Ultomiris
These highlights do not include all the information needed to use ULTOMIRIS safely and effectively. See full prescribing information for ULTOMIRIS. ULTOMIRIS (ravulizumab-cwvz) injection, for intravenous or subcutaneous use Initial U.S. Approval: 2018
a9a590d9-0217-43c7-908d-e62a71279791
HUMAN PRESCRIPTION DRUG LABEL
Mar 28, 2024
Alexion Pharmaceuticals Inc.
DUNS: 789359510
Products 4
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
ravulizumab
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (1)
ravulizumab
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (1)
RAVULIZUMAB
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
ravulizumab
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (1)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC 25682-031-01
ULTOMIRIS®
(ravulizumab-cwvz)
injection for subcutaneous use
245 mg/3.5 mL (70 mg/mL)
Rx only
Sterile Solution
Store Refrigerated at 36°F - 46°F
(2°C - 8°C) in Carton to Protect from Light
Do Not Freeze or Shake
(See Bottom for Additional Storage and Drug Information)
Keep Out of Reach of Children
ATTENTION: Dispense the Enclosed
Medication Guide to Each Patient
IMPORTANT!
2 cartons required
for 1 full dose
Refer to Instructions for Use
Do Not Use if Package is Damaged
MR Unsafe
Keep Dry
Single Use (Not Reusable)
Type BF Applied Part
STERILE
EO
On-body Injector Sterilized
Using Ethylene Oxide
If stored at room temperature, discard
after 3 days. Do not return to the
refrigerator.
This Carton Contains:
1 x 3.5 mL Prefilled Cartridge
1 x On-Body Injector

BOXED WARNING SECTION
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
1.1 Paroxysmal Nocturnal Hemoglobinuria
ULTOMIRIS is indicated for the treatment of adult and pediatric patients one month of age and older with paroxysmal nocturnal hemoglobinuria (PNH).
1.2 Atypical Hemolytic Uremic Syndrome
ULTOMIRIS is indicated for the treatment of adult and pediatric patients one month of age and older with atypical hemolytic uremic syndrome (aHUS) to inhibit complement-mediated thrombotic microangiopathy (TMA).
Limitations of Use:
ULTOMIRIS is not indicated for the treatment of patients with Shiga toxin E. coli related hemolytic uremic syndrome (STEC-HUS).
1.3 Generalized Myasthenia Gravis
ULTOMIRIS is indicated for the treatment of adult patients with generalized myasthenia gravis (gMG) who are anti-acetylcholine receptor (AChR) antibody- positive.
1.4 Neuromyelitis Optica Spectrum Disorder
ULTOMIRIS is indicated for the treatment of adult patients with neuromyelitis optica spectrum disorder (NMOSD) who are anti-aquaporin-4 (AQP4) antibody positive.
ULTOMIRIS is a complement inhibitor indicated for:
-
the treatment of adult and pediatric patients one month of age and older with paroxysmal nocturnal hemoglobinuria (PNH). (1.1)
-
the treatment of adult and pediatric patients one month of age and older with atypical hemolytic uremic syndrome (aHUS) to inhibit complement-mediated thrombotic microangiopathy (TMA). (1.2)
Limitations of Use:
ULTOMIRIS is not indicated for the treatment of patients with Shiga toxin E. coli related hemolytic uremic syndrome (STEC-HUS). -
the treatment of adult patients with generalized myasthenia gravis (gMG) who are anti-acetylcholine receptor (AChR) antibody-positive. (1.3)
-
the treatment of adult patients with neuromyelitis optica spectrum disorder (NMOSD) who are anti-aquaporin-4 (AQP4) antibody positive. (1.4)
CONTRAINDICATIONS SECTION
4 CONTRAINDICATIONS
ULTOMIRIS is contraindicated for initiation in patients with unresolved serious Neisseria meningitidis infection [see Warnings and Precautions (5.1)].
ULTOMIRIS is contraindicated for initiation in patients with unresolved serious Neisseria meningitidis infection. (4)
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Serious Meningococcal Infections
ULTOMIRIS, a complement inhibitor, increases a patient's susceptibility to serious, life-threatening, or fatal infections caused by meningococcal bacteria (septicemia and/or meningitis) in any serogroup, including non- groupable strains. Life-threatening and fatal meningococcal infections have occurred in both vaccinated and unvaccinated patients treated with complement inhibitors. The initiation of ULTOMIRIS treatment is contraindicated in patients with unresolved serious Neisseria meningitidis infection.
Complete or update meningococcal vaccination (for serogroups A, C, W, Y and B) at least 2 weeks prior to administration of the first dose of ULTOMIRIS, according to current ACIP recommendations for patients receiving a complement inhibitor. Revaccinate patients in accordance with ACIP recommendations considering the duration of ULTOMIRIS therapy. Note that ACIP recommends an administration schedule in patients receiving complement inhibitors that differs from the administration schedule in the vaccine prescribing information. If urgent ULTOMIRIS therapy is indicated in a patient who is not up to date with meningococcal vaccines according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer meningococcal vaccines as soon as possible. Various durations and regimens of antibacterial drug prophylaxis have been considered, but the optimal durations and drug regimens for prophylaxis and their efficacy have not been studied in unvaccinated or vaccinated patients receiving complement inhibitors, including ULTOMIRIS. The benefits and risks of treatment with ULTOMIRIS, as well as the benefits and risks of antibacterial drug prophylaxis in unvaccinated or vaccinated patients, must be considered against the known risks for serious infections caused by Neisseria meningitidis.
Vaccination does not eliminate the risk of meningococcal infections, despite development of antibodies following vaccination.
Closely monitor patients for early signs and symptoms of meningococcal infection and evaluate patients immediately if infection is suspected. Inform patients of these signs and symptoms and instruct patients to seek immediate medical care if these signs and symptoms occur. Promptly treat known infections. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early. Consider interruption of ULTOMIRIS in patients who are undergoing treatment for serious meningococcal infection, depending on the risks of interrupting treatment in the disease being treated.
ULTOMIRIS is available only through a restricted program under a REMS [see Warnings and Precautions (5.2)].
5.2 ULTOMIRIS and SOLIRIS REMS
ULTOMIRIS is available only through a restricted program under a REMS called ULTOMIRIS and SOLIRIS REMS, because of the risk of serious meningococcal infections [see Warnings and Precautions (5.1)].
Notable requirements of the ULTOMIRIS and SOLIRIS REMS include the following:
- Prescribers must enroll in the REMS.
- Prescribers must counsel patients about the risk of serious meningococcal infection.
- Prescribers must provide the patients with the REMS educational materials.
- Prescribers must assess patient vaccination status for meningococcal vaccines (against serogroups A, C, W, Y, and B) and vaccinate if needed according to current ACIP recommendations two weeks prior to the first dose of ULTOMIRIS.
- Prescribers must provide a prescription for antibacterial drug prophylaxis if treatment must be started urgently and the patient is not up to date with meningococcal vaccines according to current ACIP recommendations at least two weeks prior to the first dose of ULTOMIRIS.
- Healthcare settings and pharmacies that dispense ULTOMIRIS must be certified in the REMS and must verify prescribers are certified.
- Patients must receive counseling from the prescriber about the need to receive meningococcal vaccines per ACIP recommendations, the need to take antibiotics as directed by the prescriber, and the signs and symptoms of meningococcal infection.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 8 months following treatment with ULTOMIRIS.
Further information is available at www.UltSolREMS.com or 1-888-765-4747.
5.3 Other Infections
Serious infections with Neisseria species (other than Neisseria meningitidis), including disseminated gonococcal infections, have been reported.
ULTOMIRIS blocks terminal complement activation; therefore, patients may have increased susceptibility to infections, especially with encapsulated bacteria, such as infections caused by Neisseria meningitidis but also Streptococcus pneumoniae, Haemophilus influenzae, and to a lesser extent, Neisseria gonorrhoeae. Children treated with ULTOMIRIS may be at increased risk of developing serious infections due to Streptococcus pneumoniae and Haemophilus influenzae type b (Hib). Administer vaccinations for the prevention of Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) infections according to ACIP recommendations. Patients receiving ULTOMIRIS are at increased risk for infections due to these organisms, even if they develop antibodies following vaccination.
5.4 Monitoring Disease Manifestations after ULTOMIRIS Discontinuation
Treatment Discontinuation for PNH
After discontinuing treatment with ULTOMIRIS, closely monitor for signs and symptoms of hemolysis, identified by elevated lactate dehydrogenase (LDH) along with sudden decrease in PNH clone size or hemoglobin, or reappearance of symptoms such as fatigue, hemoglobinuria, abdominal pain, shortness of breath (dyspnea), major adverse vascular event (including thrombosis), dysphagia, or erectile dysfunction. Monitor any patient who discontinues ULTOMIRIS for at least 16 weeks to detect hemolysis and other reactions. If signs and symptoms of hemolysis occur after discontinuation, including elevated LDH, consider restarting treatment with ULTOMIRIS.
Treatment Discontinuation for aHUS
ULTOMIRIS treatment of aHUS should be a minimum duration of 6 months. Due to heterogeneous nature of aHUS events and patient-specific risk factors, treatment duration beyond the initial 6 months should be individualized.
There are no specific data on ULTOMIRIS discontinuation.
After discontinuing treatment with ULTOMIRIS, patients should be monitored for clinical symptoms and laboratory signs of TMA complications for at least 12 months.
TMA complications post-discontinuation can be identified if any of the following is observed:
- Clinical symptoms of TMA include changes in mental status, seizures, angina, dyspnea, thrombosis or increasing blood pressure.
- In addition, at least two of the following laboratory signs observed concurrently and results should be confirmed by a second measurement 28 days apart with no interruption
- a decrease in platelet count of 25% or more as compared to either baseline or to peak platelet count during ULTOMIRIS treatment;
- an increase in serum creatinine of 25% or more as compared to baseline or to nadir during ULTOMIRIS treatment;
- an increase in serum LDH of 25% or more as compared to baseline or to nadir during ULTOMIRIS treatment.
If TMA complications occur after ULTOMIRIS discontinuation, consider reinitiation of ULTOMIRIS treatment or appropriate organ-specific supportive measures.
5.5 Thromboembolic Event Management
The effect of withdrawal of anticoagulant therapy during ULTOMIRIS treatment has not been established. Therefore, treatment with ULTOMIRIS should not alter anticoagulant management.
5.6 Infusion-Related Reactions
Intravenous or subcutaneous administration of ULTOMIRIS may result in systemic infusion-related reactions, including anaphylaxis [see Adverse Reactions (6.3)] and hypersensitivity reactions. In clinical trials, infusion-related reactions occurred in approximately 1 to 7% of patients treated with ULTOMIRIS [see Adverse Reactions (6.1)]. These events included lower back pain, abdominal pain, muscle spasms, drop in blood pressure, elevation in blood pressure, rigors, limb discomfort, drug hypersensitivity (allergic reaction), dysgeusia (bad taste), and drowsiness. These reactions did not require discontinuation of ULTOMIRIS. If signs of cardiovascular instability or respiratory compromise occur, interrupt ULTOMIRIS infusion and institute appropriate supportive measures.
5.7 Allergies to Acrylic Adhesives
The on-body injector of ULTOMIRIS uses acrylic adhesive. For patients with a known allergy to acrylic adhesive, use of this product may result in an allergic reaction. Premedication can be considered, and supportive measures should be instituted if signs of allergy appear.
- Other Infections: Use caution when administering ULTOMIRIS to patients with any other systemic infection. (5.3)
- Infusion-Related Reactions: Monitor during infusion, interrupt for reactions, and institute appropriate supportive measures. (5.6)
- Allergies to Acrylic Adhesives: The on-body injector of ULTOMIRIS uses acrylic adhesive. For patients with a known allergy to acrylic adhesive, use of this product may result in an allergic reaction. (5.7)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Serious Meningococcal Infections [see Warnings and Precautions (5.1)]
- Other Infections [see Warnings and Precautions (5.3)]
- Infusion-Related Reactions [see Warnings and Precautions (5.6)]
- Allergies to Acrylic Adhesives [see Warnings and Precautions (5.7)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Adult Population with PNH Treated with Intravenous ULTOMIRIS
The data described below reflect exposure of 441 adult patients with PNH in Phase 3 studies who received intravenously administered ULTOMIRIS (n = 222) or eculizumab (n = 219) at the recommended dosing regimens with median treatment duration of 6 months for ULTOMIRIS and 6 months for eculizumab. The most frequent adverse reactions (≥ 10%) with ULTOMIRIS were upper respiratory tract infection and headache. Table 11 describes adverse reactions that occurred at a rate of 5% or more among patients treated with ULTOMIRIS in PNH studies.
Serious adverse reactions were reported in 15 (6.8%) patients with PNH receiving ULTOMIRIS. The serious adverse reactions in patients treated with ULTOMIRIS included hyperthermia and pyrexia. No serious adverse reaction was reported in more than 1 patient treated with ULTOMIRIS.
One fatal case of sepsis was identified in a patient treated with ULTOMIRIS.
Table 11: Adverse Reactions Reported in 5% or More of Intravenous ULTOMIRIS-Treated Patients in Complement Inhibitor Naïve and Eculizumab- Experienced Adult Patients with PNH|
Body System |
Number of Patients | |
|---|---|---|
|
ULTOMIRIS (IV) |
Eculizumab | |
| ||
|
Gastrointestinal disorders | ||
|
Diarrhea |
19 (9) |
12 (5) |
|
Nausea |
19 (9) |
19 (9) |
|
Abdominal pain |
13 (6) |
16 (7) |
|
General disorders and administration site conditions | ||
|
Pyrexia |
15 (7) |
18 (8) |
|
Infections and infestations | ||
|
Upper respiratory tract infection* |
86 (39) |
86 (39) |
|
Musculoskeletal and connective tissue disorders | ||
|
Pain in extremity |
14 (6) |
11 (5) |
|
Arthralgia |
11 (5) |
12 (5) |
|
Nervous system disorders | ||
|
Headache |
71 (32) |
57 (26) |
|
Dizziness |
12 (5) |
14 (6) |
Clinically relevant adverse reactions in 1% of patients include infusion- related reactions.
Pediatric Population with PNH Treated with Intravenous ULTOMIRIS
In pediatric patients with PNH (aged 9 to 17 years old) included in the pediatric PNH Phase 3 study, the safety profile appeared similar to that observed in adult patients with PNH and in pediatric and adult patients with aHUS. The most common adverse reactions (> 20%) were upper respiratory tract infection, anemia, abdominal pain, and headache. Table 12 describes the adverse reactions that occurred at a rate of 10% or more among pediatric patients treated with ULTOMIRIS administered intravenously in Study ALXN1210-PNH-304.
Table 12: Adverse Reactions Reported in 10% or More of Intravenous ULTOMIRIS-Treated Pediatric Patients with PNH in Study ALXN1210-PNH-304|
Body System |
Treatment Naïve |
Eculizumab Experienced |
Total |
|---|---|---|---|
|
n (%) |
n (%) |
n (%) | |
| |||
|
Blood and lymphatic system disorders | |||
|
Anemia* |
1 (20) |
2 (25) |
3 (23) |
|
Gastrointestinal disorders | |||
|
Abdominal pain |
0 (0) |
3 (38) |
3 (23) |
|
Constipation |
0 (0) |
2 (25) |
2 (15) |
|
General disorders and administration site conditions | |||
|
Pyrexia |
1 (20) |
1 (13) |
2 (15) |
|
Infections and infestations | |||
|
Upper Respiratory tract infection† |
1 (20) |
6 (75) |
7 (54) |
|
Musculoskeletal and connective tissue disorders | |||
|
Pain in extremity |
0 (0) |
2 (25) |
2 (15) |
|
Nervous system disorders | |||
|
Headache |
1 (20) |
2 (25) |
3 (23) |
Subcutaneous Administration of ULTOMIRIS
In the Phase 3 study ALXN1210-PNH-303 with subcutaneous administration of ULTOMIRIS via the on-body injector for adult patients with PNH, during the 10-week randomization period the most common adverse reactions (≥ 10%) with ULTOMIRIS subcutaneous administration were local injection site reactions, diarrhea, and headache. Table 13 describes adverse reactions that occurred at a rate of 10% or more among adult patients treated with ULTOMIRIS in Study ALXN1210-PNH-303 during the 10-week randomized period.
Table 13: Adverse Reactions Reported in 10% or More of ULTOMIRIS On- Body Delivery System for Subcutaneous Administration (SUBQ)-Treated and Intravenous ULTOMIRIS-Treated Adult Patients with PNH in Study ALXN1210-PNH-303|
Number of Patients | ||
|---|---|---|
|
Body System |
ULTOMIRIS (SUBQ) |
ULTOMIRIS (IV) |
| ||
|
Gastrointestinal disorders | ||
|
Diarrhea |
11 (13) |
2 (4) |
|
General disorders and administration site conditions | ||
|
Injection site reaction* |
23 (27) |
0 (0) |
|
Infections and infestations | ||
|
Upper respiratory tract infection† |
7 (8) |
6 (13) |
|
Nervous system disorders | ||
|
Headache |
11 (13) |
4 (9) |
Atypical Hemolytic Uremic Syndrome (aHUS)
The data described below reflect exposure of 58 adult and 16 pediatric patients with aHUS in single-arm trials who received ULTOMIRIS administered intravenously at the recommended dose and schedule. The most frequent adverse reactions reported in ≥ 20% of patients treated with ULTOMIRIS were upper respiratory tract infection, diarrhea, nausea, vomiting, headache, hypertension, and pyrexia. Table 14, Table 15 and Table 16 describe adverse reactions that occurred at a rate of 10% or more among patients treated with ULTOMIRIS in aHUS studies. Serious adverse reactions were reported in 42 (57%) patients with aHUS receiving ULTOMIRIS. The most frequent serious adverse reactions reported in more than 2 patients (2.7%) treated with ULTOMIRIS were hypertension, pneumonia, and abdominal pain. Four patients died during the ALXN1210-aHUS-311 study. The cause of death was sepsis in 2 patients and intracranial hemorrhage in 1 patient. The fourth patient, who was excluded from the trial after a diagnosis of STEC-HUS, died due to pretreatment cerebral arterial thrombosis.
Table 14: Adverse Reactions Reported in ≥ 10% of Intravenous ULTOMIRIS-Treated Patients with aHUS in Study ALXN1210-aHUS-311|
Body System |
ALXN1210-aHUS-311 | |
|---|---|---|
|
All Grades* |
≥ Grade 3 | |
| ||
|
Blood and lymphatic system disorders | ||
|
Anemia |
8 (14) |
0 (0) |
|
Gastrointestinal disorders | ||
|
Diarrhea |
18 (31) |
2 (3) |
|
Nausea |
15 (26) |
2 (3) |
|
Vomiting |
15 (26) |
2 (3) |
|
Constipation |
8 (14) |
1 (2) |
|
Abdominal pain |
7 (12) |
1 (2) |
|
General disorders and administration site conditions | ||
|
Pyrexia |
11 (19) |
1 (2) |
|
Edema peripheral |
10 (17) |
0 (0) |
|
Fatigue |
8 (14) |
0 (0) |
|
Infections and infestations | ||
|
Upper respiratory tract infection† |
15 (26) |
0 (0) |
|
Urinary tract infection |
10 (17) |
5 (9) |
|
Gastrointestinal infection‡ |
8 (14) |
2 (3) |
|
Metabolism and nutrition disorders | ||
|
Hypokalemia |
6 (10) |
1 (2) |
|
Musculoskeletal and connective tissue disorders | ||
|
Arthralgia |
13 (22) |
0 (0) |
|
Back pain |
7 (12) |
1 (2) |
|
Muscle spasms |
6 (10) |
0 (0) |
|
Pain in extremity |
6 (10) |
0 (0) |
|
Nervous system disorders | ||
|
Headache |
23 (40) |
1 (2) |
|
Psychiatric disorders | ||
|
Anxiety |
8 (14) |
1 (2) |
|
Respiratory, thoracic and mediastinal disorders | ||
|
Cough |
10 (17) |
0 (0) |
|
Dyspnea |
10 (17) |
1 (2) |
|
Skin and subcutaneous tissue disorders | ||
|
Alopecia |
6 (10) |
0 (0) |
|
Dry skin |
6 (10) |
0 (0) |
|
Vascular disorders | ||
|
Hypertension |
14 (24) |
7 (12) |
Clinically relevant adverse reactions include viral tonsilitis (in < 10% of patients) and infusion-related reactions (in 3% of patients).
Table 15: Adverse Reactions Reported in ≥ 10% of Intravenous ULTOMIRIS-Treated Patients with aHUS in Study ALXN1210-aHUS-312|
Body System |
ALXN1210-aHUS-312 | |
|---|---|---|
|
All Grades* |
≥ Grade 3 | |
| ||
|
Blood and lymphatic system disorders | ||
|
Anemia |
2 (13) |
1 (6) |
|
Lymphadenopathy |
2 (13) |
0 (0) |
|
Gastrointestinal disorders | ||
|
Diarrhea |
6 (38) |
0 (0) |
|
Constipation |
4 (25) |
0 (0) |
|
Vomiting |
4 (25) |
1 (6) |
|
Abdominal pain |
3 (19) |
0 (0) |
|
Nausea |
2 (13) |
0 (0) |
|
General disorders and administration site conditions | ||
|
Pyrexia |
8 (50) |
0 (0) |
|
Infections and infestations | ||
|
Upper respiratory tract infection† |
7 (44) |
1 (6) |
|
Gastroenteritis viral |
2 (13) |
2 (13) |
|
Pneumonia |
2 (13) |
1 (6) |
|
Tonsillitis |
2 (13) |
0 (0) |
|
Injury, poisoning and procedural complications | ||
|
Contusion |
3 (19) |
0 (0) |
|
Investigations | ||
|
Vitamin D decreased |
3 (19) |
0 (0) |
|
Metabolism and nutrition disorders | ||
|
Decreased appetite |
2 (13) |
0 (0) |
|
Iron deficiency |
2 (13) |
0 (0) |
|
Musculoskeletal and connective tissue disorders | ||
|
Myalgia |
3 (19) |
0 (0) |
|
Pain in extremity |
2 (13) |
0 (0) |
|
Nervous system disorders | ||
|
Headache |
5 (31) |
0 (0) |
|
Respiratory, thoracic and mediastinal disorders | ||
|
Cough |
3 (19) |
0 (0) |
|
Dyspnea |
2 (13) |
0 (0) |
|
Skin and subcutaneous tissue disorders | ||
|
Rash |
3 (19) |
0 (0) |
|
Vascular disorders | ||
|
Hypertension |
4 (25) |
1 (6) |
|
Hypotension |
2 (13) |
0 (0) |
Clinically relevant adverse reactions in < 10% of patients include viral infection.
Table 16: Adverse Reactions Reported in ≥ 10% of Intravenous ULTOMIRIS-Treated Patients from Birth to 16 Years of Age with aHUS in Study ALXN1210-aHUS-312|
Body System |
ALXN1210-aHUS-312 | |||
|---|---|---|---|---|
|
Age 0 to < 2 |
Age 2 to < 12 |
Age 12 to 16 |
Total | |
|
n (%) |
n (%) |
n (%) |
n (%) | |
| ||||
|
Blood and lymphatic system disorders | ||||
|
Lymphadenopathy |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
Gastrointestinal disorders | ||||
|
Diarrhea |
1 (50) |
3 (25) |
1 (100) |
5 (33) |
|
Constipation |
0 (0) |
4 (33) |
0 (0) |
4 (27) |
|
Vomiting |
0 (0) |
3 (25) |
0 (0) |
3 (20) |
|
Abdominal pain |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
General disorders and administration site conditions | ||||
|
Pyrexia |
1 (50) |
5 (42) |
1 (100) |
7 (47) |
|
Infections and infestations | ||||
|
Upper respiratory tract infection* |
1 (50) |
6 (50) |
0 (0) |
7 (47) |
|
Gastroenteritis viral |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
Tonsillitis |
1 (50) |
1 (8) |
0 (0) |
2 (13) |
|
Injury, poisoning and procedural complications | ||||
|
Contusion |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
Investigations | ||||
|
Vitamin D decreased |
0 (0) |
2 (17) |
1 (100) |
3 (20) |
|
Metabolism and nutrition disorders | ||||
|
Decreased appetite |
1 (50) |
1 (8) |
0 (0) |
2 (13) |
|
Iron deficiency |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
Musculoskeletal and connective tissue disorders | ||||
|
Myalgia |
1 (50) |
1 (8) |
0 (0) |
2 (13) |
|
Pain in extremity |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
|
Nervous system disorders | ||||
|
Headache |
0 (0) |
4 (33) |
0 (0) |
4 (27) |
|
Respiratory, thoracic and mediastinal disorders | ||||
|
Cough |
0 (0) |
3 (25) |
0 (0) |
3 (20) |
|
Dyspnea |
1 (50) |
1 (8) |
0 (0) |
2 (13) |
|
Skin and subcutaneous tissue disorders | ||||
|
Rash |
1 (50) |
2 (17) |
0 (0) |
3 (20) |
|
Vascular disorders | ||||
|
Hypertension |
1 (50) |
3 (25) |
0 (0) |
4 (27) |
|
Hypotension |
0 (0) |
2 (17) |
0 (0) |
2 (13) |
Clinically relevant adverse reactions in < 10% of patients include viral infection.
Generalized Myasthenia Gravis (gMG)
Adult Population with gMG Treated with Intravenous ULTOMIRIS
The safety of ULTOMIRIS has been evaluated in 175 adult patients with gMG, including 169 patients who received at least one dose of intravenously administered ULTOMIRIS, 142 patients who were exposed for at least 6 months, and 95 who were exposed for at least 12 months [see Clinical Studies (14.3)]. In a randomized, double-blind, placebo-controlled trial (ALXN1210-MG-306), the most frequent adverse reactions (≥ 10%) with ULTOMIRIS were diarrhea and upper respiratory tract infection. Table 17 describes adverse reactions that occurred at a rate of 5% or more and at greater frequency than placebo. Serious adverse reactions were reported in 20 (23%) patients with gMG receiving ULTOMIRIS and in 14 (16%) patients receiving placebo. The most frequent serious adverse reactions were infections reported in at least 8 (9%) patients treated with ULTOMIRIS and in 4 (4%) patients treated with placebo [see Warnings and Precautions (5.3)]. Of these infections, one fatal case of COVID-19 pneumonia was identified in a patient treated with ULTOMIRIS and one case of infection led to discontinuation of ULTOMIRIS.
Table 17: Adverse Reactions Reported in ≥ 5% and at Greater Frequency than Placebo in Intravenous ULTOMIRIS-Treated Adult Patients with gMG in Study ALXN1210-MG-306|
Body System |
Number of Patients | |
|---|---|---|
|
ULTOMIRIS (IV) |
Placebo | |
|
Gastrointestinal Disorders | ||
|
Diarrhea |
13 (15) |
11 (12) |
|
Abdominal pain |
5 (6) |
0 |
|
Infections and Infestations | ||
|
Upper respiratory tract infection |
12 (14) |
7 (8) |
|
Urinary tract infection |
5 (6) |
4 (4) |
|
Musculoskeletal and Connective Tissue Disorders | ||
|
Back Pain |
7 (8) |
5 (6) |
|
Nervous System Disorders | ||
|
Dizziness |
8 (9) |
3 (3) |
Neuromyelitis Optica Spectrum Disorder (NMOSD)
Adult Population with NMOSD Treated with Intravenous ULTOMIRIS
The safety of ULTOMIRIS has been evaluated in 58 adult patients with NMOSD who received at least one dose of ULTOMIRIS administered intravenously [see Clinical Studies (14.3)]. In Study ALXN1210-NMO-307, an open-label multicenter trial, the most frequent adverse reactions (≥10%) with ULTOMIRIS were COVID-19, headache, back pain, urinary tract infection and arthralgia.
Table 18 describes adverse reactions that occurred at a rate of 5% or more in patients treated with ULTOMIRIS administered intravenously. Serious adverse reactions were reported in 8 (13.8%) patients with NMOSD receiving ULTOMIRIS.
Table 18: Adverse Reactions Reported in ≥ 5% in Intravenous ULTOMIRIS- Treated Adult Patients with NMOSD in Study ALXN1210-NMO-307|
Body System |
ULTOMIRIS (IV) |
|---|---|
|
Blood and Lymphatic System Disorder | |
|
Lymphadenopathy |
3 (5) |
|
Gastrointestinal Disorders | |
|
Constipation |
4 (7) |
|
Vomiting |
4 (7) |
|
Diarrhea |
3 (5) |
|
Gastroesophageal reflux disease |
3 (5) |
|
General Disorders and Administration Site Reactions | |
|
Pyrexia |
5 (9) |
|
Chills |
3 (5) |
|
Fatigue |
3 (5) |
|
Malaise |
3 (5) |
|
Non-cardiac chest pain |
3 (5) |
|
Vaccination site pain |
3 (5) |
|
Infections and Infestations | |
|
COVID-19 |
14 (24) |
|
Urinary tract infection |
6 (10) |
|
Cystitis |
5 (9) |
|
Upper respiratory tract infection |
5 (9) |
|
Nasopharyngitis |
3 (5) |
|
Sinusitis |
3 (5) |
|
Injury, Poisoning and Procedural Complications | |
|
Infusion related reaction |
4 (7) |
|
Musculoskeletal and Connective Tissue Disorders | |
|
Back pain |
7 (12) |
|
Arthralgia |
6 (10) |
|
Myalgia |
3 (5) |
|
Nervous System Disorders | |
|
Headache |
14 (24) |
|
Dizziness |
4 (7) |
|
Migraine |
3 (5) |
|
Respiratory, thoracic and mediastinal disorders | |
|
Cough |
3 (5) |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of ULTOMIRIS. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to ULTOMIRIS exposure.
Serious Adverse Reaction: Anaphylaxis [see Warnings and Precautions (5.6)]
Most common adverse reactions in patients with PNH (incidence ≥ 10%) were upper respiratory tract infection and headache. Injection site reactions and diarrhea occurred in patients (incidence ≥ 10%) receiving ULTOMIRIS subcutaneously. (6.1)
Most common adverse reactions in patients with aHUS (incidence ≥ 20%) were upper respiratory tract infection, diarrhea, nausea, vomiting, headache, hypertension, and pyrexia. (6.1)
Most common adverse reactions in adult patients with gMG (incidence ≥ 10%) were diarrhea and upper respiratory tract infection. (6.1)
Most common adverse reactions in adult patients with NMOSD (incidence ≥ 10%) were COVID-19, headache, back pain, arthralgia, and urinary tract infection. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alexion Pharmaceuticals, Inc. at 1-844-259-6783 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Plasma Exchange, Plasmapheresis, and Intravenous Immunoglobulins
Concomitant use of ULTOMIRIS with plasma exchange (PE), plasmapheresis (PP), or intravenous immunoglobulin (IVIg) treatment can reduce serum ravulizumab concentrations and requires a supplemental dose of ULTOMIRIS [see Dosage and Administration (2.5)].
7.2 Neonatal Fc Receptor Blockers
Concomitant use of ULTOMIRIS with neonatal Fc receptor (FcRn) blockers (e.g., efgartigimod) may lower systemic exposures and reduce effectiveness of ULTOMIRIS. Closely monitor for reduced effectiveness of ULTOMIRIS.
- Plasma Exchange, Plasmapheresis, or Intravenous Immunoglobulins: concomitant use requires supplemental dose of ULTOMIRIS. (7.1)
- Neonatal Fc Receptor Blockers (FcRn): Closely monitor for reduced effectiveness of ULTOMIRIS. (7.2)
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Boxed Warning |
02/2024 |
|
Indications and Usage (1.4) |
03/2024 |
|
Dosage and Administration (2.2, 2.3, 2.6) |
03/2024 |
|
Contraindications (4) |
02/2024 |
|
Warnings and Precautions (5.1, 5.2, 5.3, 5.6) |
03/2024 |
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage Information
ULTOMIRIS may be administered as an intravenous infusion (ULTOMIRIS vial for intravenous administration) in adult or pediatric patients one month of age and older or as a subcutaneous injection for maintenance (ULTOMIRIS on-body delivery system for subcutaneous administration) in adult patients.
Vials are intended for intravenous use only, and on-body delivery systems (prefilled cartridge and on-body injector) are intended for subcutaneous maintenance use only.
2.2 Recommended Vaccination and Prophylaxis for Meningococcal Infection
Vaccinate patients against meningococcal infection (serogroups A, C, W, Y and B) according to current ACIP recommendations at least 2 weeks prior to initiation of ULTOMIRIS [see Warnings and Precautions (5.1)].
If urgent ULTOMIRIS therapy is indicated in a patient who is not up to date with meningococcal vaccines according to ACIP recommendations, provide the patient with antibacterial drug prophylaxis and administer these vaccines as soon as possible.
Healthcare providers who prescribe ULTOMIRIS must enroll in the ULTOMIRIS and SOLIRIS REMS [see Warnings and Precautions (5.2)].
2.3 Recommended Dosage for Intravenous Administration in Adult and
Pediatric Patients with PNH, aHUS, gMG, or NMOSD
The recommended intravenous ULTOMIRIS loading and maintenance dosing in adult and pediatric patients, one month of age or older weighing 5 kg or greater, with PNH or aHUS, or in adult patients with gMG or NMOSD weighing 40 kg or greater, is based on the patient's body weight, as shown in Table 1, with maintenance doses administered every 4 or 8 weeks, starting 2 weeks after loading dose.
The intravenous (IV) dosing schedule is allowed to occasionally vary within 7 days of the scheduled infusion day (except for the first maintenance dose of ULTOMIRIS); but subsequent doses should be administered according to the original schedule.
Following a missed intravenous ULTOMIRIS dose, the patient should contact their health care provider immediately.
Table 1: ULTOMIRIS Vial for Intravenous (IV) Administration Weight- Based Dosing Regimen – PNH, aHUS, gMG, or NMOSD*|
Indications |
Body Weight Range |
Loading Dose |
Maintenance Dose (mg) and Dosing Interval | |
|---|---|---|---|---|
| ||||
|
PNH or aHUS |
5 to less than 10 |
600 |
300 |
Every 4 weeks |
|
10 to less than 20 |
600 |
600 | ||
|
20 to less than 30 |
900 |
2,100 |
Every 8 weeks | |
|
30 to less than 40 |
1,200 |
2,700 | ||
|
PNH, aHUS, gMG, or NMOSD |
40 to less than 60 |
2,400 |
3,000 |
Every 8 weeks |
|
60 to less than 100 |
2,700 |
3,300 | ||
|
100 or greater |
3,000 |
3,600 |
Refer to Table 2 for treatment initiation instructions in patients who are complement inhibitor treatment-naïve, or switching treatment from subcutaneous (SUBQ) administration of ULTOMIRIS or eculizumab.
Table 2: ULTOMIRIS Vial for Intravenous (IV) Administration Treatment Initiation Instructions – PNH, aHUS, gMG, or NMOSD|
Population |
Weight-based ULTOMIRIS IV Loading Dose |
Time of First ULTOMIRIS IV Weight-based Maintenance Dose |
|---|---|---|
| ||
|
Not currently on ULTOMIRIS or eculizumab treatment |
At treatment start |
2 weeks after ULTOMIRIS IV loading dose |
|
Currently treated with eculizumab |
At time of next scheduled eculizumab dose |
2 weeks after ULTOMIRIS IV loading dose |
|
Currently treated with ULTOMIRIS on-body delivery system for subcutaneous administration (SUBQ)* |
Not applicable |
1 week after last ULTOMIRIS SUBQ maintenance dose |
2.4 Recommended Dosage for Subcutaneous Administration in Adult Patients
with PNH or aHUS
Subcutaneous (SUBQ) dosing of ULTOMIRIS is not approved for use in pediatric patients.
The recommended subcutaneous ULTOMIRIS maintenance dose is 490 mg once weekly in adult patients greater than or equal to 40 kg body weight with PNH or aHUS. The 490 mg dose of ULTOMIRIS is delivered using 2 on-body delivery systems. Each on-body delivery system consists of 1 on-body injector and 1 prefilled cartridge containing 245 mg of ravulizumab.
The subcutaneous dosing schedule is allowed to occasionally vary by ± 1 day of the scheduled dose day, but the subsequent dose should be administered according to the original schedule.
Following a missed or partial subcutaneous ULTOMIRIS dose, the patient should contact their health care provider immediately.
Refer to Table 3 for treatment initiation instructions in patients who are complement inhibitor treatment-naïve or switching treatment from intravenous administration of ULTOMIRIS or eculizumab.
Table 3: ULTOMIRIS On-Body Delivery System for Subcutaneous (SUBQ) Administration Treatment Initiation Instructions – Adults with PNH or aHUS|
Population |
Weight-based ULTOMIRIS IV Loading Dose* |
Time of First ULTOMIRIS 490 mg SUBQ Maintenance Dose |
|---|---|---|
| ||
|
Not currently on ULTOMIRIS or eculizumab treatment |
At treatment start |
2 weeks after ULTOMIRIS IV loading dose |
|
Currently treated with eculizumab |
At time of next scheduled eculizumab dose |
2 weeks after ULTOMIRIS IV loading dose |
|
Currently treated with ULTOMIRIS intravenous (IV) administration |
Not applicable |
8 weeks after last ULTOMIRIS IV maintenance dose |
2.5 Dosing Considerations
Supplemental Dose of ULTOMIRIS
Plasma exchange (PE), plasmapheresis (PP), and intravenous immunoglobulin (IVIg) have been shown to reduce ULTOMIRIS serum levels. A supplemental dose of ULTOMIRIS is required in the setting of PE, PP, or IVIg (Table 4).
Table 4: Supplemental Dose of ULTOMIRIS after PE, PP, or IVIg*|
Body Weight Range (kg) |
Most Recent ULTOMIRIS Dose (mg) |
Supplemental Dose (mg) following each PE or PP Intervention |
Supplemental Dose (mg) following Completion of an IVIg Cycle |
|---|---|---|---|
|
Abbreviations: IVIg = intravenous immunoglobulin; PE = plasma exchange; PP = plasmapheresis | |||
| |||
|
40 to less than 60 |
2,400 |
1,200 |
600 |
|
3,000 |
1,500 | ||
|
60 to less than 100 |
2,700 |
1,500 |
600 |
|
3,300 |
1,800 | ||
|
100 or greater |
3,000 |
1,500 |
600 |
|
3,600 |
1,800 | ||
|
Timing of ULTOMIRIS Supplemental Dose |
Within 4 hours following each PE or PP intervention |
Within 4 hours following completion of an IVIg cycle |
2.6 Preparation and Administration
Preparation of ULTOMIRIS Vials for Intravenous Administration
Each vial of ULTOMIRIS is intended for single-dose only.
ULTOMIRIS vials are for intravenous administration by a healthcare provider and are intended for intravenous administration only.
Dilute before use.
Do not mix ULTOMIRIS 100 mg/mL (3 mL and 11 mL vials) and 10 mg/mL (30 mL vial) concentrations together.
Use aseptic technique to prepare ULTOMIRIS as follows:
The number of vials to be diluted is determined based on the individual patient's weight and the prescribed dose [see Dosage and Administration (2.2)].
Prior to dilution, visually inspect the solution in the vials; the solution should be free of any particulate matter or precipitation. Do not use if there is evidence of particulate matter or precipitation.
Withdraw the calculated volume of ULTOMIRIS from the appropriate number of vials and dilute in an infusion bag using 0.9% Sodium Chloride Injection, USP to a final concentration of:
- 50 mg/mL for the 3 mL and 11 mL vial sizes or
- 5 mg/mL for the 30 mL vial size.
The product should be mixed gently. Do not shake. Protect from light. Do not freeze.
Refer to the following reference tables for IV preparation and minimum infusion duration:
- ULTOMIRIS 100 mg/mL (3 mL and 11 mL vials): see Table 5 (loading doses), Table 6 (maintenance doses), and Table 7 (supplemental doses)
- ULTOMIRIS 10 mg/mL (30 mL vial): see Table 8 (loading doses), Table 9 (maintenance doses), and Table 10 (supplemental doses)
Administer the prepared solution immediately following preparation.
If the diluted ULTOMIRIS infusion solution is not used immediately, storage under refrigeration at 2°C - 8°C (36°F - 46°F) must not exceed 24 hours taking into account the expected infusion time. Once removed from refrigeration, administer the diluted ULTOMIRIS infusion solution within 6 hours if prepared with ULTOMIRIS 30 mL vials or within 4 hours if prepared with ULTOMIRIS 3 mL or 11 mL vials.
Intravenous Administration of ULTOMIRIS (Healthcare Providers)
Only administer as an intravenous infusion through a 0.2 or 0.22 micron filter.
Dilute ULTOMIRIS to a final concentration of:
- 50 mg/mL for the 3 mL and 11 mL vial sizes or
- 5 mg/mL for the 30 mL vial size.
Prior to administration, allow the admixture to adjust to room temperature (18°C - 25°C, 64°F - 77°F). Do not heat the admixture in a microwave or with any heat source other than ambient air temperature.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
After administration of ULTOMIRIS, flush the entire line with 0.9% Sodium Chloride Injection, USP.
Table 5: IV Loading Dose Reference Table for ULTOMIRIS 100 mg/mL (3 mL and 11 mL Vials)|
Body Weight Range |
Loading Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
| ||||||
|
5 to less than 10‡ |
600 |
6 |
6 |
12 |
1.4 |
9 |
|
10 to less than 20‡ |
600 |
6 |
6 |
12 |
0.8 |
15 |
|
20 to less than 30‡ |
900 |
9 |
9 |
18 |
0.6 |
30 |
|
30 to less than 40‡ |
1,200 |
12 |
12 |
24 |
0.5 |
48 |
|
40 to less than 60 |
2,400 |
24 |
24 |
48 |
0.8 |
60 |
|
60 to less than 100 |
2,700 |
27 |
27 |
54 |
0.6 |
90 |
|
100 or greater |
3,000 |
30 |
30 |
60 |
0.4 |
150 |
|
Body Weight Range |
Maintenance Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
| ||||||
|
5 to less than 10‡ |
300 |
3 |
3 |
6 |
0.8 |
8 |
|
10 to less than 20‡ |
600 |
6 |
6 |
12 |
0.8 |
15 |
|
20 to less than 30‡ |
2,100 |
21 |
21 |
42 |
1.3 |
33 |
|
30 to less than 40‡ |
2,700 |
27 |
27 |
54 |
1.1 |
50 |
|
40 to less than 60 |
3,000 |
30 |
30 |
60 |
0.9 |
67 |
|
60 to less than 100 |
3,300 |
33 |
33 |
66 |
0.7 |
95 |
|
100 or greater |
3,600 |
36 |
36 |
72 |
0.5 |
144 |
|
Body Weight Range (kg)* |
Supplemental Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
|
Note: Refer to Table 4 for selection of ravulizumab supplemental dose | ||||||
| ||||||
|
40 to less than 60 |
600 |
6 |
6 |
12 |
0.25 |
48 |
|
1,200 |
12 |
12 |
24 |
0.42 |
57 | |
|
1,500 |
15 |
15 |
30 |
0.5 |
60 | |
|
60 to less than 100 |
600 |
6 |
6 |
12 |
0.20 |
60 |
|
1,500 |
15 |
15 |
30 |
0.36 |
83 | |
|
1,800 |
18 |
18 |
36 |
0.42 |
86 | |
|
100 or greater |
600 |
6 |
6 |
12 |
0.17 |
71 |
|
1,500 |
15 |
15 |
30 |
0.25 |
120 | |
|
1,800 |
18 |
18 |
36 |
0.28 |
129 |
|
Body Weight Range |
Loading Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
| ||||||
|
5 to less than 10‡ |
600 |
60 |
60 |
120 |
3.8 |
32 |
|
10 to less than 20‡ |
600 |
60 |
60 |
120 |
1.9 |
64 |
|
20 to less than 30‡ |
900 |
90 |
90 |
180 |
1.5 |
120 |
|
30 to less than 40‡ |
1,200 |
120 |
120 |
240 |
1.3 |
185 |
|
40 to less than 60 |
2,400 |
240 |
240 |
480 |
1.9 |
253 |
|
60 to less than 100 |
2,700 |
270 |
270 |
540 |
1.7 |
318 |
|
100 or greater |
3,000 |
300 |
300 |
600 |
1.8 |
334 |
|
Body Weight Range |
Maintenance Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
| ||||||
|
5 to less than 10‡ |
300 |
30 |
30 |
60 |
1.9 |
32 |
|
10 to less than 20‡ |
600 |
60 |
60 |
120 |
1.9 |
64 |
|
20 to less than 30‡ |
2,100 |
210 |
210 |
420 |
3.3 |
128 |
|
30 to less than 40‡ |
2,700 |
270 |
270 |
540 |
2.8 |
193 |
|
40 to less than 60 |
3,000 |
300 |
300 |
600 |
2.3 |
261 |
|
60 to less than 100 |
3,300 |
330 |
330 |
660 |
2 |
330 |
|
100 or greater |
3,600 |
360 |
360 |
720 |
2.2 |
328 |
|
Body Weight Range (kg)* |
Supplemental Dose (mg) |
ULTOMIRIS |
Volume of NaCl Diluent† (mL) |
Total Volume (mL) |
Minimum Infusion Time |
Maximum Infusion Rate |
|---|---|---|---|---|---|---|
|
Note: Refer to Table 4 for selection of ravulizumab supplemental dose | ||||||
| ||||||
|
40 to less than 60 |
600 |
60 |
60 |
120 |
0.5 |
240 |
|
1,200 |
120 |
120 |
240 |
1.0 |
240 | |
|
1,500 |
150 |
150 |
300 |
1.2 |
250 | |
|
60 to less than 100 |
600 |
60 |
60 |
120 |
0.4 |
300 |
|
1,500 |
150 |
150 |
300 |
1.0 |
300 | |
|
1,800 |
180 |
180 |
360 |
1.1 |
327 | |
|
100 or greater |
600 |
60 |
60 |
120 |
0.4 |
300 |
|
1,500 |
150 |
150 |
300 |
1.0 |
300 | |
|
1,800 |
180 |
180 |
360 |
1.1 |
327 |
If an adverse reaction occurs during the intravenous administration of ULTOMIRIS, the infusion may be slowed or stopped at the discretion of the physician. Monitor the patient for at least 1 hour following completion of the infusion for signs or symptoms of an infusion-related reaction.
Preparation of ULTOMIRIS On-Body Delivery System for Subcutaneous Administration
ULTOMIRIS on-body delivery system is intended for administration by patients/caregivers. Patients/caregivers may administer after training from a healthcare provider. Refer to the Instructions for Use for detailed instructions on how to use and administer subcutaneous ULTOMIRIS.
- Remove 2 cartons of ULTOMIRIS on-body delivery system for subcutaneous administration from the refrigerator. Two on-body injectors and 2 prefilled cartridges are required for a full dose (490 mg).
- Inspect the packaging. The on-body injectors or cartridges should not be used if they have been dropped or appear to be broken or damaged.
- Wait at least 45 minutes for the on-body injectors and prefilled cartridges in the cartons to naturally reach room temperature prior to administration. Do not return to the refrigerator. Discard after 3 days if unused.
- Before administration, visually inspect the solution. The solution should not be injected if it contains flakes or particles, or is cloudy or discolored.
Subcutaneous Administration of ULTOMIRIS On-Body Delivery System
ULTOMIRIS on-body delivery system is for subcutaneous administration into the abdomen, thigh, or upper arm region. A patient may self-administer, or the patient caregiver may administer ULTOMIRIS on-body delivery system after the healthcare provider determines it is appropriate. Injection sites should be rotated, and injections should not be given into areas where the skin is tender, bruised, red, or hard. Avoid injecting into areas with scars or stretch marks. The 2 on-body delivery systems can be administered concurrently or sequentially. Each injection is delivered over approximately 10 minutes.
- Load the first clean cartridge into the first on-body injector and secure in place before closing the cartridge door on the injector. Do not insert the cartridge more than 5 minutes before the injection to avoid drying out the solution.
- Peel away the adhesive backing of the first on-body injector and apply onto the clean, dry, chosen injection site (thigh, abdomen, or upper arm).
- Start the injection by firmly pressing and releasing the blue start button.
- Do not remove until the injection is complete (signaled by the solid green status light, 3 beeping sounds, and the white plunger filling the medicine window).
- Repeat steps 1-4 for the second on-body injector.
If an allergic reaction occurs during the subcutaneous administration of ULTOMIRIS, treatment should be stopped, the on-body injector(s) should be removed, and the patient should seek medical attention prior to further administration.
The patient should monitor for signs or symptoms of infusion-related reaction for at least 1 hour following completion of the injection.
Any unused medicinal product and waste material should be disposed of in accordance with local requirements.
- See Full Prescribing Information for instructions on dosage, preparation, and administration. (2.1, 2.2, 2.3, 2.4, 2.5, 2.6)
- Dilute ULTOMIRIS before use. (2.6)
- Only administer as an intravenous infusion through a 0.2 or 0.22 micron filter. (2.6)
USE IN SPECIFIC POPULATIONS SECTION
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on ULTOMIRIS use in pregnant women to inform a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with untreated PNH and aHUS in pregnancy (see Clinical Considerations). Animal studies using a mouse analogue of the ravulizumab-cwvz molecule (murine anti- mouse complement component 5 [C5] antibody) showed increased rates of developmental abnormalities and an increased rate of dead and moribund offspring at doses 0.8-2.2 times the human dose (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-associated maternal and/or fetal/neonatal risk
PNH in pregnancy is associated with adverse maternal outcomes, including worsening cytopenias, thrombotic events, infections, bleeding, miscarriages, and increased maternal mortality, and adverse fetal outcomes, including fetal death and premature delivery.
In pregnancy, aHUS is associated with adverse maternal outcomes, including preeclampsia and preterm delivery, and adverse fetal/neonatal outcomes, including intrauterine growth restriction (IUGR), fetal death and low birth weight.
Data
Animal Data
Animal reproduction studies were conducted in mice using doses of a murine anti-C5 antibody that approximated 1-2.2 times (loading dose) and 0.8-1.8 times (maintenance dose) the recommended human ULTOMIRIS dose, based on a body weight comparison. When animal exposure to the antibody occurred in the time period from before mating until early gestation, no decrease in fertility or reproductive performance was observed. When maternal exposure to the antibody occurred during organogenesis, 2 cases of retinal dysplasia and 1 case of umbilical hernia were observed among 230 offspring born to mothers exposed to the higher antibody dose; however, the exposure did not increase fetal loss or neonatal death. When maternal exposure to the antibody occurred in the time period from implantation through weaning, a higher number of male offspring became moribund or died (1/25 controls, 2/25 low dose group, 5/25 high dose group). Surviving offspring had normal development and reproductive function. Human IgG are known to cross the human placental barrier, and thus ULTOMIRIS may potentially cause terminal complement inhibition in fetal circulation.
8.2 Lactation
Risk summary
There are no data on the presence of ravulizumab-cwvz in human milk, the effect on the breastfed child, or the effect on milk production. Since many medicinal products and immunoglobulins are secreted into human milk, and because of the potential for serious adverse reactions in a nursing child, breastfeeding should be discontinued during treatment and for 8 months after the final dose.
8.4 Pediatric Use
The safety and effectiveness of ULTOMIRIS administered intravenously for the treatment of PNH have been established in pediatric patients aged one month and older. Use of ULTOMIRIS for this indication is supported by evidence from adequate and well-controlled trials in adults with additional pharmacokinetic, efficacy and safety data in pediatric patients aged 9 to 17 years [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.1)]. The safety and efficacy for the treatment of pediatric and adult patients with PNH appear similar. Use of ULTOMIRIS administered intravenously in pediatric patients with PNH aged less than 9 years and body weight < 30 kg is based on extrapolation of pharmacokinetic / pharmacodynamic (PK/PD), and efficacy and safety data from aHUS and PNH clinical studies [see Clinical Pharmacology (12.3) and Clinical Studies (14)].
The safety and effectiveness of ULTOMIRIS administered intravenously for the treatment of aHUS have been established in pediatric patients aged one month and older. Use of ULTOMIRIS for this indication is supported by evidence from adequate and well-controlled studies in adults with additional pharmacokinetic, safety, and efficacy data in pediatric patients aged 10 months to < 17 years. The safety and efficacy of ULTOMIRIS administered intravenously for the treatment of aHUS appear similar in pediatric and adult patients [see Adverse Reactions (6.1), and Clinical Studies (14.2)].
The safety and effectiveness of ULTOMIRIS for the treatment of gMG or NMOSD in pediatric patients have not been established.
Subcutaneous administration of ULTOMIRIS has not been evaluated and is not approved for use in pediatric patients.
8.5 Geriatric Use
Clinical studies of ULTOMIRIS did not include sufficient numbers of subjects aged 65 and over (58 patients with PNH, 9 with aHUS, 54 with gMG, and 7 with NMOSD) to determine whether they respond differently from younger subjects.
Other reported clinical experience has not identified differences in responses between elderly and younger patients.
Pediatric Use: Subcutaneous dosing of ULTOMIRIS is not approved for use in pediatric patients. (8.4)
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ravulizumab-cwvz is a terminal complement inhibitor that specifically binds to the complement protein C5 with high affinity, thereby inhibiting its cleavage to C5a (the proinflammatory anaphylatoxin) and C5b (the initiating subunit of the membrane attack complex [MAC or C5b-9]) thus preventing MAC formation. ULTOMIRIS inhibits terminal complement-mediated intravascular hemolysis in patients with PNH and complement-mediated thrombotic microangiopathy (TMA) in patients with aHUS.
The precise mechanism by which ravulizumab-cwvz exerts its therapeutic effect in gMG patients is unknown, but is presumed to involve reduction of terminal complement complex C5b-9 deposition at the neuromuscular junction.
The precise mechanism by which ravulizumab-cwvz exerts its therapeutic effect in NMOSD is unknown, but is presumed to involve inhibition of aquaporin-4 antibody-induced terminal complement C5b-9 deposition.
12.2 Pharmacodynamics
Complete inhibition of serum free C5 (concentration of less than 0.5 mcg/mL) was observed by the end of the first ULTOMIRIS intravenous infusion and sustained throughout the entire 26-week treatment period in both adult and pediatric patients with PNH, in the majority (93%) of adult and pediatric patients with aHUS, in all adult patients with gMG, and in the majority (98.3%) of adult patients with NMOSD.
Complete inhibition of serum free C5 (concentration of less than 0.5 mcg/mL) was observed by the end of the first ULTOMIRIS subcutaneous administration and was sustained throughout the entire treatment period.
The extent and duration of the pharmacodynamic response in patients with PNH, aHUS, gMG, or NMOSD were exposure-dependent for ULTOMIRIS. Free C5 levels of < 0.5 mcg/mL were correlated with maximal intravascular hemolysis control and complete terminal complement inhibition in patients with PNH.
Complete terminal complement inhibition following initiation of ULTOMIRIS intravenous treatment led to normalization of serum LDH by week 4 in complement-inhibitor naïve patients with PNH, and maintained LDH normalization in patients previously treated with eculizumab with PNH [see Clinical Studies (14)].
The PD results following ULTOMIRIS subcutaneous treatment are consistent with results in adult patients with PNH and aHUS treated with intravenous ULTOMIRIS.
12.3 Pharmacokinetics
Following ULTOMIRIS intravenous (IV) treatment, ravulizumab-cwvz pharmacokinetics increase proportionally over a dose range of 200 to 5400 mg. Ravulizumab-cwvz Cmax and Ctrough parameters are presented in Table 19, Table 20, Table 21, and Table 22.
Table 19: Mean (%CV) Pharmacokinetic Parameters Following Intravenous ULTOMIRIS Treatment in Patients with PNH who are Complement Inhibitor-Naïve and Patients Previously Treated with Eculizumab|
Pediatric Patients |
Adult Patients | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
ALXN1210-PNH-304 |
ALXN1210-PNH-301 |
ALXN1210-PNH-302 | |||||||
|
N |
Complement Inhibitor-Naïve |
N |
Previously Treated with Eculizumab |
N |
Complement Inhibitor-Naïve |
N |
Previously Treated with Eculizumab | ||
|
Abbreviations: LD = Loading Dose; MD = Maintenance Dose | |||||||||
|
Cmax |
LD |
4 |
733 (14.5) |
8 |
885 (19.3) |
125 |
771 (21.5) |
95 |
843 (24.1) |
|
MD |
4 |
1490 (26.7) |
8 |
1705 (9.7) |
124 |
1,379 (20.0) |
95 |
1,386 (19.4) | |
|
Ctrough |
LD |
4 |
368 (14.7) |
8 |
452 (15.1) |
125 |
391 (35.0) |
96 |
405 (29.9) |
|
MD |
4 |
495 (21.3) |
8 |
566 (12.2) |
124 |
473 (33.4) |
95 |
501 (28.6) |
|
Pediatric Patients |
Adult Patients | ||||||
|---|---|---|---|---|---|---|---|
|
N |
< 20 kg |
N |
≥ 20 to < 40 kg |
N |
≥ 40 kg | ||
|
Abbreviations: LD = Loading Dose; MD = Maintenance Dose; Q4W = Every 4 Weeks; Q8W = Every 8 Weeks | |||||||
|
Cmax |
LD |
8 |
656 (38.1) |
4 |
600 (17.3) |
52 |
754 (35.2) |
|
MD |
7 |
1,467 (37.8) |
6 |
1,863 (15.3) |
46 |
1,458 (17.6) | |
|
Ctrough |
LD |
9 |
241 (52.1) |
5 |
186 (16.5) |
55 |
313 (33.9) |
|
MD |
7 |
683 (46.1) |
6 |
549 (34.1) |
46 |
507 (42.5) |
|
N |
Adult Patients (ALXN1210-MG-306) | ||
|---|---|---|---|
|
Abbreviations: LD = Loading Dose; MD=Maintenance Dose | |||
|
Cmax |
LD |
86 |
874 (21.1) |
|
MD |
76 |
1548 (23.2) | |
|
Ctrough |
LD |
85 |
418 (27.6) |
|
MD |
70 |
587 (29.6) |
|
N |
Adult Patients (ALXN1210-NMO-307) | ||
|---|---|---|---|
|
Abbreviations: LD = Loading Dose; MD=Maintenance Dose | |||
|
Cmax |
LD |
58 |
935.3 (17.3) |
|
MD |
56 |
1836.4 (19.4) | |
|
Ctrough |
LD |
58 |
459.1 (19.7) |
|
MD |
54 |
796.9 (27.1) |
Following ULTOMIRIS subcutaneous (SUBQ) treatment, the mean (%CV) ravulizumab- cwvz trough concentration at steady state is 737.7 (28.3%) mcg/mL.
The estimated bioavailability of ULTOMIRIS subcutaneous treatment is approximately 79%.
Distribution
The mean (standard deviation [SD]) volume of distribution at steady state in patients with PNH, aHUS, gMG, or NMOSD are shown in Table 23.
Elimination
The mean (standard deviation [SD]) terminal elimination half-life and clearance of ravulizumab-cwvz are shown in Table 23.
Table 23: Distribution, Biotransformation, and Elimination Parameters Following Intravenous ULTOMIRIS or ULTOMIRIS On-Body Delivery System for Subcutaneous Administration (SUBQ) Treatment|
Adult and Pediatric Patients with PNH |
Adult and Pediatric Patients with aHUS |
Adult Patients with gMG |
Adult Patients with NMOSD |
Adult Patients with PNH | |
|---|---|---|---|---|---|
| |||||
|
Distribution | |||||
|
Volume of distribution at steady state (liters) |
5.30 (0.95) |
5.22 (1.85) |
5.74 (1.16) |
4.77 (0.819) |
5.30 (0.95)* |
|
Biotransformation and Elimination | |||||
|
Terminal elimination half-life (days) |
49.6 (9.08) |
51.8 (16.2) |
56.6 (8.36) |
64.3 (11.0) |
52.4 (9.72) |
|
Clearance (liters/day) |
0.08 (0.02) |
0.08 (0.04) |
0.08 (0.02) |
0.05 (0.016) |
0.07 (0.02)* |
Specific Populations
No clinically significant differences in the pharmacokinetics of ravulizumab- cwvz were observed based on sex, age (10 months to 83 years), race, hepatic impairment, or any degree of renal impairment, including patients with proteinuria or receiving dialysis.
Body weight was a clinically significant covariate on the pharmacokinetics of ravulizumab-cwvz.
Drug Interactions
No drug-drug interaction studies have been performed.
Neonatal Fc Receptor blocker treatment may interfere with the endosomal neonatal FcRn recycling mechanism of monoclonal antibodies such as ravulizumab and thereby decrease serum ravulizumab concentrations [see Drug Interactions (7.1, 7.2)].
Concomitant PE, PP, or IVIg treatment requires a supplemental dose of ULTOMIRIS [see Dosage and Administration (2.5)].
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of ULTOMIRIS or other ravulizumab-cwvz products.
The immunogenicity of ravulizumab-cwvz has been evaluated using an enzyme- linked immunosorbent assay (ELISA) for the detection of binding anti- ravulizumab-cwvz antibodies. For patients whose sera tested positive in the screening immunoassay, an in vitro biological assay was performed to detect neutralizing antibodies.
In clinical studies with intravenous administration of ULTOMIRIS, treatment- emergent antibodies to ravulizumab-cwvz were detected in 1 of 219 (0.5%) patients with PNH [see Clinical Studies (14.1)] and 1 of 71 (1.4%) patients with aHUS [see Clinical Studies (14.2)]. In these 2 patient populations, the observed ADA were non-neutralizing with no apparent impact on PK, safety, or efficacy. In the gMG study (N=86) and NMOSD study (N=58), no treatment- emergent antibodies to ravulizumab-cwvz were detected [see Clinical Studies (14.3 & 14.4)].
In patients receiving subcutaneous administration of ULTOMIRIS (N=128), there were no treatment-emergent anti-drug antibodies observed.
However, the assay used to measure anti-drug antibodies (ADA) is subject to interference by serum ravulizumab-cwvz, possibly resulting in an underestimation of the incidence of antibody formation. Due to the limitation of the assay conditions, the potential clinical impact of antibodies to ravulizumab-cwvz is not known.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patients and/or caregivers to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Serious Meningococcal Infections
Advise patients of the risk of serious meningococcal infection. Inform patients of the need to complete or update their meningococcal vaccinations at least 2 weeks prior to receiving the first dose of ULTOMIRIS or receive antibacterial drug prophylaxis if ULTOMIRIS treatment must be initiated immediately and they have not been previously vaccinated. Inform patients of the requirement to be revaccinated according to current ACIP recommendations for meningococcal infection while on ULTOMIRIS therapy [see Warnings and Precautions (5.1)].
Inform patients that vaccination may not prevent serious meningococcal infection and to seek immediate medical attention if the following signs or symptoms occur [see Warnings and Precautions (5.1)]:
- fever
- fever and a rash
- headache with nausea or vomiting
- fever with high heart rate
- headache and a fever
- headache with a stiff neck or stiff back
- confusion
- muscle aches with flu-like symptoms
- eyes sensitive to light
Inform patients that they will be given a Patient Safety Card for ULTOMIRIS that they should carry with them at all times during and for 8 months following treatment with ULTOMIRIS. This card describes symptoms which, if experienced, should prompt the patient to immediately seek medical evaluation.
ULTOMIRIS and SOLIRIS REMS
ULTOMIRIS is available only through a restricted program called ULTOMIRIS and SOLIRIS REMS [see Warnings and Precautions (5.2)].
Inform the patient of the following notable requirements:
- Patients must receive counseling about the risk of serious meningococcal infections.
- Patients must receive written educational materials about this risk.
- Patients must be instructed to carry the Patient Safety Card with them at all times during and for 8 months following treatment with ULTOMIRIS.
- Patients must be instructed to complete or update meningococcal vaccines for serogroups A, C, W, Y and B per ACIP recommendations as directed by the prescriber prior to treatment with ULTOMIRIS.
- Patients must receive antibiotics as directed by the prescriber if they are not up to date with meningococcal vaccines and have to start ULTOMIRIS right away.
Other Infections
Counsel patients of the increased risk of infections, particularly those due to encapsulated bacteria, especially Neisseria species. Advise patients of the need for vaccination against meningococcal infections according to current medical guidelines. Counsel patients about gonorrhea prevention and advise regular testing for patients at risk. Advise patients to report any new signs and symptoms of infection.
Discontinuation
Inform patients with PNH or aHUS that they may develop serious hemolysis or TMA, respectively, when ULTOMIRIS is discontinued and that they will be monitored by their healthcare professional for at least 16 weeks for PNH or at least 12 months for aHUS following ULTOMIRIS discontinuation [see Warnings and Precautions (5.4)].
Inform patients who discontinue ULTOMIRIS to keep the Patient Safety Card with them for 8 months after the last ULTOMIRIS dose, because the increased risk of meningococcal infection persists for several months following discontinuation of ULTOMIRIS.
Infusion-Related Reactions
Advise patients that administration of ULTOMIRIS may result in infusion- related reactions [see Warnings and Precautions (5.6)].
Allergies to Acrylic Adhesives
Advise patients that the single-use on-body injector used in subcutaneous administration of ULTOMIRIS contains acrylic adhesive that may cause allergic reactions to individuals sensitive to acrylic adhesives [see Warnings and Precautions (5.7)].
Administration
Provide training to patients and caregivers on proper subcutaneous administration technique and how to use the single-use on-body injector with prefilled cartridge correctly.
Inform patients that 2 on-body delivery systems (on-body injector with prefilled -cartridge) are required for a full dose.
Additionally, inform patients that it will take about 10 minutes to administer each ULTOMIRIS on-body delivery system for subcutaneous administration.
The single-use on-body injector with prefilled cartridge is not made with natural rubber latex.
SPL UNCLASSIFIED SECTION
Manufactured by:
Alexion Pharmaceuticals, Inc.
121 Seaport Boulevard
Boston, MA 02210 USA
US License Number 1743
This product, or its use, may be covered by one or more US patents, including US Patent No. 9,079,949; 9,107,861; 9,206,251; 9,371,377; 9,663,574; 9,803,007; 10,227,400; 10,584,164; and 11,365,241 in addition to others including patents pending.
ULTOMIRIS is a trademark of Alexion Pharmaceuticals, Inc.
© 2024 Alexion Pharmaceuticals, Inc.
SPL MEDGUIDE SECTION
|
This Medication Guide has been approved by the U.S. Food and Drug Administration. |
Revised: 03/2024 | ||
|
MEDICATION GUIDE | |||
|
What is the most important information I should know about ULTOMIRIS? | |||
|
ULTOMIRIS increases your chance of getting serious meningococcal infections caused by**Neisseria meningitidis*** bacteria**.Meningococcal infections may quickly become life-threatening or cause death if not recognized and treated early. * You must complete or update your meningococcal vaccine(s) at least 2 weeks before your first dose of ULTOMIRIS. * If you have not completed your meningococcal vaccines and ULTOMIRIS must be started right away, you should receive the required vaccine(s) as soon as possible. * If you have not been vaccinated and ULTOMIRIS must be started right away, you should also receive antibiotics to take for as long as your healthcare provider tells you. * If you had a meningococcal vaccine in the past, you might need additional vaccines before starting ULTOMIRIS. Your healthcare provider will decide if you need additional meningococcal vaccines. * Meningococcal vaccines do not prevent all meningococcal infections.Call your healthcare provider or get emergency medical care right away if you get any of these signs and symptoms of a serious meningococcal infection: | |||
|
| ||
|
Your healthcare provider will give you a Patient Safety Card about the risk of serious meningococcal infection. Carry it with you at all times during treatment and for 8 months after your last dose of ULTOMIRIS. Your risk of meningococcal infection may continue for several months after your last dose of ULTOMIRIS. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly. | |||
|
ULTOMIRIS is only available through a program called the ULTOMIRIS and SOLIRIS Risk Evaluation and Mitigation Strategy (REMS). Before you can receive ULTOMIRIS, your healthcare provider must: | |||
| |||
|
ULTOMIRIS may also increase the risk of other types of serious infections caused by encapsulated bacteria, including Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria gonorrhoeae**.** | |||
| |||
|
For more information about side effects, see**"What are the possible side effects of ULTOMIRIS?"** | |||
|
What is ULTOMIRIS? | |||
|
ULTOMIRIS is a prescription medicine called a monoclonal antibody. ULTOMIRIS is used to treat:
| |||
|
It is not known if ULTOMIRIS is safe and effective in children younger than 1
month of age. | |||
|
Who should not receive ULTOMIRIS? | |||
|
Before you receive ULTOMIRIS, tell your healthcare provider about all of your medical conditions, including if you: | |||
| |||
|
Tell your healthcare provider about all the medicines you take, including
prescription and over-the-counter medicines, vitamins, and herbal supplements.
ULTOMIRIS and other medicines can affect each other causing side effects. | |||
|
How should I receive ULTOMIRIS? | |||
| |||
|
Adults with PNH, aHUS, gMG, or NMOSD when administered intravenously (by vein) | |||
| |||
|
Children 1 month of age and older with PNH or aHUS when administered intravenously (by vein) | |||
|
Your child will be given intravenous ULTOMIRIS infusion by a healthcare provider through a needle placed in a vein | |||
| |||
|
Adults with PNH or aHUS when administered subcutaneously (under your skin) | |||
| |||
|
If you are changing treatment between ULTOMIRIS administered intravenously, ULTOMIRIS administered subcutaneously, or SOLIRIS: | |||
|
*From intravenous ULTOMIRIS to subcutaneous ULTOMIRIS, you should receive your first dose of subcutaneous ULTOMIRIS 8 weeks after your last dose of intravenous ULTOMIRIS. No intravenous ULTOMIRIS starting dose is needed. *From subcutaneous ULTOMIRIS to intravenous ULTOMIRIS, you should receive your first dose of intravenous ULTOMIRIS 1 week after your last dose of subcutaneous ULTOMIRIS. *From SOLIRIS to intravenous ULTOMIRIS, you should receive your starting dose of intravenous ULTOMIRIS at time of your next scheduled dose of SOLIRIS. *From SOLIRIS to subcutaneous ULTOMIRIS, you should receive your starting dose of intravenous ULTOMIRIS at time of your next scheduled dose of SOLIRIS, and then your first dose of subcutaneous ULTOMIRIS 2 weeks after your starting dose of intravenous ULTOMIRIS.
| |||
|
| ||
| |||
|
| ||
|
If you miss an ULTOMIRIS intravenous or subcutaneous dose, or administer a partial subcutaneous dose of ULTOMIRIS, call your healthcare provider right away. | |||
|
What are the possible side effects of ULTOMIRIS? | |||
|
ULTOMIRIS can cause serious side effects including: See***"What is the most important information I should know about ULTOMIRIS?"**** *Infusion-related reactions. Infusion-related reactions may happen during your ULTOMIRIS intravenous or subcutaneous treatment. Symptoms of an infusion-related reaction with ULTOMIRIS may include lower back pain, abdominal pain, muscle spasms, changes in blood pressure, tiredness, feeling faint, shaking chills (rigors), discomfort in your arms or legs, bad taste, or drowsiness. Stop treatment of ULTOMIRIS and tell your healthcare provider right away if you develop these symptoms, or any other symptoms during your ULTOMIRIS infusion that may mean you are having a serious infusion-related reaction, including: | |||
|
| ||
|
*Allergic reactions to acrylic adhesive. Allergic reactions to the acrylic adhesive may happen with your subcutaneous ULTOMIRIS treatment. If you have an allergic reaction during the delivery of subcutaneous ULTOMIRIS, remove the on-body injector and get medical help right away. Your healthcare provider may treat you with medicines to help prevent or treat allergic reaction symptoms as needed. | |||
|
The most common side effects of ULTOMIRIS in people treated for PNH are: | |||
|
| ||
|
The most common side effects of ULTOMIRIS in people treated for aHUS are: | |||
|
| ||
|
The most common side effects of ULTOMIRIS in people with gMG are: | |||
|
| ||
|
The most common side effects of ULTOMIRIS in people with NMOSD are: | |||
|
| ||
|
Tell your healthcare provider about any side effect that bothers you or that
does not go away. | |||
|
General information about the safe and effective use of ULTOMIRIS. | |||
|
What are the ingredients in ULTOMIRIS? | |||
|
Active ingredient: ravulizumab-cwvz. | |||
|
Inactive ingredients: | |||
|
Intravenous: | |||
|
ULTOMIRIS 100 mg/mL: L-arginine, polysorbate 80 (vegetable origin), sodium phosphate dibasic, sodium phosphate monobasic, sucrose and Water for Injection. | |||
|
ULTOMIRIS 10 mg/mL: polysorbate 80 (vegetable origin), sodium chloride, sodium phosphate dibasic, sodium phosphate monobasic and Water for Injection. | |||
|
Subcutaneous: | |||
|
ULTOMIRIS 70 mg/mL: L-arginine, polysorbate 80 (vegetable origin), sodium phosphate dibasic, sodium phosphate monobasic, sucrose, and Water for Injection. | |||
|
Manufactured by Alexion Pharmaceuticals, Inc., 121 Seaport Boulevard, Boston,
MA 02210 USA. | |||
INSTRUCTIONS FOR USE SECTION
|
This Instructions for Use has been approved by the U.S. Food and Drug Administration. |
Issued: 07/2022 | ||||||
|
INSTRUCTIONS FOR USE | |||||||
|
Single-Use, On-Body Injector and 245 mg/3.5 mL Prefilled Cartridge | |||||||
|
This Instructions for Use contains information on how to inject ULTOMIRIS subcutaneously using an on-body delivery system. | |||||||
|
Read this Instructions for Use prior to each use of the ULTOMIRIS on-body injector and prefilled cartridge as there may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment. See the Medication Guide that comes with ULTOMIRIS for important information. | |||||||
|
Important Information You Need to Know Before Injecting ULTOMIRIS Subcutaneously | |||||||
| |||||||
|
|
1 Full Dose of ULTOMIRIS = |
| |||||
|
Guide to Parts | |||||||
|
Prefilled cartridge (Also referred to as "Cartridge") | |||||||
|
| |||||||
|
On-Body Injector (Also referred to as "Injector") | |||||||
|
| |||||||
|
Important: Needle is inside. | |||||||
|
Important | |||||||
|
Storing your ULTOMIRIS on-body injector and prefilled cartridge: | |||||||
| |||||||
|
Using your ULTOMIRIS on-body injector and prefilled cartridge: | |||||||
|
*Do not shake or drop the injector or cartridge. *Do not remove the injector or cartridge from the carton or clear tray until you are ready to inject. *Do not press the blue start button on the injector until you place the loaded injector onto your skin and are ready to inject. *After you insert the cartridge into the injector,make sure you inject within 5 minutes. Loading the cartridge more than 5 minutes before your injection can dry out the medicine. *Do not use the injector or cartridge if the packaging appears to be opened, or if the injector or cartridge has been dropped or appears to be broken or damaged. Part of the on-body injector or prefilled cartridge may be broken even if you cannot see the damage. *Do not reuse the on-body injector and prefilled cartridge.They are single-use only. *Do not let the injector get wet from water or other liquids. It contains electronic parts that should not get wet.
| |||||||
|
Step 1: Prepare | |||||||
|
1A |
Remove2 ULTOMIRIS on-body delivery system cartons from the refrigerator. You will need to use2 injectors and2 cartridges for a full dose. (See Figure A) | ||||||
|
| |||||||
|
1B |
Wait at least45 minutes. | ||||||
|
Important: Wait at least45 minutes for the injectors and cartridges in the cartons to naturally reach room temperature. (See Figure B) | |||||||
|
*Do not use a microwave, hot water, hair dryer, or any other heat sources to warm the prefilled cartridge. *Do not return to the refrigerator. The injectors and cartridges may be stored in the original carton box at room temperature between 68°F to 77°F (20°C to 25°C) for up to 3 days. Throw away (discard) after 3 days if unused. | |||||||
|
See the Frequently Asked Questions section for additional information on returning the on-body injector and prefilled cartridge to the refrigerator. | |||||||
|
| |||||||
|
1C |
Open the cartons and peel away the white paper covers (See Figure C). Remove the plastic covers from the clear trays using the finger hole (See Figure D). | ||||||
|
|
| ||||||
|
Leave the injectors and cartridges in the trays until ready to use. | |||||||
|
*Do not touch the blue start button until the injectors are on your skin and you are ready to inject. *Do not use if the white paper cover(s) or plastic cover(s) is missing or damaged. If either is missing, call 1-888-765-4747. | |||||||
|
1D |
Gather all supplies needed for your injection and then wash your hands with soap and water. You can also wear gloves. | ||||||
|
On a clean, well-lit work surface, place the: | |||||||
|
*2 clear trays containing the on-body injectors and prefilled cartridges (See Figure E) | |||||||
|
| |||||||
|
Additional supplies (See Figure F): | |||||||
| |||||||
|
| |||||||
|
1E |
Prepare and clean2 different injection sites. Wipe both injection sites with a new alcohol wipe and let your skin air dry. (See Figure G) | ||||||
|
The sites you may choose are: | |||||||
|
| |||||||
|
*Do not inject into areas of the skin that are tender, bruised, red or hard, or areas with wrinkles, skin folds, scars, tattoos, stretch marks, moles, or excessive hair. *Do not use the same sites 2 weeks in a row. Change (rotate) your injection sites every week to reduce irritation. | |||||||
|
REPEAT Steps 2A - 3C for each injection | |||||||
|
Step 2: Get Ready | |||||||
|
2A |
Swing open the blue cartridge door (See Figure H). Leave the door open.Do not close the cartridge door before the cartridge is loaded. | ||||||
|
The door should not be closed when removed from the package. If the door is closed,press firmly on theribbed side of the door andswing the door to open. (See Figure I) | |||||||
|
|
| ||||||
|
2B |
Inspect the cartridge. (See Figure J) | ||||||
|
| |||||||
|
Check the expiration date.Do not use the cartridge if the expiration date has passed. | |||||||
|
Check the medicine in the cartridge. The medicine should be clear and colorless to slightly yellow in color. | |||||||
|
*Do not use if the medicine is cloudy, discolored, or contains flakes or particles. *Do not use if any part of cartridge looks cracked, broken, or if pieces are missing. | |||||||
|
In any of the above cases, use a new on-body injector and prefilled cartridge and contact 1-888-765-4747. | |||||||
|
2C |
Clean the cartridge bottom with a new alcohol wipe. (See Figure K) | ||||||
|
| |||||||
|
With 1 hand, hold the prefilled cartridge barrel in the middle. | |||||||
|
*Do not hold it by the ends. *Do not turn (rotate) or remove the top or bottom of the cartridge. *Do not touch the cartridge bottom after cleaning. | |||||||
|
2D |
Load the cleaned cartridge into the injector andgently press on the top until it is secured in place. (See Figure L) | ||||||
|
Insert the cartridge into the injector with the arrow pointing down (bottom first). | |||||||
| |||||||
|
| |||||||
|
Important: Do not insert the cartridge more than 5 minutes before your injection. This can dry out the medicine. See the Frequently Asked Questions section for more information. | |||||||
|
2E |
Close the cartridge door. Squeeze it firmly until it snaps shut and there are no gaps between the injector and the cartridge door. (See Figure M) | ||||||
|
Do not re-open door or remove the cartridge. | |||||||
|
Do not touch the blue start button until you have placed the injector onto your skin or the injectorwill not work. | |||||||
|
| |||||||
|
Important: Go to the next step right away after loading the cartridge and closing the door. | |||||||
|
Step 3: Inject | |||||||
|
3A |
Peel away both green pull tabs to show adhesive. (See Figure N) | ||||||
|
| |||||||
|
The Injector will turn on when the smaller pull tab is removed (along with battery strip). | |||||||
|
You will hear 3 "beeps" repeating every 30 seconds until the blue button is pressed. | |||||||
|
The status light will begin to flash blue. | |||||||
|
*Do not pull the skin adhesive backing off of the injector. *Do not touch the skin adhesive. *Do not touch the start button until you have placed the loaded injector onto your skin.
| |||||||
|
3B |
Stick the injector onto the clean, dry, chosen injection site(s). (See Figure O) | ||||||
|
| |||||||
|
Place the injector so that: | |||||||
| |||||||
|
Firmly press the injector onto the skin. | |||||||
|
Run your finger around the adhesive edges to make sure the adhesive is secure. | |||||||
|
*Do not move the loaded injector after it has been placed onto your skin. | |||||||
|
Important: If placing on stomach, stretch any loose skin as shown with 1 hand. Standing up may make this easier. | |||||||
|
3C |
Firmly press and release the blue start button on the injector to start the injection. (See Figure P) | ||||||
|
| |||||||
| |||||||
|
Important: If you have a serious allergic reaction (such as chest pain, trouble breathing, facial swelling, and/or feeling faint),remove the injector(s) to stop the injection and get medical help right away. | |||||||
|
3D |
REPEAT Steps 2A - 3C with thesecond injector. | ||||||
|
You must use 2 injectors to receive 1 full dose. | |||||||
|
When the second injector is activated, continue to Step 4. | |||||||
|
| |||||||
|
Step 4: Monitor | |||||||
|
4A |
Monitor both injectors until they are complete. Each injection takes about 10 minutes to finish. (See Figure Q) | ||||||
|
The Injection is complete when each injector: | |||||||
| |||||||
|
|
| ||||||
|
Step 5: Removal and Disposal | |||||||
|
5A |
Remove the injectors after both injections are complete. Grip the adhesive and peel the injectors off your skin. (See Figure R) | ||||||
|
The green status light will turn off when the injector is removed from your
skin. | |||||||
|
| |||||||
|
5B |
Dispose of (throw away) the used ULTOMIRIS on-body injectors and prefilled cartridges. (See Figure S) | ||||||
| |||||||
|
| |||||||
|
5C |
Check the injection sites. | ||||||
| |||||||
|
Troubleshooting | |||||||
|
What do I do if the loaded on-body injector status light flashes red and I hear "beeps"? | |||||||
|
Important: If the status light turns red, injector leaks, or either injector does not complete injection, remove and call 1-888-765-4747 immediately (See Figure T). | |||||||
|
A red status light indicates that the injector will not work. | |||||||
|
| |||||||
|
Frequently Asked Questions | |||||||
|
How many on-body injectors do I need for a full dose? | |||||||
| |||||||
|
What happens if the status light flashes red and I hear beeps? | |||||||
| |||||||
|
I cannot open the blue cartridge door. How do I open it? | |||||||
| |||||||
|
What if the on-body injector does not beep and the blue status light does not blink when I remove the pull tabs? | |||||||
| |||||||
|
What if I push the blue start button before I stick the on-body injector on the skin? | |||||||
| |||||||
|
What if the on-body injector is already on the skin but does not start after pressing the blue start button? | |||||||
| |||||||
|
What if a part of the packaging is missing or damaged (for example: carton, paper cover, plastic cover, etc.)? | |||||||
|
*Do not use the on-body injector or prefilled cartridge and contact 1-888-765-4747. | |||||||
|
What happens if I do not inject within 5 minutes after loading the prefilled cartridge? | |||||||
| |||||||
|
If I am not ready to inject after waiting at least 45 minutes, can I return the on-body injector and prefilled cartridge to the refrigerator? | |||||||
|
*Do not return to the refrigerator the on-body injectors and prefilled cartridges after they reach room temperature. This may degrade the medicine. If needed, the on-body injectors and prefilled cartridges may be stored in the original carton box at room temperature between 68°F to 77°F (20°C to 25°C) for up to 3 days. Throw away after 3 days if unused. | |||||||
|
For any additional questions or support, contact1-888-765-4747. | |||||||
|
Additional Environmental Conditions | |||||||
| |||||||
|
Symbol Table | |||||||
|
|
|
|
|
|
| ||
|
|
|
|
|
|
| ||
|
|
| ||||||
|
Manufactured by: |
DOSAGE FORMS & STRENGTHS SECTION
3 DOSAGE FORMS AND STRENGTHS
Intravenous:
- Injection: 300 mg/3 mL (100 mg/mL) as a translucent, clear to yellowish color solution in a single-dose vial
- Injection: 1,100 mg/11 mL (100 mg/mL) as a translucent, clear to yellowish color solution in a single-dose vial
- Injection: 300 mg/30 mL (10 mg/mL) as a clear to translucent, slight whitish color solution in a single-dose vial
Subcutaneous:
- Injection: 245 mg/3.5 mL (70 mg/mL) as a translucent, clear to yellowish color solution in a single-dose prefilled cartridge for use only with supplied single-use on-body injector
Intravenous
Injection: 300 mg/30 mL (10 mg/mL) solution in a single-dose vial. (3)
Injection: 300 mg/3 mL (100 mg/mL) solution in a single-dose vial. (3)
Injection: 1,100 mg/11 mL (100 mg/mL) solution in a single-dose vial. (3)
Subcutaneous
Injection: 245 mg/3.5 mL (70 mg/mL) solution in a single-dose prefilled cartridge for use only with supplied single-use on-body injector. (3)
DESCRIPTION SECTION
11 DESCRIPTION
Ravulizumab-cwvz, a complement inhibitor, is a humanized monoclonal antibody (mAb) produced in Chinese hamster ovary (CHO) cells. Ravulizumab-cwvz consists of 2 identical 448 amino acid heavy chains and 2 identical 214 amino acid light chains and has a molecular weight of approximately 148 kDa. The constant regions of ravulizumab-cwvz include the human kappa light chain constant region, and the protein engineered "IgG2/4" heavy chain constant region.
The heavy chain CH1 domain, hinge region, and the first 5 amino acids of the CH2 domain match the human IgG2 amino acid sequence, residues 6 to 36 in the CH2 region (common to both human IgG2 and IgG4 amino acid sequences), while the remainder of the CH2 domain and the CH3 domain match the human IgG4 amino acid sequence. The heavy and light chain variable regions that form the human C5 binding site consist of human framework regions grafted to murine complementarity-determining regions.
Intravenous:
ULTOMIRIS 100 mg/mL (3 mL and 11 mL vials)
ULTOMIRIS (ravulizumab-cwvz) injection 100 mg/mL is a sterile, translucent, clear to yellowish color, preservative-free solution for intravenous use. Each single-dose vial contains 300 mg or 1,100 mg ravulizumab-cwvz at a concentration of 100 mg/mL with a pH of 7.4. Each mL also contains L-arginine (4.33 mg), polysorbate 80 (0.5 mg) (vegetable origin), sodium phosphate dibasic (4.42 mg), sodium phosphate monobasic (4.57 mg), sucrose (50 mg) and Water for Injection, USP.
ULTOMIRIS 10 mg/mL (30 mL vial)
ULTOMIRIS (ravulizumab-cwvz) injection 10 mg/mL is a sterile, clear to translucent, slight whitish color, preservative-free solution for intravenous use. Each single-dose vial contains 300 mg ravulizumab-cwvz at a concentration of 10 mg/mL with a pH of 7.0. Each mL also contains polysorbate 80 (0.2 mg) (vegetable origin), sodium chloride (8.77 mg), sodium phosphate dibasic (1.78 mg), sodium phosphate monobasic (0.46 mg), and Water for Injection, USP.
Subcutaneous:
ULTOMIRIS 70 mg/mL (3.5 mL prefilled cartridge and on-body injector)
ULTOMIRIS (ravulizumab-cwvz) injection 70 mg/mL is a sterile, translucent, clear to yellowish color, preservative-free solution for subcutaneous use. Each on-body delivery system (single-dose prefilled cartridge only for use with single-use on-body injector) delivers a 3.5 mL solution containing 245 mg of ravulizumab-cwvz, L-arginine (15.2 mg), polysorbate 80 (1.75 mg) (vegetable origin), sodium phosphate dibasic (15.4 mg), sodium phosphate monobasic (16.1 mg), sucrose (175 mg), and Water for Injection, USP with a pH of 7.4.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal carcinogenicity studies of ravulizumab-cwvz have not been conducted.
Genotoxicity studies have not been conducted with ravulizumab-cwvz.
Effects of ravulizumab-cwvz upon fertility have not been studied in animals. Intravenous injections of male and female mice with a murine anti-C5 antibody at up to 0.8-2.2 times the equivalent of the clinical dose of ULTOMIRIS had no adverse effects on mating or fertility.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Intravenous:
ULTOMIRIS (ravulizumab-cwvz) injection 100 mg/mL is translucent, clear to yellowish color solution supplied in one single-dose vial per carton as:
- 300 mg/3 mL (100 mg/mL) (NDC 25682-025-01)
- 1,100 mg/11 mL (100 mg/mL) (NDC 25682-028-01)
ULTOMIRIS (ravulizumab-cwvz) injection 10 mg/mL is clear to translucent, slight whitish color solution supplied in one single-dose vial per carton as:
- 300 mg/30 mL (10 mg/mL) (NDC 25682-022-01)
Subcutaneous:
ULTOMIRIS (ravulizumab-cwvz) injection 70 mg/mL is translucent, clear to yellowish color solution supplied in one single-dose cartridge as part of a single-use on-body delivery system:
- 245 mg/3.5 mL (70 mg/mL) carton containing one prefilled cartridge co-packaged with one on-body injector: NDC 25682-031-01
16.2 Storage and Handling
Intravenous:
Store ULTOMIRIS vials refrigerated at 2°C - 8°C (36°F - 46°F) in the original carton to protect from light. Do not freeze. Do not shake.
Refer to Dosage and Administration (2) for information on the stability and storage of diluted solutions of ULTOMIRIS.
Subcutaneous:
Store ULTOMIRIS prefilled cartridges and on-body injectors refrigerated at 2°C
- 8°C (36°F - 46°F) in the original carton to protect from light and physical damage. Do not freeze. Do not shake or drop. Do not allow the on-body injector to get wet from water or other liquids.
If removed from the refrigerator, store ULTOMIRIS on-body injector and prefilled cartridge in the original carton box at room temperature between 68°F - 77°F (20°C - 25°C) for up to 3 days. If stored at room temperature, discard after 3 days. Do not return to the refrigerator.
The single-use on-body injector with prefilled cartridge is not made with natural rubber latex.



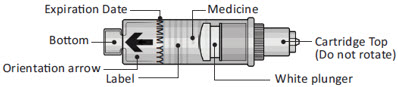
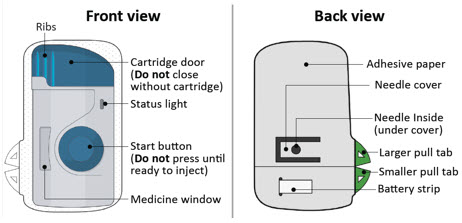


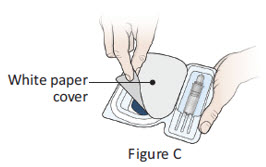
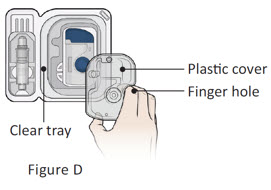
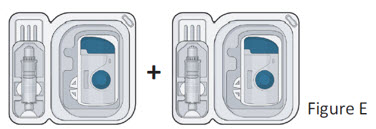

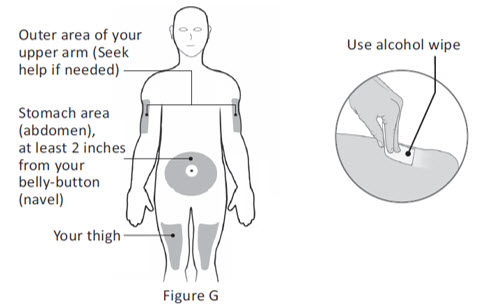
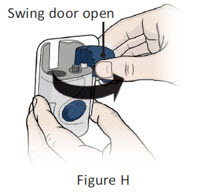
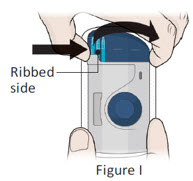
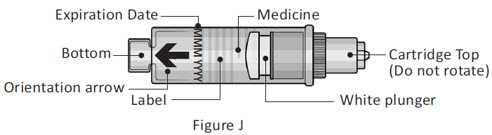
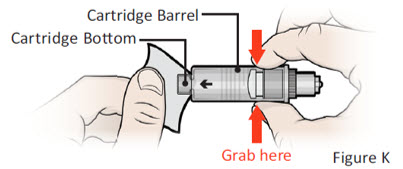
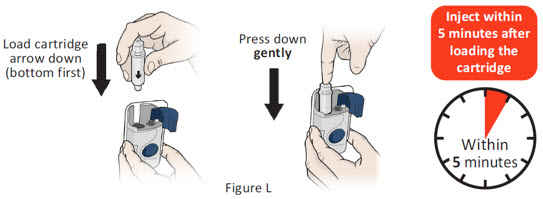

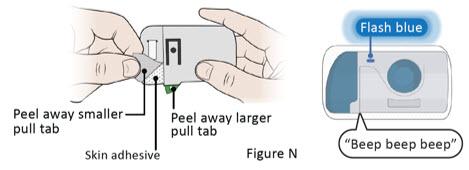
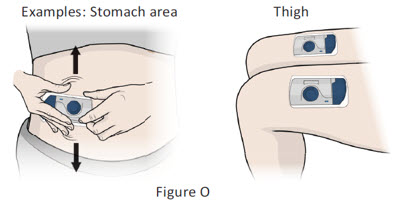
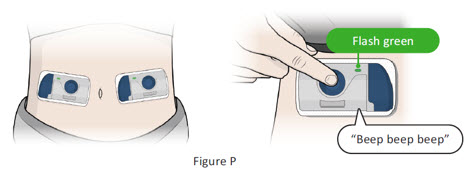

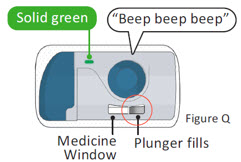

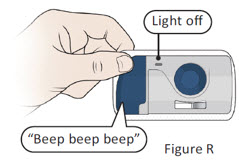

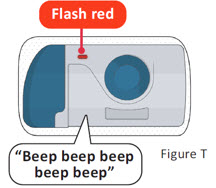
 Refer to
Instructions for Use
Refer to
Instructions for Use Do not use
if packaging is damaged
Do not use
if packaging is damaged Keep Dry
Keep Dry Single Use
Single Use Type BF Applied
Part
Type BF Applied
Part Sterilized using
ethylene oxide
Sterilized using
ethylene oxide Caution
Caution Use-By Date
Use-By Date Batch Code
Batch Code Catalogue Number
Catalogue Number ULTOMIRIS On-
Body Delivery System
ULTOMIRIS On-
Body Delivery System Open Here
Open Here Serial Number
Serial Number MR Unsafe
MR Unsafe