Diazepam
Diazepam Tablets USP C-IV
75661b9e-576a-4bde-aecd-587fdfdf1c28
HUMAN PRESCRIPTION DRUG LABEL
Jul 6, 2023
Mayne Pharma Commercial LLC
DUNS: 867220261
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Diazepam
PRODUCT DETAILS
INGREDIENTS (5)
Diazepam
PRODUCT DETAILS
INGREDIENTS (4)
Diazepam
PRODUCT DETAILS
INGREDIENTS (5)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
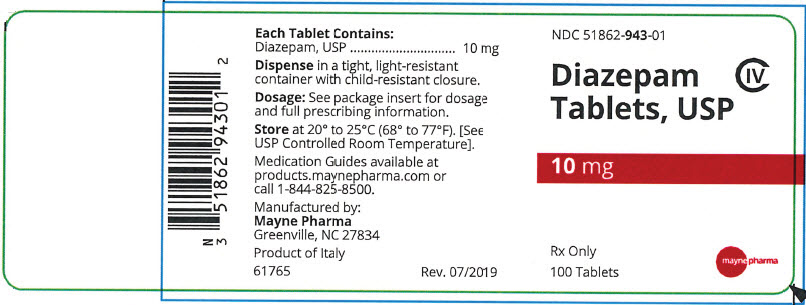
PRINCIPAL DISPLAY PANEL - 10 mg Tablet Bottle Label
NDC 51862-943-01
Diazepam
Tablets, USP
CIV
10 mg
Rx Only
100 Tablets
mayne pharma
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS
Side effects most commonly reported were drowsiness, fatigue, muscle weakness, and ataxia. The following have also been reported:
**Central Nervous System:**confusion, depression, dysarthria, headache, slurred speech, tremor, vertigo
**Gastrointestinal System:**constipation, nausea, gastrointestinal disturbances
**Special Senses:**blurred vision, diplopia, dizziness
**Cardiovascular System:**hypotension
**Psychiatric and Paradoxical Reactions:**stimulation, restlessness, acute hyperexcited states, anxiety, agitation, aggressiveness, irritability, rage, hallucinations, psychoses, delusions, increased muscle spasticity, insomnia, sleep disturbances, and nightmares. Inappropriate behavior and other adverse behavioral effects have been reported when using benzodiazepines. Should these occur, use of the drug should be discontinued. They are more likely to occur in children and in the elderly.
**Urogenital System:**incontinence, changes in libido, urinary retention
**Skin and Appendages:**skin reactions
**Laboratories:**elevated transaminases and alkaline phosphatase
**Other:**changes in salivation, including dry mouth, hypersalivation
Antegrade amnesia may occur using therapeutic dosages, the risk increasing at higher dosages. Amnestic effects may be associated with inappropriate behavior.
Minor changes in EEG patterns, usually low-voltage fast activity, have been observed in patients during and after diazepam therapy and are of no known significance.
Because of isolated reports of neutropenia and jaundice, periodic blood counts and liver function tests are advisable during long-term therapy.
Postmarketing Experience
Injury, Poisoning and Procedural Complications
There have been reports of falls and fractures in benzodiazepine users. The risk is increased in those taking concomitant sedatives (including alcohol), and in the elderly.
PRECAUTIONS SECTION
PRECAUTIONS
General
If diazepam is to be combined with other psychotropic agents or anticonvulsant drugs, careful consideration should be given to the pharmacology of the agents to be employed - particularly with known compounds that may potentiate the action of diazepam, such as phenothiazines, narcotics, barbiturates, MAO inhibitors and other antidepressants (seeDrug Interactions).
The usual precautions are indicated for severely depressed patients or those in whom there is any evidence of latent depression or anxiety associated with depression, particularly the recognition that suicidal tendencies may be present and protective measures may be necessary.
Psychiatric and paradoxical reactions are known to occur when using benzodiazepines (seeADVERSE REACTIONS). Should this occur, use of the drug should be discontinued. These reactions are more likely to occur in children and the elderly.
A lower dose is recommended for patients with chronic respiratory insufficiency, due to the risk of respiratory depression.
Benzodiazepines should be used with extreme caution in patients with a history of alcohol or drug abuse (seeDRUG ABUSE AND DEPENDENCE).
In debilitated patients, it is recommended that the dosage be limited to the smallest effective amount to preclude the development of ataxia or oversedation (2 mg to 2.5 mg once or twice daily, initially, to be increased gradually as needed and tolerated).
Some loss of response to the effects of benzodiazepines may develop after repeated use of diazepam for a prolonged time.
Information for Patients
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Risks from Concomitant Use with Opioids
Advise both patients and caregivers about the risks of potentially fatal respiratory depression and sedation when diazepam is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined (see WARNINGS: Risks from Concomitant Use with Opioidsand PRECAUTIONS: Drug Interactions).
Abuse, Misuse, and Addiction
Inform patients that the use of diazepam tablets, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug (see WARNING : Abuse, Misuse, and Addictionand DRUG ABUSE AND DEPENDENCE).
Withdrawal Reactions
Inform patients that the continued use of diazepam tablets may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of diazepam tablets may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage reduction of diazepam tablets may require a slow taper (see WARNINGS: Dependence and Withdrawal Reactionsand DRUG ABUSE AND DEPENDENCE).
Patients should be advised against the simultaneous ingestion of alcohol and other CNS-depressant drugs during diazepam therapy. As is true of most CNS- acting drugs, patients receiving diazepam should be cautioned against engaging in hazardous occupations requiring complete mental alertness, such as operating machinery or driving a motor vehicle.
Drug Interactions
Opioids
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABA Asites and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and monitor patients closely for respiratory depression and sedation.
Centrally Acting Agents
If diazepam is to be combined with other centrally acting agents, careful consideration should be given to the pharmacology of the agents employed particularly with compounds that may potentiate or be potentiated by the action of diazepam, such as phenothiazines, antipsychotics, anxiolytics/sedatives, hypnotics, anticonvulsants, narcotic analgesics, anesthetics, sedative antihistamines, narcotics, barbiturates, MAO inhibitors and other antidepressants.
Alcohol
Concomitant use with alcohol is not recommended due to enhancement of the sedative effect.
Antacids
Diazepam peak concentrations are 30% lower when antacids are administered concurrently. However, there is no effect on the extent of absorption. The lower peak concentrations appear due to a slower rate of absorption, with the time required to achieve peak concentrations on average 20 - 25 minutes greater in the presence of antacids. However, this difference was not statistically significant.
Compounds Which Inhibit Certain Hepatic Enzymes
There is a potentially relevant interaction between diazepam and compounds which inhibit certain hepatic enzymes (particularly cytochrome P450 3A and 2C19). Data indicate that these compounds influence the pharmacokinetics of diazepam and may lead to increased and prolonged sedation. At present, this reaction is known to occur with cimetidine, ketoconazole, fluvoxamine, fluoxetine, and omeprazole.
Phenytoin
There have also been reports that the metabolic elimination of phenytoin is decreased by diazepam.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In studies in which mice and rats were administered diazepam in the diet at a dose of 75 mg/kg/day (approximately 6 and 12 times, respectively, the maximum recommended human dose [MRHD=1 mg/kg/day] on a mg/m 2basis) for 80 and 104 weeks, respectively, an increased incidence of liver tumors was observed in males of both species. The data currently available are inadequate to determine the mutagenic potential of diazepam. Reproduction studies in rats showed decreases in the number of pregnancies and in the number of surviving offspring following administration of an oral dose of 100 mg/kg/day (approximately 16 times the MRHD on a mg/m 2basis) prior to and during mating and throughout gestation and lactation. No adverse effects on fertility or offspring viability were noted at a dose of 80 mg/kg/day (approximately 13 times the MRHD on a mg/m 2basis).
Pregnancy
Category D
(seeWARNINGS: Pregnancy).
Pediatric Use
Safety and effectiveness in pediatric patients below the age of 6 months have not been established.
Geriatric Use
In elderly patients, it is recommended that the dosage be limited to the smallest effective amount to preclude the development of ataxia or oversedation (2 mg to 2.5 mg once or twice daily, initially to be increased gradually as needed and tolerated).
Extensive accumulation of diazepam and its major metabolite, desmethyldiazepam, has been noted following chronic administration of diazepam in healthy elderly male subjects. Metabolites of this drug are known to be substantially excreted by the kidney, and the risk of toxic reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Hepatic Insufficiency
Decreases in clearance and protein binding, and increases in volume of distribution and half-life has been reported in patients with cirrhosis. In such patients, a 2- to 5- fold increase in mean half-life has been reported. Delayed elimination has also been reported for the active metabolite desmethyldiazepam. Benzodiazepines are commonly implicated in hepatic encephalopathy. Increases in half-life have also been reported in hepatic fibrosis and in both acute and chronic hepatitis (seeCLINICAL PHARMACOLOGY: Pharmacokinetics in Special Populations: Hepatic Insufficiency).
OVERDOSAGE SECTION
OVERDOSAGE
Overdose of benzodiazepines is usually manifested by central nervous system depression ranging from drowsiness to coma. In mild cases, symptoms include drowsiness, confusion, and lethargy. In more serious cases, symptoms may include ataxia, diminished reflexes, hypotonia, hypotension, respiratory depression, coma (rarely), and death (very rarely). Overdose of benzodiazepines in combination with other CNS depressants (including alcohol) may be fatal and should be closely monitored.
Management of Overdosage
Following overdose with oral benzodiazepines, general supportive measures should be employed including the monitoring of respiration, pulse, and blood pressure. Vomiting should be induced (within 1 hour) if the patient is conscious. Gastric lavage should be undertaken with the airway protected if the patient is unconscious. Intravenous fluids should be administered. If there is no advantage in emptying the stomach, activated charcoal should be given to reduce absorption. Special attention should be paid to respiratory and cardiac function in intensive care. General supportive measures should be employed, along with intravenous fluids, and an adequate airway maintained. Should hypotension develop, treatment may include intravenous fluid therapy, repositioning, judicious use of vasopressors appropriate to the clinical situation, if indicated, and other appropriate countermeasures. Dialysis is of limited value.
As with the management of intentional overdosage with any drug, it should be considered that multiple agents may have been ingested.
Flumazenil, a specific benzodiazepine-receptor antagonist, is indicated for the complete or partial reversal of the sedative effects of benzodiazepines and may be used in situations when an overdose with a benzodiazepine is known or suspected. Prior to the administration of flumazenil, necessary measures should be instituted to secure airway, ventilation and intravenous access. Flumazenil is intended as an adjunct to, not as a substitute for, proper management of benzodiazepine overdose. Patients treated with flumazenil should be monitored for resedation, respiratory depression and other residual benzodiazepine effects for an appropriate period after treatment. The prescriber should be aware of a risk of seizure in association with flumazenil treatment, particularly in long-term benzodiazepine users and in cyclic antidepressant overdose**.Caution should be observed in the use of flumazenil in epileptic patients treated with benzodiazepines. The complete flumazenil package insert, includingCONTRAINDICATIONS****, WARNINGS,andPRECAUTIONS**, should be consulted prior to use.
Withdrawal symptoms of the barbiturate type have occurred after the discontinuation of benzodiazepines (seeDRUG ABUSE AND DEPENDENCE).
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
Dosage should be individualized for maximum beneficial effect. While the usual daily dosages given below will meet the needs of most patients, there will be some who may require higher doses. In such cases dosage should be increased cautiously to avoid adverse effects.
|
ADULTS: |
USUAL DAILY DOSE: |
|---|---|
|
Management of Anxiety Disorders and Relief of Symptoms of Anxiety. |
Depending upon severity of symptoms – 2 mg to 10 mg, 2 to 4 times daily |
|
Symptomatic Relief in Acute Alcohol Withdrawal. |
10 mg, 3 or 4 times during the first 24 hours, reducing to 5 mg, 3 or 4 times daily as needed |
|
Adjunctively for Relief of Skeletal Muscle Spasm. |
2 mg to 10 mg, 3 or 4 times daily |
|
Adjunctively in Convulsive Disorders |
2 mg to 10 mg, 2 to 4 times daily |
|
Geriatric Patients, or in the presence of debilitating disease. |
2 mg to 2.5 mg, 1 or 2 times daily initially; increase gradually as needed and tolerated |
|
PEDIATRIC PATIENTS: | |
|
Because of varied responses to CNS-acting drugs, initiate therapy with lowest dose and increase as required. Not for use in pediatric patients under 6 months. |
1 mg to 2.5 mg, 3 or 4 times daily initially; increase gradually as needed and tolerated |
Discontinuation or Dosage Reduction of Diazepam
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue diazepam tablets or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly (see WARNINGS: Dependence and Withdrawal Reactionsand DRUG ABUSE AND DEPENDENCE: Dependence).
HOW SUPPLIED SECTION
HOW SUPPLIED
Diazepam Tablets USP 2 mg are white, flat-faced, bevel edge, bisected tablets imprinted MYX/941 on one side and 2 imprinted on the other side. Supplied in bottles of 100 (NDC 51862-941-01) and 500 (NDC 51862-941-05) tablets.
Diazepam Tablets USP 5 mg are yellow, flat-faced, bevel edge, bisected tablets imprinted MYX/942 on one side and 5 imprinted on the other side. Supplied in bottles of 100 (NDC 51862-942-01), 500 (NDC 51862-942-05) and 1000 (NDC 51862-942-10) tablets.
Diazepam Tablets USP 10 mg are light blue, flat-faced, bevel edge, bisected tablets imprinted MYX/943 on one side and 10 imprinted on the other side. Supplied in bottles of 100 (NDC 51862-943-01), 500 (NDC 51862-943-05) and 1000 (NDC 51862-943-10) tablets.
STORAGE
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Dispense in tight, light-resistant container with child-resistant closure.
