Registrants1
Companies and organizations registered with the FDA for this drug approval, including their contact information and regulatory details.
171714327
Manufacturing Establishments1
FDA-registered manufacturing facilities and establishments involved in the production, packaging, or distribution of this drug product.
Bryant Ranch Prepack
Bryant Ranch Prepack
171714327
Products1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
LORYNA
Product Details
Drug Labeling Information
Complete FDA-approved labeling information including indications, dosage, warnings, contraindications, and other essential prescribing details.
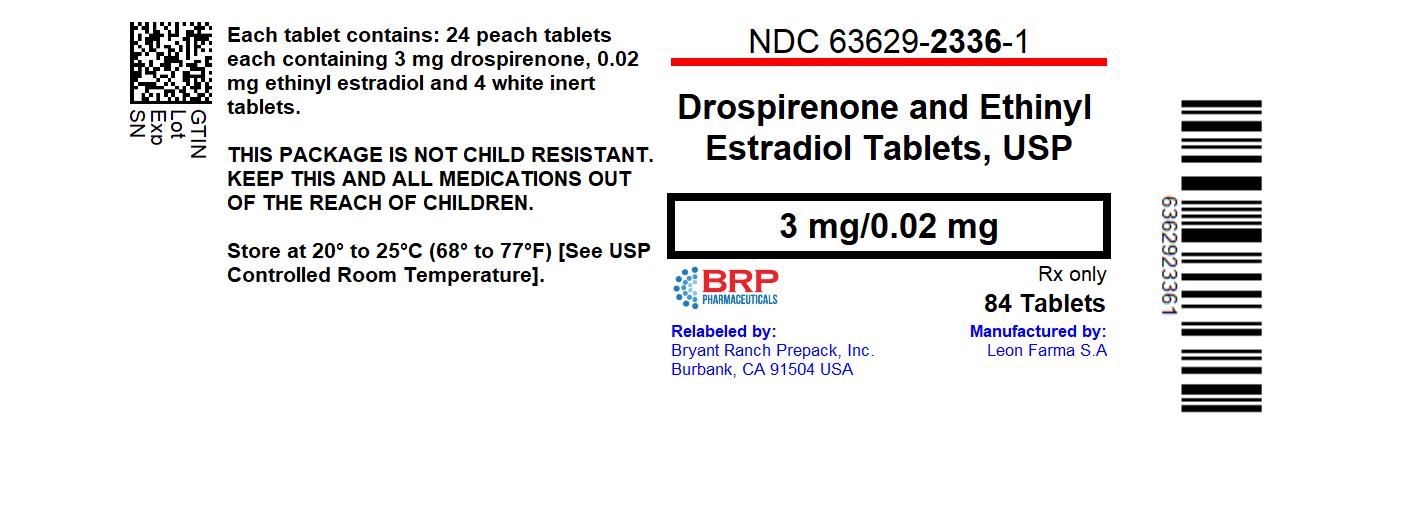
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Drospirenone Estradiol Est Tab, #84
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
Warnings and Precautions (5.3) 4/2022
DESCRIPTION SECTION
11 DESCRIPTION
Loryna (drospirenone and ethinyl estradiol tablets, USP) provides an oral contraceptive regimen consisting of 24 peach active film-coated tablets each containing 3 mg of drospirenone and 0.02 mg of ethinyl estradiol and 4 white inert film coated tablets.
Each active tablet consists of black iron oxide, croscarmellose sodium, lactose fast flo, polyethylene glycol, magnesium stearate, polysorbate 80, polyvinyl alcohol, povidone K-30, pregelatinized starch, talc, titanium dioxide, red iron oxide, yellow iron oxide.
The inert tablet consists of andydrous lactose, magnesium stearate, povidone K-30, polyethylene glycol, polyvinyl alcohol-part hydrolyzed, talc and titanium dioxide.
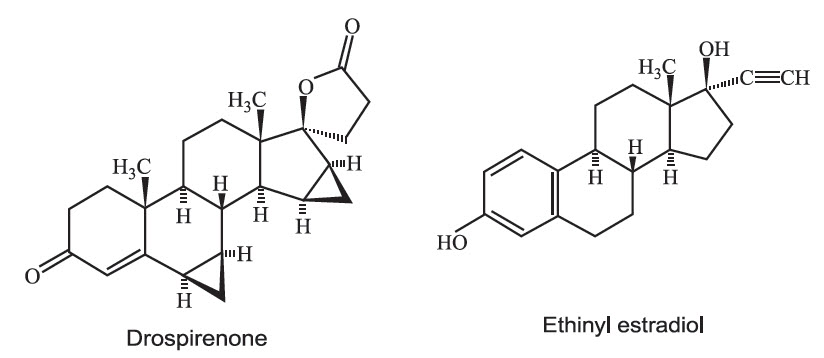
Drospirenone (6R,7R,8R,9S,10R,13S,14S,15S,16S,17S)-1,3’,4’,6,6a,7,8,9,10,11,12,13,14,15,15a,16-hexadecahydro-10,13-dimethylspiro-[17H-dicyclopropa- [6,7:15,16] cyclopenta[a]phenanthrene-17,2’(5H)-furan]-3,5’(2H)-dione) is a synthetic progestational compound and has a molecular weight of 366.5 and a molecular formula of C24H30O3.
Ethinyl estradiol (19-nor-17α-pregna 1,3,5(10)-triene-20-yne-3, 17-diol) is a synthetic estrogenic compound and has a molecular weight of 296.4 and a molecular formula of C20H24O2.
The structural formulas are as follows:
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
COCs lower the risk of becoming pregnant primarily by suppressing ovulation. Other possible mechanisms may include cervical mucus changes that inhibit sperm penetration and the endometrial changes that reduce the likelihood of implantation.
12.2 Pharmacodynamics
Drospirenone is a spironolactone analogue with anti-mineralocorticoid and antiandrogenic activity. The estrogen in drospirenone and ethinyl estradiol is ethinyl estradiol.
Contraception
Two studies evaluated the effect of 3 mg DRSP / 0.02 mg EE combinations on the suppression of ovarian activity as assessed by measurement of follicle size via transvaginal ultrasound and serum hormone (progesterone and estradiol) analyses during two treatment cycles (21-day active tablet period plus 7-day pill-free period). More than 90% of subjects in these studies demonstrated ovulation inhibition. One study compared the effect of 3 mg DRSP/0.02 mg EE combinations with two different regimens (24-day active tablet period plus 4-day pill-free period vs. 21-day active tablet period plus 7-day pill-free period) on the suppression of ovarian activity during two treatment cycles. During the first treatment cycle, there were no subjects (0/49, 0%) taking the 24-day regimen who ovulated compared to 1 subject (1/50, 2%) using the 21-day regimen. After intentionally introduced dosing errors (3 missed active tablets on Days 1 to 3) during the second treatment cycle, there was 1 subject (1/49, 2%) taking the 24-day regimen who ovulated compared to 4 subjects (4/50, 8%) using the 21-day regimen.
Acne
Acne vulgaris is a skin condition with a multifactorial etiology including androgen stimulation of sebum production. While the combination of EE and DRSP increases sex hormone binding globulin (SHBG) and decreases free testosterone, the relationship between these changes and a decrease in the severity of facial acne in otherwise healthy women with this skin condition has not been established. The impact of the antiandrogenic activity of DRSP on acne is not known.
12.3 Pharmacokinetics
Absorption
The absolute bioavailability of DRSP from a single entity tablet is about 76%. The absolute bioavailability of EE is approximately 40% as a result of presystemic conjugation and first-pass metabolism. The absolute bioavailability of drospirenone and ethinyl estradiol, which is a combination tablet of DRSP and EE stabilized by betadex as a clathrate (molecular inclusion complex), has not been evaluated. The bioavailability of EE is similar when dosed via a betadex clathrate formulation compared to when it is dosed as a free steroid. Serum concentrations of DRSP and EE reached peak levels within 1 to 2 hours after administration of drospirenone and ethinyl estradiol.
The pharmacokinetics of DRSP are dose proportional following single doses ranging from 1 to 10 mg. Following daily dosing of drospirenone and ethinyl estradiol, steady state DRSP concentrations were observed after 8 days. There was about 2 to 3 fold accumulation in serum Cmax and AUC (0–24h) values of DRSP following multiple dose administration of drospirenone and ethinyl estradiol (seeTable 2).
For EE, steady-state conditions are reported during the second half of a treatment cycle. Following daily administration of drospirenone and ethinyl estradiol, serum Cmax and AUC (0–24h) values of EE accumulate by a factor of about 1.5 to 2 (seeTable 2).
TABLE 2: Pharmacokinetic Parameters of Drospirenone and Ethinyl Estradiol (DRSP 3 mg and EE 0.02 mg)|
DRSP | |||||
|
Cycle / Day |
No. of Subjects |
C** maxa(ng/mL)** |
Tmaxb (h) |
AUC(0–24h)a(ng•h/mL) |
t1/2a (h) |
|
1/1 |
23 |
38.4 (25) |
1.5 (1–2) |
268 (19) |
NAc |
|
1/21 |
23 |
70.3 (15) |
1.5 (1–2) |
763 (17) |
30.8 (22) |
|
EE | |||||
|
Cycle / Day |
No. of Subjects |
C**** max****a** (pg/mL)** |
Tmaxb (h) |
AUC(0–24h)a (pg•h/mL) |
t1/2a (h) |
|
1/1 |
23 |
32.8 (45) |
1.5 (1–2) |
108 (52) |
NAc |
|
1/21 |
23 |
45.1 (35) |
1.5 (1–2) |
220 (57) |
NA c |
a) geometric mean (geometric coefficient of variation)
b) median (range)
c) NA = Not available
Food Effect
The rate of absorption of DRSP and EE following single administration of a formulation similar to drospirenone and ethinyl estradiol was slower under fed (high fat meal) conditions with the serum Cmax being reduced about 40% for both components. The extent of absorption of DRSP, however, remained unchanged. In contrast, the extent of absorption of EE was reduced by about 20% under fed conditions.
Distribution
DRSP and EE serum concentrations decline in two phases. The apparent volume of distribution of DRSP is approximately 4 L/kg and that of EE is reported to be approximately 4 to 5 L/kg.
DRSP does not bind to SHBG or corticosteroid binding globulin (CBG) but binds about 97% to other serum proteins.
Multiple dosing over 3 cycles resulted in no change in the free fraction (as measured at trough concentrations). EE is reported to be highly but non- specifically bound to serum albumin (approximately 98.5 %) and induces an increase in the serum concentrations of both SHBG and CBG. EE induced effects on SHBG and CBG were not affected by variation of the DRSP dosage in the range of 2 to 3 mg.
Metabolism
The two main metabolites of DRSP found in human plasma were identified to be the acid form of DRSP generated by opening of the lactone ring and the 4,5-dihydrodrospirenone-3-sulfate, formed by reduction and subsequent sulfation. These metabolites were shown not to be pharmacologically active. Drospirenone is also subject to oxidative metabolism catalyzed by CYP3A4.
EE has been reported to be subject to significant gut and hepatic first-pass metabolism. Metabolism of EE and its oxidative metabolites occur primarily by conjugation with glucuronide or sulfate. CYP3A4 in the liver is responsible for the 2-hydroxylation which is the major oxidative reaction. The 2-hydroxy metabolite is further transformed by methylation and glucuronidation prior to urinary and fecal excretion.
Excretion
DRSP serum concentrations are characterized by a terminal disposition phase half-life of approximately 30 hours after both single and multiple dose regimens. Excretion of DRSP was nearly complete after ten days and amounts excreted were slightly higher in feces compared to urine. DRSP was extensively metabolized and only trace amounts of unchanged DRSP were excreted in urine and feces. At least 20 different metabolites were observed in urine and feces. About 38 to 47% of the metabolites in urine were glucuronide and sulfate conjugates. In feces, about 17 to 20% of the metabolites were excreted as glucuronides and sulfates.
For EE the terminal disposition phase half-life has been reported to be approximately 24 hours. EE is not excreted unchanged. EE is excreted in the urine and feces as glucuronide and sulfate conjugates and undergoes enterohepatic circulation.
Use in Specific Populations
Pediatric Use: Safety and efficacy of drospirenone and ethinyl estradiol have been established in women of reproductive age. Efficacy is expected to be the same for postpubertal adolescents under the age of 18 and for users 18 years and older. Use of this product before menarche is not indicated.
Geriatric Use: Drospirenone and ethinyl estradiol have not been studied in postmenopausal women and are not indicated in this population.
Race: No clinically significant difference was observed between the pharmacokinetics of DRSP or EE in Japanese versus Caucasian women (age 25 to 35) when 3mg DRSP/0.02 mg EE was administered daily for 21 days. Other ethnic groups have not been specifically studied.
**Renal Impairment:**Drospirenone and ethinyl estradiol are contraindicated in patients with renal impairment.
The effect of renal impairment on the pharmacokinetics of DRSP (3 mg daily for 14 days) and the effect of DRSP on serum potassium concentrations were investigated in three separate groups of female subjects (n=28, age 30 to 65). All subjects were on a low potassium diet. During the study, 7 subjects continued the use of potassium-sparing drugs for the treatment of their underlying illness. On the 14th day (steady-state) of DRSP treatment, the serum DRSP concentrations in the group with CLcr of 50 to 79 mL/min were comparable to those in the control group with CLcr ≥ 80 mL/min. The serum DRSP concentrations were on average 37% higher in the group with CLcr of 30 to 49 mL/min compared to those in the control group. DRSP treatment did not show any clinically significant effect on serum potassium concentration. Although hyperkalemia was not observed in the study, in five of the seven subjects who continued use of potassium-sparing drugs during the study, mean serum potassium concentrations increased by up to 0.33 mEq/L. [See CONTRAINDICATIONS (4),and WARNINGS AND PRECAUTIONS (5.2)]
Hepatic Impairment: Drospirenone and ethinyl estradiol are contraindicated in patients with hepatic disease.
The mean exposure to DRSP in women with moderate liver impairment is approximately three times higher than the exposure in women with normal liver function. Drospirenone and ethinyl estradiol have not been studied in women with severe hepatic impairment. [seeCONTRAINDICATIONS (4), and WARNINGS AND PRECAUTIONS (5.4)]
Drug Interactions
Consult the labeling of all concurrently used drugs to obtain further information about interactions with oral contraceptives or the potential for enzyme alterations.
Effects of Other Drugs on Combined Oral Contraceptives
Substances diminishing the efficacy of COCs: Drugs or herbal products that induce certain enzymes, including CYP3A4, may decrease the effectiveness of COCs or increase breakthrough bleeding.
Substances increasing the plasma concentrations of COCs: Co-administration of atorvastatin and certain COCs containing ethinyl estradiol increase AUC values for ethinyl estradiol by approximately 20%. Ascorbic acid and acetaminophen may increase plasma ethinyl estradiol concentrations, possibly by inhibition of conjugation. In a clinical drug-drug interaction study conducted in 20 premenopausal women, co-administration of a DRSP (3 mg)/ ethinyl estradiol (0.02 mg) COC with the strong CYP3A4 inhibitor ketoconazole (200 mg twice daily) for 10 days increased the AUC(0-24h) of DRSP and ethinyl estradiol by 2.68-fold (90% CI: 2.44, 2.95) and 1.40-fold (90% CI: 1.31, 1.49), respectively. The increases in Cmax were 1.97-fold (90% CI: 1.79, 2.17) and 1.39-fold (90% CI: 1.28, 1.52) for DRSP and ethinyl estradiol, respectively. Although no clinically relevant effects on safety or laboratory parameters including serum potassium were observed, this study only assessed subjects for 10 days. The clinical impact for a patient taking a DRSP- containing COC concomitantly with chronic use of a CYP3A4/5 inhibitor is unknown [seeWARNINGS AND PRECAUTIONS (5.2)].
**HIV/HCV protease inhibitors and non-nucleoside reverse transcriptase inhibitors:**Significant changes (increase or decrease) in the plasma concentrations of estrogen and progestin have been noted in some cases of co- administration with HIV/HCV protease inhibitors or with non-nucleoside reverse transcriptase inhibitors.
**Antibiotics:**There have been reports of pregnancy while taking hormonal contraceptives and antibiotics, but clinical pharmacokinetic studies have not shown consistent effects of antibiotics on plasma concentrations of synthetic steroids.
Effects of Combined Oral Contraceptives on Other Drugs
COCs containing ethinyl estradiol may inhibit the metabolism of other compounds. COCs have been shown to significantly decrease plasma concentrations of lamotrigine, likely due to induction of lamotrigine glucuronidation. This may reduce seizure control; therefore, dosage adjustments of lamotrigine may be necessary. Consult the labeling of the concurrently-used drug to obtain further information about interactions with COCs or the potential for enzyme alterations.
In vitro, ethinyl estradiol is a reversible inhibitor of CYP2C19, CYP1A1 and CYP1A2 as well as a mechanism-based inhibitor of CYP3A4/5, CYP2C8, and CYP2J2. Metabolism of DRSP and potential effects of DRSP on hepatic CYP enzymes have been investigated in in vitro and in vivo studies. In in vitro studies DRSP did not affect turnover of model substrates of CYP1A2 and CYP2D6, but had an inhibitory influence on the turnover of model substrates of CYP1A1, CYP2C9, CYP2C19 and CYP3A4, with CYP2C19 being the most sensitive enzyme. The potential effect of DRSP on CYP2C19 activity was investigated in a clinical pharmacokinetic study using omeprazole as a marker substrate. In the study with 24 postmenopausal women [including 12 women with homozygous (wild type) CYP2C19 genotype and 12 women with heterozygous CYP2C19 genotype] the daily oral administration of 3 mg DRSP for 14 days did not affect the oral clearance of omeprazole (40 mg, single oral dose) and the CYP2C19 product 5-hydroxy omeprazole. Furthermore, no significant effect of DRSP on the systemic clearance of the CYP3A4 product omeprazole sulfone was found. These results demonstrate that DRSP did not inhibit CYP2C19 and CYP3A4 in vivo.
Two additional clinical drug-drug interaction studies using simvastatin and midazolam as marker substrates for CYP3A4 were each performed in 24 healthy postmenopausal women. The results of these studies demonstrated that pharmacokinetics of the CYP3A4 substrates were not influenced by steady state DRSP concentrations achieved after administration of 3 mg DRSP/day.
Women on thyroid hormone replacement therapy may need increased doses of thyroid hormone because serum concentration of thyroid-binding globulin increases with use of COCs.
Interactions With Drugs That Have the Potential to Increase Serum Potassium Concentration
There is a potential for an increase in serum potassium concentration in women taking drospirenone and ethinyl estradiol with other drugs that may increase serum potassium concentration [seeWARNINGS AND PRECAUTIONS (5.2)].
A drug-drug interaction study of DRSP 3 mg/estradiol (E2) 1 mg versus placebo was performed in 24 mildly hypertensive postmenopausal women taking enalapril maleate 10 mg twice daily. Potassium concentrations were obtained every other day for a total of 2 weeks in all subjects. Mean serum potassium concentrations in the DRSP/E2 treatment group relative to baseline were 0.22 mEq/L higher than those in the placebo group. Serum potassium concentrations also were measured at multiple time points over 24 hours at baseline and on Day 14. On Day 14, the ratios for serum potassium Cmax and AUC in the DRSP/E2 group to those in the placebo group were 0.955 (90% CI: 0.914, 0.999) and 1.010 (90% CI: 0.944, 1.08), respectively. No patient in either treatment group developed hyperkalemia (serum potassium concentrations >5.5 mEq/L).
DOSAGE FORMS & STRENGTHS SECTION
Highlight: Loryna (drospirenone and ethinyl estradiol tablets) consists of 28 film-coated tablets in the following order (3):
•24 peach tablets, each containing 3 mg drospirenone (DRSP) and 0.02 mg ethinyl estradiol (EE)
•4 white inert tablets
3 DOSAGE FORMS AND STRENGTHS
Loryna (drospirenone and ethinyl estradiol tablets, USP) is available in blister packs.
Each blister pack (28 film-coated tablets) contains in the following order:
• 24 peach tablets each containing 3 mg drospirenone (DRSP) and 0.02 mg ethinyl estradiol (EE)
• 4 white inert tablets
CONTRAINDICATIONS SECTION
Highlight: * Renal impairment (4)
- Adrenal insufficiency (4)
- A high risk of arterial or venous thrombotic diseases (4)
- Undiagnosed abnormal uterine bleeding (4)
- Breast cancer or other estrogen- or progestin-sensitive cancer (4)
- Liver tumors or liver disease (4)
- Pregnancy (4)
- Co-administration with Hepatitis C drug combinations containing ombitasvir, paritaprevir/ritonavir, with or without dasabuvir (4)
4 CONTRAINDICATIONS
Loryna is contraindicated in females who are known to have or develop the following conditions:
- Renal impairment
- Adrenal insufficiency
- A high risk of arterial or venous thrombotic diseases. Examples include women who are known to:
- Smoke, if over age 35 [seeBOXED WARNING and WARNINGS AND PRECAUTIONS (5.1)]
- Have deep vein thrombosis or pulmonary embolism, now or in the past [see WARNINGS AND PRECAUTIONS (5.1)]
- Have cerebrovascular disease [seeWARNINGS AND PRECAUTIONS (5.1)]
- Have coronary artery disease [seeWARNINGS AND PRECAUTIONS (5.1)]
- Have thrombogenic valvular or thrombogenic rhythm diseases of the heart (for example, subacute bacterial endocarditis with valvular disease, or atrial fibrillation) [see** WARNINGS AND PRECAUTIONS (5.1)**]
- Have inherited or acquired hypercoagulopathies [see** WARNINGS AND PRECAUTIONS (5.1)**]
- Have uncontrolled hypertension [see** WARNINGS AND PRECAUTIONS (5.6)**]
- Have diabetes mellitus with vascular disease [seeWARNINGS AND PRECAUTIONS (5.8)]
- Have headaches with focal neurological symptoms or have migraine headaches with or without aura if over age 35 [seeWARNINGS AND PRECAUTIONS (5.9)]
- Undiagnosed abnormal uterine bleeding [seeWARNINGS AND PRECAUTIONS (5.10)]
- Current diagnosis of, or history of, breast cancer, which may be hormone-sensitive** [see WARNINGS AND PRECAUTIONS (5.3)]**
- Liver tumors, benign or malignant, or liver disease** [see WARNINGS AND PRECAUTIONS (5.4) and USE IN SPECIFIC POPULATIONS (8.7)]**
- Pregnancy, because there is no reason to use COCs during pregnancy** [see WARNINGS AND PRECAUTIONS (5.11) and USE IN SPECIFIC POPULATIONS (8.1)]**
- Use of Hepatitis C drug combinations containing ombitasvir, paritaprevir/ritonavir, with or without dasabuvir due to the potential for ALT elevations** [see WARNINGS AND PRECAUTIONS (5.5) and DRUG INTERACTIONS (7.3)].**
BOXED WARNING SECTION
** WARNING: CIGARETTE SMOKING AND SERIOUS CARDIOVASCULAR EVENTS**
DRUG INTERACTIONS SECTION
Highlight: Drugs or herbal products that induce certain enzymes (for example, CYP3A4) may decrease the effectiveness of COCs or increase breakthrough bleeding. Counsel patients to use a back-up or alternative method of contraception when enzyme inducers are used with COCs. (7.1)
7 DRUG INTERACTIONS
Consult the labeling of all concurrently-used drugs to obtain further information about interactions with hormonal contraceptives or the potential for enzyme alterations.
7.1 Effects of Other Drugs on Combined Oral Contraceptives
Substances diminishing the efficacy of COCs: Drugs or herbal products that induce certain enzymes, including cytochrome P450 3A4 (CYP3A4), may decrease the effectiveness of COCs or increase breakthrough bleeding. Some drugs or herbal products that may decrease the effectiveness of hormonal contraceptives include phenytoin, barbiturates, carbamazepine, bosentan, felbamate, griseofulvin, oxcarbazepine, rifampin, topiramate and products containing St. John’s wort. Interactions between oral contraceptives and other drugs may lead to breakthrough bleeding and/or contraceptive failure. Counsel women to use an alternative method of contraception or a back-up method when enzyme inducers are used with COCs, and to continue back-up contraception for 28 days after discontinuing the enzyme inducer to ensure contraceptive reliability.
Substances increasing the plasma concentrations of COCs: Co-administration of atorvastatin and certain COCs containing EE increase AUC values for EE by approximately 20%. Ascorbic acid and acetaminophen may increase plasma EE concentrations, possibly by inhibition of conjugation.
Concomitant administration of moderate or strong CYP3A4 inhibitors such as azole antifungals (e.g., ketoconazole, itraconazole, voriconazole, fluconazole), verapamil, macrolides (e.g., clarithromycin, erythromycin), diltiazem, and grapefruit juice can increase the plasma concentrations of the estrogen or the progestin or both. In a clinical drug-drug interaction study conducted in premenopausal women, once daily co-administration of DRSP 3 mg/EE 0.02 mg containing tablets with strong CYP3A4 inhibitor, ketoconazole 200 mg twice daily for 10 days resulted in a moderate increase of DRSP systemic exposure. The exposure of EE was increased mildly [seeWARNINGS AND PRECAUTIONS (5.2)and CLINICAL PHARMACOLOGY (12.3)].
Human immunodeficiency virus (HIV)/Hepatitis C virus (HCV) protease inhibitors and non-nucleoside reverse transcriptase inhibitors: Significant changes (increase or decrease) in the plasma concentrations of estrogen and progestin have been noted in some cases of co-administration with HIV/HCV protease inhibitors or with non-nucleoside reverse transcriptase inhibitors.
Antibiotics: There have been reports of pregnancy while taking hormonal contraceptives and antibiotics, but clinical pharmacokinetic studies have not shown consistent effects of antibiotics on plasma concentrations of synthetic steroids.
7.2 Effects of Combined Oral Contraceptives on Other Drugs
COCs containing EE may inhibit the metabolism of other compounds. COCs have been shown to significantly decrease plasma concentrations of lamotrigine, likely due to induction of lamotrigine glucuronidation. This may reduce seizure control; therefore, dosage adjustments of lamotrigine may be necessary. Consult the labeling of the concurrently-used drug to obtain further information about interactions with COCs or the potential for enzyme alterations.
COCs Increasing the Plasma Concentrations of CYP450 Enzymes: In clinical studies, administration of a hormonal contraceptive containing EE did not lead to any increase or only to a weak increase in plasma concentrations of CYP3A4 substrates (e.g., midazolam) while plasma concentrations of CYP2C19 substrates (e.g., omeprazole and voriconazole) and CYP1A2 substrates (e.g., theophylline and tizanidine) can have a weak or moderate increase.
Clinical studies did not indicate an inhibitory potential of DRSP towards human CYP enzymes at clinically relevant concentrations [seeCLINICAL PHARMACOLOGY (12.3)].
Women on thyroid hormone replacement therapy may need increased doses of thyroid hormone because serum concentration of thyroid-binding globulin increases with use of COCs.
Potential to Increase Serum Potassium Concentration: There is a potential for an increase in serum potassium concentration in women taking drospirenone and ethinyl estradiol with other drugs that may increase serum potassium concentration [seeWARNINGS AND PRECAUTIONS (5.2)and CLINICAL PHARMACOLOGY (12.3)]
7.3 Concomitant Use with HCV Combination Therapy- Liver Enzyme Elevation
Do not co-administer drospirenone and ethinyl estradiol with HCV drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to potential for ALT elevations [seeWARNINGS AND PRECAUTIONS (5.5)].
7.4 Interference with Laboratory Tests
The use of contraceptive steroids may influence the results of certain laboratory tests, such as coagulation factors, lipids, glucose tolerance, and binding proteins. DRSP causes an increase in plasma renin activity and plasma aldosterone induced by its mild anti-mineralocorticoid activity. [See WARNINGS AND PRECAUTIONS (5.13)and DRUG INTERACTIONS (7.2)].
USE IN SPECIFIC POPULATIONS SECTION
Highlight: Nursing Mothers: Not recommended; can decrease milk production. (8.3)
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
There is little or no increased risk of birth defects in women who inadvertently use COCs during early pregnancy. Epidemiologic studies and meta- analyses have not found an increased risk of genital or non-genital birth defects (including cardiac anomalies and limb-reduction defects) following exposure to low dose COCs prior to conception or during early pregnancy.
The administration of COCs to induce withdrawal bleeding should not be used as a test for pregnancy. COCs should not be used during pregnancy to treat threatened or habitual abortion.
Women who do not breastfeed may start COCs no earlier than four weeks postpartum.
8.3 Nursing Mothers
When possible, advise the nursing mother to use other forms of contraception until she has weaned her child. Estrogen-containing COCs can reduce milk production in breastfeeding mothers. This is less likely to occur once breastfeeding is well-established; however, it can occur at any time in some women. Small amounts of oral contraceptive steroids and/or metabolites are present in breast milk.
After oral administration of 3 mg DRSP/0.03 mg EE (Yasmin) tablets, about 0.02% of the DRSP dose was excreted into the breast milk of postpartum women within 24 hours. This results in a maximal daily dose of about 0.003 mg DRSP in an infant.
8.4 Pediatric Use
Safety and efficacy of drospirenone and ethinyl estradiol have been established in women of reproductive age. Efficacy is expected to be the same for postpubertal adolescents under the age of 18 and for users 18 years and older. Use of this product before menarche is not indicated.
8.5 Geriatric Use
Drospirenone and ethinyl estradiol have not been studied in postmenopausal women and is not indicated in this population.
8.6 Patients with Renal Impairment
Drospirenone and ethinyl estradiol is contraindicated in patients with renal impairment [seeCONTRAINDICATIONS (4)and WARNINGS AND PRECAUTIONS (5.2)].
In subjects with creatinine clearance (CLcr) of 50 to 79 mL/min, serum DRSP levels were comparable to those in a control group with CLcr ≥80 mL/min. In subjects with CLcr of 30 to 49 mL/min, serum DRSP concentrations were on average 37% higher than those in the control group. In addition, there is a potential to develop hyperkalemia in subjects with renal impairment whose serum potassium is in the upper reference range, and who are concomitantly using potassium sparing drugs [seeCLINICAL PHARMACOLOGY (12.3)].
8.7 Patients with Hepatic Impairment
Drospirenone and ethinyl estradiol is contraindicated in patients with hepatic disease [seeCONTRAINDICATIONS (4)and WARNINGS AND PRECAUTIONS (5.4)]. The mean exposure to DRSP in women with moderate liver impairment is approximately three times higher than the exposure in women with normal liver function. Drospirenone and ethinyl estradiol has not been studied in women with severe hepatic impairment
8.8 Race
No clinically significant difference was observed between the pharmacokinetics of DRSP or EE in Japanese versus Caucasian women [seeCLINICAL PHARMACOLOGY (12.3)].
ADVERSE REACTIONS SECTION
Highlight: * The most frequent adverse reactions (≥ 2%) in contraception and acne clinical trials were: headache/migraine (6.7%), menstrual irregularities (4.7%), nausea/vomiting (4.2%), breast pain/tenderness (4.0%) and mood changes (2.2%). (6.1)
- The most frequent adverse reactions (≥ 2%) in PMDD clinical trials were: menstrual irregularities (24.9%), nausea (15.8%), headache (13.0%), breast tenderness (10.5%), fatigue (4.2%), irritability (2.8%), decreased libido (2.8%), increased weight (2.5%), and affect lability (2.1%). (6.1)
**To report SUSPECTED ADVERSE REACTIONS, contact Xiromed, LLC. At 1-844-XIROMED (844-947-6633) or FDA at 1-800-FDA-1088 or **www.fda.gov/medwatch
6 ADVERSE REACTIONS
The following serious adverse reactions with the use of COCs are discussed elsewhere in the labeling:
•Serious cardiovascular events and stroke [seeBOXED WARNINGand** WARNINGS AND PRECAUTIONS (5.1)**]
•Vascular events [seeWARNINGS AND PRECAUTIONS (5.1)]
•Liver disease [seeWARNINGS AND PRECAUTIONS (5.4)]
Adverse reactions commonly reported by COC users are:
•Irregular uterine bleeding
•Nausea
•Breast tenderness
•Headache
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Contraception and Acne Clinical Trials
The data provided reflect the experience with the use of drospirenone and ethinyl estradiol in the adequate and well-controlled studies for contraception (N=1,056) and for moderate acne vulgaris (N=536).
For contraception, a Phase 3, multicenter, multinational, open-label study was conducted to evaluate safety and efficacy up to one year in 1,027 women aged 17 to 36 who took at least one dose of drospirenone and ethinyl estradiol. A second Phase 3 study was a single center, open-label, active-controlled study to evaluate the effect of 7 28-day cycles of drospirenone and ethinyl estradiol on carbohydrate metabolism, lipids and hemostasis in 29 women aged 18 to 35. For acne, two multicenter, double-blind, randomized, placebo- controlled studies, in 536 women aged 14 to 45 with moderate acne vulgaris who took at least one dose of drospirenone and ethinyl estradiol, evaluated the safety and efficacy during up to 6 cycles.
The adverse reactions seen across the 2 indications overlapped, and are reported using the frequencies from the pooled dataset. The most common adverse reactions (≥ 2% of users) were: headache/migraine (6.7%), menstrual irregularities (including vaginal hemorrhage [primarily spotting] and metrorrhagia (4.7%), nausea/vomiting (4.2%), breast pain/tenderness (4%) and mood changes (mood swings, depression, depressed mood and affect lability) (2.2%).
PMDD Clinical Trials
Safety data from trials for the indication of PMDD are reported separately due to differences in study design and setting in the Contraception and Acne studies as compared to the PMDD clinical program.
Two (one parallel and one crossover designed) multicenter, double-blind, randomized, placebo-controlled trials for the secondary indication of treating the symptoms of PMDD evaluated safety and efficacy of drospirenone and ethinyl estradiol during up to 3 cycles among 285 women aged 18–42, diagnosed with PMDD and who took at least one dose of drospirenone and ethinyl estradiol.
Common adverse reactions (≥ 2% of users) were: menstrual irregularities (including vaginal hemorrhage [primarily spotting] and metrorrhagia) (24.9%), nausea (15.8%), headache (13.0%), breast tenderness (10.5%), fatigue (4.2%), irritability (2.8%), decreased libido (2.8%), increased weight (2.5%), and affect lability (2.1%).
Adverse Reactions (≥1%) Leading to Study Discontinuation:
** Contraception Clinical Trials**
Of 1,056 women, 6.6% discontinued from the clinical trials due to an adverse reaction; the most frequent adverse reactions leading to discontinuation were headache/migraine (1.6%) and nausea/vomiting (1.0%).
Acne Clinical Trials
Of 536 women, 5.4% discontinued from the clinical trials due to an adverse reaction; the most frequent adverse reaction leading to discontinuation was menstrual irregularities (including menometrorrhagia, menorrhagia, metrorrhagia and vaginal hemorrhage) (2.2%) .
PMDD Clinical Trials
Of 285 women, 11.6% discontinued from the clinical trials due to an adverse reaction; the most frequent adverse reactions leading to discontinuation were: nausea/vomiting (4.6%), menstrual irregularity (including vaginal hemorrhage, menorrhagia, menstrual disorder, menstruation irregular and metrorrhagia) (4.2%), fatigue (1.8%), breast tenderness (1.4%), depression (1.4%), headache (1.1%), and irritability (1.1%).
Serious Adverse Reactions
Contraception Clinical Trials: migraine and cervical dysplasia
**Acne Clinical Trials:**none reported in the clinical trials
PMDD Clinical Trials: cervical dysplasia
6.2 Postmarketing Experience
Five studies that compared breast cancer risk between ever-users (current or past use) of COCs and never-users of COCs reported no association between ever use of COCs and breast cancer risk, with effect estimates ranging from 0.90 - 1.12 (Figure 3).
Three studies compared breast cancer risk between current or recent COC users (<6 months since last use) and never users of COCs (Figure 3). One of these studies reported no association between breast cancer risk and COC use. The other two studies found an increased relative risk of 1.19 - 1.33 with current or recent use. Both of these studies found an increased risk of breast cancer with current use of longer duration, with relative risks ranging from 1.03 with less than one year of COC use to approximately 1.4 with more than 8-10 years of COC use.
Figure 3: Relative Studies of Risk of Breast Cancer with Combined Oral Contraceptives
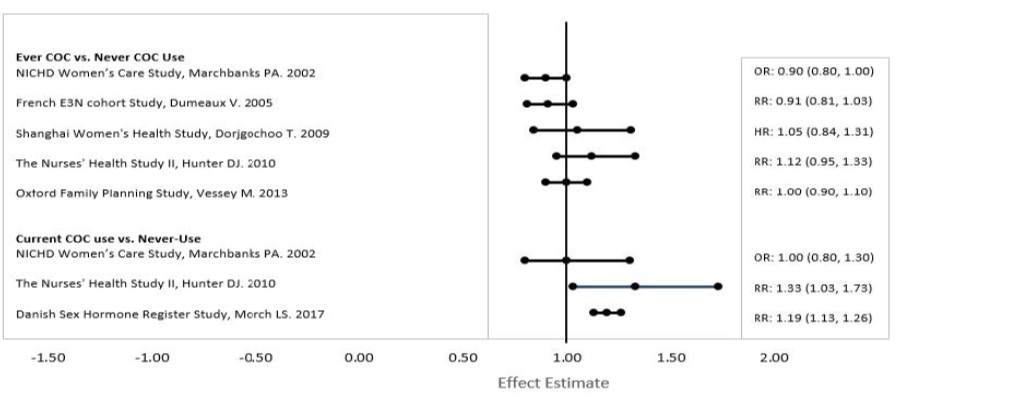
RR = relative risk; OR = odds ratio; HR = hazard ratio. “ever COC” are females with current or past COC use; “never COC use” are females that never used COCs.
The following adverse reactions have been identified during post approval use of drospirenone and ethinyl estradiol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions are grouped into System Organ Classes, and ordered by frequency.
Vascular disorders: Venous and arterial thromboembolic events (including pulmonary emboli, deep vein thrombosis, cerebral thrombosis, retinal thrombosis, myocardial infarction and stroke), hypertension (including hypertensive crisis)
Hepatobiliary disorders: Gallbladder disease, liver function disturbances, liver tumors
Immune system disorders: Hypersensitivity (including anaphylactic reaction)
Metabolism and nutrition disorders: Hyperkalemia, hypertriglyceridemia, changes in glucose tolerance or effect on peripheral insulin resistance (including diabetes mellitus)
Skin and subcutaneous tissue disorders: Chloasma, angioedema, erythema nodosum, erythema multiforme
Gastrointestinal disorders: Inflammatory bowel disease
Musculoskeletal and connective tissue disorders: Systemic lupus erythematosus
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
14.1 Oral Contraceptive Clinical Trial
In the primary contraceptive efficacy study of drospirenone and ethinyl estradiol (3 mg DRSP/0.02 mg EE) of up to 1 year duration, 1,027 subjects were enrolled and completed 11,480 28-day cycles of use. The age range was 17 to 36 years. The racial demographic was: 87.8% Caucasian, 4.6% Hispanic, 4.3% Black, 1.2% Asian, and 2.1% other. Women with a BMI greater than 35 were excluded from the trial. The pregnancy rate (Pearl Index) was 1.41 (95% CI [0.73, 2.47]) per 100 woman-years of use based on 12 pregnancies that occurred after the onset of treatment and within 14 days after the last dose of drospirenone and ethinyl estradiol in women 35 years of age or younger during cycles in which no other form of contraception was used.
14.2 Premenstrual Dysphoric Disorder Clinical Trials
Two multicenter, double-blind, randomized, placebo-controlled studies were conducted to evaluate the effectiveness of drospirenone and ethinyl estradiol in treating the symptoms of PMDD. Women aged 18 to 42 who met DSM-IV criteria for PMDD, confirmed by prospective daily ratings of their symptoms, were enrolled. Both studies measured the treatment effect of drospirenone and ethinyl estradiol using the Daily Record of Severity of Problems scale, a patient-rated instrument that assesses the symptoms that constitute the DSM-IV diagnostic criteria. The primary study was a parallel group design that included 384 evaluable reproductive-aged women with PMDD who were randomly assigned to receive drospirenone and ethinyl estradiol or placebo treatment for 3 menstrual cycles. The supportive study, a crossover design, was terminated prematurely prior to achieving recruitment goals due to enrollment difficulties. A total of 64 women of reproductive age with PMDD were treated initially with drospirenone and ethinyl estradiol or placebo for up to 3 cycles followed by a washout cycle and then crossed over to the alternate medication for 3 cycles.
Efficacy was assessed in both studies by the change from baseline during treatment using a scoring system based on the first 21 items of the Daily Record of Severity of Problems. Each of the 21 items was rated on a scale from 1 (not at all) to 6 (extreme); thus a maximum score of 126 was possible. In both trials, women who received drospirenone and ethinyl estradiol had statistically significantly greater improvement in their Daily Record of Severity of Problems scores. In the primary study, the average decrease (improvement) from baseline was 37.5 points in women taking drospirenone and ethinyl estradiol, compared to 30.0 points in women taking placebo.
14.3 Acne Clinical Trials
In two multicenter, double-blind, randomized, placebo-controlled studies, 889 subjects, ages 14 to 45 years, with moderate acne received drospirenone and ethinyl estradiol or placebo for six 28-day cycles. The primary efficacy endpoints were the percent change in inflammatory lesions, non-inflammatory lesions, total lesions, and the percentage of subjects with a "clear" or "almost clear" rating on the Investigator's Static Global Assessment (ISGA) scale on day 15 of cycle 6, as presented inTable 3:
Table 3: Efficacy Results for Acne Trials*
| ||||
|
Study 1 |
Study 2 | |||
|
Drospirenone and Ethinyl Estradiol N=228 |
Placebo N=230 |
Drospirenone and Ethinyl Estradiol N=218 |
Placebo N=213 | |
|
ISGA Success Rate |
35 (15%) |
10 (4%) |
46 (21%) |
19 (9%) |
|
Inflammatory Lesions Mean Baseline Count Mean Absolute (%) Reduction |
33 15 (48%) |
33 11 (32%) |
32 16 (51%) |
32 11 (34%) |
|
Non-inflammatory Lesions Mean Baseline Count Mean Absolute (%) Reduction |
47 18 (39%) |
47 10 (18%) |
44 17 (42%) |
44 11 (26%) |
|
Total lesions Mean Baseline Count Mean Absolute (%) reduction |
80 33 (42%) |
80 21 (25%) |
76 33 (46%) |
76 22 (31%) |
OVERDOSAGE SECTION
10 OVERDOSAGE
There have been no reports of serious ill effects from overdose, including ingestion by children. Overdosage may cause withdrawal bleeding in females and nausea.
DRSP is a spironolactone analogue which has anti-mineralocorticoid properties. Serum concentration of potassium and sodium, and evidence of metabolic acidosis, should be monitored in cases of overdose.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling. (Patient Information)
•Counsel patients that cigarette smoking increases the risk of serious cardiovascular events from COC use, and that women who are over 35 years old and smoke should not use COCs.
•Counsel patients that the increased risk of VTE compared to non-users of COCs is greatest after initially starting a COC or restarting (following a 4-week or greater pill-free interval) the same or a different COC.
•Counsel patients about the information regarding the risk of VTE with DRSP- containing COCs compared to COCs that contain levonorgestrel or some other progestins.
•Counsel patients that Loryna tablets do not protect against HIV-infection (AIDS) and other sexually transmitted diseases.
•Counsel patients on Warnings and Precautions associated with COCs.
•Counsel patients that Loryna tablets contain DRSP. Drospirenone may increase potassium. Patients should be advised to inform their healthcare provider if they have kidney, liver or adrenal disease because the use of Loryna tablets in the presence of these conditions could cause serious heart and health problems. They should also inform their healthcare provider if they are currently on daily, long-term treatment (NSAIDs, potassium-sparing diuretics, potassium supplementation, ACE inhibitors, angiotensin-II receptor antagonists, heparin or aldosterone antagonists) for a chronic condition or taking strong CYP3A4 inhibitors.
•Inform patients that Loryna tablets are not indicated during pregnancy. If pregnancy occurs during treatment with Loryna tablets, instruct the patient to stop further intake .
•Counsel patients to take one tablet daily by mouth at the same time every day. Instruct patients what to do in the event pills are missed. See**“WHAT TO DO IF YOU MISS PILLS”section inFDA-APPROVED PATIENT LABELING**.
•Counsel patients to use a back-up or alternative method of contraception when enzyme inducers are used with COCs.
•Counsel patients who are breastfeeding or who desire to breastfeed that COCs may reduce breast milk production. This is less likely to occur if breastfeeding is well established.
•Counsel any patient who starts COCs postpartum, and who has not yet had a period, to use an additional method of contraception until she has taken a peach tablet for 7 consecutive days.
•Counsel patients that amenorrhea may occur. Rule out pregnancy in the event of amenorrhea in two or more consecutive cycles.
LORYNA is a registered trademark of Xiromed Pharma España, S.L.
Manufactured by Laboratorios Leon Farma S.A., Spain
For Xiromed, LLC., Florham Park, NJ 07932
Product of Spain
Rev. 06/2022
PI-114-02
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Loryna (drospirenone and ethinyl estradiol tablets, USP) 3 mg/0.02 mg are available as follows:
Each blister card contains 24 active tablets and 4 inactive tablets. The 24 active tablets are peach, round, film-coated, debossed with SZ on one side and U2 on the other side. The 4 inert tablets are white, round, film-coated, debossed with SZ on one side and J1 on the other side.
NDC 63629-2336-01, one box containing 3 individual unit cartons.
REFERENCES SECTION
15 REFERENCES
1. Seeger, J.D., Loughlin, J., Eng, P.M., Clifford, C.R., Cutone, J., and Walker, A.M. (2007). Risk of thromboembolism in women taking ethinylestradiol/drospirenone and other oral contraceptives. Obstet Gynecol 110, 587-593.
2. Dinger, J.C., Heinemann, L.A., and Kuhl-Habich, D. (2007). The safety of a drospirenone-containing oral contraceptive: final results from the European Active Surveillance Study on oral contraceptives based on 142,475 women-years of observation. Contraception 75, 344-354.
3. Combined hormonal contraceptives (CHCs) and the risk of cardiovascular endpoints. Sidney, S. (primary author), http://www.fda.gov/downloads/Drugs/DrugSafety/UCM277384.pdf, accessed Oct 27, 2011.
4. Lidegaard, O., Lokkegaard, E., Svendsen, A.L., and Agger, C. (2009). Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ 339, b2890.
5. Lidegaard, O., Nielsen, L.H., Skovlund, C.W., Skjeldestad, F.E., and Lokkegaard, E. (2011). Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ 343, d6423.
6. van Hylckama Vlieg, A., Helmerhorst, F.M., Vandenbroucke, J.P., Doggen, C.J., and Rosendaal, F.R. (2009). The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ 339, b2921.
7. Dinger, J., Assmann, A., Mohner, S., and Minh, T.D. (2010). Risk of venous thromboembolism and the use of dienogest- and drospirenone-containing oral contraceptives: results from a German case-control study. J Fam Plann Reprod Health Care 36, 123-129.
8. Jick, S.S., and Hernandez, R.K. (2011). Risk of non-fatal venous thromboembolism in women using oral contraceptives containing drospirenone compared with women using oral contraceptives containing levonorgestrel: case- control study using United States claims data. BMJ 342, d2151.
9. Parkin, L., Sharples, K., Hernandez, R.K., and Jick, S.S. (2011). Risk of venous thromboembolism in users of oral contraceptives containing drospirenone or levonorgestrel: nested case-control study based on UK General Practice Research Database. BMJ 342, d2139.
