Manufacturing Establishments2
FDA-registered manufacturing facilities and establishments involved in the production, packaging, or distribution of this drug product.
Baxter Healthcare Corporation
750455891
Baxter Healthcare Corporation
194684502
Products4
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
HEPARIN SODIUM IN SODIUM CHLORIDE
Product Details
HEPARIN SODIUM IN SODIUM CHLORIDE
Product Details
HEPARIN SODIUM IN SODIUM CHLORIDE
Product Details
HEPARIN SODIUM IN SODIUM CHLORIDE
Product Details
Drug Labeling Information
Complete FDA-approved labeling information including indications, dosage, warnings, contraindications, and other essential prescribing details.
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
Container Label
Container Label
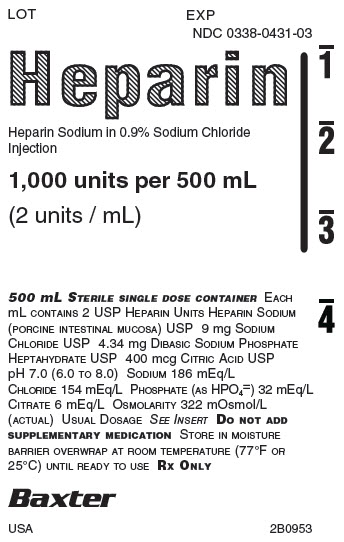
LOT EXP
NDC 0338-0431-03
Heparin
Heparin Sodium in 0.9% Sodium Chloride
Injection
1,000 units per 500 mL
****(2 units/mL)
500 mL STERILE SINGLE DOSE CONTAINEREACH
mL CONTAINS 2 USP HEPARIN UNITS HEPARIN SODIUM
(PORCINE INTESTINAL MUCOSA) USP 9 mg SODIUM
CHLORIDE USP 4.34 mg DIBASIC SODIUM PHOSPHATE
HEPTAHYDRATE USP 400 mcg CITRIC ACID USP
pH 7.0 (6.0 TO 8.0) SODIUM 186 mEq/L
CHLORIDE 154 mEq/L PHOSPHATE (AS HPO4=) 32 mEq/L
CITRATE 6 mEq/L OSMOLARITY 322 mOsmol/L
(ACTUAL) USUAL DOSAGE SEE INSERTDO NOT ADD
SUPPLEMENTARY MEDICATION STORE IN MOISTURE
BARRIER OVERWRAP AT ROOM TEMPERATURE (77°F OR
25°C) UNTIL READY TO USERX ONLY
Baxter** Logo**
USA 2B0953
1
2
Container Label
Container Label
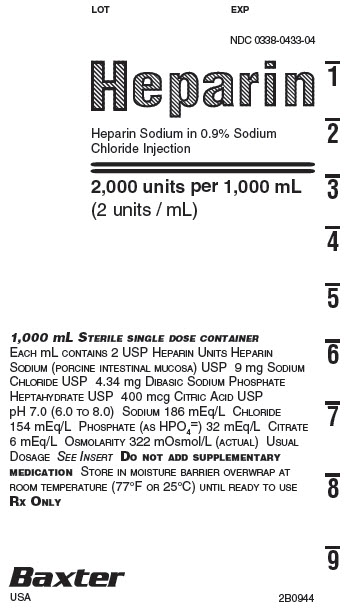
LOT EXP
NDC 0338-0433-04
Heparin
Heparin Sodium in 0.9% Sodium
Chloride Injection
2,000 units per 1,000 mL
(2 units / mL)
1,000 mL STERILE SINGLE DOSE CONTAINER
EACH mL CONTAINS 2 USP HEPARIN UNITS HEPARIN
SODIUM (PORCINE INTESTINAL MUCOSA) USP 9 mg SODIUM
CHLORIDE USP 4.34 mg DIBASIC SODIUM PHOSPHATE
HEPTAHYDRATE USP 400 mcg CITRIC ACID USP
pH 7.0 (6.0 TO 8.0) SODIUM 186 mEq/L CHLORIDE
154 mEq/L PHOSPHATE (AS HPO4=) 32 mEq/L CITRATE
6 mEq/L OSMOLARITY 322 mOsmol/L (ACTUAL) USUAL
DOSAGE SEE INSERTDO NOT ADD SUPPLEMENTARY
MEDICATION STORE IN MOISTURE BARRIER OVERWRAP AT
ROOM TEMPERATURE (77°F OR 25°C) UNTIL READY TO USE
RX ONLY
Baxter** Logo**
USA 2B0944
07-25-58-614
1
2
3
4
5
6
7
8
9
Container Label
Container Label
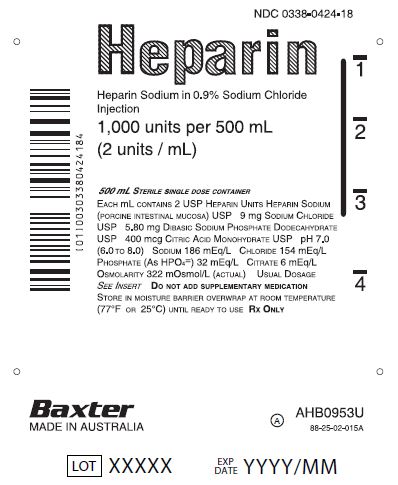
NDC 0338-0424-18
Heparin
Heparin Sodium in 0.9% Sodium Chloride
Injection
1,000 units per 500 mL
(2 units / mL)
500 mL STERILE SINGLE DOSE CONTAINER
****EACH mL CONTAINS 2 USP HEPARIN UNITS HEPARIN SODIUM
(PORCINE INTESTINAL MUCOSA) USP 9 mg SODIUM CHLORIDE
USP 5.80 mg DIBASIC SODIUM PHOSPHATE DODECAHYDRATE
USP 400 mcg CITRIC ACID MONOHYDRATE USP pH 7.0
(6.0 TO 8.0) SODIUM 186 mEq/L CHLORIDE 154 mEq/L
PHOSPHATE (AS HPO4=) 32 mEq/L CITRATE 6 mEq/L
OSMOLARITY 322 mOsmol/L (ACTUAL) USUAL DOSAGE
SEE INSERTDO NOT ADD SUPPLEMENTARY MEDICATION
STORE IN MOISTURE BARRIER OVERWRAP AT ROOM TEMPERATURE
(77°F OR 25°C) UNTIL READY TO USERX ONLY
Baxter** Logo**
MADE IN AUSTRALIA
AHB0953U
A
88-25-02-015A
LOT XXXXX
EXP
DATE
YYYY/MM
1
2
3
4
Barcode
(01)00303380424184
Container Label
Container Label
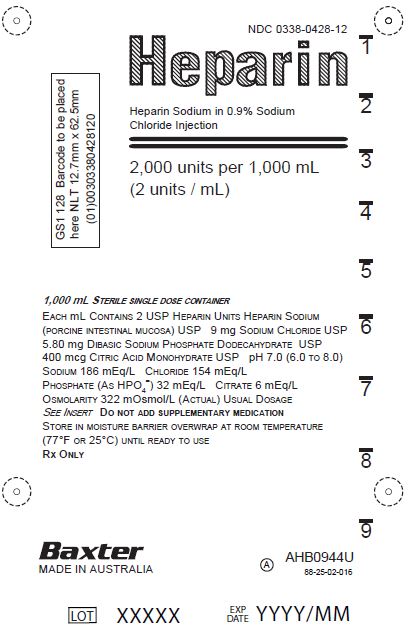
NDC 0338-0428-12
Heparin
Heparin Sodium in 0.9% Sodium Chloride
Injection
2,000 units per 1,000 mL
(2 units / mL)
1,000 mL STERILE SINGLE DOSE CONTAINER
****EACH mL CONTAINS 2 USP HEPARIN UNITS HEPARIN SODIUM
(PORCINE INTESTINAL MUCOSA) USP 9 mg SODIUM CHLORIDE USP
5.80 mg DIBASIC SODIUM PHOSPHATE DODECAHYDRATE USP
400 mcg CITRIC ACID MONOHYDRATE USP pH 7.0 (6.0 TO 8.0)
SODIUM 186 mEq/L CHLORIDE 154 mEq/L
PHOSPHATE (AS HPO4=) 32 mEq/L CITRATE 6 mEq/L
OSMOLARITY 322 mOsmol/L (ACTUAL) USUAL DOSAGE
SEE INSERTDO NOT ADD SUPPLEMENTARY MEDICATION
STORE IN MOISTURE BARRIER OVERWRAP AT ROOM TEMPERATURE
(77°F OR 25°C) UNTIL READY TO USERX ONLY
Baxter** Logo**
MADE IN AUSTRALIA
AHB0944U
A
88-25-02-016
LOT XXXXX
EXP
DATE
YYYY/MM
1
2
3
4
5
6
7
8
9
GS1 128 Barcode to be placed
here NLT 12.7mm x 62.5mm
(01)00303380428120
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Heparin interacts with the naturally occurring plasma protein, Antithrombin III, to induce a conformational change, which markedly enhances the serine protease activity of Antithrombin III, thereby inhibiting the activated coagulation factors involved in the closing sequence, particularly Xa and IIa. Small amounts of heparin inhibit Factor Xa, and larger amounts inhibit thrombin (Factor IIa). Heparin also prevents the formation of a stable fibrin clot by inhibiting the activation of the fibrin stabilizing factor. Heparin does not have fibrinolytic activity; therefore, it will not lyse existing clots.
12.2 Pharmacodynamics
Various times (activated clotting time, activated partial thromboplastin time, prothrombin time, whole blood clotting time) are prolonged by full therapeutic doses of heparin; in most cases, they are not measurably affected by low doses of heparin. Bleeding time is usually unaffected by heparin.
12.3 Pharmacokinetics
Absorption
Heparin is not absorbed through the gastrointestinal tract and therefore administered via parenteral route. Peak plasma concentration and the onset of action are achieved immediately after intravenous administration.
Distribution
Heparin is highly bound to antithrombin, fibrinogens, globulins, serum proteases and lipoproteins. The volume of distribution is 0.07 L/kg.
Elimination
Metabolism
Heparin does not undergo enzymatic degradation.
Excretion
Heparin is mainly cleared from the circulation by liver and reticuloendothelial cells mediated uptake into extravascular space. Heparin undergoes biphasic clearance, a) rapid saturable clearance (zero order process due to binding to proteins, endothelial cells and macrophages) and b) slower first order elimination. Low doses of heparin are cleared mostly by a saturable, rapid, zero-order process. Slower first order elimination usually occurs with very high doses of heparin and is dependent on renal function. The plasma half-life is dose-dependent, and it ranges from 0.5 to 2 h.
Specific Populations
Geriatric Patients
Patients over 60 years of age, following similar doses of heparin, may have higher plasma levels of heparin and longer activated partial thromboplastin times (APTTs) compared with patients under 60 years of age [see Use in Specific Populations (8.5)].
Renal and Hepatic Impairment
The rate of clearance of unfractionated heparin may be decreased in patients with renal or hepatic impairment. Patients with renal or hepatic impairment, following similar doses of heparin may have higher plasma levels of heparin compared with patient with normal renal and hepatic function [see Warnings and Precautions (5.1)].
WARNINGS AND PRECAUTIONS SECTION
Highlight: •
Hemorrhage: Fatal cases have occurred. Monitor for signs of bleeding and manage promptly. (5.1)
•
HIT and HITT: Monitor for signs and symptoms and discontinue if indicative of HIT or HITT. (5.2)
•
Hyperkalemia: Measure plasma potassium in patients at risk of hyperkalemia before starting heparin therapy and periodically in all patients. (5.6)
•
Elevations of serum aminotransferases: Interpret elevation of these enzymes with caution. (5.7)
5 WARNINGS AND PRECAUTIONS
5.1 Hemorrhage
Avoid using heparin in the presence of major bleeding, except when the benefits of heparin therapy outweigh the potential risks.
Hemorrhage can occur at virtually any site in patients receiving heparin. Fatal hemorrhages have occurred. A higher incidence of bleeding has been reported in patients, particularly women, over 60 years of age [see Use in Specific Populations (8.5)]. An unexplained fall in hematocrit, fall in blood pressure, or any other unexplained symptom should lead to serious consideration of hemorrhagic event.
Use heparin sodium with caution in disease states in which there is increased risk of hemorrhage, including:
•
Cardiovascular - Subacute bacterial endocarditis, severe hypertension.
•
Surgical - During and immediately following (a) spinal tap or spinal anesthesia or (b) major surgery, especially involving the brain, spinal cord, or eye.
•
Hematologic - Conditions associated with increased bleeding tendencies, such as hemophilia, thrombocytopenia, and some vascular purpuras.
•
Gastrointestinal - Ulcerative lesions and continuous tube drainage of the stomach or small intestine.
•
Patients with hereditary antithrombin III deficiency receiving concurrent antithrombin III therapy – The anticoagulant effect of heparin is enhanced by concurrent treatment with antithrombin III (human) in patients with hereditary antithrombin III deficiency. To reduce the risk of bleeding, reduce the heparin dose during concomitant treatment with antithrombin III (human).
•
Other - Menstruation, liver disease with impaired hemostasis.
5.2 Heparin-Induced Thrombocytopenia and Heparin-Induced Thrombocytopenia
with Thrombosis
Heparin-induced thrombocytopenia (HIT) is a serious immune-mediated reaction. HIT occurs in patients treated with heparin and is due to the development of antibodies to a platelet Factor 4-heparin complex that induce in vivo platelet aggregation. HIT may progress to the development of venous and arterial thromboses, a condition referred to as heparin-induced thrombocytopenia with thrombosis (HITT). Thrombotic events may also be the initial presentation for HITT. These serious thromboembolic events include deep vein thrombosis, pulmonary embolism, cerebral vein thrombosis, limb ischemia, stroke, myocardial infarction, mesenteric thrombosis, renal arterial thrombosis, skin necrosis, gangrene of the extremities that may lead to amputation, and possibly death.
Once HIT or HITT is diagnosed or strongly suspected, discontinue all heparin sources (including heparin flushes) and use an alternative anticoagulant.
Immune-mediated HIT is diagnosed based on clinical findings supplemented by laboratory tests confirming the presence of antibodies to heparin, or platelet activation induced by heparin. Obtain platelet counts at baseline and periodically during heparin administration. A drop in platelet count greater than 50% from baseline is considered indicative of HIT. Platelet counts begin to fall 5 to 10 days after exposure to heparin in heparin–naive individuals and reach a threshold by days 7 to 14. In contrast, “rapid onset” HIT can occur very quickly (within 24 hours following heparin initiation), especially in patients with a recent exposure to heparin (i.e., previous 3 months). Thrombosis development shortly after documenting thrombocytopenia is a characteristic finding in almost half of all patients with HIT.
Monitor any degree of thrombocytopenia closely. If the platelet count falls below 100,000/mm3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant. HIT or HITT can occur up to several weeks after the discontinuation of heparin therapy. Evaluate patients presenting with thrombocytopenia or thrombosis after discontinuation of heparin sodium for HIT or HITT.
5.3 Thrombocytopenia
Thrombocytopenia in patients receiving heparin has been reported at frequencies up to 30%. It can occur 2 to 20 days (average 5 to 9) following the onset of heparin therapy. Obtain platelet counts before and periodically during heparin therapy. Mild thrombocytopenia (count greater than 100,000/mm3) may remain stable or reverse even if heparin is continued. However, monitor thrombocytopenia of any degree closely. If the count falls below 100,000/mm3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant [see Warnings and Precautions (5.2)].
5.4 Heparin Resistance
Increased resistance to heparin is frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer, in postsurgical patients, and patients with anti-thrombin deficiency. Consider measurement of anti-thrombin levels if heparin resistance is suspected. Monitor coagulation tests frequently in such patients. It may be necessary to adjust the dose of heparin based on coagulation test monitoring, such as anti-Factor Xa levels and/or partial thromboplastin time.
5.5 Hypersensitivity
Hypersensitivity reactions with chills, fever and urticaria as the most usual manifestations and also asthma, rhinitis, lacrimation, and anaphylactoid reactions have been reported. Patients with documented hypersensitivity to heparin should be given the drug only in clearly life-threatening situations. Because Heparin Sodium in Sodium Chloride Injection is derived from animal tissue, it should be used with caution in patients with a history of allergy to pork products.
5.6 Hyperkalemia
Heparin can suppress adrenal secretion of aldosterone leading to hyperkalemia, particularly in patients with diabetes mellitus, chronic renal failure, pre- existing metabolic acidosis, a raised plasma potassium, or taking potassium sparing drugs. The risk of hyperkalemia appears to increase with duration of therapy but is usually reversible upon discontinuation of heparin.
Measure plasma potassium in patients at risk of hyperkalemia before starting heparin therapy and periodically in all patients treated for more than 5 days or earlier as deemed fit by the clinician.
5.7 Elevations of Serum Aminotransferases
Significant elevations of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels have occurred patients who have received heparin. Elevation of these enzymes in patients receiving heparin should be interpreted with caution. These elevations typically resolve upon heparin discontinuation.
5.8 Laboratory Tests
Periodic platelet counts, hematocrits, and tests for occult blood in stool are recommended during the entire course of heparin therapy, regardless of the route of administration.
DRUG INTERACTIONS SECTION
Highlight: Drugs that interfere with platelet aggregation or drugs that counteract coagulation may induce bleeding (7.2)
7 DRUG INTERACTIONS
7.1 Oral Anticoagulants
Heparin sodium may prolong the one-stage prothrombin time. Therefore, when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hours after the last intravenous dose or 24 hours after the last subcutaneous dose should elapse before blood is drawn if a valid prothrombin time is to be obtained.
7.2 Platelet Inhibitors
Drugs such as NSAIDS (including acetylsalicylic acid, ibuprofen, indomethacin, and celecoxib), dextran, phenylbutazone, thienopyridines, dipyridamole, hydroxychloroquine, glycoprotein IIv/IIa antagonists (including abciximab, eptifibatide, and tirofiban), and others that interfere with platelet- aggregation reactions (the main hemostatic defense of heparinized patients) may induce bleeding and should be used with caution in patients receiving heparin sodium. To reduce the risk of bleeding, a reduction in the dose of antiplatelet agent or heparin is recommended.
7.3 Other Medications that May Interfere with Heparin
Digitalis, tetracyclines, nicotine or antihistamines may partially counteract the anticoagulant action of heparin sodium. Intravenous nitroglycerin administered to heparinized patients may result in a decrease of the partial thromboplastin time with subsequent rebound effect upon discontinuation of nitroglycerin. Careful monitoring of partial thromboplastin time and adjustment of heparin dosage are recommended during coadministration of heparin and intravenous nitroglycerin.
Antithrombin III (human) – The anticoagulant effect of heparin is enhanced by concurrent treatment with antithrombin III (human) in patients with hereditary antithrombin III deficiency. To reduce the risk of bleeding, a reduced dosage of heparin is recommended during treatment with antithrombin III (human).
USE IN SPECIFIC POPULATIONS SECTION
Highlight: Geriatric Use: A higher incidence of bleeding has been reported in patients over 60 years of age, especially women (5.7, 8.5)
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on Heparin Sodium in Sodium Chloride Injection use in pregnant women to inform a drug-associated risk of major birth defects and miscarriage. In published reports heparin exposure during pregnancy did not show evidence of an increased risk of adverse maternal or fetal outcomes in humans (see Data). Consider the benefits and risks of Heparin Sodium in Sodium Chloride Injection for the mother and possible risks to the fetus when prescribing Heparin Sodium in Sodium Chloride Injection to a pregnant woman.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. However, the background risk in the U.S. general population of major birth defects is 2 to 4% and of miscarriage is 15 to 20% of clinically recognized pregnancies.
Data
Human Data
The maternal and fetal outcomes associated with uses of heparin via various dosing methods and administration routes during pregnancy have been investigated in numerous studies. These studies generally reported normal deliveries with no maternal or fetal bleeding and no other complications.
Animal Data
In a published study conducted in rats and rabbits, pregnant animals received heparin intravenously during organogenesis at a dose of 10,000 units/kg/day, more than 50 times the maximum human daily dose based on body weight. The number of early resorptions increased in both species. There was no evidence of teratogenic effects.
8.2 Lactation
Risk Summary
There is no information regarding the presence of heparin in human milk, the effects on the breastfed child, or the effects on milk production. Due to its large molecular weight, heparin is not likely to be excreted in human milk.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for heparin and any potential adverse effects on the breastfed child from heparin or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
A higher incidence of bleeding has been reported in patients over 60 years of age, especially women [see Warnings and Precautions (5.1)]. Clinical studies indicate that lower doses of heparin may be indicated in these patients [see Clinical Pharmacology (12.3)].
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Heparin Sodium in Sodium Chloride Injection in VIAFLEX PLUS plastic container is supplied as follows:
|
Product Description |
Size |
Code |
NDC |
|
1,000 USP Heparin Units in |
500 mL |
2B0953 |
0338-0431-03 |
|
1,000 USP Heparin Units in |
500 mL |
AHB0953U |
0338-0424-18 |
|
2,000 USP Heparin Units in |
1,000 mL |
2B0944 |
0338-0433-04 |
|
2,000 USP Heparin Units in |
1,000 mL |
AHB0944U |
0338-0428-12 |
Store at 25°C (77°F). Brief exposure up to 40°C (104°F) does not adversely affect the product. Avoid excessive heat.
