Junel
Junel 21 Day (norethindrone acetate and ethinyl estradiol tablets USP)Junel Fe 28 Day(norethindrone acetate and ethinyl estradiol tablets USP and ferrous fumarate tablets*)*Ferrous fumarate tablets are not USP for dissolution and assay.
8b82ad14-580c-4145-b825-dce849f95363
HUMAN PRESCRIPTION DRUG LABEL
Aug 14, 2023
Teva Pharmaceuticals USA, Inc.
DUNS: 001627975
Products 4
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Norethindrone Acetate and Ethinyl Estradiol
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Norethindrone Acetate and Ethinyl Estradiol
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Norethindrone Acetate and Ethinyl Estradiol and Ferrous Fumarate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Norethindrone Acetate and Ethinyl Estradiol and Ferrous Fumarate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
Drug Labeling Information
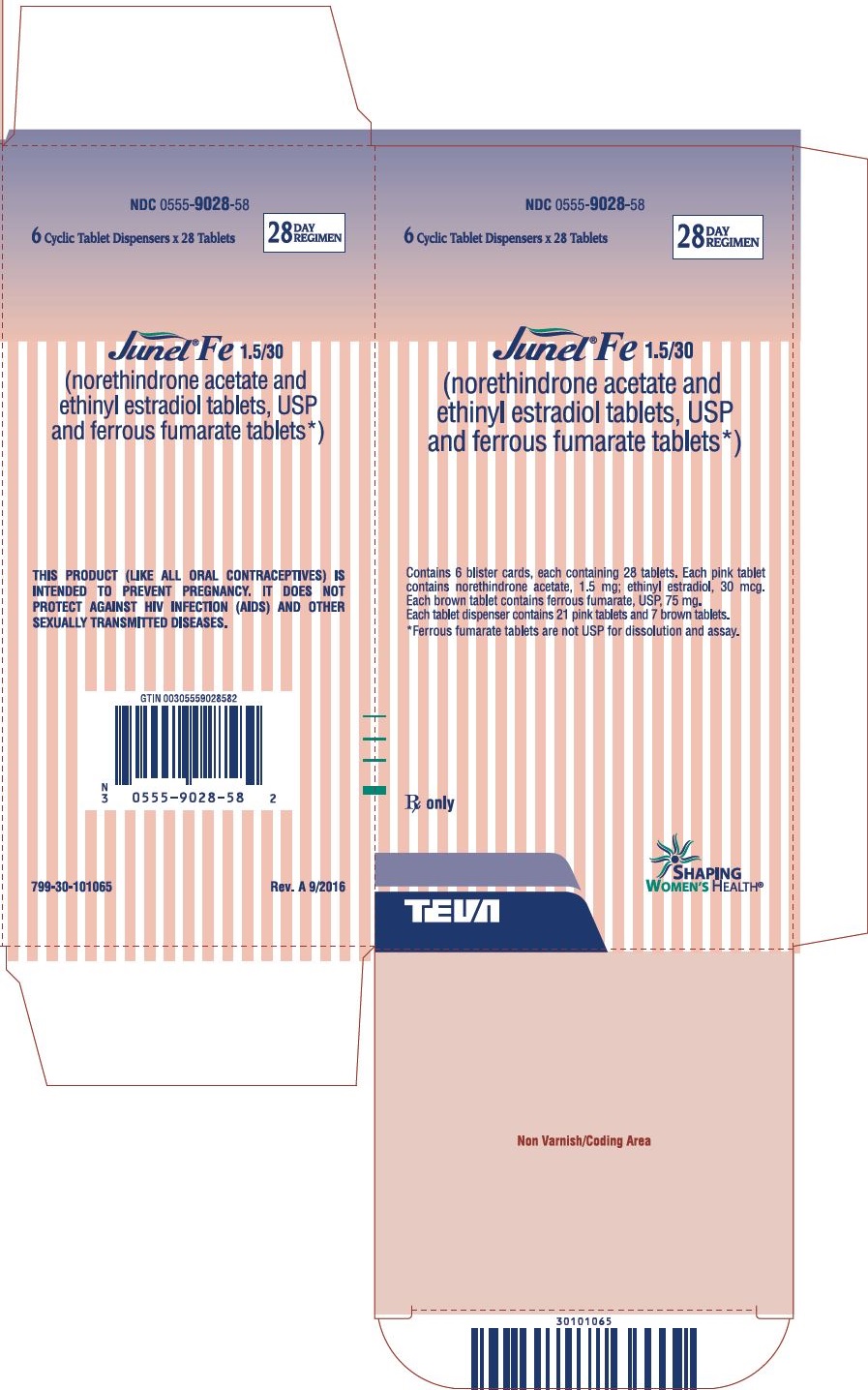
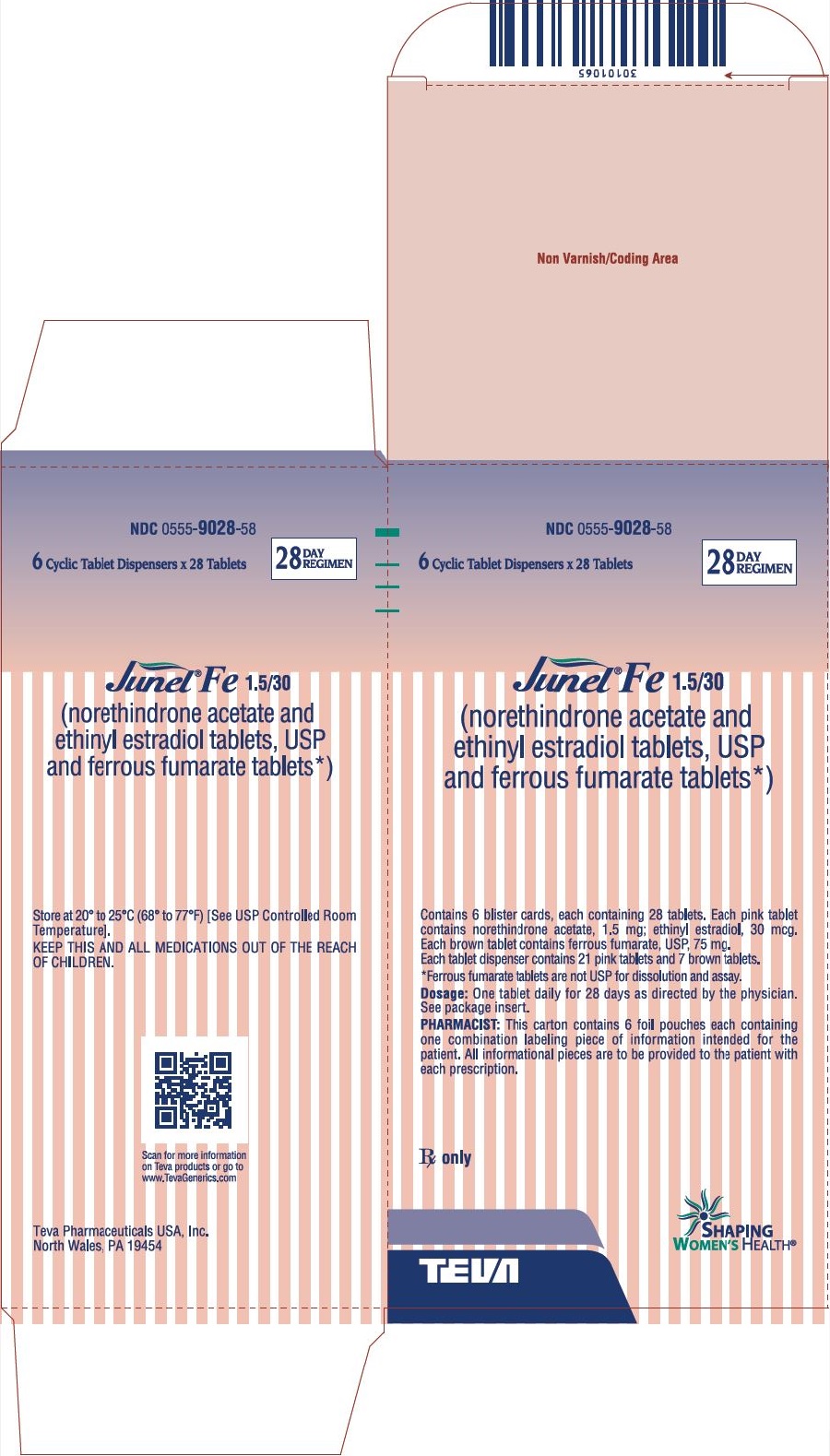
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Package/Label Display Panel
NDC 0555-9028-58
6 Cyclic Tablet Dispensers x 28 Tablets
28
DAY
REGIMEN
Junel® Fe 1.5/30
(norethindrone acetate and
ethinyl estradiol tablets, USP
and ferrous fumarate tablets*)
Contains 6 blister cards, each containing 28 tablets. Each pink tablet
contains norethindrone acetate, 1.5 mg; ethinyl estradiol, 30 mcg.
Each brown tablet contains ferrous fumarate, USP, 75 mg.
Each tablet dispenser contains 21 pink tablets and 7 brown tablets.
*Ferrous fumarate tablets are not USP for dissolution and assay.
Rx only
SHAPING
WOMEN’S HEALTH®
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
Junel21 and Junel Fe 28 are indicated for the prevention of pregnancy in women who elect to use oral contraceptives as a method of contraception.
Oral contraceptives are highly effective. Table I lists the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
TABLE I: LOWEST EXPECTED AND TYPICAL FAILURE RATES DURING THE FIRST YEAR OF CONTINUOUS USE OF A METHOD|
% Of Women Experiencing an Unintended Pregnancy in the First Year of Continuous Use | ||
|
Method |
Lowest |
Typical** |
|
(No contraception) |
(85) |
(85) |
|
Oral contraceptives |
0.1 |
3 |
|
Diaphragm with spermicidal cream or jelly |
6 |
20 |
|
Spermicides alone (foam, creams, gels, vaginal suppositories, and vaginal film) |
6 |
26 |
|
Vaginal Sponge |
9 |
20 |
|
Implant |
0.05 |
0.05 |
|
Injection: depot medroxyprogesterone acetate |
0.3 |
0.3 |
|
IUD |
1.5 |
2 |
|
Condom without spermicides |
5 |
21 |
|
Cervical Cap with spermicidal cream or jelly |
9 |
20 |
|
Periodic abstinence (all methods) |
1 to 9 |
25 |
|
Withdrawal |
4 |
19 |
|
Female sterilization |
0.5 |
0.5 |
|
Male sterilization |
0.10 |
0.15 |
|
Adapted from RA Hatcher et al, Reference 7. |
- The authors' best guess of the percentage of women expected to experience an accidental pregnancy among couples who initiate a method (not necessarily for the first time) and who use it consistently and correctly during the first year if they do not stop for any other reason.
** This term represents “typical” couples who initiate use of a method (not necessarily for the first time), who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
*** N/A-Data not available.
SPL PATIENT PACKAGE INSERT SECTION
DETAILED PATIENT PACKAGE INSERT
|
Cigarette smoking increases the risk of serious cardiovascular side effects
from oral contraceptive use. |
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against HIV infection (AIDS) and other sexually transmitted infections.
What You Should Know About Oral Contraceptives
Any woman who considers using oral contraceptives (the “birth control pill” or “the pill”) should understand the benefits and risks of using this form of birth control. This leaflet will give you much of the information you will need to make this decision and will also help you determine if you are at risk of developing any of the serious side effects of the pill. It will tell you how to use the pill properly so that it will be as effective as possible. However, this leaflet is not a replacement for a careful discussion between you and your healthcare provider. You should discuss the information provided in this leaflet with him or her, both when you first start taking the pill and during your revisits. You should also follow your healthcare provider's advice with regard to regular check-ups while you are on the pill.
EFFECTIVENESS OF ORAL CONTRACEPTIVES
Oral contraceptives or “birth control pills” or “the pill” are used to prevent pregnancy and are more effective than other non-surgical methods of birth control. When they are taken correctly, the chance of becoming pregnant is less than 1% (1 pregnancy per 100 women per year of use) when used perfectly, without missing any pills. Typical failure rates are actually 3% per year. The chance of becoming pregnant increases with each missed pill during a menstrual cycle.
In comparison, typical failure rates for other methods of birth control during the first year of use are as follows:
Implant: <1%
Injection: <1%
IUD: <1 to 2%
Diaphragm with spermicides: 20%
Spermicides alone: 26%
Vaginal Sponge: 20 to 40%
Female sterilization: <1%
Male sterilization: <1%
Cervical Cap: 20 to 40%
Condom alone (male): 14%
Condom alone (female): 21%
Periodic abstinence: 25%
Withdrawal: 19%
No method: 85%
WHO SHOULD NOT TAKE ORAL CONTRACEPTIVES
|
Cigarette smoking increases the risk of serious cardiovascular side effects
from oral contraceptive use. |
Some women should not use the pill. For example, you should not take the pill if you are pregnant or think you may be pregnant.
You should also not use the pill if you have any of the following conditions:
- A history of heart attack or stroke
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), or eyes
- A history of blood clots in the deep veins of your legs
- Chest pain (angina pectoris)
- Known or suspected breast cancer
- Unexplained vaginal bleeding (until a diagnosis is reached by your doctor)
- Yellowing of the whites of the eyes or of the skin (jaundice) during pregnancy or during previous use of the pill
- Liver tumor (benign or cancerous)
- Take any Hepatitis C drug combination containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme “alanine aminotransferase” (ALT) in the blood.
Tell your healthcare provider if you have ever had any of these conditions. Your healthcare provider can recommend a safer method of birth control.
OTHER CONSIDERATIONS BEFORE TAKING ORAL CONTRACEPTIVES
Tell your healthcare provider if you have:
- Breast nodules, fibrocystic disease of the breast, an abnormal breast x-ray or mammogram
- Diabetes
- Elevated cholesterol or triglycerides
- High blood pressure
- Migraine or other headaches or epilepsy
- Depression
- Gallbladder, heart, or kidney disease
- History of scanty or irregular menstrual periods
Women with any of these conditions should be checked often by their healthcare provider if they choose to use oral contraceptives.
Also, be sure to inform your doctor or healthcare provider if you smoke or are on any medications.
RISKS OF TAKING ORAL CONTRACEPTIVES
1.Risk of Developing Blood Clots
Blood clots and blockage of blood vessels are the most serious side effects of
taking oral contraceptives; in particular, a clot in the legs can cause
thrombophlebitis, and a clot that travels to the lungs can cause a sudden
blocking of the vessel carrying blood to the lungs. Rarely, clots occur in the
blood vessels of the eye and may cause blindness, double vision, or impaired
vision.
If you take oral contraceptives and need elective surgery, need to stay in bed
for a prolonged illness, or have recently delivered a baby, you may be at risk
of developing blood clots. You should consult your doctor about stopping oral
contraceptives three to four weeks before surgery and not taking oral
contraceptives for two weeks after surgery or during bed rest. You should also
not take oral contraceptives soon after delivery of a baby. It is advisable to
wait for at least four weeks after delivery if you are not breastfeeding. If
you are breastfeeding, you should wait until you have weaned your child before
using the pill. (See also the section on Breastfeeding in GENERAL
PRECAUTIONS.)
2.Heart Attacks and Strokes
Oral contraceptives may increase the tendency to develop strokes (stoppage or
rupture of blood vessels in the brain) and angina pectoris and heart attacks
(blockage of blood vessels in the heart). Any of these conditions can cause
death or disability.
Smoking greatly increases the possibility of suffering heart attacks and
strokes. Furthermore, smoking and the use of oral contraceptives greatly
increase the chances of developing and dying of heart disease.
3.Gallbladder Disease
Oral contraceptive users probably have a greater risk than nonusers of having
gallbladder disease, although this risk may be related to pills containing
high doses of estrogens.
4.Liver Tumors
In rare cases, oral contraceptives can cause benign but dangerous liver
tumors. These benign liver tumors can rupture and cause fatal internal
bleeding. In addition, a possible but not definite association has been found
with the pill and liver cancers in two studies, in which a few women who
developed these very rare cancers were found to have used oral contraceptives
for long periods. However, liver cancers are extremely rare. The chance of
developing liver cancer from using the pill is thus even rarer.
5.Risk of Cancer
****It is not known if hormonal birth control pills cause breast cancer. Some
studies, but not all, suggest that there could be a slight increase in the
risk of breast cancer among current users with longer duration of use.
If you have breast cancer now, or have had it in the past, do not use hormonal birth control because some breast cancers are sensitive to hormones.
Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives.
ESTIMATED RISK OF DEATH FROM A BIRTH CONTROL METHOD OR PREGNANCY
All methods of birth control and pregnancy are associated with a risk of developing certain diseases which may lead to disability or death. An estimate of the number of deaths associated with different methods of birth control and pregnancy has been calculated and is shown in the following table.
ANNUAL NUMBER OF BIRTH-RELATED OR METHOD-RELATED DEATHS ASSOCIATED WITH CONTROL OF FERTILITY PER 100,000 NONSTERILE WOMEN, BY FERTILITY CONTROL METHOD ACCORDING TO AGE|
Method of control and outcome |
15 to 19 |
20 to 24 |
25 to 29 |
30 to 34 |
35 to 39 |
40 to 44 |
|
No fertility control methods* |
7.0 |
7.4 |
9.1 |
14.8 |
25.7 |
28.2 |
|
Oral contraceptives non-smoker** |
0.3 |
0.5 |
0.9 |
1.9 |
13.8 |
31.6 |
|
Oral contraceptives smoker** |
2.2 |
3.4 |
6.6 |
13.5 |
51.1 |
117.2 |
|
IUD** |
0.8 |
0.8 |
1.0 |
1.0 |
1.4 |
1.4 |
|
Condom* |
1.1 |
1.6 |
0.7 |
0.2 |
0.3 |
0.4 |
|
Diaphragm/spermicide* |
1.9 |
1.2 |
1.2 |
1.3 |
2.2 |
2.8 |
|
Periodic abstinence* |
2.5 |
1.6 |
1.6 |
1.7 |
2.9 |
3.6 |
*Deaths are birth related.
**Deaths are method related.
In the above table, the risk of death from any birth control method is less than the risk of childbirth, except for oral contraceptive users over the age of 35 who smoke and pill users over the age of 40 even if they do not smoke. It can be seen in the table that for women aged 15 to 39, the risk of death was highest with pregnancy (7 to 26 deaths per 100,000 women, depending on age). Among pill users who do not smoke, the risk of death was always lower than that associated with pregnancy for any age group, although over the age of 40, the risk increases to 32 deaths per 100,000 women, compared to 28 associated with pregnancy at that age. However, for pill users who smoke and are over the age of 35, the estimated number of deaths exceeds those for other methods of birth control. If a woman is over the age of 40 and smokes, her estimated risk of death is four times higher (117/100,000 women) than the estimated risk associated with pregnancy (28/100,000 women) in that age group.
The suggestion that women over 40 who don't smoke should not take oral contraceptives is based on information from older higher dose pills and on less selective use of pills than is practiced today. An Advisory Committee of the FDA discussed this issue in 1989 and recommended that the benefits of oral contraceptive use by healthy, non-smoking women over 40 years of age may outweigh the possible risks. However, all women, especially older women, are cautioned to use the lowest dose pill that is effective.
WARNING SIGNALS
If any of these adverse effects occur while you are taking oral contraceptives, call your doctor immediately:
- Sharp chest pain, coughing of blood, or sudden shortness of breath (indicating a possible clot in the lung)
- Pain in the calf (indicating a possible clot in the leg)
- Crushing chest pain or heaviness in the chest (indicating a possible heart attack)
- Sudden severe headache or vomiting, dizziness or fainting, disturbances of vision or speech, weakness, or numbness in an arm or leg (indicating a possible stroke)
- Sudden partial or complete loss of vision (indicating a possible clot in the eye)
- Breast lumps (indicating possible breast cancer or fibrocystic disease of the breast; ask your doctor or healthcare provider to show you how to examine your breasts)
- Severe pain or tenderness in the stomach area (indicating a possibly ruptured liver tumor)
- Difficulty in sleeping, weakness, lack of energy, fatigue, or change in mood (possibly indicating severe depression)
- Jaundice or a yellowing of the skin or eyeballs, accompanied frequently by fever, fatigue, loss of appetite, dark colored urine, or light colored bowel movements (indicating possible liver problems)
SIDE EFFECTS OF ORAL CONTRACEPTIVES
1.Vaginal Bleeding
Irregular vaginal bleeding or spotting may occur while you are taking the
pills. Irregular bleeding may vary from slight staining between menstrual
periods to breakthrough bleeding which is a flow much like a regular period.
Irregular bleeding occurs most often during the first few months of oral
contraceptive use, but may also occur after you have been taking the pill for
some time. Such bleeding may be temporary and usually does not indicate
serious problems. It is important to continue taking your pills on schedule.
If the bleeding occurs in more than one cycle or lasts for more than a few
days, talk to your doctor or healthcare provider.
2.Contact Lenses
If you wear contact lenses and notice a change in vision or an inability to
wear your lenses, contact your doctor or healthcare provider.
3.Fluid Retention
Oral contraceptives may cause edema (fluid retention) with swelling of the
fingers or ankles and may raise your blood pressure. If you experience fluid
retention, contact your doctor or healthcare provider.
4.Melasma
A spotty darkening of the skin is possible, particularly of the face.
5.Other Side Effects
Other side effects may include change in appetite, headache, nervousness,
depression, dizziness, loss of scalp hair, rash, and vaginal infections.
If any of these side effects bother you, call your doctor or healthcare provider.
GENERAL PRECAUTIONS
1.Missed Periods and Use of Oral Contraceptives Before or During Early Pregnancy
There may be times when you may not menstruate regularly after you have
completed taking a cycle of pills. If you have taken your pills regularly and
miss one menstrual period, continue taking your pills for the next cycle but
be sure to inform your healthcare provider before doing so. If you have not
taken the pills daily as instructed and missed a menstrual period, or if you
missed two consecutive menstrual periods, you may be pregnant. Check with your
healthcare provider immediately to determine whether you are pregnant. Do not
continue to take oral contraceptives until you are sure you are not pregnant,
but continue to use another method of contraception.
There is no conclusive evidence that oral contraceptive use is associated with
an increase in birth defects, when taken inadvertently during early pregnancy.
Previously, a few studies had reported that oral contraceptives might be
associated with birth defects, but these studies have not been confirmed.
Nevertheless, oral contraceptives or any other drugs should not be used during
pregnancy unless clearly necessary and prescribed by your doctor. You should
check with your doctor about risks to your unborn child of any medication
taken during pregnancy.
2.While Breastfeeding
If you are breastfeeding, consult your doctor before starting oral
contraceptives. Some of the drug will be passed on to the child in the milk. A
few adverse effects on the child have been reported, including yellowing of
the skin (jaundice) and breast enlargement. In addition, oral contraceptives
may decrease the amount and quality of your milk. If possible, do not use oral
contraceptives while breastfeeding. You should use another method of
contraception since breastfeeding provides only partial protection from
becoming pregnant, and this partial protection decreases significantly as you
breastfeed for longer periods of time. You should consider starting oral
contraceptives only after you have weaned your child completely.
3.Laboratory Tests
If you are scheduled for any laboratory tests, tell your doctor you are taking
birth control pills. Certain blood tests may be affected by birth control
pills.
4.Drug Interactions
Certain drugs may interact with birth control pills to make them less
effective in preventing pregnancy or cause an increase in breakthrough
bleeding. Such drugs include rifampin; drugs used for epilepsy such as
barbiturates (for example, phenobarbital), carbamazepine, and phenytoin
(Dilantin® is one brand of this drug); troglitazone; phenylbutazone; and
possibly certain antibiotics. You may need to use additional contraception
when you take drugs which can make oral contraceptives less effective.
Birth control pills interact with certain drugs. These drugs include
acetaminophen, clofibric acid, cyclosporine, morphine, prednisolone, salicylic
acid, temazepam, and theophylline. You should tell your doctor if you are
taking any of these medications.
5.This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted infections such as Chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
INSTRUCTIONS TO PATIENT
TABLET DISPENSER
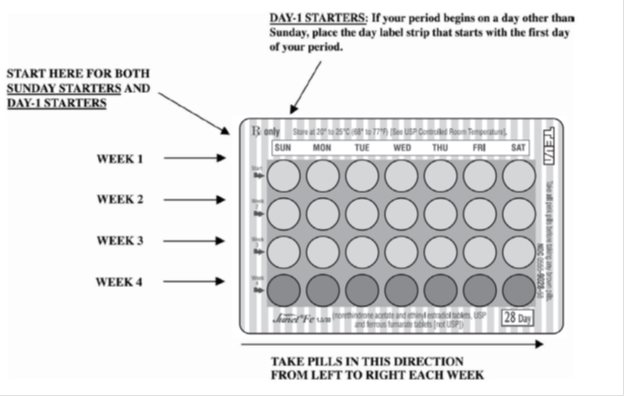
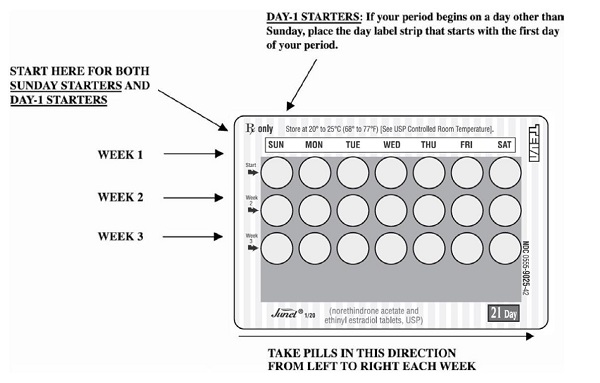
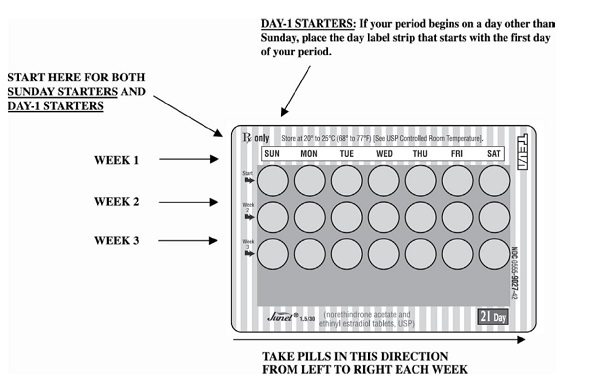
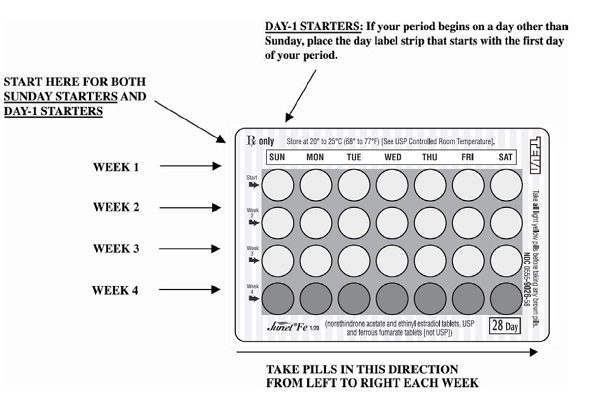
The Junel tablet dispenser has been designed to make oral contraceptive dosing as easy and as convenient as possible. The tablets are arranged in either three or four rows of seven tablets each, with the days of the week appearing above the first row of tablets.
|
If your TABLET DISPENSER contains: |
You are taking: |
|
21 light yellow tablets |
Junel 21 1/20 |
|
21 pink tablets |
Junel 21 1.5/30 |
|
21 light yellow tablets and |
Junel Fe 1/20 |
|
21 pink tablets and |
Junel Fe 1.5/30 |
Each light yellow tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol.
Each pink tablet contains 1.5 mg norethindrone acetate and 30 mcg ethinyl estradiol.
Each brown tablet contains 75 mg ferrous fumarate, and is intended to help you remember to take the tablets correctly. These brown tablets are not intended to have any health benefit.
DIRECTIONS
To remove a tablet, press down on it with your thumb or finger. The tablet will drop through the back of the tablet dispenser. Do not press with your thumbnail, fingernail, or any other sharp object.
HOW TO TAKE THE PILL
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING YOUR PILLS:
-
BE SURE TO READ THESE DIRECTIONS:
Before you start taking your pills.
Anytime you are not sure what to do. -
THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME. If you miss pills you could get pregnant.
This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant. -
MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH DURING THE FIRST 1 to 3 PACKS OF PILLS. If you do have spotting or light bleeding or feel sick to your stomach, do not stop taking the pill. The problem will usually go away. If it doesn't go away, check with your doctor or clinic.
-
MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills. On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
-
IF YOU HAVE VOMITING OR DIARRHEA, for any reason, or IF YOU TAKE SOME MEDICINES, including some antibiotics, your birth control pills may not work as well. Use a back-up birth control method (such as condoms or foam) until you check with your doctor or clinic.
-
IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your doctor or clinic about how to make pill-taking easier or about using another method of birth control.
-
IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your doctor or clinic.
BEFORE** YOU START TAKING YOUR PILLS**
-
DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
-
LOOK AT YOUR PILL PACK TO SEE IF IT HAS 21 OR 28 PILLS:
The 21-Day pill pack has 21 “active” light yellow or pink pills (with hormones) to take for 3 weeks, followed by 1 week without pills.
The 28-Day pill pack has 21 “active” light yellow or pink pills (with hormones) to take for 3 weeks, followed by 1 week of reminder brown pills (without hormones). -
ALSO FIND:
- where on the pack to start taking pills,
- in what order to take the pills.
- the week numbers as shown in the following pictures:
Junel 21 1/20 will contain:ALL LIGHT YELLOW PILLS
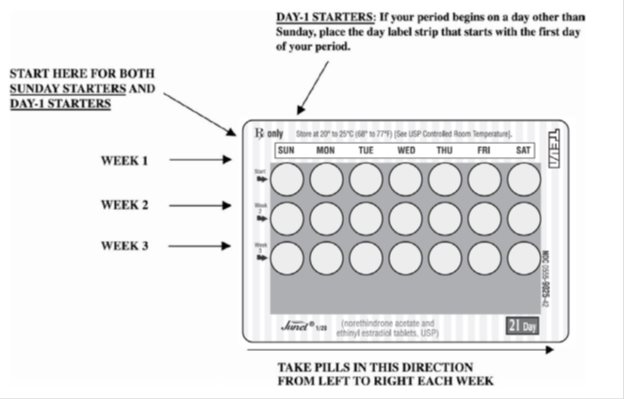
Junel 21 1.5/30 will contain:ALL PINK PILLS
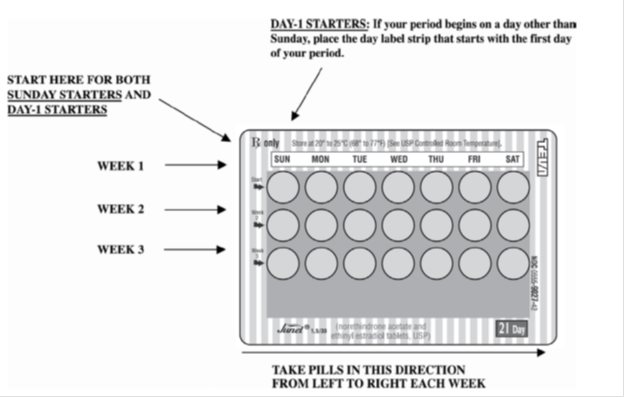
Junel Fe 1/20 will contain:21 LIGHT YELLOW PILLS forWEEKS 1, 2, and 3.WEEK 4 will containBROWN PILLS ONLY
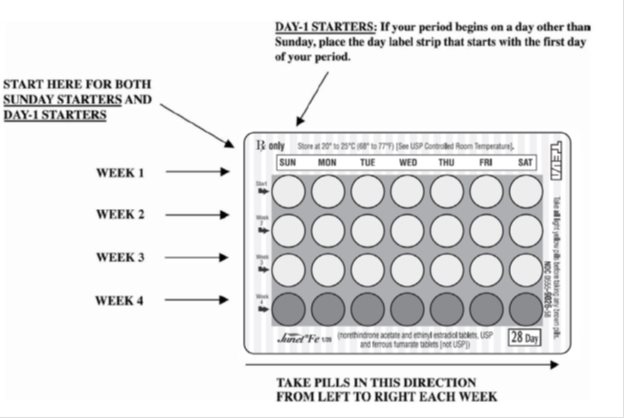
Junel Fe 1.5/30 will contain:21 PINK PILLS forWEEKS 1, 2, and 3. WEEK 4 will containBROWN PILLS ONLY.
4. BE SURE YOU HAVE READY AT ALL TIMES:
ANOTHER KIND OF BIRTH CONTROL (such as condoms or foam) to use as a back-up in
case you miss pills.
An EXTRA, FULL PILL PACK.
WHEN TO START THEFIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills. Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
DAY-1 START:
- Pick the day label strip that starts with the first day of your period. (This is the day you start bleeding or spotting, even if it is almost midnight when the bleeding begins.)
- Place this day label strip on the tablet dispenser over the area that has the days of the week (starting with Sunday) printed on the plastic.
- Take the first “active” light yellow or pink pill of the first pack during the first 24 hours of your period.
- You will not need to use a back-up method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY-START:
- Take the first “active” light yellow or pink pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
- Use another method of birth control as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days). Condoms or foam are good back-up methods of birth control.
WHAT TO DO DURING THE MONTH
1.TAKE ONE PILL AT THE SAME TIME EVERY DAY UNTIL THE PACK IS EMPTY.
Do not skip pills even if you are spotting or bleeding between monthly periods
or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2.WHEN YOU FINISH A PACK OR SWITCH YOUR BRAND OF PILLS:
**21 pills:**Wait 7 days to start the next pack. You will probably have your
period during that week. Be sure that no more than 7 days pass between 21-day
packs.
**28 pills:**Start the next pack on the day after your last “reminder” pill.
Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
If youMISS 1light yellow or pink “active” pill:
- Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
- You do not need to use a back-up birth control method if you have sex.
If youMISS 2light yellow or pink “active” pills in a row inWEEK 1 OR WEEK 2of your pack:
- Take 2 pills on the day you remember and 2 pills the next day.
- Then take 1 pill a day until you finish the pack.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
If youMISS 2light yellow or pink “active” pills in a row inTHE 3rd WEEK:
1.If you are a Day 1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest of
the pack and start a new pack of pills that same day.
- You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
If youMISS 3 OR MORElight yellow or pink “active” pills in a row (during the first 3 weeks):
1.If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest of
the pack and start a new pack of pills that same day.
- You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
A REMINDER FOR THOSE ON 28-DAY PACKS
IF YOU FORGET ANY OF THE 7 BROWN “REMINDER” PILLS IN WEEK 4:
THROW AWAY THE PILLS YOU MISSED.
KEEP TAKING 1 PILL EACH DAY UNTIL THE PACK IS EMPTY.
YOU DO NOT NEED A BACK-UP METHOD.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED:
Use a BACK-UP METHOD anytime you have sex.
KEEP TAKING ONE LIGHT YELLOW OR PINK “ACTIVE” PILL EACH DAY until you can reach your doctor or clinic.
PREGNANCY DUE TO PILL FAILURE
The incidence of pill failure resulting in pregnancy is approximately 1% (i.e., one pregnancy per 100 women per year) if taken every day as directed, but more typical failure rates are about 3%. If failure does occur, the risk to the fetus is minimal.
PREGNANCY AFTER STOPPING THE PILL
There may be some delay in becoming pregnant after you stop using oral contraceptives, especially if you had irregular menstrual cycles before you used oral contraceptives. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped taking the pill and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the pill.
OVERDOSAGE
Serious ill effects have not been reported following ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea and withdrawal bleeding in females. In case of overdosage, contact your healthcare provider or pharmacist.
OTHER INFORMATION
Your healthcare provider will take a medical and family history and examine you before prescribing oral contraceptives. The physical examination may be delayed to another time if you request it and your healthcare provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year. Be sure to inform your healthcare provider if there is a family history of any of the conditions listed previously in this leaflet. Be sure to keep all appointments with your healthcare provider, because this is a time to determine if there are early signs of side effects of oral contraceptive use.
Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who may want birth control pills.
HEALTH BENEFITS FROM ORAL CONTRACEPTIVES
In addition to preventing pregnancy, use of oral contraceptives may provide certain benefits. They are:
- Menstrual cycles may become more regular
- Blood flow during menstruation may be lighter and less iron may be lost. Therefore, anemia due to iron deficiency is less likely to occur
- Pain or other symptoms during menstruation may be encountered less frequently
- Ectopic (tubal) pregnancy may occur less frequently
- Noncancerous cysts or lumps in the breast may occur less frequently
- Acute pelvic inflammatory disease may occur less frequently
- Oral contraceptive use may provide some protection against developing two forms of cancer: cancer of the ovaries and cancer of the lining of the uterus.
If you want more information about birth control pills, ask your doctor or pharmacist. They have a more technical leaflet called the “Physician Insert”, which you may wish to read.
Remembering to take tablets according to schedule is stressed because of its importance in providing you the greatest degree of protection.
MISSED MENSTRUAL PERIODS FOR BOTH DOSAGE REGIMENS
At times there may be no menstrual period after a cycle of pills. Therefore, if you miss one menstrual period but have taken the pills exactly as you were supposed to, continue as usual into the next cycle. If you have not taken the pills correctly and miss a menstrual period, you may be pregnant and should stop taking oral contraceptives until your doctor or healthcare provider determines whether or not you are pregnant. Until you can get to your doctor or healthcare provider, use another form of contraception. If two consecutive menstrual periods are missed, you should stop taking pills until it is determined whether or not you are pregnant. Although there does not appear to be any increase in birth defects in newborn babies if you become pregnant while using oral contraceptives, you should discuss the situation with your doctor or healthcare provider.
Periodic Examination
Your doctor or healthcare provider will take a complete medical and family history before prescribing oral contraceptives. At that time and about once a year thereafter, he or she will generally examine your blood pressure, breasts, abdomen, and pelvic organs (including a Papanicolaou smear, i.e., test for cancer).
Keep this and all drugs out of the reach of children.
Rx only
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Brands listed are the trademarks of their respective owners.
Teva Pharmaceuticals USA, Inc.
North Wales, PA 19454
Rev. D 8/2023
To report SUSPECTED ADVERSE REACTIONS, contact Teva at 1-888-838-2872 or FDA at 1800-FDA-1088 or www.fda.gov/medwatch.
PRECAUTIONS SECTION
PRECAUTIONS
1. Patients should be counseled that this product does not protect against
HIV infection (AIDS) and other sexually transmitted infections.
2. Physical Examination and Follow-Up
It is good medical practice for all women to have annual history and physical examinations, including women using oral contraceptives. The physical examination, however, may be deferred until after initiation of oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology, and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
3. Lipid Disorders
Women who are being treated for hyperlipidemia should be followed closely if they elect to use oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult.
4. Liver Function
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
5. Fluid Retention
Oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
6. Contact Lenses
Contact lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
7. Drug Interactions
Effects of Other Drugs on Oral Contraceptives (69)
Rifampin: Metabolism of both norethindrone and ethinyl estradiol is increased by rifampin. A reduction in contraceptive effectiveness and increased incidence of breakthrough bleeding and menstrual irregularities have been associated with concomitant use of rifampin.
Anticonvulsants: Anticonvulsants such as phenobarbital, phenytoin, and carbamazepine, have been shown to increase the metabolism of ethinyl estradiol and/or norethindrone, which could result in a reduction in contraceptive effectiveness.
Troglitazone: Administration of troglitazone with an oral contraceptive containing ethinyl estradiol and norethindrone reduced the plasma concentrations of both by approximately 30%, which could result in a reduction in contraceptive effectiveness.
Antibiotics: Pregnancy while taking oral contraceptives has been reported when the oral contraceptives were administered with antimicrobials such as ampicillin, tetracycline, and griseofulvin. However, clinical pharmacokinetic studies have not demonstrated any consistent effect of antibiotics (other than rifampin) on plasma concentrations of synthetic steroids.
Atorvastatin: Coadministratrion of atorvastatin and an oral contraceptive increased AUC values for norethindrone and ethinyl estradiol by approximately 30% and 20%, respectively.
Concomitant Use with HCV Combination Therapy**– Liver Enzyme Elevation**
****Coadministration of Junel with HCV drug combinations containing
ombitasvir/paritaprevir/ritonavir, with or without dasabuvir is
contraindicated due to potential for ALT elevations (see Warnings,RISK OF
LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT).
Coadministration of Junel and glecaprevir/pibrentasvir is not recommended due
to potential for ALT elevations.
Other: Ascorbic acid and acetaminophen may increase plasma ethinyl estradiol concentrations, possibly by inhibition of conjugation. A reduction in contraceptive effectiveness and increased incidence of breakthrough bleeding has been suggested with phenylbutazone.
Effects of Oral Contraceptives on Other Drugs
Oral contraceptive combinations containing ethinyl estradiol may inhibit the metabolism of other compounds. Increased plasma concentrations of cyclosporine, prednisolone, and theophylline have been reported with concomitant administration of oral contraceptives. In addition, oral contraceptives may induce the conjugation of other compounds. Decreased plasma concentrations of acetaminophen and increased clearance of temazepam, salicylic acid, morphine, and clofibric acid have been noted when these drugs were administered with oral contraceptives.
8. Interactions With Laboratory Tests
Certain endocrine and liver function tests and blood components may be affected by oral contraceptives:
- Increased prothrombin and factors VII, VIII, IX, and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability.
- Increased thyroid binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG; free T4 concentration is unaltered.
- Other binding proteins may be elevated in serum.
- Sex-binding globulins are increased and result in elevated levels of total circulating sex steroids and corticoids; however, free or biologically active levels remain unchanged.
- Triglycerides may be increased.
- Glucose tolerance may be decreased.
- Serum folate levels may be depressed by oral contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.
9. Carcinogenesis
SeeWARNINGS section.
10. Pregnancy
Discontinue Junel if pregnancy occurs because there is no reason to use COCs in pregnancy. SeeWARNINGS section.
11. Lactation
Small amounts of oral contraceptive steroids have been identified in human milk, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use oral contraceptives but to use other forms of contraception until she has completely weaned her child.
12. Pediatric Use
Safety and efficacy of Junel have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and for users 16 years and older. Use of this product before menarche is not indicated.
SPL UNCLASSIFIED SECTION
BRIEF SUMMARY PATIENT PACKAGE INSERT
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against HIV infection (AIDS) and other sexually transmitted infections.
Oral contraceptives, also known as “birth control pills” or “the pill,” are taken to prevent pregnancy and, when taken correctly, have a failure rate of about 1% per year when used without missing any pills. The typical failure rate of large numbers of pill users is less than 3% per year when women who miss pills are included. For most women, oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
For the majority of women, oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be life-threatening or may cause temporary or permanent disability. The risks associated with taking oral contraceptives increase significantly if you:
- Smoke
- Have high blood pressure, diabetes, high cholesterol
- Have or have had clotting disorders, heart attack, stroke, angina pectoris, cancer of the breast, jaundice, or malignant or benign liver tumors.
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
|
Cigarette smoking increases the risk of serious cardiovascular side effects
from oral contraceptive use. |
Most side effects of the pill are not serious. The most common side effects are nausea, vomiting, bleeding between menstrual periods, weight gain, breast tenderness, and difficulty wearing contact lenses. These side effects, especially nausea, vomiting, and breakthrough bleeding may subside within the first three months of use.
The serious side effects of the pill occur very infrequently, especially if you are in good health and are young. However, you should know that the following medical conditions have been associated with or made worse by the pill:
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), stoppage or rupture of a blood vessel in the brain (stroke), blockage of blood vessels in the heart (heart attack or angina pectoris) or other organs of the body. As mentioned above, smoking increases the risk of heart attacks and strokes and subsequent serious medical consequences.
- Liver tumors, which may rupture and cause severe bleeding. A possible but not definite association has been found with the pill and liver cancer. However, liver cancers are extremely rare. The chance of developing liver cancer from using the pill is thus even rarer.
- High blood pressure, although blood pressure usually returns to normal when the pill is stopped.
The symptoms associated with these serious side effects are discussed in the detailed leaflet given to you with your supply of pills. Notify your doctor or healthcare provider if you notice any unusual physical disturbances while taking the pill. In addition, drugs such as rifampin, as well as some anticonvulsants and some antibiotics, may decrease oral contraceptive effectiveness.
There may be slight increases in the risk of breast cancer among current users of hormonal birth control pills with longer duration of use of 8 years or more. Some studies have found an increase in the risk of developing cancer of the cervix in women taking the pill, but this finding may be related to differences in sexual behavior or other factors not related to use of the pill.
Taking the pill provides some important non-contraceptive benefits. These include less painful menstruation, less menstrual blood loss and anemia, fewer pelvic infections, and fewer cancers of the ovary and the lining of the uterus.
Be sure to discuss any medical condition you may have with your healthcare provider. Your healthcare provider will take a medical and family history and examine you before prescribing oral contraceptives. The physical examination may be delayed to another time if you request it and your healthcare provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year while taking oral contraceptives. The detailed patient information leaflet gives you further information which you should read and discuss with your healthcare provider.
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted infections such as Chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B and syphilis.
INSTRUCTIONS TO PATIENT
TABLET DISPENSER
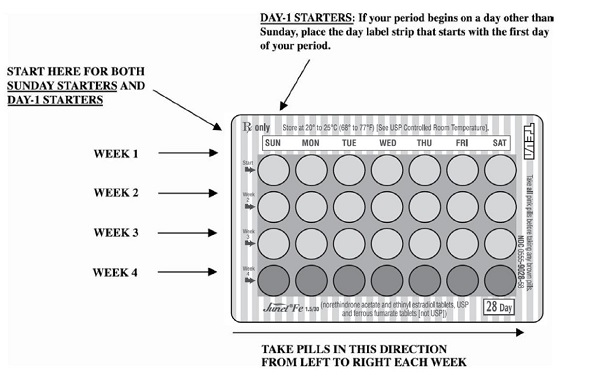
The Junel tablet dispenser has been designed to make oral contraceptive dosing as easy and as convenient as possible. The tablets are arranged in either three or four rows of seven tablets each, with the days of the week appearing above the first row of tablets.
|
If your TABLET DISPENSER contains: |
You are taking: |
|
21 light yellow tablets |
Junel 21 1/20 |
|
21 pink tablets |
Junel 21 1.5/30 |
|
21 light yellow tablets and |
Junel Fe 1/20 |
|
21 pink tablets and |
Junel Fe 1.5/30 |
Each light yellow tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol.
Each pink tablet contains 1.5 mg norethindrone acetate and 30 mcg ethinyl estradiol.
Each brown tablet contains 75 mg ferrous fumarate, and is intended to help you remember to take the tablets correctly. These brown tablets are not intended to have any health benefit.
DIRECTIONS
****To remove a tablet, press down on it with your thumb or finger. The
tablet will drop through the back of the tablet dispenser. Do not press with
your thumbnail, fingernail, or any other sharp object.
HOW TO TAKE THE PILL
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING YOUR PILLS:
-
BE SURE TO READ THESE DIRECTIONS:
Before you start taking your pills.
Anytime you are not sure what to do. -
THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME. If you miss pills you could get pregnant.
This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant. -
MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH DURING THE FIRST 1 to 3 PACKS OF PILLS. If you do have spotting or light bleeding or feel sick to your stomach, do not stop taking the pill. The problem will usually go away. If it doesn't go away, check with your doctor or clinic.
-
MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills. On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
-
IF YOU HAVE VOMITING OR DIARRHEA, for any reason, or IF YOU TAKE SOME MEDICINES, including some antibiotics, your birth control pills may not work as well. Use a back-up birth control method (such as condoms or foam) until you check with your doctor or clinic.
-
IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your doctor or clinic about how to make pill-taking easier or about using another method of birth control.
-
IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your doctor or clinic.
BEFORE** YOU START TAKING YOUR PILLS**
-
DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
-
LOOK AT YOUR PILL PACK TO SEE IF IT HAS 21 OR 28 PILLS:
The 21-Day pill pack has 21 “active” light yellow or pink pills (with hormones) to take for 3 weeks, followed by 1 week without pills.
The 28-Day pill pack has 21 “active” light yellow or pink pills (with hormones) to take for 3 weeks, followed by 1 week of reminder brown pills (without hormones). -
ALSO FIND:
- where on the pack to start taking pills,
- in what order to take the pills (follow the arrows), and
- the week numbers as shown in the following pictures:
Junel 21 1/20 will contain:ALL LIGHT YELLOW PILLS
 ****
****
Junel 21 1.5/30 will contain:ALL PINK PILLS
Junel Fe 1/20 will contain: 21 LIGHT YELLOW PILLS for WEEKS 1, 2, and 3. WEEK 4 will contain BROWN PILLS ONLY.
 ****
****
Junel Fe 1.5/30 will contain: 21 PINK PILLS for WEEKS 1, 2, and 3. WEEK 4 will contain BROWN PILLS ONLY.
4. BE SURE YOU HAVE READY AT ALL TIMES:
ANOTHER KIND OF BIRTH CONTROL (such as condoms or foam) to use as a back-up in
case you miss pills.
An EXTRA, FULL PILL PACK.
WHEN TO START THEFIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills. Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
DAY-1 START:
- Pick the day label strip that starts with the first day of your period. (This is the day you start bleeding or spotting, even if it is almost midnight when the bleeding begins.)
- Place this day label strip on the tablet dispenser over the area that has the days of the week (starting with Sunday) printed on the plastic.
- Take the first “active” light yellow or pink pill of the first pack during the first 24 hours of your period.
- You will not need to use a back-up method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY START:
- Take the first “active” light yellow or pink pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
- Use another method of birth control as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days). Condoms or foam are good back-up methods of birth control.
WHAT TO DO DURING THE MONTH
1.TAKE ONE PILL AT THE SAME TIME EVERY DAY UNTIL THE PACK IS EMPTY.
Do not skip pills even if you are spotting or bleeding between monthly periods
or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2.WHEN YOU FINISH A PACK OR SWITCH YOUR BRAND OF PILLS:
**21 pills:**Wait 7 days to start the next pack. You will probably have your
period during that week. Be sure that no more than 7 days pass between 21-day
packs.
**28 pills:**Start the next pack on the day after your last “reminder” pill.
Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
If youMISS 1 light yellow or pink “active” pill:
- Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
- You do not need to use a back-up birth control method if you have sex.
If youMISS 2 light yellow or pink “active” pills in a row inWEEK 1 OR WEEK 2 of your pack:
- Take 2 pills on the day you remember and 2 pills the next day.
- Then take 1 pill a day until you finish the pack.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
If youMISS 2 light yellow or pink “active” pills in a row inTHE 3rd WEEK:
1.If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter**:**
Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest of
the pack and start a new pack of pills that same day.
- You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
If youMISS 3 OR MORE light yellow or pink “active” pills in a row (during the first 3 weeks):
1.If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
****Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest
of the pack and start a new pack of pills that same day.
- You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or foam) as a back-up method of birth control until you have taken a light yellow or pink “active” pill every day for 7 days.
|
A REMINDER FOR THOSE ON 28-DAY PACKS |
|
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE
MISSED: |
Based on his or her assessment of your medical needs, your doctor or healthcare provider has prescribed this drug for you. Do not give this drug to anyone else.
Keep this and all drugs out of the reach of children.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Teva Pharmaceuticals USA, Inc.
****North Wales, PA 19454
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
Combination oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
Pharmacokinetics
The pharmacokinetics of Junel have not been characterized; however, the following pharmacokinetic information regarding norethindrone acetate and ethinyl estradiol is taken from the literature.
Absorption
Norethindrone acetate appears to be completely and rapidly deacetylated to norethindrone after oral administration, since the disposition of norethindrone acetate is indistinguishable from that of orally administered norethindrone (1). Norethindrone acetate and ethinyl estradiol are subject to first-pass metabolism after oral dosing, resulting in an absolute bioavailability of approximately 64% for norethindrone and 43% for ethinyl estradiol (1-3).
Distribution
Volume of distribution of norethindrone and ethinyl estradiol ranges from 2 to 4 L/kg (1 to 3). Plasma protein binding of both steroids is extensive (greater than 95%); norethindrone binds to both albumin and sex hormone binding globulin, whereas ethinyl estradiol binds only to albumin (4).
Metabolism
Norethindrone undergoes extensive biotransformation, primarily via reduction, followed by sulfate and glucuronide conjugation. The majority of metabolites in the circulation are sulfates, with glucuronides accounting for most of the urinary metabolites (5). A small amount of norethindrone acetate is metabolically converted to ethinyl estradiol. Ethinyl estradiol is also extensively metabolized, both by oxidation and by conjugation with sulfate and glucuronide. Sulfates are the major circulating conjugates of ethinyl estradiol and glucuronides predominate in urine.
The primary oxidative metabolite is 2-hydroxy ethinyl estradiol, formed by the CYP3A4 isoform of cytochrome P450. Part of the first-pass metabolism of ethinyl estradiol is believed to occur in gastrointestinal mucosa. Ethinyl estradiol may undergo enterohepatic circulation (6).
Excretion
Norethindrone and ethinyl estradiol are excreted in both urine and feces, primarily as metabolites (5, 6). Plasma clearance values for norethindrone and ethinyl estradiol are similar (approximately 0.4 L/hr/kg) (1-3).
Special Population
Race:
The effect of race on the disposition of Junel has not been evaluated.
Renal Insufficiency
The effect of renal disease on the disposition of Junel has not been evaluated. In premenopausal women with chronic renal failure undergoing peritoneal dialysis who received multiple doses of an oral contraceptive containing ethinyl estradiol and norethindrone, plasma ethinyl estradiol concentrations were higher and norethindrone concentrations were unchanged compared to concentrations in premenopausal women with normal renal function.
Hepatic Insufficiency
The effect of hepatic disease on the disposition of Junel has not been evaluated. However, ethinyl estradiol and norethindrone may be poorly metabolized in patients with impaired liver function.
Drug-Drug Interactions
Numerous drug-drug interactions have been reported for oral contraceptives. A summary of these is found under PRECAUTIONS, Drug Interactions.
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
The tablet dispenser has been designed to make oral contraceptive dosing as easy and as convenient as possible. The tablets are arranged in either three or four rows of seven tablets each, with the days of the week appearing on the tablet dispenser above the first row of tablets.
**Note:**Each tablet dispenser has been preprinted with the days of the week, starting with Sunday, to facilitate a Sunday-Start regimen. Six different day label strips have been provided with the Detailed Patient & Brief Summary Patient Package Insert in order to accommodate a Day-1 Start regimen. If the patient is using the Day-1 Start regimen, she should place the self-adhesive day label strip that corresponds to her starting day over the preprinted days.
Important: The patient should be instructed to use an additional method of protection until after the first week of administration in the initial cycle when utilizing the Sunday-Start regimen.
The possibility of ovulation and conception prior to initiation of use should be considered.
Dosage and Administration for 21-Day Dosage Regimen
To achieve maximum contraceptive effectiveness, Junel21must be taken exactly as directed and at intervals not exceeding 24 hours. Junel** 21 **provides the patient with a convenient tablet schedule of “3 weeks on --1 week off”. Two dosage regimens are described, one of which may be more convenient or suitable than the other for an individual patient. For the initial cycle of therapy, the patient begins her tablets according to the Day-1 Start or Sunday-Start regimen. With either regimen, the patient takes one tablet daily for 21 consecutive days followed by one week of no tablets.
1.Sunday-Start Regimen: The patient begins taking tablets from the top row on the first Sunday after menstrual flow begins. When menstrual flow begins on Sunday, the first tablet is taken on the same day. The last tablet in the dispenser will then be taken on a Saturday, followed by no tablets for a week (7 days). For all subsequent cycles, the patient then begins a new 21-tablet regimen on the eighth day, Sunday, after taking her last tablet. Following this regimen, of 21 days on--7 days off, the patient will start all subsequent cycles on a Sunday. 2.Day-1 Regimen: The first day of menstrual flow is Day 1. The patient places the self-adhesive day label strip that corresponds to her starting day over the preprinted days on the tablet dispenser. She starts taking one tablet daily, beginning with the first tablet in the top row. The patient completes her 21-tablet regimen when she has taken the last tablet in the tablet dispenser. She will then take no tablets for a week (7 days). For all subsequent cycles, the patient begins a new 21-tablet regimen on the eighth day after taking her last tablet, again starting with the first tablet in the top row after placing the appropriate day label strip over the preprinted days on the tablet dispenser. Following this regimen of 21 days on - 7 days off, the patient will start all subsequent cycles on the same day of the week as the first course. Likewise, the interval of no tablets will always start on the same day of the week.
Tablets should be taken regularly with a meal or at bedtime. It should be stressed that efficacy of medication depends on strict adherence to the dosage schedule.
Special Notes on Administration
Menstruation usually begins two or three days, but may begin as late as the fourth or fifth day, after discontinuing medication. If spotting occurs while on the usual regimen of one tablet daily, the patient should continue medication without interruption.
If the patient forgets to take one or more tablets, the following is suggested:
One tablet is missed
- take tablet as soon as remembered
- take next tablet at the regular time
Two consecutive tablets are missed (week 1 or week 2)
- take two tablets as soon as remembered
- take two tablets the next day
- use another birth control method for seven days following the missed tablets
Two consecutive tablets are missed (week 3)
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
Three(or more) consecutive tablets are missed
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
The possibility of ovulation occurring increases with each successive day that scheduled tablets are missed. While there is little likelihood of ovulation occurring if only one tablet is missed, the possibility of spotting or bleeding is increased. This is particularly likely to occur if two or more consecutive tablets are missed.
In the rare case of bleeding which resembles menstruation, the patient should be advised to discontinue medication and then begin taking tablets from a new tablet dispenser on the next Sunday or the first day (Day 1), depending on her regimen. Persistent bleeding which is not controlled by this method indicates the need for reexamination of the patient, at which time nonfunctional causes should be considered.
Dosage and Administration for 28-Day Dosage Regimen
To achieve maximum contraceptive effectiveness, Junel** Fe**should be taken exactly as directed and at intervals not exceeding 24 hours.
Junel** Fe**provides a continuous administration regimen consisting of 21 light yellow or pink tablets of Junel and 7 brown non-hormone containing tablets of ferrous fumarate. The ferrous fumarate tablets are present to facilitate ease of drug administration via a 28-day regimen and do not serve any therapeutic purpose. There is no need for the patient to count days between cycles because there are no “off-tablet days.”
1.**Sunday-Start Regimen:**The patient begins taking the first light yellow or pink tablet from the top row of the dispenser (labeled Sunday) on the first Sunday after menstrual flow begins. When the menstrual flow begins on Sunday, the first light yellow or pink tablet is taken on the same day. The patient takes one light yellow or pink tablet daily for 21 days. The last light yellow or pink tablet in the dispenser will be taken on a Saturday. Upon completion of all 21 light yellow or pink tablets, and without interruption, the patient takes one brown tablet daily for 7 days. Upon completion of this first course of tablets, the patient begins a second course of 28-day tablets, without interruption, the next day (Sunday), starting with the Sunday light yellow or pink tablet in the top row. Adhering to this regimen of one light yellow or pink tablet daily for 21 days, followed without interruption by one brown tablet daily for seven days, the patient will start all subsequent cycles on a Sunday.
2.Day-1 Start Regimen: The first day of menstrual flow is Day 1. The patient places the self-adhesive day label strip that corresponds to her starting day over the preprinted days on the tablet dispenser. She starts taking one light yellow or pink tablet daily, beginning with the first light yellow or pink tablet in the top row. After the last light yellow or pink tablet (at the end of the third row) has been taken, the patient will then take the brown tablets for a week (7 days). For all subsequent cycles, the patient begins a new 28 tablet regimen on the eighth day after taking her last light yellow or pink tablet, again starting with the first tablet in the top row after placing the appropriate day label strip over the preprinted days on the tablet dispenser. Following this regimen of 21 light yellow or pink tablets and 7 brown tablets, the patient will start all subsequent cycles on the same day of the week as the first course.
Tablets should be taken regularly with a meal or at bedtime. It should be stressed that efficacy of medication depends on strict adherence to the dosage schedule.
Special Notes on Administration
Menstruation usually begins two or three days, but may begin as late as the fourth or fifth day, after the brown tablets have been started. In any event, the next course of tablets should be started without interruption. If spotting occurs while the patient is taking light yellow or pink tablets, continue medication without interruption.
If the patient forgets to take one or more light yellow or pink tablets, the following is suggested:
One tablet is missed
- take tablet as soon as remembered
- take next tablet at the regular time
Two consecutive tablets are missed (week 1 or week 2)
- take two tablets as soon as remembered
- take two tablets the next day
- use another birth control method for seven days following the missed tablets
Two consecutive tablets are missed (week 3)
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
Three(or more) consecutive tablets are missed
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
The possibility of ovulation occurring increases with each successive day that scheduled light yellow or pink tablets are missed. While there is little likelihood of ovulation occurring if only one light yellow or pink tablet is missed, the possibility of spotting or bleeding is increased. This is particularly likely to occur if two or more consecutive light yellow or pink tablets are missed.
If the patient forgets to take any of the seven brown tablets in week four, those brown tablets that were missed are discarded and one brown tablet is taken each day until the pack is empty. A back-up birth control method is not required during this time. A new pack of tablets should be started no later than the eighth day after the last light yellow or pink tablet was taken.
In the rare case of bleeding which resembles menstruation, the patient should be advised to discontinue medication and then begin taking tablets from a new tablet dispenser on the next Sunday or the first day (Day-1), depending on her regimen. Persistent bleeding which is not controlled by this method indicates the need for reexamination of the patient, at which time nonfunctional causes should be considered.
Use of Oral Contraceptives in the Event of a Missed Menstrual Period
- If the patient has not adhered to the prescribed dosage regimen, the possibility of pregnancy should be considered after the first missed period and oral contraceptives should be withheld until pregnancy has been ruled out.
- If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing the contraceptive regimen.
After several months on treatment, bleeding may be reduced to a point of virtual absence. This reduced flow may occur as a result of medication, in which event it is not indicative of pregnancy.
