Hydroxychloroquine sulfate
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use HYDROXYCHLOROQUINE SULFATE TABLETS safely and effectively. See full prescribing information for HYDROXYCHLOROQUINE SULFATE TABLETS. HYDROXYCHLOROQUINE SULFATE Tablets, for oral use Initial U.S. Approval: 1955
b47e12d3-0395-4462-b856-2ecb033f11e6
HUMAN PRESCRIPTION DRUG LABEL
Apr 2, 2024
McKesson Corporation dba SKY Packaging
DUNS: 140529962
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Hydroxychloroquine sulfate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
Drug Labeling Information
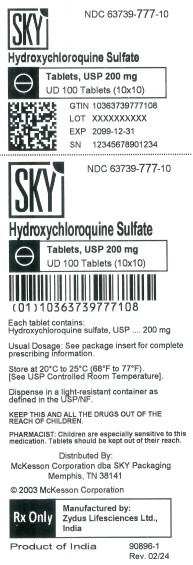
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
HYDROXYCHLOROQUINE 200MG
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
Hydroxychloroquine sulfate is contraindicated in patients with known hypersensitivity to 4-aminoquinoline compounds.
• Patients with hypersensitivity to 4-aminoquinoline compounds (4) (4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are described in greater detail in other
sections:
• Cardiomyopathy and Ventricular Arrhythmias [see Warnings and Precautions (5.1)]
• Retinal Toxicity [see Warnings and Precautions (5.2)]
• Serious Skin Reactions [see Warnings and Precautions (5.3)]
• Worsening of Psoriasis [see Warnings and Precautions (5.4)]
• Risks Associated with Use in Porphyria [see Warnings and Precautions (5.5)]
• Hematologic Toxicity [see Warnings and Precautions (5.6)]
• Hemolytic Anemia Associated with G6PD [see Warnings and Precautions (5.7)]
• Skeletal Muscle Myopathy or Neuropathy [see Warnings and Precautions (5.8)]
• Neuropsychiatric Reactions Including Suicidality [see Warnings and Precautions (5.9)]
• Hypoglycemia [see Warnings and Precautions (5.10)]
• Renal Toxicity [see Warnings and Precautions (5.11)]
The following adverse reactions have been identified during post-approval use
of 4-aminoquinoline drugs, including
hydroxychloroquine sulfate. Because these reactions are reported voluntarily
from a population of uncertain size, it is
not always possible to reliably estimate their frequency or establish a causal
relationship to drug exposure:
- Blood and lymphatic system disorders: Bone marrow depression, anemia,
aplastic anemia, agranulocytosis,
leukopenia, thrombocytopenia
- Cardiac disorders: Cardiomyopathy, cardiac failure, QT-interval
prolongation, ventricular tachycardia, torsades de
pointes, atrioventricular block, bundle branch block, sick sinus syndrome,
pulmonary hypertension
- Ear and labyrinth disorders: Vertigo, tinnitus, nystagmus, sensorineural
hearing loss
- Eye disorders: Retinopathy, retinal pigmentation changes (typically bull’s
eye appearance), visual field defects
(paracentral scotomas), macular degeneration, corneal edema, corneal
opacities, decreased dark adaptation
- Gastrointestinal disorders: Nausea, vomiting, diarrhea, abdominal pain
- General disorders: Fatigue
- Hepatobiliary disorders: Abnormal liver function tests, fulminant hepatic
failure
- Immune system disorders: Urticaria, angioedema, bronchospasm
- Metabolism and nutrition disorders: Anorexia, hypoglycemia, weight loss
- Musculoskeletal and connective tissue disorders: Proximal myopathy,
depressed tendon reflexes, abnormal
nerve conduction
- Nervous system disorders: Ataxia, dizziness, headache, seizure,
extrapyramidal disorders (dystonia, dyskinesia,
tremor)
- Neuropsychiatric disorders: Affect/emotional lability, irritability,
nervousness, psychosis, suicidal ideation, suicidal
behavior, depression, hallucinations, anxiety, agitation, confusion,
delusions, paranoia, mania and sleep disorders
(insomnia, night terrors, nightmares)
- Skin and subcutaneous tissue disorders: Alopecia, hair color changes, rash,
pruritus, photosensitivity, psoriasis
exacerbation, hyperpigmentation, exfoliative dermatitis, erythema multiforme,
acute generalized exanthematous
pustulosis, Drug Rash with Eosinophilia and Systemic Symptoms (DRESS
syndrome), Stevens-Johnson
syndrome (SJS), toxic epidermal necrolysis (TEN)
The most common adverse reactions reported are: nausea, vomiting, diarrhea, and abdominal pain. (6) (6)
To report SUSPECTED ADVERSE REACTIONS, contact Zydus Pharmaceuticals (USA)
Inc. at 1-877-993-8779 or FDA at
** 1-800-FDA-1088 or www.fda.gov/medwatch.** (6)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Drugs Prolonging QT Interval and Other Arrhythmogenic Drugs
Hydroxychloroquine sulfate prolongs the QT interval. There may be an increased
risk of inducing ventricular
arrhythmias if hydroxychloroquine sulfate is used concomitantly with other
arrhythmogenic drugs. Therefore,
hydroxychloroquine sulfate is not recommended in patients taking other drugs
that have the potential to prolong the QT
interval or are arrhythmogenic [see Warnings and Precautions (5.1].
7.2 Insulin or Other Antidiabetic Drugs
Hydroxychloroquine sulfate may enhance the effects of insulin and antidiabetic
drugs, and consequently increase the
hypoglycemic risk. Therefore, a decrease in dosage of insulin and other
antidiabetic drugs may be necessary [see Warnings and Precautions (5.10)] .
7.3 Drugs that Lower the Seizure Threshold
Hydroxychloroquine sulfate can lower the seizure threshold. Co-administration
of hydroxychloroquine sulfate with other
antimalarials known to lower the seizure threshold (e.g., mefloquine) may
increase the risk of seizures.
7.4 Antiepileptics
The activity of antiepileptic drugs might be impaired if co-administered with hydroxychloroquine sulfate.
7.5 Methotrexate
Concomitant use of hydroxychloroquine sulfate and methotrexate may increase the incidence of adverse reactions.
7.6 Cyclosporine
An increased plasma cyclosporin level was reported when cyclosporin and
hydroxychloroquine sulfate were
co-administered. Monitor serum cyclosporine levels closely in patients
receiving combined therapy.
7.7 Digoxin
Concomitant hydroxychloroquine sulfate and digoxin therapy may result in
increased serum digoxin levels. Monitor
serum digoxin levels closely in patients receiving combined therapy.
7.8 Cimetidine
Concomitant use of cimetidine resulted in a 2-fold increase of exposure of
chloroquine, which is structurally related to
hydroxychloroquine. Interaction of cimetidine with hydroxychloroquine cannot
be ruled out. Avoid concomitant use of
cimetidine.
7.9 Rifampicin
Lack of efficacy of hydroxychloroquine was reported when rifampicin was
concomitantly administered. Avoid
concomitant use of rifampicin.
7.10 Praziquantel
Chloroquine has been reported to reduce the bioavailability of praziquantel.
Interaction of praziquantel with
hydroxychloroquine cannot be ruled out.
7.11 Antacids and kaolin
Antacids and kaolin can reduce absorption of chloroquine; an interval of at
least 4 hours between intake of these
agents and chloroquine should be observed. Interaction of antacids and kaolin
with hydroxychloroquine cannot be
ruled out.
7.12 Ampicillin
In a study of healthy volunteers, chloroquine significantly reduced the
bioavailability of ampicillin. Interaction of
ampicillin with hydroxychloroquine cannot be ruled out.
• Drugs Prolonging QT Interval and Other Arrhythmogenic Drugs. (7.1)
• See FPI for more important drug interactions. (7) (7)
See 17 for PATIENT COUNSELING INFORMATION. Revised: 02/2024 (7)
REFERENCES SECTION
15 REFERENCES
1 Center for Disease Control and Prevention. Malaria.
https://www.cdc.gov/parasites/malaria/index.html
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
Warnings and Precautions, Risks Associated with Use in Porphyria (5.5) 07/2023
Warnings and Precautions, Neuropsychiatric Reactions Including Suicidality
(5.9) 07/2023
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Administer hydroxychloroquine sulfate tablet orally with food or milk. Do not crush or divide the tablets.
2.2 Dosage for Malaria in Adult and Pediatric Patients
Hydroxychloroquine sulfate is not recommended in pediatric patients less than
31 kg because the lowest available
strength (200 mg) exceeds the recommended dose for these patients and it
cannot be divided.
Prophylaxis
Treatment must start 2 weeks before travel to an endemic area. Advise the
patient to take the prophylaxis dosage once
a week, staring 2 weeks prior to travel to the endemic area, on the same day
every week, continuing the same weekly
dose while in the endemic area, and for 4 weeks after leaving the endemic
area. The recommended prophylaxis
dosage is:
• Adult patients: 400 mg once a week
• Pediatric patients ≥ 31kg: 6.5 mg/kg actual body weight (up to 400 mg) once
a week
Treatment of Uncomplicated Malaria
The dosages for the treatment of uncomplicated malaria are:
• Adult patients: Administer 800 mg initially; subsequently administer 400 mg
at 6 hours, 24 hours, and 48 hours
after the initial dose (total dosage = 2,000 mg).
• Pediatric patients ≥ 31 kg: Administer 13 mg/kg (up to 800 mg) initially;
subsequently administer 6.5 mg/kg (up
to 400 mg) at 6 hours, 24 hours, and 48 hours after the initial dose (total
dosage = 31 mg/kg - up to 2,000 mg).
For radical cure of P. vivax and P. ovale infections, concomitant therapy with
an 8-aminoquinoline drug is necessary
[see Microbiology (12.4)].
2.3 Dosage for Rheumatoid Arthritis in Adults
The recommended dosage is:
• Initial dosage: 400 mg to 600 mg daily as a single daily dose or two divided
doses. The action of
hydroxychloroquine is cumulative and may require weeks to months for maximum
therapeutic effect. Daily
doses exceeding 5 mg/kg (actual weight) of hydroxychloroquine sulfate increase
the incidence of retinopathy
[see Warnings and Precautions (5.2)].
• Chronic dosage: 200 mg once daily to 400 mg daily, as a single dose or two
divided doses.
Corticosteroids, salicylates, and other antirheumatic agents may be used
concomitantly with hydroxychloroquine
sulfate.
2.4 Dosage for Systemic Lupus Erythematosus in Adults
The recommended dosage is 200 mg given once daily, or 400 mg given once daily or in two divided doses.
2.5 Dosage for Chronic Discoid Lupus Erythematosus in Adults
The recommended dosage is 200 mg given once daily, or 400 mg given once daily or in two divided doses.
Malaria in Adult and Pediatric Patients (2.2): (2)
• Prophylaxis: Begin weekly doses 2 weeks prior to travel to the endemic area,
continue weekly doses while in the
endemic area, and continue the weekly doses for 4 weeks after leaving the
endemic area:
- Adults: 400 mg once a week
- Pediatric patients ≥ 31 kg: 6.5 mg/kg up to 400 mg, once a week (2)
• Treatment of Uncomplicated Malaria: See Full Prescribing Information (FPI) for complete dosing information. (2)
(2)
(2)
(2)
(2)
Rheumatoid Arthritis in Adults (2.3): (2)
• Initial dosage: 400 mg to 600 mg daily
• Chronic dosage: 200 mg once daily or 400 mg once daily (or in two divided
doses) (2)
Systemic Lupus Erythematosus in Adults (2.4): (2)
• 200 mg once daily or 400 mg once daily (or in two divided doses) (2)
Chronic Discoid Lupus Erythematosus in Adults (2.5): (2)
• 200 mg once daily or 400 mg once daily (or in two divided doses) (2)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Tablets: 200 mg of hydroxychloroquine sulfate, white to off-white, capsule-
shaped, biconvex, film-coated tablets
debossed with “ZC38” on one side and plain on other side.
Tablets: 200 mg of hydroxychloroquine sulfate (3) (3)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in
women exposed to hydroxychloroquine
sulfate during pregnancy. Encourage patients to register by contacting
1-877-311-8972.
Risk Summary
Prolonged clinical experience over decades of use and available data from
published epidemiologic and clinical studies
with hydroxychloroquine sulfate use in pregnant women have not identified a
drug-associated risk of major birth
defects, miscarriage, or adverse maternal, or fetal outcomes (see Data). There
are risks to the mother and fetus
associated with untreated or increased disease activity from malaria,
rheumatoid arthritis, and systemic lupus
erythematosus in pregnancy (see Clinical Considerations). Animal reproduction
studies were not conducted with
hydroxychloroquine.
The estimated background risk of major birth defects and miscarriage for the
indicated populations is unknown. All
pregnancies have a background risk of birth defect, loss, or other adverse
outcomes. In the US general population, the
estimated background risk of major birth defects and miscarriage in clinically
recognized pregnancies is 2% to 4% and
15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo-Fetal Risk
Malaria: Malaria during pregnancy increases the risk for adverse pregnancy
outcomes, including maternal anemia,
prematurity, spontaneous abortion, and stillbirth.
Rheumatoid Arthritis: Published data suggest that increased disease activity
is associated with the risk of developing
adverse pregnancy outcomes in women with rheumatoid arthritis Adverse
pregnancy outcomes include preterm
delivery (before 37 weeks of gestation), low birth weight (less than 2,500 g)
infants, and small for gestational age at
birth.
Systemic Lupus Erythematosus: Pregnant women with systemic lupus
erythematosus, especially those with increased
disease activity, are at increased risk of adverse pregnancy outcomes,
including spontaneous abortion, fetal death,
preeclampsia, preterm birth, and intrauterine growth restriction. Passage of
maternal auto-antibodies across the
placenta may result in neonatal illness, including neonatal lupus and
congenital heart block.
Data
Human Data
Data from published epidemiologic and clinical studies have not established an
association with hydroxychloroquine
sulfate use during pregnancy and major birth defects, miscarriage, or adverse
maternal or fetal outcomes.
Hydroxychloroquine readily crosses the placenta with cord blood levels
corresponding to maternal plasma levels. No
retinal toxicity, ototoxicity, cardiotoxicity, or growth and developmental
abnormalities have been observed in children
who were exposed to hydroxychloroquine in utero. Available epidemiologic and
clinical studies have methodological
limitations including small sample size and study design.
8.2 Lactation
Risk Summary
Published lactation data report that hydroxychloroquine is present in human
milk at low levels. No adverse reactions
have been reported in breastfed infants. No retinal toxicity, ototoxicity,
cardiotoxicity, or growth and developmental
abnormalities have been observed in children who were exposed to
hydroxychloroquine through breastmilk. There is
no information on the effect of hydroxychloroquine on milk production. The
developmental and health benefits of
breastfeeding should be considered along with the mother’s clinical need for
hydroxychloroquine sulfate and any
potential adverse effects on the breastfed child from hydroxychloroquine
sulfate or from the underlying maternal
condition.
8.4 Pediatric Use
The safety and effectiveness of hydroxychloroquine sulfate have been
established in pediatric patients for the
treatment of uncomplicated malaria due to P. falciparum, P. malariae, P.
vivax, and P. ovale, as well as for the
prophylaxis of malaria in geographic areas where chloroquine resistance is not
reported. However, this product cannot
be directly administered to pediatric patients weighing less than 31 kg
because the film-coated tablets cannot be
crushed or divided [see Dosage and Administration (2.1, 2.2)].
The safety and effectiveness of hydroxychloroquine sulfate have not been
established in pediatric patients for the
treatment of rheumatoid arthritis, chronic discoid lupus erythematosus, or
systemic lupus erythematosus.
8.5 Geriatric Use
Clinical trials of hydroxychloroquine sulfate did not include sufficient
numbers of patients 65 years of age and older to
determine whether they respond differently from younger adult patients.
Nevertheless, this drug is known to be
substantially excreted by the kidney, and the risk of toxic reactions to this
drug may be greater in patients with
impaired renal function. In general, dose selection in geriatric patients
should start with the lowest recommended
dose, taking into consideration the greater frequency of decreased hepatic,
renal or cardiac function, and of
concomitant disease or other drug therapy.
8.6 Patients with Renal or Hepatic Disease
A reduction in the dosage of hydroxychloroquine sulfate may be necessary in patients with hepatic or renal disease.
OVERDOSAGE SECTION
10 OVERDOSAGE
Hydroxychloroquine sulfate overdosage symptoms have an onset within 1 hour to
3 hours of ingestion. The following
have been reported with hydroxychloroquine sulfate overdosage:
• Cardiovascular toxicity, including QRS or QTc prolongation, ventricular
tachycardia, ventricular fibrillation,
torsade de pointes, atrioventricular block, cardiac arrest and death.
• Life-threatening hypotension is common.
• Severe hypokalemia secondary to an intracellular shift is common in severe
toxicity.
• Central nervous system (CNS) depression, seizures, visual disturbances,
transient blindness, and coma may occur.
Gastrointestinal decontamination procedures warrant consideration in patients
that present within the first hour
post-ingestion. If the level of consciousness rapidly deteriorates in severe
poisoning, consider intubation before
gastrointestinal decontamination procedures. Monitor plasma potassium levels
and manage accordingly.
Hemofiltration, hemodialysis, and hemoperfusion are not of benefit.
Consider contacting a poison center (1-800-221-2222) or a medical toxicologist
for overdosage management
recommendations.
DESCRIPTION SECTION
11 DESCRIPTION
Hydroxychloroquine sulfate tablet, USP is an antimalarial and antirheumatic
drug, chemically described as
2-[[4-[(7-Chloro-4-quinolyl) amino]pentyl] ethylamino] ethanol sulfate (1:1)
with the molecular formula
C18H26ClN3O•H2SO4. The molecular weight of hydroxychloroquine sulfate is
433.95. Its structural formula is:
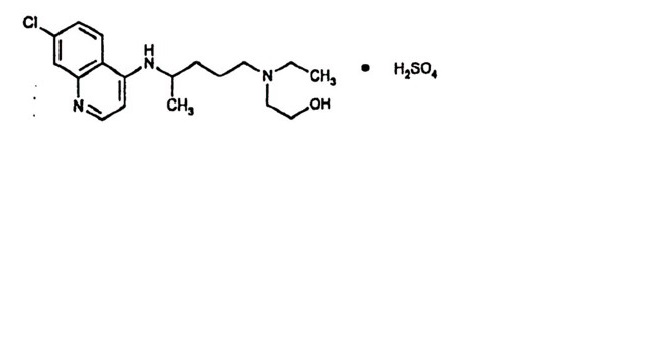
Hydroxychloroquine sulfate is a white or practically white, crystalline
powder, freely soluble in water; practically
insoluble in alcohol, chloroform, and in ether.
Each hydroxychloroquine sulfate tablet intended for oral administration
contains 200 mg of hydroxychloroquine sulfate,
USP equivalent to 155 mg base. In addition, each tablet contains the following
inactive ingredients: dibasic calcium
phosphate dihydrate, magnesium stearate, pregelatinized starch, polyethylene
glycol, polyvinyl alcohol, starch, talc and
titanium dioxide.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Malaria
Hydroxychloroquine is a 4-aminoquinoline antimalarial [see Microbiology (12.4)] and antirheumatic agent.
Rheumatoid Arthritis, Systemic Lupus Erythematosus and Chronic Discoid
Lupus
Erythematosus
The mechanisms underlying the anti-inflammatory and immunomodulatory effects
of hydroxychloroquine sulfate in the
treatment of rheumatoid arthritis, chronic discoid lupus erythematosus and
systemic lupus erythematosus are not fully
known.
12.2 Pharmacodynamics
The exposure-response relationship and time course of pharmacodynamic response
for the safety and effectiveness of
hydroxychloroquine have not been fully characterized.
12.3 Pharmacokinetics
Following oral administration, the whole blood concentration of
hydroxychloroquine at steady state is dose proportional
over a dose range from 200 mg daily to 400 mg daily of hydroxychloroquine in
rheumatoid arthritis and lupus patients.
Absorption
Following a single 200 mg oral dose of hydroxychloroquine sulfate to healthy
male volunteers, whole blood
hydroxychloroquine C was 129.6 ng/mL (plasma C was 50.3 ng/mL) with T of 3.3
hours (plasma T 3.7 hours). Peak
blood concentrations of metabolites were observed at the same time as peak
levels of hydroxychloroquine. Mean
absolute oral bioavailability is 79% (SD: 12%) in fasting conditions.
Peak blood concentrations ranged from 1,161 ng/mL to 2,436 ng/mL (mean 1,918
ng/mL) following a single dose of
155 mg intravenous infusion and from 2290 ng/mL to 4,211 ng/mL (mean 3,312
ng/mL) following a single dose of
310 mg intravenous infusion in healthy subjects. Pharmacokinetic parameters
were not significantly different over the
therapeutic dose range of 155 mg and 310 mg, indicating linear kinetics.
In patients with rheumatoid arthritis, there was large variability as to the
fraction of the dose absorbed (i.e. 30% to
100%), and mean hydroxychloroquine levels were significantly higher in
patients with less disease activity.
Distribution
Hydroxychloroquine sulfate is extensively distributed to tissues and has a
large volume of distribution. Approximately
50% of hydroxychloroquine is bound to plasma proteins.
Metabolism
Significant levels of three metabolites, desethylhydroxychloroquine (DHCQ),
desethylchloroquine (DCQ), and
bidesethylhydroxychloroquine (BDCQ) were found in plasma and blood, with DHCQ
being the major metabolite. In vitro,
hydroxychloroquine is metabolized mainly by CYP2C8, CYP3A4 and CYP2D6 as well
as by FMO-1 and MAO-A
Elimination/Excretion
Renal clearance in patients with rheumatoid arthritis treated with hydroxychloroquine sulfate for at least 6 months was similar to that in single dose studies in healthy volunteers, suggesting that no change in clearance occurred with chronic dosing. Renal clearance of unchanged hydroxychloroquine was approximately 16% to 30% of the dose after oral and IV administration. Results following a single oral dose of a 200 mg tablet demonstrated a half- life of hydroxychloroquine about 40 days in whole blood. Following chronic oral administration of hydroxychloroquine, the absorption half-life of hydroxychloroquine was approximately 3 to 4 hours and the terminal half-life ranged from 40 to 50 days in whole blood. The effective half-life of hydroxychloroquine is likely to be shorter and steady state is achieved by 6 weeks following 400 mg daily oral administration in rheumatoid arthritis patients.
Drug Interaction Studies
In vitro study suggested that hydroxychloroquine has a potential to inhibit
CYP2D6, CYP3A4, P- glycoproteins (P-gp),
MATE1 and MATE2-K.
In vitro study suggested that hydroxychloroquine has no significant potential
to inhibit CYP1A2, CYP2B6, CYP2C8,
CYP2C9, CYP2C19, and the main transporters OATP1B1, OATP1B3, OAT1, OAT3, OCT1,
and OCT2. In vitro,
hydroxychloroquine has no significant potential to induce CYP1A2, CYP2B6 and
CYP3A4.
12.4 Microbiology
Mechanism of Action in Malaria
The precise mechanism by which hydroxychloroquine exhibits activity against
Plasmodium is not known.
Hydroxychloroquine is a weak base and may exert its effect by concentrating in
the acid vesicles of the parasite and
inhibiting polymerization of heme. It can also inhibit certain enzymes by its
interaction with DNA.
Antimicrobial Activity
Hydroxychloroquine is active against the erythrocytic forms of chloroquine
sensitive strains of P. falciparum, P.
malariae, P. vivax, and P. ovale. Hydroxychloroquine is not active against the
gametocytes and exoerythrocytic forms
including the hypnozoite liver stage forms of P. vivax and P. ovale.
Drug Resistance
P. falciparum strains exhibiting reduced susceptibility to chloroquine also
show reduced susceptibility to
hydroxychloroquine. Resistance of Plasmodium parasites to chloroquine is
widespread [see Indications and Usage (1.1)].
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or genotoxicity studies have been conducted with
hydroxychloroquine. No animal studies have been
performed to evaluate the potential effects of hydroxychloroquine on
reproduction or development, or to determine
potential effects on fertility in males or females.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Hydroxychloroquine sulfate Tablets, USP contain 200 mg of hydroxychloroquine
sulfate, USP (equivalent to 155 mg
base). White to off-white, capsule-shaped, biconvex, film-coated tablets
debossed with “ZC38” on one side and plain
on other side, and are supplied as follows:
• Boxes of 10 x 10 UD 100 NDC 63739-777-10
16.2 Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP/NF. Keep
out of the reach of children.
PATIENT COUNSELING INFORMATION
17 PATIENT COUNSELING INFORMATION
Important Administration Instructions
Advise the patient to take hydroxychloroquine sulfate tablet with food or milk and not to crush or divide the tablet.
Cardiomyopathy and Ventricular Arrhythmias
Inform the patient that serious cardiac effects, life-threatening and fatal
cases have been reported with use of
hydroxychloroquine sulfate. Advise patients to seek medical attention
immediately if they experience any symptoms of
heart rhythm changes including fast or irregular heartbeat, lightheadedness,
dizziness, or syncope [see Warnings and Precautions (5.1)].
Retinal Toxicity
Inform the patient that irreversible retinal damage has been observed in some
patients with the use of
hydroxychloroquine sulfate. Advise patients of the importance of the
ophthalmology visits for monitoring their eyes.
Instruct patients to seek medical attention promptly if they experience
decreased vision or decreased dark adaptation
[see Warnings and Precautions (5.2)].
Serious Skin Reactions
Inform the patient that severe, life-threatening skin reactions have been
reported with the use of hydroxychloroquine
sulfate. Advise the patient to seek medical attention immediately if
experiencing any of the following signs and
symptoms: blisters on the skin, eyes, lips or in the mouth, itching or
burning, with or without fever [see Warnings and Precautions (5.3)].
Hepatotoxicity Associated with Porphyria Cutanea Tarda
Inform the patient that liver toxicity has been reported in when
hydroxychloroquine sulfate was used in patients with
porphyria cutanea tarda. In some cases, PCT was diagnosed only after the
occurrence of liver injury, when
hydroxychloroquine sulfate was prescribed for an approved indication. Advise
the patient to seek medical attention if
experiencing fatigue, rash, nausea, dark urine, or jaundice [see Warnings and Precautions (5.5)].
Skeletal Muscle Myopathy or Neuropathy
Inform the patient that muscle weakness and atrophy has been reported with
hydroxychloroquine sulfate use Advise
patients to report to the physician symptoms of muscle weakness [see Warnings and Precautions (5.8)].
Neuropsychiatric Reactions Including Suicidality
Alert patients to seek medical attention immediately if they experience new or
worsening depression, suicidal
thoughts, or other mood changes [see Warnings and Precautions (5.9)].
Hypoglycemia
Inform the patient that hydroxychloroquine sulfate has been associated with
severe hypoglycemia. Advise the patient
to monitor blood sugar levels if possible and to seek medical attention if
experiencing any of the signs and symptoms
of hypoglycemia such as sweating, shakiness, weakness, dizziness, tachycardia,
nausea, blurred vision, confusion,
fainting, or loss of consciousness [see Warnings and Precautions (5.10)].
Pregnancy
Inform the patient that there is a pregnancy registry that monitors pregnancy
outcomes in women exposed to
hydroxychloroquine sulfate during pregnancy. Encourage patients to register by
contacting 1-877-311-8972 [see Use in Specific Populations (8.1)].
Manufactured by:
** Zydus Lifesciences Ltd.**
India
Distributed by:
McKesson Corporation dba SKY Packaging
Memphis, TN 38141
February 2024
21415-2
