toremifene citrate
These highlights do not include all the information needed to use TOREMIFENE CITRATE TABLETS safely and effectively. See full prescribing information for TOREMIFENE CITRATE TABLETS. TOREMIFENE CITRATE tablets, oral administration Initial U.S. Approval: 1997
e897546b-4136-4cb5-a262-d94cf3fa3298
HUMAN PRESCRIPTION DRUG LABEL
Sep 19, 2025
Novadoz Pharmaceuticals LLC
DUNS: 081109687
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
toremifene citrate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Toremifene Citrate tablets, 60 mg - 30's container label

BOXED WARNING SECTION
WARNING: QT PROLONGATION
** Toremifene citrate has been shown to prolong the QTc interval in a dose- and concentration-related manner****[see Clinical Pharmacology (12.2)].Prolongation of the QT interval can result in a type of ventricular tachycardia called Torsade de pointes, which may result in syncope, seizure, and/or death. Toremifene should not be prescribed to patients with congenital/acquired QT prolongation, uncorrected hypokalemia or uncorrected hypomagnesemia. Drugs known to prolong the QT interval and strong CYP3A4 inhibitors should be avoided[see Warnings and Precautions (5.1)].**
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Toremifene citrate tablets are estrogen agonist/antagonist indicated for the treatment of metastatic breast cancer in postmenopausal women with estrogen- receptor positive or unknown tumors.
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
4.1 Hypersensitivity to the Drug
Toremifene citrate is contraindicated in patients with known hypersensitivity to the drug.
4.2 QT Prolongation, Hypokalemia, Hypomagnesemia
Toremifene should not be prescribed to patients with congenital/acquired QT prolongation (long QT syndrome), uncorrected hypokalemia, or uncorrected hypomagnesemia.
- Hypersensitivity to the drug (4.1)
- QT Prolongation, Hypokalemia, Hypomagnesemia (4.2)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Prolongation of the QT Interval
Toremifene has been shown to prolong the QTc interval in a dose- and
concentration-related manner[see Clinical Pharmacology (12.2)] .Prolongation
of the QT interval can result in a type of ventricular tachycardia called
Torsade de pointes, which may result in syncope, seizure, and/or death.
Toremifene should be avoided in patients with long QT syndrome. Caution should
be exercised in patients with congestive heart failure, hepatic impairment and
electrolyte abnormalities. Hypokalemia or hypomagnesemia must be corrected
prior to initiating toremifene and these electrolytes should be monitored
periodically during therapy. Drugs that prolong the QT interval should be
avoided. In patients at increased risk, electrocardiograms (ECGs) should be
obtained at baseline and as clinically indicated [see Drug Interactions (7.2) and Clinical Pharmacology (12.2)].
5.2 Hepatotoxicity
Hepatotoxicity, both increases in the serum concentration for grade 3 and 4 transaminitis and hyperbilirubinemia, including jaundice, hepatitis, and non- alcoholic fatty liver disease, have also been reported in clinical trials and postmarketing with toremifene citrate. Liver function tests should be performed periodically. [see Adverse Reactions (6.1), Post-marketing Experience (6.2)]
5.3 Hypercalcemia and Tumor Flare
As with other antiestrogens, hypercalcemia and tumor flare have been reported in some breast cancer patients with bone metastases during the first weeks of treatment with toremifene citrate. Tumor flare is a syndrome of diffuse musculoskeletal pain and erythema with increased size of tumor lesions that later regress. It is often accompanied by hypercalcemia. Tumor flare does not imply failure of treatment or represent tumor progression. If hypercalcemia occurs, appropriate measures should be instituted and, if hypercalcemia is severe, toremifene citrate treatment should be discontinued.
5.4 Risk of Uterine Malignancy
Endometrial cancer, endometrial hypertrophy, hyperplasia, and uterine polyps have been reported in some patients treated with toremifene citrate. Endometrial hyperplasia of the uterus was observed in animals treated with toremifene [see Nonclinical Toxicology (13.1)]. Long-term use of toremifene citrate has not been established in patients with pre-existing endometrial hyperplasia. All patients should have baseline and annual gynecological examinations. In particular, patients at high risk of endometrial cancer should be closely monitored.
5.5 General
Patients with a history of thromboembolic diseases should generally not be
treated with toremifene citrate. Patients with bone metastases should be
monitored closely for hypercalcemia during the first weeks of treatment [see Warnings and Precautions (5.2)].
Leukopenia and thrombocytopenia have been reported rarely; leukocyte and
platelet counts should be monitored when using toremifene citrate in patients
with leukopenia and thrombocytopenia.
5.6 Laboratory Tests
Periodic complete blood counts, calcium levels, and liver function tests should be obtained.
5.7 Use in Pregnancy
Based on its mechanism of action in humans and findings of increased pregnancy loss and fetal malformation in animal studies, toremifene citrate can cause fetal harm when administered to a pregnant woman. Toremifene caused embryo- fetal toxicities at maternal doses that were lower than the 60 mg daily recommended human dose on a mg/m2 basis. There are no adequate and well- controlled studies in pregnant women using toremifene citrate. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus [see Use in Specific Populations (8.1)].
5.8 Women of Childbearing Potential
Toremifene citrate is indicated only in postmenopausal women. However, premenopausal women prescribed toremifene citrate should use effective non- hormonal contraception and should be apprised of the potential hazard to the fetus should pregnancy occur.
- Prolongation of the QT Interval(5.1)
- Heptatotoxicty (5.2)
- Hypercalcemia and Tumor Flare (5.3)
- Risk of Uterine Malignancy (5.4)
- General (5.5)
- Laboratory Tests (5.6)
- Pregnancy: Fetal harm may occur when administered to a pregnant woman. Women should be advised not to become pregnant when taking toremifene citrate. (5.7, 8.1)
- Women of Childbearing Potential: Use effective nonhormonal contraception during toremifene citrate therapy. (5.8)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
6.1 Clinical Trials Experience
Adverse drug reactions are principally due to the antiestrogenic actions of
toremifene citrate and typically occur at the beginning of treatment.
The incidences of the following eight clinical toxicities were prospectively
assessed in the North American Study. The incidence reflects the toxicities
that were considered by the investigator to be drug related or possibly drug
related.
|
North American Study | ||
|
FAR60 |
TAM20 | |
|
n = 221 |
n = 215 | |
|
Hot Flashes |
35% |
30% |
|
Sweating |
20% |
17% |
|
Nausea |
14% |
15% |
|
Vaginal Discharge |
13% |
16% |
|
Dizziness |
9% |
7% |
|
Edema |
5% |
5% |
|
Vomiting |
4% |
2% |
|
Vaginal Bleeding |
2% |
4% |
Approximately 1% of patients receiving toremifene citrate (n = 592) in the
three controlled studies discontinued treatment as a result of adverse
reactions (nausea and vomiting, fatigue, thrombophlebitis, depression,
lethargy, anorexia, ischemic attack, arthritis, pulmonary embolism, and
myocardial infarction).
Serious adverse reactions occurring in at least 1% of patients receiving
toremifene citrate in the three major trials are listed in the table below.
Three prospective, randomized, controlled clinical studies (North American,
Eastern European, and Nordic) were conducted. The patients were randomized to
parallel groups receiving toremifene citrate 60 mg (FAR60) or tamoxifen 20 mg
(TAM20) in the North American Study or tamoxifen 40 mg (TAM40) in the Eastern
European and Nordic studies. The North American and Eastern European studies
also included high-dose toremifene arms of 200 and 240 mg daily, respectively
[see Clinical Studies (14)].
|
Adverse Reactions |
North American |
Eastern European |
Nordic | |||||||||
|
FAR60 |
TAM20 |
FAR60 |
TAM40 |
FAR60 |
TAM40 | |||||||
|
n=221(%) |
n=215(%) |
n=157(%) |
n=149(%) |
n=214(%) |
n=201(%) | |||||||
|
Cardiac | ||||||||||||
|
Cardiac Failure |
2 |
(1) |
1 |
(<1) |
- |
1 |
(<1) |
2 |
(1) |
3 |
(1.5) | |
|
Myocardial Infarction |
2 |
(1) |
3 |
(1.5) |
1 |
(<1) |
2 |
(1) |
- |
1 |
(<1) | |
|
Arrhythmia |
- |
- |
- |
- |
3 |
(1.5) |
1 |
(<1) | ||||
|
Angina Pectoris |
- |
- |
1 |
(<1) |
- |
1 |
(<1) |
2 |
(1) | |||
|
Ocular* | ||||||||||||
|
Cataracts |
22 |
(10) |
16 |
(7.5) |
- |
- |
- |
5 |
(3) | |||
|
Dry Eyes |
20 |
(9) |
16 |
(7.5) |
- |
- |
- |
- | ||||
|
Abnormal Visual Fields |
8 |
(4) |
10 |
(5) |
- |
- |
- |
1 |
(<1) | |||
|
Corneal Keratopathy |
4 |
(2) |
2 |
(1) |
- |
- |
- |
- | ||||
|
Glaucoma |
3 |
(1.5) |
2 |
(1) |
1 |
(<1) |
- |
- |
1 |
(<1) | ||
|
Abnormal |
- |
- |
- |
- |
3 |
(1.5) |
- | |||||
|
Vision/Diplopia | ||||||||||||
|
Thromboembolic | ||||||||||||
|
Pulmonary Embolism |
4 |
(2) |
2 |
(1) |
1 |
(<1) |
- |
- |
1 |
(<1) | ||
|
Thrombophlebitis |
- |
2 |
(1) |
1 |
(<1) |
1 |
(<1) |
4 |
(2) |
3 |
(1.5) | |
|
Thrombosis |
- |
1 |
(<1) |
1 |
(<1) |
- |
3 |
(1.5) |
4 |
(2) | ||
|
CVA/TIA |
1 |
(<1) |
- |
- |
1 |
(<1) |
4 |
(2) |
4 |
(2) | ||
|
Elevated Liver Tests** | ||||||||||||
|
AST |
11 |
(5) |
4 |
(2) |
30 |
(19) |
22 |
(15) |
32 |
(15) |
35 |
(17) |
|
Alkaline Phosphatase |
41 |
(19) |
24 |
(11) |
16 |
(10) |
13 |
(9) |
18 |
(8) |
31 |
(15) |
|
Bilirubin |
3 |
(1.5) |
4 |
(2) |
2 |
(1) |
1 |
(<1) |
2 |
(1) |
3 |
(1.5) |
|
Hypercalcemia |
6 |
(3) |
6 |
(3) |
1 |
(<1) |
- |
- |
- |
- Most of the ocular abnormalities were observed in the North American Study in which on-study and biannual ophthalmic examinations were performed. No cases of retinopathy were observed in any arm.
** Elevated defined as follows: North American Study: AST >100 IU/L; alkaline phosphatase >200 IU/L; bilirubin > 2 mg/dL. Eastern European and Nordic studies: AST, alkaline phosphatase, and bilirubin – WHO Grade 1 (1.25 times the upper limit of normal).
Other adverse reactions included leukopenia and thrombocytopenia, skin discoloration or dermatitis, constipation, dyspnea, paresis, tremor, vertigo, pruritus, anorexia, reversible corneal opacity (corneal verticulata), asthenia, alopecia, depression, jaundice, and rigors.
The incidence of AST elevations was greater in the 200 and 240 mg toremifene citrate dose arms than in the tamoxifen arms. Higher doses of toremifene citrate were also associated with an increase in nausea.
Approximately 4% of patients were withdrawn for toxicity from the high-dose toremifene citrate treatment arms. Reasons for withdrawal included hypercalcemia, abnormal liver function tests, and one case each of toxic hepatitis, depression, dizziness, incoordination, ataxia, blurry vision, diffuse dermatitis, and a constellation of symptoms consisting of nausea, sweating, and tremor.
6.2 Post-marketing Experience
The following adverse reactions were identified during post approval use of
toremifene citrate. Because these reactions are reported voluntarily from a
population of uncertain size, it is not always possible to reliably estimate
their frequency or establish a causal relationship to drug exposure.
Adverse reactions reported during post approval use of toremifene citrate have
been consistent with clinical trial experience. The most frequently reported
adverse reactions related to toremifene citrate use since market introduction
include hot flash, sweating, nausea, and vaginal discharge.
Hepatototoxicity [see Warnings and Precautions (5.2)]
Risk of Uterine Malignancy[see Warnings and Precautions (5.4)]
Hypertriglyceridemia
Most common adverse reactions are hot flashes, sweating, nausea and vaginal
discharge. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novadoz Pharmaceuticals LLC at
1-855-668-2369 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Drugs that Decrease Renal Calcium Excretion
Drugs that decrease renal calcium excretion, e.g., thiazide diuretics, may increase the risk of hypercalcemia in patients receiving toremifene citrate.
7.2 Agents that Prolong QT
The administration of toremifene citrate with agents that have demonstrated QT prolongation as one of their pharmacodynamic effects should be avoided. Should treatment with any of these agents be required, it is recommended that therapy with toremifene citrate be interrupted. If interruption of treatment with toremifene citrate is not possible, patients who require treatment with a drug that prolongs QT should be closely monitored for prolongation of the QT interval. Agents generally accepted to prolong QT interval include Class 1A (e.g., quinidine, procainamide, disopyramide) and Class III (e.g., amiodarone, sotalol, ibutilide, dofetilide) antiarrhythmics; certain antipsychotics (e.g., thioridazine, haloperidol); certain antidepressants (e.g., venlafaxine, amitriptyline); certain antibiotics (e.g., erythromycin, clarithromycin, levofloxacin, ofloxacin); and certain anti-emetics (e.g., ondansetron, granisetron). In patients at increased risk, electrocardiograms (ECGs) should be obtained and patients monitored as clinically indicated [see Boxed Warningand Warnings and Precautions (5.1)].
7.3 Effect of Strong CYP3A4 Inducers on Toremifene
Strong CYP3A4 enzyme inducers, such as dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, phenobarbital, St. John’s Wort, lower the steady-state concentration of toremifene in serum.
7.4 Effect of Strong CYP3A4 Inhibitors on Toremifene
In a study of 18 healthy subjects, 80 mg toremifene once daily coadministered
with 200 mg of ketoconazole twice daily increased the toremifene Cmax and AUC
by 1.4- and 2.9-fold, respectively. N-demethyltoremifene Cmax and AUC were
reduced by 56% and 20%, respectively.
The administration of toremifene citrate with agents that are strong CYP3A4
inhibitors (e.g., ketoconazole, itraconazole, clarithromycin, atazanavir,
indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, and
voriconazole) increase the steady-state concentration in serum and should be
avoided. Grapefruit juice may also increase plasma concentrations of
toremifene and should be avoided. Should treatment with any of these agents be
required, it is recommended that therapy with toremifene citrate be
interrupted. If interruption of treatment with toremifene citrate is not
possible, patients who require treatment with a drug that strongly inhibits
CYP3A4 should be closely monitored for prolongation of the QT interval [see Boxed Warningand Warnings and Precautions (5.1)].
7.5 Effect of Toremifene on CYP3A4 Substrates
In a study of 20 healthy subjects, 2 mg midazolam once daily (days 6 and 18)
coadministered with toremifene as a 480 mg loading dose followed by 80 mg once
daily for 16 days. Following coadministration on days 6 and 18 relevant
increases in midazolam and α-hydroxymidazolam Cmax and AUC were not observed.
Following coadministration on day 18 midazolam and α-hydroxymidazolam Cmax and
AUC were reduced by less than 20%.
Clinically relevant exposure changes in sensitive substrates due to inhibition
or induction of CYP3A4 by toremifene appear unlikely.
7.6 Effect of Toremifene on CYP2C9 Substrates
In a study of 20 healthy subjects, 500 mg tolbutamide once daily (days 7 and
19) coadministered with toremifene as a 480 mg loading dose followed by 80 mg
once daily for 16 days. Following coadministration on days 7 and 19 plasma
tolbutamide Cmax and AUC were increased by less than 30%. A reduction of
similar magnitude was observed for hydroxytolbutamide and carboxytolbutamide
Cmax and AUC.
Toremifene is a weak inhibitor of CYP2C9. Concomitant use of CYP2C9 substrates
with a narrow therapeutic index such as warfarin or phenytoin with toremifene
citrate should be done with caution and requires careful monitoring (e.g.,
substrate concentrations (if possible), appropriate laboratory markers, and
signs and symptoms of increased exposure).
- Drugs that decrease renal calcium excretion, e.g., thiazide diuretics, may increase the risk of hypercalcemia in patients receiving toremifene citrate. (7.1)
- Agents that prolong QT should be avoided. (7.2)
- Coadministration with a strong CYP3A4 inducer may result in a relevant decrease in toremifene citrate exposure and should be avoided. (7.3)
- Coadministration with a strong CYP3A4 inhibitor can result in a relevant increase in toremifene citrate exposure and should be avoided. (7.4)
- CYP2C9 substrates with a narrow therapeutic index such as warfarin or phenytoin with toremifene citrate should be used with caution and require careful monitoring. (7.6)
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Toremifene is a nonsteroidal triphenylethylene derivative. Toremifene binds to estrogen receptors and may exert estrogenic, antiestrogenic, or both activities, depending upon the duration of treatment, animal species, gender, target organ, or endpoint selected. In general, however, nonsteroidal triphenylethylene derivatives are predominantly antiestrogenic in rats and humans and estrogenic in mice. In rats, toremifene causes regression of established dimethylbenzanthracene (DMBA)-induced mammary tumors. The antitumor effect of toremifene in breast cancer is believed to be mainly due to its antiestrogenic effects, i.e., its ability to compete with estrogen for binding sites in the cancer, blocking the growth-stimulating effects of estrogen in the tumor.
12.2 Pharmacodynamics
Toremifene causes a decrease in the estradiol-induced vaginal cornification
index in some postmenopausal women, indicative of its antiestrogenic activity.
Toremifene also has estrogenic activity as shown by decreases in serum
gonadotropin concentrations (FSH and LH).
Effects on Cardiac Electrophysiology
The effect of 20 mg, 80 mg, and 300 mg of toremifene on QT interval was
evaluated in a double-blind, randomized study in healthy male subjects aged 18
to 45 years. The QT interval was measured at steady state of toremifene (Day 5
of dosing), including the time of peak plasma concentration (Tmax), at 13 time
points (4 ECGs/time point) over 24 hours post dose in a time matched analysis.
The 300 mg dose of toremifene (approximately five times the highest
recommended dose 60 mg) was chosen because this dose produces exposure to
toremifene that will cover the expected exposures that may result from
potential drug interactions and hepatic impairment [see Drug Interactions (7.2)].
Dose and concentration-related increases in the QTc interval and T wave
changes were observed (see Table 1). These effects are believed to be caused
by toremifene and N-demethyltoremifene. Toremifene had no effects on heart
rate, PR and QRS interval duration [see Boxed Warningand Warnings and Precautions (5.1)].
Table 1: QTc Prolongation in Healthy Male Volunteers
|
Treatment Arm |
Mean (90% CI) |
ΔQTc > 60 ms (n, %) |
QTc > 500 ms (n, %) |
|
Toremifene 20 mg (N = 47) |
7 (0.9, 13.6) |
0 |
0 |
|
Toremifene 80 mg (N = 47) |
26 (21.1, 31.2) |
2 (4.3%) |
0 |
|
Toremifene 300 mg (N = 48) |
65 (60.1, 69.2) |
43 (89.6%) |
5 (10.4%) |
12.3 Pharmacokinetics
Absorption – Toremifene is well absorbed after oral administration and
absorption is not influenced by food. Peak plasma concentrations are obtained
within 3 hours. Toremifene displays linear pharmacokinetics after single oral
doses of 10 to 680 mg. After multiple dosing, dose proportionality was
observed for doses of 10 to 400 mg. Steady state concentrations were reached
in about 4-6 weeks.
Distribution – Toremifene has an apparent volume of distribution of 580 L
and binds extensively (>99.5%) to serum proteins, mainly albumin.
Metabolism – Toremifene is extensively metabolized, principally by CYP3A4
to N-demethyltoremifene which is also antiestrogenic but with weak in vivo
antitumor potency. Serum concentrations of N-demethyltoremifene are 2 to 4
times higher than toremifene at steady state.
Following multiple dosing with toremifene in 20 healthy volunteers, plasma
toremifene exposure was lower on Day 17 compared to Day 5 by approximately
14%. N-demethyltoremifene exposure was higher on Day 17 compared to Day 5 by
approximately 80%. Based on these data and an in vitro induction study in
human hepatocytes, auto- induction of CYP3A4 by toremifene is likely. The
effect of auto-induction on efficacy was likely captured following prolonged
dosing in the clinical studies.
Elimination – The plasma concentration time profile of toremifene declines
biexponentially after absorption with a mean distribution half-life of about 4
hours and an elimination half-life of about 5 days. Elimination half-lives of
major metabolites, N-demethyltoremifene and (Deaminohydroxy) toremifene, were
6 and 4 days, respectively. Mean total clearance of toremifene was
approximately 5 L/h. Toremifene is eliminated as metabolites primarily in the
feces, with about 10% excreted in the urine during a 1-week period.
Elimination of toremifene is slow, in part because of enterohepatic
circulation.
Renal insufficiency – The pharmacokinetics of toremifene and
N-demethyltoremifene were similar in normals and patients with impaired kidney
function.
Hepatic insufficiency – The mean elimination half-life of toremifene was
increased by less than twofold in 10 patients with hepatic impairment
(cirrhosis or fibrosis) compared to subjects with normal hepatic function. The
pharmacokinetics of N-demethyltoremifene were unchanged in these patients. Ten
patients on anticonvulsants (phenobarbital, clonazepam, phenytoin, and
carbamazepine) showed a twofold increase in clearance and a decrease in the
elimination half-life of toremifene.
Geriatric patients – The pharmacokinetics of toremifene were studied in 10
healthy young males and 10 elderly females following a single 120 mg dose
under fasting conditions. Increases in the elimination half-life (4.2 versus
7.2 days) and the volume of distribution (457 versus 627 L) of toremifene were
seen in the elderly females without any change in clearance or AUC. The median
ages in the three controlled studies ranged from 60 to 66 years. No
significant age-related differences in toremifene citrate effectiveness or
safety were noted.
Food – The rate and extent of absorption of toremifene citrate are not
influenced by food; thus toremifene citrate may be taken with or without food.
Race – The pharmacokinetics of toremifene in patients of different races
has not been studied. Fourteen percent of patients in the North American Study
were non-Caucasian. No significant race-related differences in toremifene
citrate effectiveness or safety were noted.
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
Three prospective, randomized, controlled clinical studies (North American,
Eastern European, and Nordic) were conducted to evaluate the efficacy of
toremifene citrate for the treatment of breast cancer in postmenopausal women.
The patients were randomized to parallel groups receiving toremifene citrate
60 mg (FAR60) or tamoxifen 20 mg (TAM20) in the North American Study or
tamoxifen 40 mg (TAM40) in the Eastern European and Nordic studies. The North
American and Eastern European studies also included high-dose toremifene arms
of 200 and 240 mg daily, respectively. The studies included postmenopausal
patients with estrogen-receptor (ER) positive or estrogen-receptor (ER)
unknown metastatic breast cancer. The patients had at least one measurable or
evaluable lesion. The primary efficacy variables were response rate (RR) and
time to progression (TTP). Survival (S) was also determined. Ninety-five
percent confidence intervals (95% CI) were calculated for the difference in RR
between FAR60 and TAM groups and the hazard ratio (relative risk for an
unfavorable event, such as disease progression or death) between TAM and FAR60
for TTP and S.
Two of the 3 studies showed similar results for all effectiveness endpoints.
However, the Nordic Study showed a longer time to progression for tamoxifen
(see table).
Clinical Studies
|
Study |
North American |
Eastern European |
Nordic | |||
|
Treatment Group |
FAR60 |
TAM20 |
FAR60 |
TAM40 |
FAR60 |
TAM40 |
|
No. Patients |
221 |
215 |
157 |
149 |
214 |
201 |
|
Responses |
14 + 33 |
11 + 30 |
7 + 25 |
3 + 28 |
19 + 48 |
19 + 56 |
|
RR3(CR + PR)% |
21.3 |
19.1 |
20.4 |
20.8 |
31.3 |
37.3 |
|
Difference in RR |
2.2 |
-0.4 |
-6.0 | |||
|
95% CI4for Difference in RR |
-5.8 to 10.2 |
-9.5 to 8.6 |
-15.1 to 3.1 | |||
|
Time to Progression (TTP) | ||||||
|
Median TTP (mo.) |
5.6 |
5.8 |
4.9 |
5.0 |
7.3 |
10.2 |
|
Hazard Ratio (TAM/FAR) |
1.01 |
1.02 |
0.80 | |||
|
95% CI4 for Hazard Ratio (%) |
0.81 to 1.26 |
0.79 to 1.31 |
0.64 to 1.00 | |||
|
Survival (S) | ||||||
|
Median S (mo.) |
33.6 |
34.0 |
25.4 |
23.4 |
33.0 |
38.7 |
|
Hazard Ratio (TAM/FAR) |
0.94 |
0.96 |
0.94 | |||
|
95% CI4 for Hazard Ratio(%) |
0.74 to 1.24 |
0.72 to 1.28 |
0.73 to 1.22 |
1CR = complete response; 2PR = partial response; 3RR = response rate; 4CI =
confidence interval
The high-dose groups, toremifene 200 mg daily in the North American Study and
240 mg daily in the Eastern European Study, were not superior to the lower
toremifene dose groups, with response rates of 22.6% and 28.7%, median times
to progression of 5.6 and 6.1 months, and median survivals of 30.1 and 23.8
months, respectively. The median treatment duration in the three pivotal
studies was 5 months (range 4.2-6.3 months).
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
The dosage of toremifene citrate tablets are 60 mg, once daily, orally. Treatment is generally continued until disease progression is observed.
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Tablet is 60 mg, white to off white colored, round shaped, uncoated tablets, debossed with “MT” on one side and plain on other side and free from physical defects.
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D [see Warnings and Precautions (5.6).]
Based on its mechanism of action in humans and findings of increased pregnancy
loss and fetal malformation in animal studies, toremifene citrate can cause
fetal harm when administered to a pregnant woman. Toremifene caused embryo-
fetal toxicities at maternal doses that were lower than the 60 mg daily
recommended human dose on a mg/m2 basis. There are no adequate and well-
controlled studies in pregnant women using toremifene citrate. If this drug is
used during pregnancy, or if the patient becomes pregnant while taking this
drug, the patient should be apprised of the potential hazard to the fetus.
In animal studies, toremifene crossed the placenta and accumulated in the
rodent fetus. Administration of toremifene to pregnant rats during
organogenesis at doses of approximately 6% the daily maximum recommended human
dose of 60 mg (on a mg/m2 basis) resulted in signs of maternal toxicity and
increased preimplantation loss, increased resorptions, reduced fetal weight,
and fetal anomalies. Fetal anomalies include malformation of limbs, incomplete
ossification, misshapen bones, ribs/spine anomalies, hydroureter,
hydronephrosis, testicular displacement, and subcutaneous edema. Maternal
toxicity may have contributed to these adverse embryo-fetal effects. Similar
embryo-fetal toxicities occurred in rabbits that received toremifene at doses
approximately 40% the daily recommended human dose of 60 mg (on a mg/m2
basis). Findings in rabbits included increased preimplantation loss, increased
resorptions, and fetal anomalies, including incomplete ossification and
anencephaly.
Animal doses resulting in embryo-fetal toxicities were ≥1.0 mg/kg/day in rats
and ≥1.25 mg/kg/day in rabbits.
In rodent models of fetal reproductive tract development, toremifene produced
inhibition of uterine development in female pups similar to effects seen with
diethylstilbestrol (DES) and tamoxifen. The clinical relevance of these
changes is not known. Neonatal rodent studies have not been conducted to
assess the potential for toremifene to cause other DES-like effects in
offspring (i.e., vaginal adenosis). Vaginal adenosis in animals occurred
following treatment with other drugs of this class and has been observed in
women exposed to diethylstilbestrol in utero.
8.2 Nursing Mothers
It is not known if toremifene is excreted in human milk. Toremifene is excreted in the milk of lactating rats. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from toremifene citrate, a decision should be made to either discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.3 Pediatric Use
There is no indication for use of toremifene citrate in pediatric patients.
8.4 Geriatric Use
The pharmacokinetics of toremifene were studied in 10 healthy young males and
10 elderly females following a single 120 mg dose under fasting conditions.
Increases in the elimination half-life (4.2 versus 7.2 days) and the volume of
distribution (457 versus 627 L) of toremifene were seen in the elderly females
without any change in clearance or AUC.
The median ages in the three controlled studies ranged from 60 to 66 years. No
significant age-related differences in toremifene citrate effectiveness or
safety were noted.
8.5 Renal Impairment
The pharmacokinetics of toremifene and N-demethyltoremifene were similar in normals and in patients with impaired kidney function.
8.6 Hepatic Impairment
The mean elimination half-life of toremifene was increased by less than twofold in 10 patients with hepatic impairment (cirrhosis or fibrosis) compared to subjects with normal hepatic function. The pharmacokinetics of N-demethyltoremifene were unchanged in these patients. Ten patients on anticonvulsants (phenobarbital, clonazepam, phenytoin, and carbamazepine) showed a twofold increase in clearance and a decrease in the elimination half- life of toremifene.
8.7 Race
The pharmacokinetics of toremifene in patients of different races has not been
studied.
Fourteen percent of patients in the North American Study were non-Caucasian.
No significant race-related differences in toremifene citrate effectiveness or
safety were noted.
- Nursing Mothers: Discontinue drug or nursing taking into account the importance of the drug to the mother. (8.2)
OVERDOSAGE SECTION
10 OVERDOSAGE
Lethality was observed in rats following single oral doses that were ≥1000
mg/kg (about 150 times the recommended human dose on a mg/m2 basis) and was
associated with gastric atony/dilatation leading to interference with
digestion and adrenal enlargement.
Vertigo, headache, and dizziness were observed in healthy volunteer studies at
a daily dose of 680 mg for 5 days. The symptoms occurred in two of the five
subjects during the third day of the treatment and disappeared within 2 days
of discontinuation of the drug. No immediate concomitant changes in any
measured clinical chemistry parameters were found. In a study in
postmenopausal breast cancer patients, toremifene 400 mg/m2/day caused dose-
limiting nausea, vomiting, and dizziness, as well as reversible hallucinations
and ataxia in one patient.
Theoretically, overdose may be manifested as an increase of antiestrogenic
effects, such as hot flashes; estrogenic effects, such as vaginal bleeding; or
nervous system disorders, such as vertigo, dizziness, ataxia, and nausea.
There is no specific antidote and the treatment is symptomatic.
DESCRIPTION SECTION
11 DESCRIPTION
Toremifene citrate tablets for oral administration each contain 88.5 mg of
toremifene citrate, which is equivalent to 60 mg toremifene.
Toremifene citrate tablets are estrogen agonist/antagonist. The chemical name
of toremifene is:
2-{p-[(Z)-4-chloro-1,2-diphenyl-1-butenyl]phenoxy}-N,N-dimethylethylamine
citrate(1:1).The structural formula is:
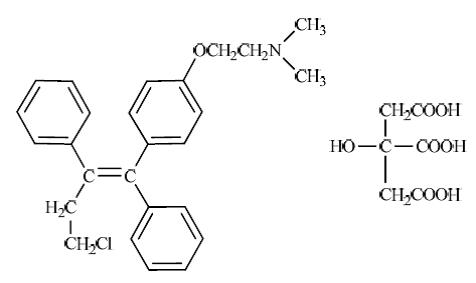
and the molecular formula is C26H28ClNO . C6H8O7. The molecular weight of
toremifene citrate is 598.10. The pKa is 7.76. Freely soluble in dimethyl
sulphoxide, sparingly soluble in methanol and insoluble in water.
Toremifene citrate tablets are available only as tablets for oral
administration. Inactive ingredients: colloidal silicon dioxide, corn starch,
lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone
K 30, and sodium starch glycolate.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, and Impairment of Fertility
Conventional carcinogenesis studies in rats at doses of 0.12 to 12 mg/kg/day
(approximately 1/50 to 2 times the daily maximum recommended human dose of 60
mg, on a mg/m2 basis) for up to 2 years did not show evidence of
carcinogenicity. Studies in mice at doses of 1.0 to 30.0 mg/kg/day
(approximately 1/15 to 2 times the daily maximum recommended human dose of 60
mg, on a mg/m2 basis) for up to 2 years revealed increased incidence of
ovarian and testicular tumors and increased incidence of osteoma and
osteosarcoma. The significance of the mouse findings is uncertain because of
the different role of estrogens in mice and the estrogenic effect of
toremifene in mice. An increased incidence of ovarian and testicular tumors in
mice has also been observed with other human estrogen agonists/antagonists
that have primarily estrogenic activity in mice. Endometrial hyperplasia of
the uterus was observed in monkeys following 52 weeks of treatment at ≥1 mg/kg
and in dogs following 16 weeks of treatment at ≥3 mg/kg with toremifene
(approximately 1/3 and 1.4 times, respectively, the daily maximum recommended
human dose of 60 mg, on a mg/m2 basis).
Toremifene has not been shown to be mutagenic in in vitro tests (Ames and E.
coli bacterial tests). Toremifene is clastogenic in vitro (chromosomal
aberrations and micronuclei formation in human lymphoblastoid MCL-5 cells) and
in vivo (chromosomal aberrations in rat hepatocytes).
Toremifene produced impairment of fertility and conception in male and female
rats at doses ≥25.0 and 0.14 mg/kg/day, respectively (approximately 4 times
and 1/50 the daily maximum recommended human dose of 60 mg, on a mg/m2 basis).
At these doses, sperm counts, fertility index, and conception rate were
reduced in males with atrophy of seminal vesicles and prostate. In females,
fertility and reproductive indices were markedly reduced with increased pre-
and post-implantation loss. In addition, offspring of treated rats exhibited
depressed reproductive indices. Toremifene produced ovarian atrophy in dogs
administered doses ≥3 mg/kg/day (approximately 1.5 times the daily maximum
recommended human dose of 60 mg, on a mg/m2 basis) for 16 weeks. Cystic
ovaries and reduction in endometrial stromal cellularity were observed in
monkeys at doses ≥1 mg/kg/day (about 1/3 the daily maximum recommended human
dose of 60 mg, on a mg/m2 basis) for 52 weeks.
HOW SUPPLIED SECTION
16 SUPPLIED/STORAGE AND HANDLING
Toremifene citrate tablets, containing toremifene citrate in an amount
equivalent to 60 mg of toremifene, are white to off white colored, round
shaped, uncoated tablets, debossed with “MT” on one side and plain on other
side and free from physical defects.
Toremifene citrate tablets are available as:
NDC 72205-050-30 bottles of 30
Store at 25°C (77°F).
** Excursions permitted to 15-30°C (59-86°F)**
** [See USP Controlled Room Temperature.]**
** Protect from heat and light.**
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Vaginal bleeding has been reported in patients using toremifene citrate.
Patients should be informed about this and instructed to contact their
physician if such bleeding or other gynecological symptoms (changes in vaginal
discharge, pelvic pain or pressure) occur. Patients should have a
gynecological examination prior to initiation of therapy and at regular
intervals while on therapy.
Liver disorders including transaminits grade 3 and 4, hyperbilirubinemia with
jaundice have been reported in patients using toremifene citrate. Patients
should have liver function tests performed periodically while on therapy.
Toremifene citrate may harm the fetus and increase the risk for pregnancy loss
[see Warnings and Precautions (5.6) and Use in Specific Populations (8.1)].
Premenopausal women using toremifene citrate should use nonhormonal
contraception during treatment and should be apprised of the potential hazard
to the fetus should pregnancy occur [see Warnings and Precautions (5.7)].
Patients with bone metastases should be informed about the typical signs and
symptoms of hypercalcemia and instructed to contact their physician for
further assessment if such signs or symptoms occur.
Patients who must take medications known to prolong the QT interval, or potent
CYP3A4 inhibitors, should be informed of the effect of toremifene on QT
interval. Toremifene has been shown to prolong the QTc interval in a dose-
related manner [see Boxed Warning, Warnings and Precautions (5.1),and Clinical Pharmacology (12.2)].
Specific interactions with foods that inhibit CYP3A4, including grapefruit
juice, have not been studied but may increase toremifene concentrations.
Patients should avoid grapefruit products and other foods that are known to
inhibit CYP3A4 during toremifene citrate treatment.
Certain other medicines, including over-the-counter medications or herbal
supplements (such as St. John’s Wort) and toremifene, can reduce
concentrations of co-administered drugs [see Drug Interactions (7.3)].
Manufactured by:
** MSN Laboratories Private Limited**
Telangana – 509 228,
INDIA
Distributed by:
** Novadoz Pharmaceuticals LLC**
Piscataway, NJ 08854 -3714
Revised: 09/2025
