drug-associated risk during pregnancy. Exposure to SSRIs, particularly later
in pregnancy, may have an increased risk for PPHN. PPHN occurs in 1-2 per 1000
live births in the general population and is associated with substantial
neonatal morbidity and mortality.
Animal Data — In embryofetal development studies in rats and rabbits, there
was no evidence of malformations or developmental variations following
administration of fluoxetine at doses up to 12.5 and 15 mg/kg/day,
respectively (1.6 and 3.9 times, respectively, the MRHD of 60 mg given to
adolescents on a mg/m2 basis) throughout organogenesis. However, in rat
reproduction studies, an increase in stillborn pups, a decrease in pup weight,
and an increase in pup deaths during the first 7 days postpartum occurred
following maternal exposure to 12 mg/kg/day (1.5 times the MRHD given to
adolescents on a mg/m2 basis) during gestation or 7.5 mg/kg/day (0.97 time the
MRHD given to adolescents on a mg/m2 basis) during gestation and lactation.
There was no evidence of developmental neurotoxicity in the surviving
offspring of rats treated with 12 mg/kg/day during gestation. The no-effect
dose for rat pup mortality was 5 mg/kg/day (0.65 time the MRHD given to
adolescents on a mg/m2 basis).
8.2 Lactation
Risk Summary
Data from published literature report the presence of fluoxetine and
norfluoxetine in human milk (see Data). There are reports of agitation,
irritability, poor feeding, and poor weight gain in infants exposed to
fluoxetine through breast milk (see Clinical Considerations). There are no
data on the effect of fluoxetine or its metabolites on milk production. The
developmental and health benefits of breastfeeding should be considered along
with the mother’s clinical need for fluoxetine and any potential adverse
effects on the breastfed child from fluoxetine or the underlying maternal
condition.
Clinical Considerations
Infants exposed to fluoxetine should be monitored for agitation, irritability,
poor feeding, and poor weight gain.
Data
A study of 19 nursing mothers on fluoxetine with daily doses of 10-60 mg
showed that fluoxetine was detectable in 30% of nursing infant sera (range: 1
to 84 ng/mL) whereas norfluoxetine was found in 85% (range: <1 to 265 ng/mL).
8.4 Pediatric Use
Use of fluoxetine in children — The efficacy of fluoxetine for the treatment
of Major Depressive Disorder was demonstrated in two 8- to 9-week placebo-
controlled clinical trials with 315 pediatric outpatients ages 8 to ≤18 [see Clinical Studies (14.1)].
The efficacy of fluoxetine for the treatment of OCD was demonstrated in one
13-week placebo-controlled clinical trial with 103 pediatric outpatients ages
7 to <18 [see Clinical Studies (14.2)].
The safety and effectiveness in pediatric patients <8 years of age in Major
Depressive Disorder and <7 years of age in OCD have not been established.
Fluoxetine pharmacokinetics were evaluated in 21 pediatric patients (ages 6 to
≤18) with Major Depressive Disorder or OCD [see Clinical Pharmacology (12.3)].
The acute adverse reaction profiles observed in the 3 studies (N=418
randomized; 228 fluoxetine-treated, 190 placebo-treated) were generally
similar to that observed in adult studies with fluoxetine. The longer-term
adverse reaction profile observed in the 19-week Major Depressive Disorder
study (N=219 randomized; 109 fluoxetine-treated, 110 placebo-treated) was also
similar to that observed in adult trials with fluoxetine [see Adverse Reactions (6.1)].
Manic reaction, including mania and hypomania, was reported in 6 (1 mania, 5
hypomania) out of 228 (2.6%) fluoxetine-treated patients and in 0 out of 190
(0%) placebo-treated patients. Mania/hypomania led to the discontinuation of 4
(1.8%) fluoxetine-treated patients from the acute phases of the 3 studies
combined. Consequently, regular monitoring for the occurrence of
mania/hypomania is recommended.
As with other SSRIs, decreased weight gain has been observed in association
with the use of fluoxetine in children and adolescent patients. After 19 weeks
of treatment in a clinical trial, pediatric subjects treated with fluoxetine
gained an average of 1.1 cm less in height and 1.1 kg less in weight than
subjects treated with placebo. In addition, fluoxetine treatment was
associated with a decrease in alkaline phosphatase levels. The safety of
fluoxetine treatment for pediatric patients has not been systematically
assessed for chronic treatment longer than several months in duration. In
particular, there are no studies that directly evaluate the longer-term
effects of fluoxetine on the growth, development and maturation of children
and adolescent patients. Therefore, height and weight should be monitored
periodically in pediatric patients receiving fluoxetine [see Warnings and Precautions (5.6)].
Fluoxetine is approved for use in pediatric patients with MDD and OCD [see Box Warning and Warnings and Precautions (5.1)]. Anyone considering the use of
fluoxetine in a child or adolescent must balance the potential risks with the
clinical need.
Animal Data — Significant toxicity on muscle tissue, neurobehavior,
reproductive organs, and bone development has been observed following exposure
of juvenile rats to fluoxetine from weaning through maturity. Oral
administration of fluoxetine to rats from weaning postnatal day 21 through
adulthood day 90 at 3, 10, or 30 mg/kg/day was associated with testicular
degeneration and necrosis, epididymal vacuolation and hypospermia (at 30
mg/kg/day corresponding to plasma exposures [AUC] approximately 5-10 times the
average AUC in pediatric patients at the MRHD of 20 mg/day), increased serum
levels of creatine kinase (at AUC as low as 1 - 2 times the average AUC in
pediatric patients at the MRHD of
20 mg/day), skeletal muscle degeneration and necrosis, decreased femur
length/growth and body weight gain (at AUC 5 - 10 times the average AUC in
pediatric patients at the MRHD of 20 mg/day). The high dose of 30 mg/kg/day
exceeded a maximum tolerated dose. When animals were evaluated after a drug-
free period (up to 11 weeks after cessation of dosing), fluoxetine was
associated with neurobehavioral abnormalities (decreased reactivity at AUC as
low as approximately 0.1-0.2 times the average AUC in pediatric patients at
the MRHD and learning deficit at the high dose), and reproductive functional
impairment (decreased mating at all doses and impaired fertility at the high
dose). In addition, the testicular and epididymal microscopic lesions and
decreased sperm concentrations found in high dose group were also observed,
indicating that the drug effects on reproductive organs are irreversible. The
reversibility of fluoxetine-induced muscle damage was not assessed.
These fluoxetine toxicities in juvenile rats have not been observed in adult
animals. Plasma exposures (AUC) to fluoxetine in juvenile rats receiving 3,
10, or 30 mg/kg/day doses in this study are approximately 0.1 - 0.2, 1 - 2,
and 5 - 10 times, respectively, the average exposure in pediatric patients
receiving the MRHD of 20 mg/day. Rat exposures to the major metabolite,
norfluoxetine, are approximately 0.3 - 0.8, 1 - 8, and 3 - 20 times,
respectively, the pediatric exposure at the MRHD.
A specific effect on bone development was reported in juvenile mice
administered fluoxetine by the intraperitoneal route to 4 week old mice for 4
weeks at doses 0.5 and 2 times the oral MRHD of 20 mg/day on mg/m2 basis.
There was a decrease in bone mineralization and density at both doses, but the
overall growth (body weight gain or femur length) was not affected.
Use of fluoxetine in combination with olanzapine in children and adolescents:
Safety and efficacy of fluoxetine and olanzapine in combination in patients 10
to 17 years of age have been established for the acute treatment of depressive
episodes associated with Bipolar I Disorder. Safety and effectiveness of
fluoxetine and olanzapine in combination in patients less than 10 years of age
have not been established.
8.5 Geriatric Use
U.S fluoxetine clinical trials included 687 patients ≥65 years of age and 93
patients ≥75 years of age. The efficacy in geriatric patients has been
established [see Clinical Studies (14.1)]. For pharmacokinetic information in
geriatric patients, [see Clinical Pharmacology (12.4)]. No overall differences
in safety or effectiveness were observed between these subjects and younger
subjects, and other reported clinical experience has not identified
differences in responses between the elderly and younger patients, but greater
sensitivity of some older individuals cannot be ruled out. SNRIs and SSRIs,
including fluoxetine, have been associated with cases of clinically
significant hyponatremia in elderly patients, who may be at greater risk for
this adverse reaction [see Warnings and Precautions (5.9)].
Clinical studies of olanzapine and fluoxetine in combination did not include
sufficient numbers of patients ≥65 years of age to determine whether they
respond differently from younger patients.
8.6 Hepatic Impairment
In subjects with cirrhosis of the liver, the clearances of fluoxetine and its active metabolite, norfluoxetine, were decreased, thus increasing the elimination half-lives of these substances. A lower or less frequent dose of fluoxetine should be used in patients with cirrhosis. Caution is advised when using fluoxetine in patients with diseases or conditions that could affect its metabolism [see Dosage and Administration (2.7) and Clinical Pharmacology (12.4)].
• Pregnancy: SSRI use, particularly later in pregnancy, may increase risk for
persistent pulmonary hypertension and symptoms of poor adaptation (respiratory
distress, temperature instability, feeding difficulty, hypotonia, tremor,
irritability) in the neonate (8.1)
• Pediatric Use: Safety and effectiveness of fluoxetine in patients
<8 years of age with Major Depressive Disorder and <7 years of age with OCD
have not been established. Safety and effectiveness of fluoxetine and
olanzapine in combination in patients <10 years of age for depressive episodes
associated with Bipolar I Disorder have not been established (8.4)
• Hepatic Impairment: Lower or less frequent dosing may be appropriate in
patients with cirrhosis (8.6)
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.3 Dependence
Fluoxetine has not been systematically studied, in animals or humans, for its potential for abuse, tolerance, or physical dependence. While the premarketing clinical experience with fluoxetine did not reveal any tendency for a withdrawal syndrome or any drug seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed. Consequently, healthcare providers should carefully evaluate patients for history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of fluoxetine (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
DESCRIPTION SECTION
11 DESCRIPTION
Fluoxetine capsules, USP are a selective serotonin reuptake inhibitor for oral administration. It is designated (±)-N- methyl-3-phenyl-3-[(α,α,α-trifluoro-p- tolyl)oxy]propylamine hydrochloride and has the empirical formula of C17H18F3NO•HCl. Its molecular weight is 345.79. The structural formula is:
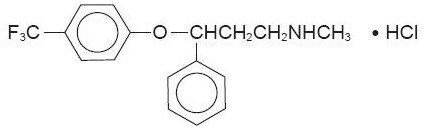
Fluoxetine hydrochloride, USP is a white to off-white crystalline solid with a
solubility of 14 mg/mL in water.
Each capsule contains fluoxetine hydrochloride equivalent to 10 mg (32.3
µmol), 20 mg (64.7 µmol), or 40 mg (129.3 µmol) of fluoxetine and the
following inactive ingredients: pregelatinized starch. The capsule shells and
imprinting ink contain FD&C Blue- 1 (brilliant blue FCF), gelatin, titanium
dioxide, sodium lauryl sulfate, shellac, povidone, sodium hydroxide, black
iron oxide and potassium hydroxide.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Although the exact mechanism of fluoxetine is unknown, it is presumed to be linked to its inhibition of CNS neuronal uptake of serotonin.
12.2 Pharmacodynamics
Studies at clinically relevant doses in man have demonstrated that fluoxetine
blocks the uptake of serotonin into human platelets. Studies in animals also
suggest that fluoxetine is a much more potent uptake inhibitor of serotonin
than of norepinephrine.
Antagonism of muscarinic, histaminergic, and α1-adrenergic receptors has been
hypothesized to be associated with various anticholinergic, sedative, and
cardiovascular effects of classical tricyclic antidepressant (TCA) drugs.
Fluoxetine binds to these and other membrane receptors from brain tissue much
less potently in vitro than do the tricyclic drugs.
12.3 Pharmacokinetics
Systemic Bioavailability — In man, following a single oral 40 mg dose, peak
plasma concentrations of fluoxetine from 15 to 55 ng/mL are observed after 6
to 8 hours.
Food does not appear to affect the systemic bioavailability of fluoxetine,
although it may delay its absorption by 1 to 2 hours, which is probably not
clinically significant. Thus, fluoxetine may be administered with or without
food.
Protein Binding — Over the concentration range from 200 to 1000 ng/mL,
approximately 94.5% of fluoxetine is bound in vitro to human serum proteins,
including albumin and α1-glycoprotein. The interaction between fluoxetine and
other highly protein-bound drugs has not been fully evaluated, but may be
important.
Enantiomers — Fluoxetine is a racemic mixture (50/50) of R-fluoxetine and
S-fluoxetine enantiomers. In animal models, both enantiomers are specific and
potent serotonin uptake inhibitors with essentially equivalent pharmacologic
activity. The S-fluoxetine enantiomer is eliminated more slowly and is the
predominant enantiomer present in plasma at steady state.
Metabolism — Fluoxetine is extensively metabolized in the liver to
norfluoxetine and a number of other unidentified metabolites. The only
identified active metabolite, norfluoxetine, is formed by demethylation of
fluoxetine. In animal models, S-norfluoxetine is a potent and selective
inhibitor of serotonin uptake and has activity essentially equivalent to R-
or S-fluoxetine. R-norfluoxetine is significantly less potent than the parent
drug in the inhibition of serotonin uptake. The primary route of elimination
appears to be hepatic metabolism to inactive metabolites excreted by the
kidney.
Variability in Metabolism — A subset (about 7%) of the population has reduced
activity of the drug metabolizing enzyme cytochrome P450 2D6 (CYP2D6). Such
individuals are referred to as “poor metabolizers” of drugs such as
debrisoquin, dextromethorphan, and the TCAs. In a study involving labeled and
unlabeled enantiomers administered as a racemate, these individuals
metabolized S-fluoxetine at a slower rate and thus achieved higher
concentrations of S-fluoxetine. Consequently, concentrations of
S-norfluoxetine at steady state were lower. The metabolism of R-fluoxetine in
these poor metabolizers appears normal. When compared with normal
metabolizers, the total sum at steady state of the plasma concentrations of
the 4 active enantiomers was not significantly greater among poor
metabolizers. Thus, the net pharmacodynamic activities were essentially the
same. Alternative, nonsaturable pathways (non-2D6) also contribute to the
metabolism of fluoxetine. This explains how fluoxetine achieves a steady-state
concentration rather than increasing without limit.
Because fluoxetine’s metabolism, like that of a number of other compounds
including TCAs and other selective serotonin reuptake inhibitors (SSRIs),
involves the CYP2D6 system, concomitant therapy with drugs also metabolized by
this enzyme system (such as the TCAs) may lead to drug interactions [see Drug Interactions (7.7)].
Accumulation and Slow Elimination — The relatively slow elimination of
fluoxetine (elimination half-life of 1 to 3 days after acute administration
and 4 to 6 days after chronic administration) and its active metabolite,
norfluoxetine (elimination half-life of 4 to 16 days after acute and chronic
administration), leads to significant accumulation of these active species in
chronic use and delayed attainment of steady state, even when a fixed dose is
used [see Warnings and Precautions (5.14)]. After 30 days of dosing at 40
mg/day, plasma concentrations of fluoxetine in the range of 91 to
302 ng/mL and norfluoxetine in the range of 72 to 258 ng/mL have been
observed. Plasma concentrations of fluoxetine were higher than those predicted
by single-dose studies, because fluoxetine’s metabolism is not proportional to
dose. Norfluoxetine, however, appears to have linear pharmacokinetics. Its
mean terminal half-life after a single dose was 8.6 days and after multiple
dosing was 9.3 days. Steady-state levels after prolonged dosing are similar to
levels seen at 4 to 5 weeks.
The long elimination half-lives of fluoxetine and norfluoxetine assure that,
even when dosing is stopped, active drug substance will persist in the body
for weeks (primarily depending on individual patient characteristics, previous
dosing regimen, and length of previous therapy at discontinuation). This is of
potential consequence when drug discontinuation is required or when drugs are
prescribed that might interact with fluoxetine and norfluoxetine following the
discontinuation of fluoxetine.
12.4 Specific Populations
Liver Disease — As might be predicted from its primary site of metabolism,
liver impairment can affect the elimination of fluoxetine. The elimination
half-life of fluoxetine was prolonged in a study of cirrhotic patients, with a
mean of 7.6 days compared with the range of 2 to 3 days seen in subjects
without liver disease; norfluoxetine elimination was also delayed, with a mean
duration of 12 days for cirrhotic patients compared with the range of 7 to 9
days in normal subjects. This suggests that the use of fluoxetine in patients
with liver disease must be approached with caution. If fluoxetine is
administered to patients with liver disease, a lower or less frequent dose
should be used [see Dosage and Administration (2.7) and Use in Specific Populations (8.6)].
Renal Disease — In depressed patients on dialysis (N=12), fluoxetine
administered as 20 mg once daily for 2 months produced steady-state fluoxetine
and norfluoxetine plasma concentrations comparable with those seen in patients
with normal renal function. While the possibility exists that renally excreted
metabolites of fluoxetine may accumulate to higher levels in patients with
severe renal dysfunction, use of a lower or less frequent dose is not
routinely necessary in renally impaired patients.
Geriatric Pharmacokinetics — The disposition of single doses of fluoxetine in
healthy elderly subjects (>65 years of age) did not differ significantly from
that in younger normal subjects. However, given the long half-life and
nonlinear disposition of the drug, a single-dose study is not adequate to rule
out the possibility of altered pharmacokinetics in the elderly, particularly
if they have systemic illness or are receiving multiple drugs for concomitant
diseases. The effects of age upon the metabolism of fluoxetine have been
investigated in 260 elderly but otherwise healthy depressed patients (≥60
years of age) who received 20 mg fluoxetine for 6 weeks. Combined fluoxetine
plus norfluoxetine plasma concentrations were 209.3 ± 85.7 ng/mL at the end of
6 weeks. No unusual age-associated pattern of adverse reactions was observed
in those elderly patients.
Pediatric Pharmacokinetics (children and adolescents) — Fluoxetine
pharmacokinetics were evaluated in 21 pediatric patients (10 children ages 6
to <13, 11 adolescents ages 13 to <18) diagnosed with Major Depressive
Disorder or Obsessive Compulsive Disorder (OCD). Fluoxetine 20 mg/day was
administered for up to 62 days. The average steady-state concentrations of
fluoxetine in these children were 2-fold higher than in adolescents (171 and
86 ng/mL, respectively). The average norfluoxetine steady-state concentrations
in these children were 1.5-fold higher than in adolescents (195 and 113 ng/mL,
respectively). These differences can be almost entirely explained by
differences in weight. No gender-associated difference in fluoxetine
pharmacokinetics was observed. Similar ranges of fluoxetine and norfluoxetine
plasma concentrations were observed in another study in 94 pediatric patients
(ages 8 to <18) diagnosed with Major Depressive Disorder.
Higher average steady-state fluoxetine and norfluoxetine concentrations were
observed in children relative to adults; however, these concentrations were
within the range of concentrations observed in the adult population. As in
adults, fluoxetine and norfluoxetine accumulated extensively following
multiple oral dosing; steady-state concentrations were achieved within 3 to 4
weeks of daily dosing.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Fluoxetine Capsules, USP 10 mg* are white to off-white powder filled in size
‘2’ hard gelatin capsules with opaque light blue cap and opaque light blue
body, imprinted “FLUOXETINE 10 mg” on cap and “R147” on body with white ink
and are supplied in bottles of 30,100,1000.
Bottles of 30 NDC 25000-147-03
Bottles of 100 NDC 25000-147-08
Bottles of 1000 NDC 25000-147-14
Fluoxetine Capsules, USP 20 mg* are white to off-white powder filled in size
‘2’ hard gelatin capsules with opaque light blue cap and opaque light
torquoise blue body, imprinted “FLUOXETINE 20 mg” on cap and “R148” on body
with black ink and are supplied in bottles of 100, 1000.
Bottles of 100 NDC 25000-148-08
Bottles of 1000 NDC 25000-148-14
Fluoxetine Capsules, USP 40 mg* are white to off-white powder filled in size ‘0’ hard gelatin capsules with opaque light blue cap and opaque white body, imprinted “FLUOXETINE 40 mg” on cap and “R149” on body with black ink and are supplied in bottles of 100,500.
Bottles of 100 NDC 25000-149-08
Bottles of 500 NDC 25000-149-12
- Fluoxetine base equivalent.
16.2 Storage and Handling
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59°
to 86°F) [see USP Controlled Room Temperature].
Protect from light.
Dispense in a tight, light-resistant container with a child-resistant closure.
SPL MEDGUIDE SECTION
SPL MEDGUIDE SECTION
Medication Guide
** Fluoxetine (floo ox' e teen) Capsules, USP**
for oral use
Read the Medication Guide that comes with fluoxetine capsules before you start
taking it and each time you get a refill. There may be new information. This
Medication Guide does not take the place of talking to your healthcare
provider about your medical condition or treatment. Talk with your healthcare
provider if there is something you do not understand or want to learn more
about.
What is the most important information I should know about fluoxetine
capsules?
Fluoxetine capsules and other antidepressant medicines may cause serious side
effects, including:
1. Suicidal thoughts or actions:
• Fluoxetine capsules and other antidepressant medicines may increase
suicidal thoughts or actions in some children, teenagers, or young adults
within the** first few months of treatment or when the dose is changed.**
• Depression or other serious mental illnesses are the most important causes
of suicidal thoughts or actions.
• Watch for these changes and call your healthcare provider right away if you
notice:
• New or sudden changes in mood, behavior, actions, thoughts, or feelings,
especially if severe.
• Pay particular attention to such changes when fluoxetine capsules are
started or when the dose is changed.
Keep all follow-up visits with your healthcare provider and call between
visits if you are worried about symptoms.
Call your healthcare provider right away if you have any of the following
symptoms, or call 911 if an emergency, especially if they are new, worse, or
worry you:
• attempts to commit suicide
• acting on dangerous impulses
• acting aggressive or violent
• thoughts about suicide or dying
• new or worse depression
• new or worse anxiety or panic attacks
• feeling agitated, restless, angry or irritable
• trouble sleeping
• an increase in activity or talking more than what is normal for you
• other unusual changes in behavior or mood
Call your healthcare provider right away if you have any of the following
symptoms, or call 911 if an emergency. Fluoxetine capsules may be associated
with these serious side effects:
2. Serotonin Syndrome. This condition can be life-threatening and may
include:
• agitation, hallucinations, coma or other changes in mental status
• coordination problems or muscle twitching (overactive reflexes)
• racing heartbeat, high or low blood pressure
• sweating or fever
• nausea, vomiting, or diarrhea
• muscle rigidity
• dizziness
• flushing
• tremor
• seizures
3. Severe allergic reactions:
• trouble breathing
• swelling of the face, tongue, eyes or mouth
• rash, itchy welts (hives) or blisters, alone or with fever or joint pain
4. Abnormal bleeding: Fluoxetine capsules and other antidepressant
medicines may increase your risk of bleeding or bruising, especially if you
take the blood thinner warfarin (Coumadin®, Jantoven®), a non-steroidal anti-
inflammatory drug (NSAIDs, like ibuprofen or naproxen), or aspirin.
5. Visual problems:
• eye pain
• changes in vision
• swelling or redness in or around the eye
Only some people are at risk for these problems. You may want to undergo an
eye examination to see if you are at risk and receive preventative treatment
if you are.
6. Seizures or convulsions
7. Manic episodes:
• greatly increased energy
• severe trouble sleeping
• racing thoughts
• reckless behavior
• unusually grand ideas
• excessive happiness or irritability
• talking more or faster than usual
8. Changes in appetite or weight. Children and adolescents should have
height and weight monitored during treatment.
9. Low salt (sodium) levels in the blood. Elderly people may be at greater
risk for this. Symptoms may include:
• headache
• weakness or feeling unsteady
• confusion, problems concentrating or thinking or memory problems
10. Changes in the electrical activity of your heart (QT prolongation and
ventricular arrhythmia including Torsades de Pointes). This condition can be
life threatening. The symptoms may include:
• fast, slow, or irregular heartbeat
• shortness of breath
• dizziness or fainting
*11. Sexual problems (dysfunction).Taking selective serotonin reuptake
inhibitors (SSRIs), including fluoxetine capsules, may cause sexual problems.
• Symptoms in males may include:
• Delayed ejaculation or inability to have an ejaculation
• Decreased sex drive
• Problems getting or keeping an erection
• Symptoms in females may include:
• Decreased sex drive
• Delayed orgasm or inability to have an orgasm
Talk to your healthcare provider if you develop any changes in your sexual
function or if you have any questions or concerns about sexual problems during
treatment with fluoxetine capsules. There may be treatments your healthcare
provider can suggest.
Do not stop fluoxetine capsules without first talking to your healthcare
provider. Stopping fluoxetine capsules too quickly may cause serious
symptoms including:
• anxiety, irritability, high or low mood, feeling restless or changes in
sleep habits
• headache, sweating, nausea, dizziness
• electric shock-like sensations, shaking, confusion
What are fluoxetine capsules?
Fluoxetine capsules are a prescription medicine used to treat depression. It
is important to talk with your healthcare provider about the risks of treating
depression and also the risks of not treating it. You should discuss all
treatment choices with your healthcare provider.
Fluoxetine capsules are used to treat:
• Major Depressive Disorder (MDD)
• Obsessive Compulsive Disorder (OCD)
• Bulimia Nervosa
• Panic Disorder
• Depressive episodes associated with Bipolar I Disorder, taken with
olanzapine (Zyprexa)
• Treatment Resistant Depression (depression that has not gotten better with
at least 2 other treatments), taken with olanzapine (Zyprexa)
Not approved for use in children
Talk to your healthcare provider if you do not think that your condition is
getting better with fluoxetine capsules treatment.
** Who should not take fluoxetine capsules?
Do not take fluoxetine capsules if you:
• are allergic to fluoxetine hydrochloride or any of the ingredients in
fluoxetine capsules. See the end of this Medication Guide for a complete list
of ingredients in fluoxetine capsules.
• take a Monoamine Oxidase Inhibitor (MAOI). Ask your healthcare provider or
pharmacist if you are not sure if you take an MAOI, including the antibiotic
linezolid.
• Do not take an MAOI within 5 weeks of stopping fluoxetine capsules unless
directed to do so by your physician.
• Do not start fluoxetine capsules if you stopped taking an MAOI in the last 2
weeks unless directed to do so by your physician.
People who take fluoxetine capsules close in time to an MAOI may have
serious or even life-threatening side effects. Get medical help right away if
you have any of these symptoms:
• high fever
• uncontrolled muscle spasms
• stiff muscles
• rapid changes in heart rate or blood pressure
• confusion
• loss of consciousness (pass out)
• take Mellaril® (thioridazine). Do not take Mellaril® within 5 weeks of
stopping fluoxetine capsules because this can cause serious heart rhythm
problems or sudden death.
• take the antipsychotic medicine pimozide (Orap®) because this can cause
serious heart problems.
What should I tell my healthcare provider before taking fluoxetine capsules?
Ask if you are not sure.
Before starting fluoxetine capsules, tell your healthcare provider if you:
• Are taking certain drugs or treatments such as:
• Triptans used to treat migraine headache
• Medicines used to treat mood, anxiety, psychotic or thought disorders,
including tricyclics, lithium, buspirone, SSRIs, SNRIs, MAOIs or
antipsychotics
• Amphetamines
• Tramadol, fentanyl, meperidine, methadone, or other opioids
• Over-the-counter supplements such as tryptophan or St. John’s Wort
• Electroconvulsive therapy (ECT)
• have liver problems
• have kidney problems
• have heart problems
• have or had seizures or convulsions
• have bipolar disorder or mania
• have low sodium levels in your blood
• have a history of a stroke
• have high blood pressure
• have or had bleeding problems
• are pregnant or plan to become pregnant. Taking fluoxetine capsules late in
pregnancy may lead to an increased risk of certain problems in your newborn.
Talk to your healthcare provider about the benefits and risks of treating
depression during pregnancy.
○ If you become pregnant while taking fluoxetine capsules, talk to your
healthcare provider about registering with the National Pregnancy Registry for
Antidepressants. You can register by calling 1-844-405-6185 or go to
https://womensmentalhealth.org/clinical-and-research-
programs/pregnancyregistry/antidepressants/.
• are breast-feeding or plan to breast-feed. Fluoxetine may pass into your
breast milk. Talk to your healthcare provider about the best way to feed your
baby if taking fluoxetine capsules.
Tell your healthcare provider about all the medicines that you take,
including prescription and non-prescription medicines, vitamins, and herbal
supplements.
Fluoxetine capsules and some medicines may interact with each other, may not
work as well, or may cause serious side effects.
Your healthcare provider or pharmacist can tell you if it is safe to take
fluoxetine capsules with your other medicines. Do not start or stop any
medicine while taking fluoxetine capsules without talking to your healthcare
provider first.
If you take fluoxetine capsules, you should not take any other medicines that
contain fluoxetine hydrochloride including:
|
•Symbyax |
How should I take fluoxetine capsules?
• Take fluoxetine capsules exactly as prescribed. Your healthcare provider may
need to change the dose of fluoxetine capsules until it is the right dose for
you.
• Fluoxetine capsules may be taken with or without food.
• If you miss a dose of fluoxetine capsules, take the missed dose as soon as
you remember. If it is almost time for the next dose, skip the missed dose and
take your next dose at the regular time. Do not take two doses of fluoxetine
capsules at the same time.
• If you take too much fluoxetine capsules, call your healthcare provider or
poison control center right away, or get emergency treatment.
** What should I avoid while taking fluoxetine capsules?**
Fluoxetine capsules can cause sleepiness or may affect your ability to make
decisions, think clearly, or react quickly. You should not drive, operate
heavy machinery, or do other dangerous activities until you know how
fluoxetine capsules affects you. Do not drink alcohol while using fluoxetine
capsules.
** What are the possible side effects of fluoxetine capsules?**
Fluoxetine capsules may cause serious side effects, including:
• See “What is the most important information I should know about fluoxetine
capsules?”
• Problems with blood sugar control. People who have diabetes and take
fluoxetine capsules may have problems with low blood sugar while taking
fluoxetine capsules. High blood sugar can happen when fluoxetine capsules are
stopped. Your healthcare provider may need to change the dose of your diabetes
medicines when you start or stop taking fluoxetine capsules.
• Feeling anxious or trouble sleeping
Common possible side effects in people who take fluoxetine capsules include:
• unusual dreams
• sexual problems
• loss of appetite, diarrhea, indigestion, nausea or vomiting, weakness, or
dry mouth
• flu symptoms
• feeling tired or fatigued
• change in sleep habits
• yawning
• sinus infection or sore throat
• tremor or shaking
• sweating
• feeling anxious or nervous
• hot flashes
• rash
Other side effects in children and adolescents include:
• increased thirst
• abnormal increase in muscle movement or agitation
• nose bleed
• urinating more often
• heavy menstrual periods
• possible slowed growth rate and weight change. Your child’s height and
weight should be monitored during treatment with fluoxetine capsules.
Tell your healthcare provider if you have any side effect that bothers you or
that does not go away. These are not all the possible side effects of
fluoxetine capsules. For more information, ask your healthcare provider or
pharmacist.
CALL YOUR DOCTOR FOR MEDICAL ADVICE ABOUT SIDE EFFECTS. YOU MAY REPORT SIDE
EFFECTS TO THE FDA AT 1-800-FDA-1088.
** How should I store fluoxetine capsules?**
• Store fluoxetine capsules at 20° to 25°C (68° to 77°F); excursions permitted
to 15° to 30°C (59° to 86°F).
• Keep fluoxetine capsules away from light.
• Keep fluoxetine capsules bottle closed tightly.
Keep fluoxetine capsules and all medicines out of the reach of children.
General information about fluoxetine capsules
Medicines are sometimes prescribed for purposes other than those listed in a
Medication Guide. Do not use fluoxetine capsules for a condition for which it
was not prescribed. Do not give fluoxetine capsules to other people, even if
they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about
fluoxetine capsules. If you would like more information, talk with your
healthcare provider. You may ask your healthcare provider or pharmacist for
information about fluoxetine capsules that is written for healthcare
professionals.
For more information about fluoxetine capsules call Marksans at
1-877-376-4271.
What are the ingredients in fluoxetine capsules?
Active ingredient: fluoxetine hydrochloride USP
Inactive ingredients: pregelatinized starch. The capsule shells and imprinting ink contain FD&C Blue - 1 (brilliant blue FCF), gelatin, titanium dioxide, sodium lauryl sulfate, shellac, povidone, sodium hydroxide, black iron oxide and potassium hydroxide.
All trademarks are the property of their respective owners.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Time-Cap Labs, lnc.
7 Michael Avenue, Farmingdale,
NY 11735, USA
Manufactured by:
Marksans Pharma Ltd.
Plot No. L-82, L-83 Verna Indl. Estate
Verna, Goa-403722, India
Revised: 09/2023
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Major Depressive Disorder
Initial Treatment
Adult — Initiate fluoxetine 20 mg/day orally in the morning. Consider a dose
increase after several weeks if insufficient clinical improvement is observed.
Administer doses above 20 mg/day once daily in the morning or twice daily
(i.e., morning and noon).The maximum fluoxetine dose should not exceed 80
mg/day.
In controlled trials used to support the efficacy of fluoxetine, patients were
administered morning doses ranging from 20 to 80 mg/day. Studies comparing
fluoxetine 20, 40, and 60 mg/day to placebo indicate that 20 mg/day is
sufficient to obtain a satisfactory response in Major Depressive Disorder in
most cases [see Clinical Studies (14.1)].
Pediatric (children and adolescents) — Initiate fluoxetine 10 or 20 mg/day.
After 1 week at 10 mg/day, increase the dose to 20 mg/day. However, due to
higher plasma levels in lower weight children, the starting and target dose in
this group may be 10 mg/day. Consider a dose increase to 20 mg/day after
several weeks if insufficient clinical improvement is observed. In the short-
term (8 to 9 week) controlled clinical trials of fluoxetine supporting its
effectiveness in the treatment of Major Depressive Disorder, patients were
administered fluoxetine doses of 10 to 20 mg/day [see Clinical Studies (14.1)].
All patients — As with other drugs effective in the treatment of Major
Depressive Disorder, the full effect may be delayed until 4 weeks of treatment
or longer.
Periodically reassess to determine the need for maintenance treatment.
Switching Patients to a Tricyclic Antidepressant (TCA) — Dosage of a TCA may
need to be reduced, and plasma TCA concentrations may need to be monitored
temporarily when fluoxetine is coadministered or has been recently
discontinued [see Warnings and Precautions (5.2) and Drug Interactions (7.7)].
2.2 Obsessive Compulsive Disorder
Initial Treatment
Adult — Initiate fluoxetine 20 mg/day, orally in the morning. Consider a dose
increase after several weeks if insufficient clinical improvement is observed.
The full therapeutic effect may be delayed until 5 weeks of treatment or
longer. Administer doses above 20 mg/day once daily in the morning or twice
daily (i.e., morning and noon). A dose range of 20 to 60 mg/day is
recommended; however, doses of up to 80 mg/day have been well tolerated in
open studies of OCD. The maximum fluoxetine dose should not exceed 80 mg/day.
In the controlled clinical trials of fluoxetine supporting its effectiveness
in the treatment of OCD, patients were administered fixed daily doses of 20,
40, or 60 mg of fluoxetine or placebo [see Clinical Studies (14.2)]. In one of
these studies, no dose-response relationship for effectiveness was
demonstrated.
Pediatric (children and adolescents) — In adolescents and higher weight
children, initiate treatment with a dose of 10 mg/day. After 2 weeks, increase
the dose to 20 mg/day. Consider additional dose increases after several more
weeks if insufficient clinical improvement is observed. A dose range of 20 to
60 mg/day is recommended.
In lower weight children, initiate treatment with a dose of 10 mg/day.
Consider additional dose increases after several more weeks if insufficient
clinical improvement is observed. A dose range of 20 to 30 mg/day is
recommended. Experience with daily doses greater than 20 mg is very minimal,
and there is no experience with doses greater than 60 mg.
In the controlled clinical trial of fluoxetine supporting its effectiveness in
the treatment of OCD, patients were administered fluoxetine doses in the range
of 10 to 60 mg/day [see Clinical Studies (14.2)].
Periodically reassess to determine the need for treatment.
2.3 Bulimia Nervosa
Initial Treatment — Administer fluoxetine 60 mg/day in the morning. For some
patients it may be advisable to titrate up to this target dose over several
days. Fluoxetine doses above 60 mg/day have not been systematically studied in
patients with bulimia. In the controlled clinical trials of fluoxetine
supporting its effectiveness in the treatment of Bulimia Nervosa, patients
were administered fixed daily fluoxetine doses of 20 or 60 mg, or placebo [see Clinical Studies (14.3)]. Only the 60 mg dose was statistically significantly
superior to placebo in reducing the frequency of binge-eating and vomiting.
Periodically reassess to determine the need for maintenance treatment.
2.4 Panic Disorder
Initial Treatment — Initiate treatment with fluoxetine 10 mg/day. After one
week, increase the dose to 20 mg/day. Consider a dose increase after several
weeks if no clinical improvement is observed. Fluoxetine doses above 60 mg/day
have not been systematically evaluated in patients with Panic Disorder. In the
controlled clinical trials of fluoxetine supporting its effectiveness in the
treatment of Panic Disorder, patients were administered fluoxetine doses in
the range of 10 to 60 mg/day [see Clinical Studies (14.4)]. The most
frequently administered dose in the 2 flexible-dose clinical trials was 20
mg/day.
Periodically reassess to determine the need for continued treatment.
2.5 Fluoxetine and Olanzapine in Combination: Depressive Episodes
Associated with Bipolar I Disorder
When using fluoxetine and olanzapine in combination, also refer to the
Clinical Studies section of the package insert for Symbyax.
Adult — Administer fluoxetine in combination with oral olanzapine once daily
in the evening, without regard to meals, generally beginning with 5 mg of oral
olanzapine and 20 mg of fluoxetine. Make dosage adjustments, if indicated,
according to efficacy and tolerability within dose ranges of fluoxetine 20 to
50 mg and oral olanzapine 5 to 12.5 mg.
Antidepressant efficacy was demonstrated with olanzapine and fluoxetine in
combination with a dose range of olanzapine 6 to 12 mg and fluoxetine 25 to 50
mg. Safety of co-administration of doses above 18 mg olanzapine with 75 mg
fluoxetine has not been evaluated in clinical studies. Periodically re-examine
the need for continued pharmacotherapy.
Children and adolescents (10 -17 years of age) — Administer olanzapine and
fluoxetine combination once daily in the evening, generally beginning with 2.5
mg of olanzapine and 20 mg of fluoxetine. Make dosage adjustments, if
indicated, according to efficacy and tolerability. Safety of co-administration
of doses above 12 mg of olanzapine with 50 mg of fluoxetine has not been
evaluated in pediatric clinical studies. Periodically re-examine the need for
continued pharmacotherapy.
Safety and efficacy of fluoxetine in combination with olanzapine was
determined in clinical trials supporting approval of Symbyax (fixed-dose
combination of olanzapine and fluoxetine). Symbyax is dosed between 3 mg/25 mg
(olanzapine/fluoxetine) per day and 12 mg/50 mg (olanzapine/fluoxetine) per
day. The following table demonstrates the appropriate individual component
doses of fluoxetine and olanzapine versus Symbyax. Adjust dosage, if
indicated, with the individual components according to efficacy and
tolerability.
Table 1: Approximate Dose Correspondence Between Symbyax1 and the Combination of Fluoxetine and Olanzapine
|
|
Use in Combination | |
|
For Symbyax (mg/day) |
Olanzapine (mg/day) |
Fluoxetine (mg/day) |
|
3 mg olanzapine/25 mg fluoxetine |
2.5 |
20 |
|
6 mg olanzapine/25 mg fluoxetine |
5 |
20 |
|
12 mg olanzapine/25 mg fluoxetine |
10+2.5 |
20 |
|
6 mg olanzapine/50 mg fluoxetine |
5 |
40+10 |
|
12 mg olanzapine/50 mg fluoxetine |
10+2.5 |
40+10 |
1Symbyax (olanzapine/fluoxetine HCL) is a fixed-dose combination of
fluoxetine and olanzapine.
Fluoxetine monotherapy is not indicated for the treatment of depressive
episodes associated with Bipolar I Disorder.****
2.6 Fluoxetine and Olanzapine in Combination: Treatment Resistant
Depression
When using fluoxetine and olanzapine in combination, also refer to the
Clinical Studies section of the package insert for Symbyax.
Administer fluoxetine in combination with oral olanzapine once daily in the
evening, without regard to meals, generally beginning with 5 mg of oral
olanzapine and 20 mg of fluoxetine. Adjust dosage, if indicated, according to
efficacy and tolerability within dose ranges of fluoxetine 20 to 50 mg and
oral olanzapine 5 to 20 mg. Antidepressant efficacy was demonstrated with
olanzapine and fluoxetine in combination with a dose range of olanzapine 6 to
18 mg and fluoxetine 25 to 50 mg.
Safety and efficacy of fluoxetine in combination with olanzapine was
determined in clinical trials supporting approval of Symbyax (fixed dose
combination of olanzapine and fluoxetine). Symbyax is dosed between 3 mg/25 mg
(olanzapine/fluoxetine) per day and 12 mg/50 mg (olanzapine/fluoxetine) per
day. Table 1 demonstrates the appropriate individual component doses of
fluoxetine and olanzapine versus Symbyax. Adjust dosage, if indicated, with
the individual components according to efficacy and tolerability.
Periodically re-examine the need for continued pharmacotherapy.
Safety of coadministration of doses above 18 mg olanzapine with 75 mg
fluoxetine has not been evaluated in clinical studies.
Fluoxetine monotherapy is not indicated for the treatment of treatment
resistant depression (Major Depressive Disorder in patients who do not respond
to 2 antidepressants of adequate dose and duration in the current episode).
2.7 Dosing in Specific Populations
Geriatric — Consider a lower or less frequent dosage for the elderly [see Use in Specific Populations (8.5)].
Hepatic Impairment — As with many other medications, use a lower or less
frequent dosage in patients with hepatic impairment [see Clinical Pharmacology (12.4) and Use in Specific Populations (8.6)].
Concomitant Illness — Patients with concurrent disease or on multiple
concomitant medications may require dosage adjustments [see Clinical Pharmacology (12.4) and Warnings and Precautions (5.12)].
Fluoxetine and Olanzapine in Combination — Use a starting dose of oral
olanzapine 2.5 to 5 mg with fluoxetine
20 mg for patients with a predisposition to hypotensive reactions, patients
with hepatic impairment, or patients who exhibit a combination of factors that
may slow the metabolism of olanzapine or fluoxetine in combination (female
gender, geriatric age, non-smoking status), or those patients who may be
pharmacodynamically sensitive to olanzapine. Titrate slowly and adjust dosage
as needed in patients who exhibit a combination of factors that may slow
metabolism.
Fluoxetine and olanzapine in combination have not been systematically studied in patients over 65 years of age or in patients less than 10 years of age [see Warnings and Precautions (5.16) and Drug Interactions (7.7)].
2.8 Discontinuation of Treatment
Symptoms associated with discontinuation of fluoxetine, SNRIs, and SSRIs, have been reported [see Warnings and Precautions (5.15)].
2.9 Switching a Patient To or From a Monoamine Oxidase Inhibitor (MAOI)
Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with fluoxetine. Conversely, at least 5 weeks should be allowed after stopping fluoxetine before starting an MAOI intended to treat psychiatric disorders [see Contraindications (4.1)].
2.10 Use of Fluoxetine with Other MAOIs such as Linezolid or Methylene Blue
Do not start fluoxetine in a patient who is being treated with linezolid or
intravenous methylene blue because there is an increased risk of serotonin
syndrome. In a patient who requires more urgent treatment of a psychiatric
condition, other interventions, including hospitalization, should be
considered [see Contraindications (4.1)].
In some cases, a patient already receiving fluoxetine therapy may require
urgent treatment with linezolid or intravenous methylene blue. If acceptable
alternatives to linezolid or intravenous methylene blue treatment are not
available and the potential benefits of linezolid or intravenous methylene
blue treatment are judged to outweigh the risks of serotonin syndrome in a
particular patient, fluoxetine should be stopped promptly, and linezolid or
intravenous methylene blue can be administered. The patient should be
monitored for symptoms of serotonin syndrome for five weeks or until 24 hours
after the last dose of linezolid or intravenous methylene blue, whichever
comes first. Therapy with fluoxetine may be resumed 24 hours after the last
dose of linezolid or intravenous methylene blue [see Warnings and Precautions (5.2)].
The risk of administering methylene blue by non-intravenous routes (such as
oral tablets or by local injection) or in intravenous doses much lower than 1
mg/kg with Fluoxetine is unclear. The healthcare provider should,
nevertheless, be aware of the possibility of emergent symptoms of serotonin
syndrome with such use [see Warnings and Precautions (5.2)].
|
Indication |
Adult |
Pediatric |
|
MDD (2.1) |
20 mg/day in am (initial dose) |
10 to 20 mg/day (initial dose) |
|
OCD (2.2) |
20 mg/day in am (initial dose) |
10 mg/day (initial dose) |
|
Bulimia Nervosa (2.3) |
60 mg/day in am | |
|
Panic Disorder (2.4) |
10 mg/day (initial dose) | |
|
Depressive Episodes Associated with Bipolar I Disorder (2.5) |
Oral in combination with olanzapine: 5 mg of oral olanzapine and 20 mg of fluoxetine once daily (initial dose) |
Oral in combination with olanzapine: 2.5 mg of oral olanzapine and 20 mg of
fluoxetine once |
|
Treatment Resistant Depression (2.6) |
Oral in combination with olanzapine: 5 mg of oral olanzapine and 20 mg of
fluoxetine once daily |
• A lower or less frequent dosage should be used in patients with hepatic
impairment, the elderly, and for patients with concurrent disease or on
multiple concomitant medications (2.7)
Fluoxetine and olanzapine in combination:
• Dosage adjustments should be made with the individual components according
to efficacy and tolerability (2.5, 2.6)
• Fluoxetine monotherapy is not indicated for the treatment of Depressive
Episodes associated with Bipolar I Disorder or treatment resistant depression
(2.5, 2.6)
• Safety of the coadministration of doses above 18 mg olanzapine with 75 mg
fluoxetine has not been evaluated in adults (2.5,2.6)
• Safety of the coadministration of doses above 12 mg olanzapine with 50 mg
fluoxetine has not been evaluated in children and adolescents ages 10 to 17
(2.5)
