ARIPIPRAZOLE
These highlights do not include all the information needed to use ARIPIPRAZOLE TABLETS safely and effectively. See full prescribing information for ARIPIPRAZOLE TABLETS. ARIPIPRAZOLE tablets, for oral use.Initial U.S. Approval: 2002
3718e585-06b9-40fd-a3eb-18b6497a4235
HUMAN PRESCRIPTION DRUG LABEL
Aug 8, 2017
Camber Pharmaceuticals, Inc.
DUNS: 826774775
Products 6
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
aripiprazole
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Drug Labeling Information
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Increased Mortality
**Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at anincreased risk of death. Aripiprazole tablets are not approved for the treatment of patients withdementia-related psychosis **[see BOXED WARNING].
Safety Experience in Elderly Patients with Psychosis Associated with
Alzheimer’s Disease
In three, 10-week, placebo-controlled studies of aripiprazole tablets in
elderly patients with psychosis associated with Alzheimer’s disease (n=938;
mean age: 82.4 years; range: 56 to 99 years), the adverse reactions that were
reported at an incidence of ≥3% and aripiprazole tablets incidence at least
twice that for placebo were lethargy [placebo 2%, aripiprazole tablets 5%],
somnolence (including sedation) [placebo 3%, aripiprazole tablets 8%], and
incontinence (primarily, urinary incontinence) [placebo 1%, aripiprazole tablets 5%], excessive salivation [placebo 0%, aripiprazole tablets 4%], and
lightheadedness [placebo 1%, aripiprazole tablets 4%].
The safety and efficacy of aripiprazole tablets in the treatment of patients with psychosis associated with dementia have not been established. If the prescriber elects to treat such patients with aripiprazole tablets, assess for the emergence of difficulty swallowing or excessive somnolence, which could predispose to accidental injury or aspiration [see BOXED WARNING].
5.2 Cerebrovascular Adverse Events, Including Stroke
In placebo-controlled clinical studies (two flexible dose and one fixed dose study) of dementia-related psychosis, there was an increased incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, in aripiprazole-treated patients (mean age: 84 years; range: 78 to 88 years). In the fixed-dose study, there was a statistically significant dose response relationship for cerebrovascular adverse events in patients treated with aripiprazole tablets. Aripiprazole tablets are not approved for the treatment of patients with dementia-related psychosis [see BOXED WARNING].
5.3 Suicidal Thoughts and Behaviors in Children, Adolescents, and Young
Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term, placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with MDD and other psychiatric disorders. Short term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 3.
Table 3:
|
** Age Range** |
Drug-Placebo Difference in Number of ** Cases of Suicidality per 1000 Patients Treated** |
|
<18 18-24 |
Increases Compared to Placebo 14 additional cases 5 additional cases |
|
25-64 ≥65 |
Decreases Compared to Placebo 1 fewer case 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo- controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for MDD as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressivedisorder or other indications, both psychiatric and nonpsychiatric, should be alerted about theneed to monitor patients for the emergence of agitation, irritability, unusual changes in behavior,and the other symptoms described above, as well as the emergence of suicidality, and to reportsuch symptoms immediately to healthcare providers. Such monitoring should include dailyobservation by families and caregivers. Prescriptions for aripiprazole tablets should be writtenfor the smallest quantity of tablets consistent with good patient management, in order to reduce****the risk of overdose.
It should be noted that aripiprazole tablets are not approved for use in treating depression in the pediatric population.
5.4 Neuroleptic Malignant Syndrome (NMS)
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) may occur with administration of antipsychotic drugs, including aripiprazole tablets. Rare cases of NMS occurred during aripiprazole tablets treatment in the worldwide clinical database. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to exclude cases where the clinical presentation includes both serious medical illness (eg, pneumonia, systemic infection) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; 2) intensive symptomatic treatment and medical monitoring; and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
5.5 Tardive Dyskinesia
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and, thereby, may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, aripiprazole tablets should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that (1) is known to respond to antipsychotic drugs and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on aripiprazole tablets, drug discontinuation should be considered. However, some patients may require treatment with aripiprazole tablets despite the presence of the syndrome.
5.6 Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia/Diabetes Mellitus
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with aripiprazole tablets [see ADVERSE REACTIONS (6.1, 6.2)]. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of hyperglycemia-related adverse reactions in patients treated with the atypical antipsychotics. Because aripiprazole tablets were not marketed at the time these studies were performed, it is not known if aripiprazole tablets are associated with this increased risk. Precise risk estimates for hyperglycemia-related adversereactions in patients treated with atypical antipsychotics are not available.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
Adults
In an analysis of 13 placebo-controlled monotherapy trials in adults, primarily with schizophrenia or another indication, the mean change in fasting glucose in aripiprazole-treated patients (+4.4 mg/dL; median exposure 25 days; N=1057) was not significantly different than in placebo-treated patients (+2.5 mg/dL; median exposure 22 days; N=799). Table 4 shows the proportion of aripiprazole-treated patients with normal and borderline fasting glucose at baseline (median exposure 25 days) that had treatment-emergent high fasting glucose measurements compared to placebo-treated patients (median exposure 22 days).
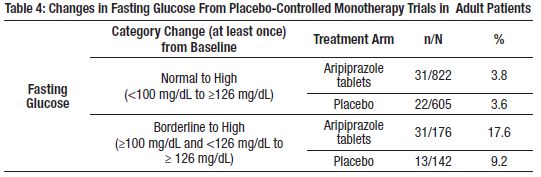
At 24 weeks, the mean change in fasting glucose in aripiprazole tablets- treated patients was not significantly different than in placebo-treated patients [+2.2 mg/dL (n=42) and +9.6 mg/dL (n=28), respectively].
Pediatric Patients and Adolescents
In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years), the mean change in fasting glucose in aripiprazole tablets- treated patients (+4.8 mg/dL; with a median exposure of 43 days; N=259) was not significantly different than in placebo-treated patients (+1.7 mg/dL; with a median exposure of 42 days; N=123).
Table 5 shows the proportion of patients with changes in fasting glucose levels from the pooled patients with adolescent schizophrenia and another indication (median exposure of 42 to 43 days).
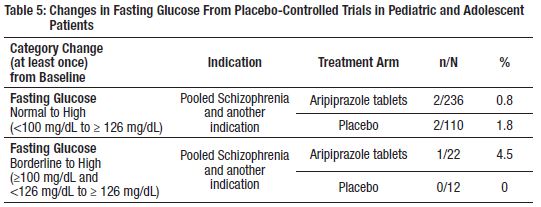
At 12 weeks in the pooled adolescent schizophrenia and another indication trials, the mean change in fasting glucose in aripiprazole tablets-treated patients was not significantly different than in placebo-treated patients [+2.4 mg/dL (n=81) and +0.1 mg/dL (n=15), respectively].
Dyslipidemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics. There were no significant differences between aripiprazole tablets- and placebo-treated patients in the proportion with changes from normal to clinically significant levels for fasting/nonfasting total cholesterol, fasting triglycerides, fasting LDLs, and fasting/nonfasting HDLs. Analyses of patients with at least 12 or 24 weeks of exposure were limited by small numbers of patients.
Adults
Table 6 shows the proportion of adult patients, primarily from pooled schizophrenia and another indication monotherapy placebo-controlled trials, with changes in total cholesterol (pooled from 17 trials; median exposure 21 to 25 days), fasting triglycerides (pooled from eight trials; median exposure 42 days), fasting LDL cholesterol (pooled from eight trials; median exposure 39 to 45 days, except for placebo-treated patients with baseline normal fasting LDL measurements, who had median treatment exposure of 24 days) and HDL cholesterol (pooled from nine trials; median exposure 40 to 42 days).
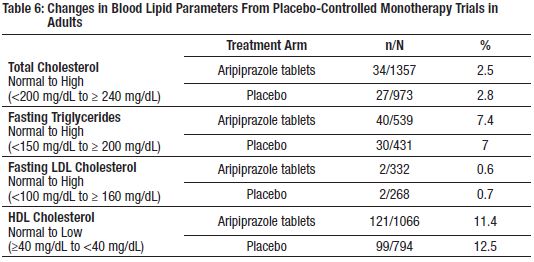
In monotherapy trials in adults, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole tablets- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 1/71 (1.4%) vs. 3/74 (4.1%); Fasting Triglycerides, 8/62 (12.9%) vs. 5/37 (13.5%); Fasting LDL Cholesterol, 0/34 (0%) vs. 1/25 (4%), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 1/42 (2.4%) vs. 3/37 (8.1%); Fasting Triglycerides, 5/34 (14.7%) vs. 5/20 (25%); Fasting LDL Cholesterol, 0/22 (0%) vs. 1/18 (5.6%), respectively.
Pediatric Patients and Adolescents
Table 7 shows the proportion of adolescents with schizophrenia (13 to 17 years) and pediatric patients with other indication (10 to 17 years) with changes in total cholesterol and HDL cholesterol (pooled from two placebo- controlled trials; median exposure 42 to 43 days) and fasting triglycerides (pooled from two placebo-controlled trials; median exposure 42 to 44 days).
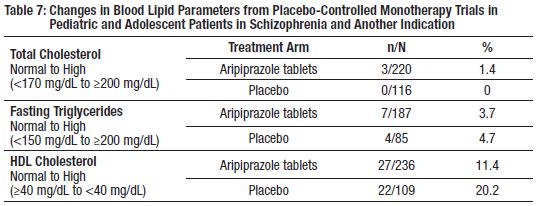
In monotherapy trials of adolescents with schizophrenia and pediatric patients with another indication, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole tablets- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 0/57 (0%) vs. 0/15 (0%); Fasting Triglycerides, 2/72 (2.8%) vs. 1/14 (7.1%), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 0/36 (0%) vs. 0/12 (0%); Fasting Triglycerides, 1/47 (2.1%) vs. 1/10 (10%), respectively.
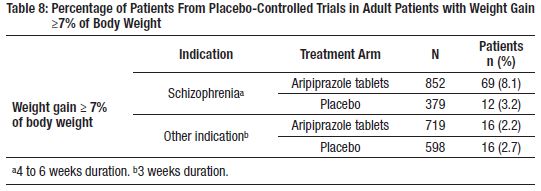
Weight Gain
Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Adults
In an analysis of 13 placebo-controlled monotherapy trials, primarily from pooled schizophrenia and another indication, with a median exposure of 21 to 25 days, the mean change in body weight in aripiprazole tablets-treated patients was +0.3 kg (N=1673) compared to –0.1 kg (N=1100) in placebo- controlled patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole tablets-treated patients was –1.5 kg (n=73) compared to –0.2 kg (n=46) in placebo-treated patients.
Table 8 shows the percentage of adult patients with weight gain ≥7% of body weight by indication.
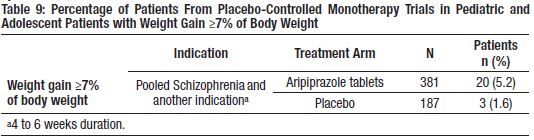
Pediatric Patients and Adolescents
In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years) with median exposure of 42 to 43 days, the mean change in body weight in aripiprazole tablets-treated patients was +1.6 kg (N=381) compared to +0.3 kg (N=187) in placebo-treated patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole tablets-treated patients was +5.8 kg (n=62) compared to +1.4 kg (n=13) in placebo-treated patients.
Table 9 shows the percentage of pediatric and adolescent patients with weight gain ≥7% of body weight by indication.
In an open-label trial that enrolled patients from the two placebo-controlled trials of adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years), 73.2% of patients (238/325) completed 26 weeks of therapy with aripiprazole tablets. After 26 weeks, 32.8% of patients gained ≥7% of their body weight, not adjusted for normal growth. To adjust for normal growth, z-scores were derived (measured in standard deviations [SD]), which normalize for the natural growth of pediatric patients and adolescents by comparisons to age- and gender-matched population standards. A z-score change <0.5 SD is considered not clinically significant. After 26 weeks, the mean change in z-score was 0.09 SD.
When treating pediatric patients for any indication, weight gain should be monitored and assessed against that expected for normal growth.
Additional pediatric use information is approved for Otsuka America Pharmaceutical, Inc.’s ABILIFY**®**** (aripiprazole) product. However, due to Otsuka America Pharmaceutical, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.**
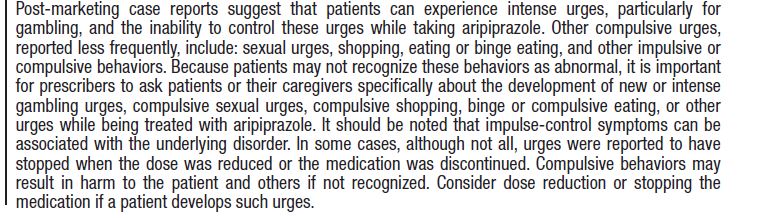
5.7 Pathological Gambling and Other Compulsive Behaviors
5.8 Orthostatic Hypotension
Aripiprazole tablets may cause orthostatic hypotension, perhaps due to its α1-adrenergic receptor antagonism. The incidence of orthostatic hypotension- associated events from short-term, placebo-controlled trials of adult patients on oral aripiprazole tablets (n=2467) included (aripiprazole tablets incidence, placebo incidence) orthostatic hypotension (1%, 0.3%), postural dizziness (0.5%, 0.3%), and syncope (0.5%, 0.4%); of pediatric patients 6 to 18 years of age (n=732) on oral aripiprazole tablets included orthostatic hypotension (0.5%, 0%), postural dizziness (0.4%, 0 %), and syncope (0.2%, 0%) [see ADVERSE REACTIONS (6.1)].
The incidence of a significant orthostatic change in blood pressure (defined as a decrease in systolic blood pressure ≥20 mmHg accompanied by an increase in heart rate ≥25 bpm when comparing standing to supine values) for aripiprazole tablets was not meaningfully different from placebo (aripiprazole tablets incidence, placebo incidence): in adult oral aripiprazole tablets- treated patients (4%, 2%), in pediatric oral aripiprazole tablets-treated patients aged 6 to 18 years (0.4%, 1%).
Aripiprazole should be used with caution in patients with known cardiovascular disease (history of myocardial infarction or ischemic heart disease, heart failure, or conduction abnormalities), cerebrovascular disease, or conditions which would predispose patients to hypotension (dehydration, hypovolemia, and treatment with antihypertensive medications) [see DRUG INTERACTIONS (7.1)].
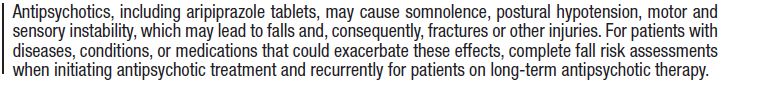
5.9 Falls
5.10 Leukopenia, Neutropenia, and Agranulocytosis
In clinical trials and/or postmarketing experience, events of leukopenia and neutropenia have been reported temporally related to antipsychotic agents, including aripiprazole tablets. Agranulocytosis has also been reported.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC)/absolute neutrophil count (ANC) and history of drug-induced leukopenia/neutropenia. In patients with a history of a clinically significant low WBC/ANC or drug-induced leukopenia/neutropenia, perform a complete blood count (CBC) frequently during the first few months of therapy. In such patients, consider discontinuation of aripiprazole tablets at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Monitor patients with clinically significant neutropenia for fever or other symptoms or signs of infection and treat promptly if such symptoms or signs occur. Discontinue aripiprazole tablets in patients with severe neutropenia (absolute neutrophil count <1000/mm3) and follow their WBC counts until recovery.
5.11 Seizures/Convulsions
In short-term, placebo-controlled trials, patients with a history of seizures excluded seizures/convulsions occurred in 0.1% (3/2467) of undiagnosed adult patients treated with oral aripiprazole tablets, in 0.1% (1/732) of pediatric patients (6 to 18 years).
As with other antipsychotic drugs, aripiprazole tablets should be used cautiously in patients with a history of seizures or with conditions that lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years or older.
5.12 Potential for Cognitive and Motor Impairment
Aripiprazole tablets, like other antipsychotics, may have the potential to impair judgment, thinking, or motor skills. For example, in short-term, placebo-controlled trials, somnolence (including sedation) was reported as follows (aripiprazole incidence, placebo incidence): in adult patients (n=2467) treated with oral aripiprazole tablets (11%, 6%), in pediatric patients ages 6 to 17 (n=611) (24%, 6%). Somnolence (including sedation) led to discontinuation in 0.3% (8/2467) of adult patients and 3% (20/732) of pediatric patients (6 to 18 years) on oral aripiprazole tablets in short-term, placebo-controlled trials.
Despite the relatively modest increased incidence of these events compared to placebo, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with aripiprazole tablets does not affect them adversely.
5.13 Body Temperature Regulation
Disruption of the body’s ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing aripiprazole tablets for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, (e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration) [see ADVERSE REACTIONS (6.2)].
5.14 Suicide
The possibility of a suicide attempt is inherent in psychotic illnesses and close supervision of high-risk patients should accompany drug therapy. Prescriptions for aripiprazole tablets should be written for the smallest quantity consistent with good patient management in order to reduce the risk of overdose [see ADVERSE REACTIONS (6.1, 6.2)].
5.15 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use, including aripiprazole tablets. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients, in particular those with advanced Alzheimer’s dementia. Aripiprazole tablets and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia [see WARNINGS AND PRECAUTIONS (5.1) and ADVERSE REACTIONS (6.2)].
- Cerebrovascular Adverse Reactions in Elderly Patients with Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack, including fatalities) (5.2)
- Neuroleptic Malignant Syndrome: Manage with immediate discontinuation and close monitoring (5.4)
- Tardive Dyskinesia: Discontinue if clinically appropriate (5.5)
- Metabolic Changes: Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain (5.6)
o Hyperglycemia/Diabetes Mellitus: Monitor glucose regularly in patients with
and at risk for diabetes (5.6)
o Dyslipidemia: Undesirable alterations in lipid levels have been observed in
patients treated with atypical antipsychotics (5.6)
o Weight Gain: Weight gain has been observed with atypical antipsychotic use.
Monitor weight (5.6) (5)
- Pathological Gambling and Other Compulsive Behaviors: Consider dose reduction or discontinuation (5.7)
- Orthostatic Hypotension: Monitor heart rate and blood pressure and warn patients with known cardiovascular or cerebrovascular disease, and risk of dehydration or syncope (5.8)
- Leukopenia, Neutropenia, and Agranulocytosis: have been reported with antipsychotics including aripiprazole tablets. Patients with a history of a clinically significant low white blood cell count (WBC) or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of aripiprazole tablets should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors (5.10)
- Seizures/Convulsions: Use cautiously in patients with a history of seizures or with conditions that lower the seizure threshold (5.11)
- Potential for Cognitive and Motor Impairment: Use caution when operating machinery (5.12)
- Suicide: The possibility of a suicide attempt is inherent in schizophrenia. Closely supervise high-risk patients (5.14)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Drugs Having Clinically Important Interactions with Aripiprazole
Tablets
Table 12: Clinically Important Drug Interactions with Aripiprazole Tablets:
1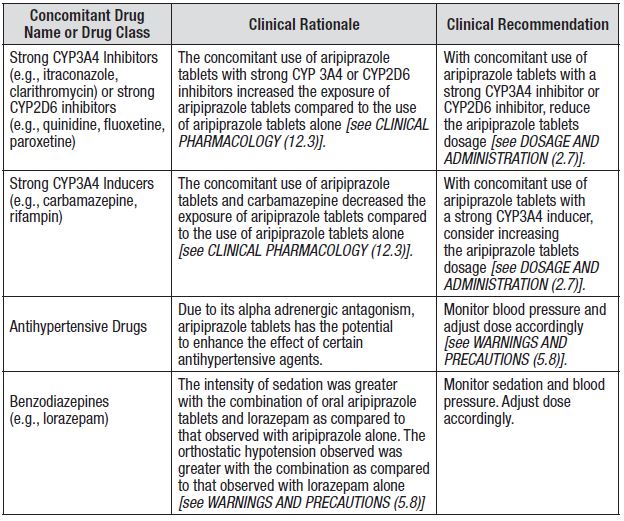
7.2 Drugs Having No Clinically Important Interactions with Aripiprazole
Tablets
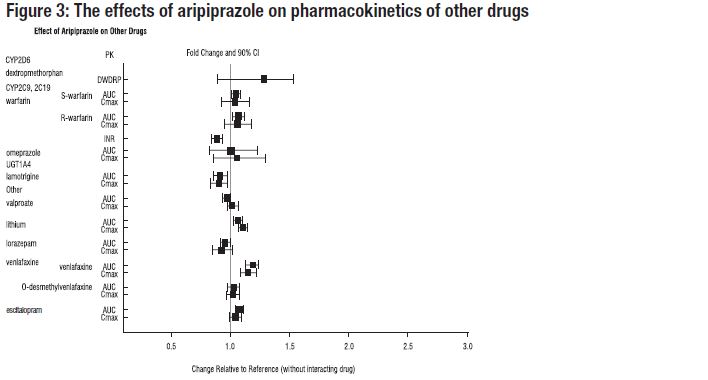
Based on pharmacokinetic studies, no dosage adjustment of aripiprazole tablets are required when administered concomitantly with famotidine, valproate, lithium, lorazepam.
In addition, no dosage adjustment is necessary for substrates of CYP2D6 (e.g., dextromethorphan, fluoxetine, paroxetine, or venlafaxine), CYP2C9 (e.g., warfarin), CYP2C19 (e.g., omeprazole, warfarin, escitalopram), or CYP3A4 (e.g., dextromethorphan) when co-administered with aripiprazole tablets. Additionally, no dosage adjustment is necessary for valproate, lithium, lamotrigine, lorazepam, or sertraline when co-administered with aripiprazole tablets [see CLINICAL PHARMACOLOGY (12.3)].
Dosage adjustment due to drug interactions (7.1): (7)
|
** Factors** |
Dosage Adjustments for (7) Aripiprazole tablets (7) |
|
Known CYP2D6 Poor Metabolizers |
Administer half of usual dose |
|
Known CYP2D6 Poor Metabolizers and strong |
Administer a quarter of usual dose |
|
Strong CYP2D6or CYP3A4 inhibitors |
Administer half of usual dose |
|
Strong CYP2D6and CYP3A4 inhibitors |
Administer a quarter of usual dose |
|
Strong CYP3A4 inducers |
Double usual dose over 1 to 2 weeks |
(7)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C:
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to aripiprazole during pregnancy. For more information contact the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit http://womensmentalhealth.org/clinical-and-research- programs/pregnancyregistry/.
Risk Summary
Neonates exposed to antipsychotic drugs (including aripiprazole tablets) during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms. Adequate and well controlled studies with aripiprazole tablets have not been conducted in pregnant women. Animal reproduction studies were conducted with aripiprazole in rats and rabbits during organogenesis, and in rats during the pre-and post-natal period. Oral and intravenous aripiprazole administration during organogenesis in rats and/or rabbits at doses higher than the maximum recommended human dose (MRHD) produced fetal death, decreased fetal weight, undescended testicles, delayed skeletal ossification, skeletal abnormalities, and diaphragmatic hernia. Oral and intravenous aripiprazole administration during the pre- and post-natal period in rats at doses higher than the maximum recommended human dose (MRHD) produced prolonged gestation, stillbirths, decreased pup weight, and decreased pup survival. Administer aripiprazole tablets during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs (including aripiprazole tablets) during the third trimester of pregnancy. These symptoms have varied in severity. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Monitor neonates for extrapyramidal and/or withdrawal symptoms.
Data
Animal Data
In animal studies, aripiprazole demonstrated developmental toxicity, including possible teratogenic effects in rats and rabbits.
Pregnant rats were treated with oral doses of 3, 10, and 30 mg/kg/day (1, 3, and 10 times the maximum recommended human dose [MRHD] on a mg/m2 basis) of aripiprazole during the period of organogenesis. Gestation was slightly prolonged at 30 mg/kg/day. Treatment at the high dose of 30 mg/kg/day caused a slight delay in fetal development (decreased fetal weight), undescended testes, and delayed skeletal ossification (also seen at 10 mg/kg/day). There were no adverse effects on embryofetal or pup survival. Delivered offspring had decreased body weights (10 and 30 mg/kg/day), and increased incidences of hepatodiaphragmatic nodules and diaphragmatic hernia at 30 mg/kg (the other dose groups were not examined for these findings). Postnatally, delayed vaginal opening was seen at 10 mg and 30 mg/kg/day and impaired reproductive performance (decreased fertility rate, corpora lutea, implants, live fetuses, and increased post-implantation loss, likely mediated through effects on female offspring) was seen at 30 mg/kg/day. Some maternal toxicity was seen at 30 mg/kg/day however, there was no evidence to suggest that these developmental effects were secondary to maternal toxicity.
Pregnant rabbits were treated with oral doses of 10, 30, and 100 mg/kg/day (2, 3, and 11 times human exposure at MRHD based on AUC and 6, 19, and 65 times the MRHD based on mg/m2) of aripiprazole during the period of organogenesis. At the high dose of 100 mg/kg/day decreased maternal food consumption, and increased abortions were seen as well as increased fetal mortality, decreased fetal weight (also seen at 30 mg/kg/day), increased incidence of a skeletal abnormality (fused sternebrae) (also seen at 30 mg/kg/day).
In a study in which rats were treated peri- and post-natally with oral doses of 3, 10, and 30 mg/kg/day (1, 3, and 10 times the MRHD on a mg/m2 basis) of aripiprazole from gestation day17 through day 21 postpartum, slight maternal toxicity, slightly prolonged gestation an increase in stillbirths and, decreases in pup weight (persisting into adulthood) and survival were seen at 30 mg/kg/day.
8.2 Labor and Delivery
The effect of aripiprazole tablets on labor and delivery in humans is unknown.
8.3 Nursing Mothers
Aripiprazole is present in human breast milk. Because of the potential for serious adverse reactions in nursing infants from aripiprazole tablets, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The pharmacokinetics of aripiprazole and dehydro-aripiprazole in pediatric patients, 10 to 17 years of age, were similar to those in adults after correcting for the differences in body weight [see CLINICAL PHARMACOLOGY (12.3)].
Schizophrenia
Safety and effectiveness in pediatric patients with schizophrenia were established in a 6-week, placebo-controlled clinical trial in 202 pediatric patients aged 13 to 17 years [see DOSAGE AND ADMINISTRATION (2.1), ADVERSE REACTIONS (6.1), and CLINICAL STUDIES (14.1)]. Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients
Information describing a clinical study in which efficacy was not demonstrated in patients ages6 to 17 years is approved for Otsuka America Pharmaceutical, Inc.’s ABILIFY®** (aripiprazole).**
Additional pediatric use information in patients ages 6 to 18 years is approved for OtsukaAmerica Pharmaceutical, Inc.’s ABILIFY®** (aripiprazole) product. However, due to Otsuka AmericaPharmaceutical, Inc.’s marketing exclusivity rights, this drug product is not labeled with thatpediatric information.**
Juvenile Animal Studies
Aripiprazole in juvenile rats caused mortality, CNS clinical signs, impaired memory and learning, and delayed sexual maturation when administered at oral doses of 10, 20, 40 mg/kg/day from weaning (21 days old) through maturity (80 days old). At 40 mg/kg/day, mortality, decreased activity, splayed hind limbs, hunched posture, ataxia, tremors and other CNS signs were observed in both genders. In addition, delayed sexual maturation was observed in males. At all doses and in a dose-dependent manner, impaired memory and learning, increased motor activity, and histopathology changes in the pituitary (atrophy), adrenals (adrenocortical hypertrophy), mammary glands (hyperplasia and increased secretion), and female reproductive organs (vaginal mucification, endometrial atrophy, decrease in ovarian corpora lutea) were observed. The changes in female reproductive organs were considered secondary to the increase in prolactin serum levels. A No Observed Adverse Effect Level (NOAEL) could not be determined and, at the lowest tested dose of 10 mg/kg/day, there is no safety margin relative to the systemic exposures (AUC0to24) for aripiprazole or its major active metabolite in adolescents at the maximum recommended pediatric dose of 15 mg/day. All drug-related effects were reversible after a 2-month recovery period, and most of the drug effects in juvenile rats were also observed in adult rats from previously conducted studies.
Aripiprazole in juvenile dogs (2 months old) caused CNS clinical signs of tremors, hypoactivity, ataxia, recumbency and limited use of hind limbs when administered orally for 6 months at 3, 10, 30 mg/kg/day. Mean body weight and weight gain were decreased up to 18% in females in all drug groups relative to control values. A NOAEL could not be determined and, at the lowest tested dose of 3 mg/kg/day, there is no safety margin relative to the systemic exposures (AUC0to24) for aripiprazole or its major active metabolite in adolescents at the maximum recommended pediatric dose of 15 mg/day. All drug-related effects were reversible after a 2-month recovery period.
8.5 Geriatric Use
No dosage adjustment is recommended for elderly patients [see BOXED WARNING, WARNINGS AND PRECAUTIONS (5.1), and CLINICAL PHARMACOLOGY (12.3)].
Of the 13,543 patients treated with oral aripiprazole tablets in clinical trials, 1073 (8%) were ≥65 years old and 799 (6%) were ≥75 years old. Placebo- controlled studies of oral aripiprazole in schizophrenia or other indications did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Aripiprazole tablets are not approved for the treatment of patients with psychosis associated with Alzheimer’s disease [see BOXED WARNING and WARNINGS AND PRECAUTIONS (5.1)].
8.6 CYP2D6 Poor Metabolizers
Dosage adjustment is recommended in known CYP2D6 poor metabolizers due to high aripiprazole concentrations. Approximately 8% of Caucasians and 3 to 8% of Black/African Americans cannot metabolize CYP2D6 substrates and are classified as poor metabolizers (PM) [see DOSAGE AND ADMINISTRATION (2.7) and CLINICAL PHARMACOLOGY (12.3)].
8.7 Hepatic and Renal Impairment
No dosage adjustment for aripiprazole tablets is required on the basis of a patient’s hepatic function (mild to severe hepatic impairment, Child-Pugh score between 5 and 15), or renal function (mild to severe renal impairment, glomerular filtration rate between 15 and 90 mL/minute) [see CLINICAL PHARMACOLOGY (12.3)].
8.8 Other Specific Populations
No dosage adjustment for aripiprazole tablets are required on the basis of a patient’s sex, race, or smoking status [see CLINICAL PHARMACOLOGY (12.3)].
- Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure (8.1)
- Nursing Mothers: Discontinue drug or nursing, taking into consideration importance of drug to the mother (8.3)
Additional pediatric use information is approved for Otsuka America Pharmaceutical, Inc.’s ABILIFY**®**** (aripiprazole) product. However, due to Otsuka America Pharmaceutical, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.** (8)
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Aripiprazole tablets, USP are available as described in Table 2.
Table 2: Aripiprazole Tablets, USP Presentations
|
** Tablet Strength** |
Tablet Color/Shape |
** Tablet Markings** |
|
** 2 mg** |
Light green to green modified rectangle |
“T” and “44” |
|
** 5 mg** |
Light blue to blue modified rectangle |
“T” and “45” |
|
** 10 mg** |
Light pink to pink modified rectangle |
“T” and “46” |
|
** 15 mg** |
Light yellow to yellow round |
“T” and “47” |
|
** 20 mg** |
White to off white round |
“T” and “48” |
|
** 30 mg** |
Light pink to pink round |
“T” and “49” |
Tablets: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg and 30 mg (3) (3)
DRUG ABUSE AND DEPENDENCE SECTION
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Aripiprazole tablet is not a controlled substance.
9.2 Abuse
Aripiprazole tablet has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of aripiprazole tablets misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior).
9.3 Dependence
In physical dependence studies in monkeys, withdrawal symptoms were observed upon abrupt cessation of dosing. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of aripiprazole in schizophrenia is unknown. However, the efficacy of aripiprazole could be mediated through a combination of partial agonist activity at D2 and 5-HT1A receptors and antagonist activity at 5-HT2A receptors. Actions at receptors other than D2, 5-HT1A, and 5-HT2A may explain some of the other clinical effects of aripiprazole (e.g., the orthostatic hypotension observed with aripiprazole may be explained by its antagonist activity at adrenergic alpha1 receptors).
12.2 Pharmacodynamics
Aripiprazole exhibits high affinity for dopamine D2 and D3, serotonin 5-HT1A and 5-HT2A receptors (Ki values of 0.34 nM, 0.8 nM, 1.7 nM, and 3.4 nM, respectively), moderate affinity for dopamine D4, serotonin 5-HT2C and 5-HT7, alpha1-adrenergic and histamine H1 receptors (Ki values of 44 nM, 15 nM, 39 nM, 57 nM, and 61 nM, respectively), and moderate affinity for the serotonin reuptake site (Ki=98 nM). Aripiprazole has no appreciable affinity for cholinergic muscarinic receptors (IC50>1000 nM). [Aripiprazole functions as a partial agonist at the dopamine D2 and the serotonin 5-HT1A receptors, and as an antagonist at serotonin 5-HT2A receptor.]
12.3 Pharmacokinetics
Aripiprazole tablets activity is presumably primarily due to the parent drug, aripiprazole, and to a lesser extent, to its major metabolite, dehydro aripiprazole, which has been shown to have affinities for D2 receptors similar to the parent drug and represents 40% of the parent drug exposure in plasma. The mean elimination half-lives are about 75 hours and 94 hours for aripiprazole and dehydro-aripiprazole, respectively. Steady-state concentrations are attained within 14 days of dosing for both active moieties. Aripiprazole accumulation is predictable from single-dose pharmacokinetics. At steady-state, the pharmacokinetics of aripiprazole is dose-proportional. Elimination of aripiprazole is mainly through hepatic metabolism involving two P450 isozymes, CYP2D6 and CYP3A4. For CYP2D6 poor metabolizers, the mean elimination half-life for aripiprazole is about 146 hours.
ORAL ADMINISTRATION
Absorption
Tablet: Aripiprazole is well absorbed after administration of the tablet, with peak plasma concentrations occurring within 3 hours to 5 hours; the absolute oral bioavailability of the tablet formulation is 87%. Aripiprazole tablets can be administered with or without food. Administration of a 15 mg aripiprazole tablet with a standard high-fat meal did not significantly affect the Cmax or AUC of aripiprazole or its active metabolite, dehydro- aripiprazole, but delayed Tmax by 3 hours for aripiprazole and 12 hours for dehydro- aripiprazole.
Distribution
The steady-state volume of distribution of aripiprazole following intravenous administration is high (404 L or 4.9 L/kg), indicating extensive extravascular distribution. At therapeutic concentrations, aripiprazole and its major metabolite are greater than 99% bound to serum proteins, primarily to albumin. In healthy human volunteers administered 0.5 to 30 mg/day aripiprazole for 14 days, there was dose-dependent D2 receptor occupancy indicating brain penetration of aripiprazole in humans.
Metabolism and Elimination
Aripiprazole is metabolized primarily by three biotransformation pathways: dehydrogenation, hydroxylation, and N-dealkylation. Based on in vitro studies, CYP3A4 and CYP2D6 enzymes are responsible for dehydrogenation and hydroxylation of aripiprazole, and N-dealkylation is catalyzed by CYP3A4. Aripiprazole is the predominant drug moiety in the systemic circulation. At steady-state, dehydro- aripiprazole, the active metabolite, represents about 40% of aripiprazole AUC in plasma.
Following a single oral dose of [14C]-labeled aripiprazole, approximately 25% and 55% of the administered radioactivity was recovered in the urine and feces, respectively. Less than 1% of unchanged aripiprazole was excreted in the urine and approximately 18% of the oral dose was recovered unchanged in the feces.
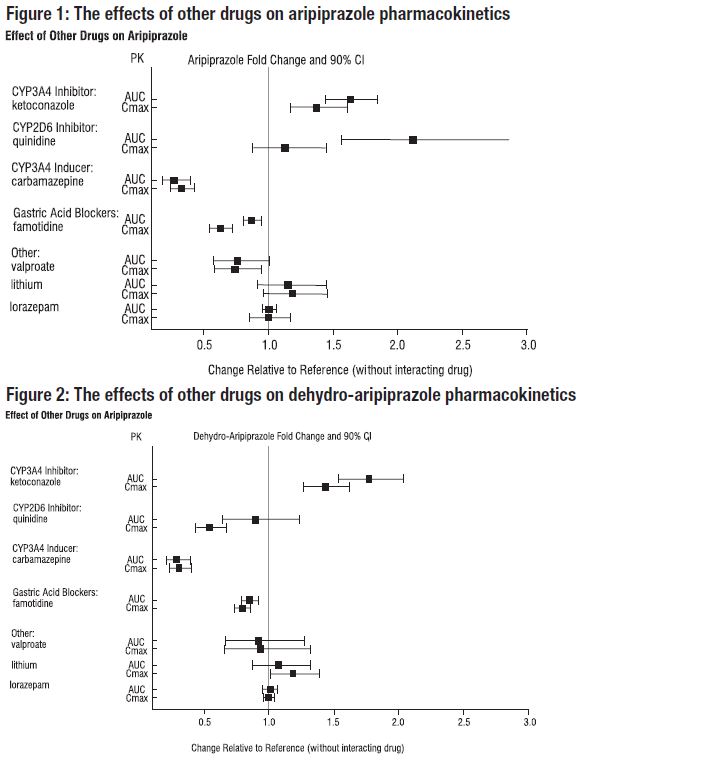
Drug Interaction Studies
Effects of other drugs on the exposures of aripiprazole and dehydro- aripiprazole are summarized in Figure 1 and Figure 2, respectively. Based on simulation, a 4.5-fold increase in mean Cmax and AUC values at steady-state is expected when extensive metabolizers of CYP2D6 are administered with both strong CYP2D6 and CYP3A4 inhibitors. A 3-fold increase in mean Cmax and AUC values at steady-state is expected in poor metabolizers of CYP2D6 administered with strong CYP3A4 inhibitors.
The effects of aripiprazole tablets on the exposures of other drugs are summarized in Figure 3.
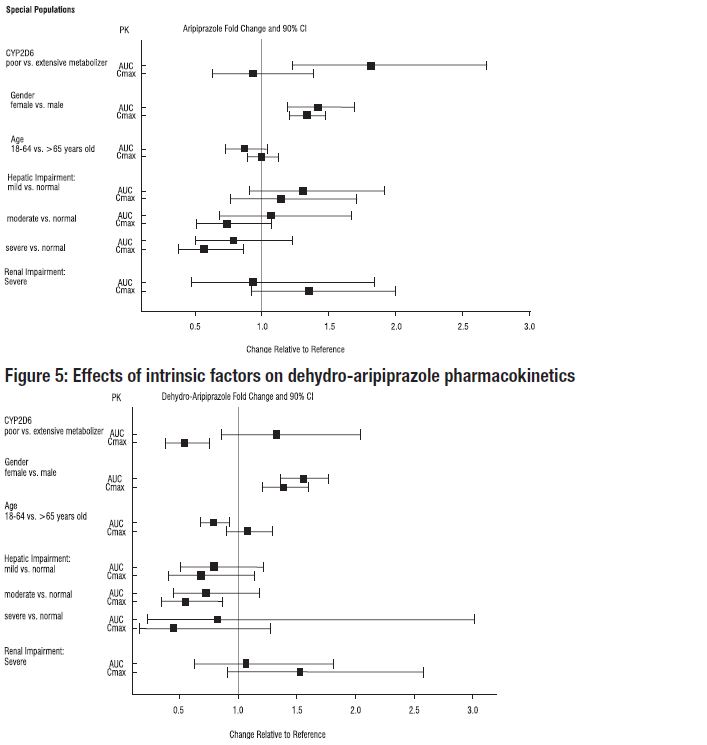
Studies in Specific Populations
Exposures of aripiprazole and dehydro-aripiprazole in specific populations are summarized in Figure 4 and Figure 5, respectively. In addition, in pediatric patients (10 to 17 years of age) administered with aripiprazole tablets (20 mg to 30 mg), the body weight corrected aripiprazole clearance was similar to the adults.
Figure 4: Effects of intrinsic factors on aripiprazole pharmacokinetics
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Lifetime carcinogenicity studies were conducted in ICR mice, Sprague-Dawley (SD) rats, and F344 rats. Aripiprazole was administered for 2 years in the diet at doses of 1, 3, 10, and 30 mg/kg/day to ICR mice and 1, 3, and 10 mg/kg/day to F344 rats (0.2 to 5 times and 0.3 to 3 times the maximum recommended human dose [MRHD] based on mg/m2, respectively). In addition, SD rats were dosed orally for 2 years at 10, 20, 40, and 60 mg/kg/day (3 to 19 times the MRHD based on mg/m2). Aripiprazole did not induce tumors in male mice or male rats. In female mice, the incidences of pituitary gland adenomas and mammary gland adenocarcinomas and adenoacanthomas were increased at dietary doses of 3 to 30 mg/kg/day (0.1 to 0.9 times human exposure at MRHD based on AUC and 0.5 to 5 times the MRHD based on mg/m2). In female rats, the incidence of mammary gland fibroadenomas was increased at a dietary dose of 10 mg/kg/day (0.1 times human exposure at MRHD based on AUC and 3 times the MRHD based on mg/m2); and the incidences of adrenocortical carcinomas and combined adrenocortical adenomas/carcinomas were increased at an oral dose of 60 mg/kg/day (14 times human exposure at MRHD based on AUC and 19 times the MRHD based on mg/m2).
Proliferative changes in the pituitary and mammary gland of rodents have been observed following chronic administration of other antipsychotic agents and are considered prolactin-mediated. Serum prolactin was not measured in the aripiprazole carcinogenicity studies. However, increases in serum prolactin levels were observed in female mice in a 13-week dietary study at the doses associated with mammary gland and pituitary tumors. Serum prolactin was not increased in female rats in 4-week and 13-week dietary studies at the dose associated with mammary gland tumors. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unknown.
Mutagenesis
The mutagenic potential of aripiprazole was tested in the in vitro bacterial reverse-mutation assay, the in vitro bacterial DNA repair assay, the in vitro forward gene mutation assay in mouse lymphoma cells, the in vitro chromosomal aberration assay in Chinese hamster lung (CHL) cells, the in vivo micronucleus assay in mice, and the unscheduled DNA synthesis assay in rats. Aripiprazole and a metabolite (2,3-DCPP) were clastogenic in the in vitro chromosomal aberration assay in CHL cells with and without metabolic activation. The metabolite, 2,3-DCPP, produced increases in numerical aberrations in the in vitro assay in CHL cells in the absence of metabolic activation. A positive response was obtained in the in vivo micronucleus assay in mice; however, the response was due to a mechanism not considered relevant to humans.
Impairment of Fertility
Female rats were treated with oral doses of 2, 6, and 20 mg/kg/day (0.6, 2, and 6 times the maximum recommended human dose [MRHD] on a mg/m2 basis) of aripiprazole from 2 weeks prior to mating through day 7 of gestation. Estrus cycle irregularities and increased corpora lutea were seen at all doses, but no impairment of fertility was seen. Increased pre-implantation loss was seen at 6 and 20 mg/kg/day and decreased fetal weight was seen at 20 mg/kg/day.
Male rats were treated with oral doses of 20, 40, and 60 mg/kg/day (6, 13, and 19 times the MRHD on a mg/m2 basis) of aripiprazole from 9 weeks prior to mating through mating. Disturbances in spermatogenesis were seen at 60 mg/kg and prostate atrophy was seen at 40 and 60 mg/kg, but no impairment of fertility was seen
13.2 Animal Toxicology and/or Pharmacology
Aripiprazole produced retinal degeneration in albino rats in a 26-week chronic toxicity study at a dose of 60 mg/kg and in a 2-year carcinogenicity study at doses of 40 mg and 60 mg/kg. The 40 mg and 60 mg/kg/day doses are 13 and 19 times the maximum recommended human dose (MRHD) based on mg/m2 and 7 to 14 times human exposure at MRHD based on AUC. Evaluation of the retinas of albino mice and of monkeys did not reveal evidence of retinal degeneration. Additional studies to further evaluate the mechanism have not been performed. The relevance of this finding to human risk is unknown.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Aripiprazole tablets, 2 mg are light green to green, modified rectangular, bevel edged biconvex tablets debossed with ‘T’ on one side and ‘44’ on other side.
Bottles of 30 Tablets NDC 31722-919-30
Bottles of 100 Tablets NDC 31722-919-01
Aripiprazole tablets, 5 mg are light blue to blue, modified rectangular, bevel
edged biconvex tablets debossed with ‘T’ on one side and ‘45’ on other side.
Bottles of 30 Tablets NDC 31722-920-30
Bottles of 100 Tablets NDC 31722-920-01
Aripiprazole tablets, 10 mg are light pink to pink, modified rectangular, bevel edged biconvex tablets debossed with ‘T’ on one side and ‘46’ on other side.
Bottles of 30 Tablets NDC 31722-921-30
Bottles of 100 Tablets NDC 31722-921-01
Aripiprazole tablets, 15 mg are light yellow to yellow, round, bevel edged biconvex tablets debossed with ‘T’ on one side and ‘47’ on other side.
Bottles of 30 Tablets NDC 31722-922-30
Bottles of 100 Tablets NDC 31722-922-01
Aripiprazole tablets, 20 mg are white to off-white, round, bevel edged biconvex tablets debossed with ‘T’ on one side and ‘48’ on other side.
Bottles of 30 Tablets NDC 31722-923-30
Bottles of 100 Tablets NDC 31722-923-01
Aripiprazole tablets, 30 mg are light pink to pink, round, bevel edged biconvex tablets debossed with ‘T’ on one side and ‘49’ on other side.
Bottles of 30 Tablets NDC 31722-924-30
Bottles of 100 Tablets NDC 31722-924-01
16.2 Storage
Store at 20º to 25º C (68º to 77ºF) [see USP Controlled Room Temperature].
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
See Medication Guide
Discuss the following issues with patients prescribed aripiprazole tablets:
Clinical Worsening of Depression and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior** and indicate a need for very close monitoring and possibly changes in the medication**[see WARNINGS AND PRECAUTIONS (5.3)].
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with aripiprazole tablets and should counsel them in its appropriate use. A patient Medication Guide including information about “Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions” is available for aripiprazole tablets. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. It should be noted that aripiprazole tablets are not approved as a single agent for treatment of depression and has not been evaluated in pediatric major depressive disorder.
Pathological Gambling and Other Compulsive Behaviors
Advise patients and their caregivers of the possibility that they may experience compulsive urges to shop, intense urges to gamble, compulsive sexual urges, binge eating and/or other compulsive urges and the inability to control these urges while taking aripiprazole tablets. In some cases, but not all, the urges were reported to have stopped when the dose was reduced or stopped [see WARNINGS AND PRECAUTIONS (5.7)].
Interference with Cognitive and Motor Performance
Because aripiprazole tablets may have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that aripiprazole tablets therapy does not affect them adversely [see WARNINGS AND PRECAUTIONS (5.12)].
Nursing
Advise patients that breastfeeding is not recommended with aripiprazole treatment because of the potential for serious adverse reactions in a nursing infant [see USE IN SPECIFIC POPULATIONS (8.3)].
Concomitant Medication
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions [see DRUG INTERACTIONS (7)].
Heat Exposure and Dehydration
Patients should be advised regarding appropriate care in avoiding overheating and dehydration [see WARNINGS AND PRECAUTIONS (5.13)].
Manufactured by:
Ascent Pharmaceuticals, Inc.
Central Islip, NY 11722
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854
ABILIFY is a trademark of Otsuka Pharmaceutical Company.
Revised: 08/2017
