Products (3)
Heparin Sodium
25021-400
ANDA090808
ANDA (C73584)
INTRAVENOUS, SUBCUTANEOUS
June 30, 2017
Heparin Sodium
25021-402
ANDA090808
ANDA (C73584)
INTRAVENOUS, SUBCUTANEOUS
June 30, 2017
Heparin Sodium
25021-403
ANDA090808
ANDA (C73584)
INTRAVENOUS, SUBCUTANEOUS
June 30, 2017
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
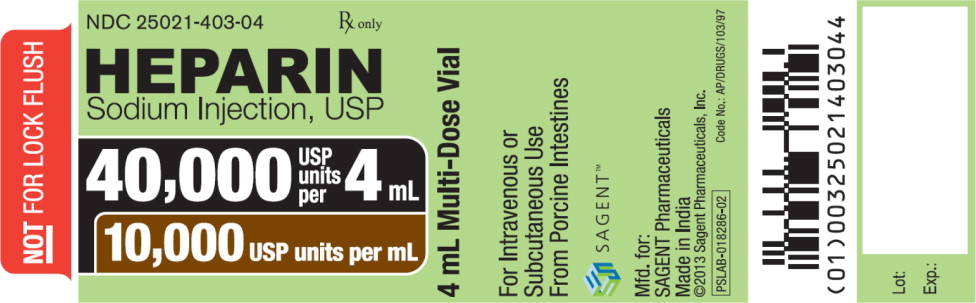
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NOT FOR LOCK FLUSH
NDC 25021-403-04
Rx only
HEPARIN Sodium Injection, USP
40,000 USP units per 40 mL
10,000 USP units per mL
4 mL Multi-Dose Vial
DESCRIPTION SECTION
11 DESCRIPTION
Heparin is a heterogeneous group of straight-chain anionic mucopolysaccharides, called glycosaminoglycans, possessing anticoagulant properties. It is composed of polymers of alternating derivations of α-D- glucosamido (N-sulfated, O-sulfated, or N-acetylated) and O-sulfated uronic acid (α-L-iduronic acid or β-D-glucuronic acid).
Structure of heparin sodium (representative subunits):

Heparin Sodium Injection, USP is a sterile solution of heparin sodium derived from porcine intestinal mucosa, standardized for anticoagulant activity. It is to be administered by intravenous or deep subcutaneous routes. The potency is determined by a biological assay using a USP reference standard based on units of heparin activity per milligram.
Heparin Sodium Injection, USP preserved with Benzyl Alcohol is available in the following concentrations per mL:
|
Heparin Sodium |
Sodium Chloride |
Benzyl Alcohol |
|---|---|---|
|
1,000 USP units |
8.6 mg |
10.42 mg |
|
5,000 USP units |
7 mg |
10.42 mg |
|
10,000 USP units |
5 mg |
10.42 mg |
pH 5.0 to 7.5; sodium hydroxide and/or hydrochloric acid added, if needed, for pH adjustment.
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Heparin interacts with the naturally occurring plasma protein, Antithrombin III, to induce a conformational change, which markedly enhances the serine protease activity of Antithrombin III, thereby inhibiting the activated coagulation factors involved in the clotting sequence, particularly Xa and IIa. Small amounts of heparin inhibit Factor Xa, and larger amounts inhibit thrombin (Factor IIa). Heparin also prevents the formation of a stable fibrin clot by inhibiting the activation of the fibrin stabilizing factor. Heparin does not have fibrinolytic activity; therefore, it will not lyse existing clots.
12.2 Pharmacodynamics
Various times (activated clotting time, activated partial thromboplastin time, prothrombin time, whole blood clotting time) are prolonged by full therapeutic doses of heparin; in most cases, they are not measurably affected by low doses of heparin. The bleeding time is usually unaffected by heparin.
12.3 Pharmacokinetics
Absorption
Heparin is not absorbed through the gastrointestinal tract and therefore administered via parenteral route. Peak plasma concentration and the onset of action are achieved immediately after intravenous administration.
Distribution
Heparin is highly bound to antithrombin, fibrinogens, globulins, serum proteases and lipoproteins. The volume of distribution is 0.07 L/kg.
Elimination
Metabolism
Heparin does not undergo enzymatic degradation.
Excretion
Heparin is mainly cleared from the circulation by liver and reticuloendothelial cells mediated uptake into extravascular space. Heparin undergoes biphasic clearance, a) rapid saturable clearance (zero order process due to binding to proteins, endothelial cells and macrophage) and b) slower first order elimination. The plasma half-life is dose-dependent and it ranges from 0.5 to 2 h.
Specific Populations
Geriatric patients
Patients over 60 years of age, following similar doses of heparin, may have higher plasma levels of heparin and longer activated partial thromboplastin times (APTTs) compared with patients under 60 years of age [see Use in Specific Populations (8.5)].
INDICATIONS & USAGE SECTION
Highlight: Heparin Sodium Injection is an anticoagulant indicated for (1)
- Prophylaxis and treatment of venous thrombosis and pulmonary embolism
- Prevention of postoperative deep venous thrombosis and pulmonary embolism in patients undergoing major abdominothoracic surgery or who, for other reasons, are at risk of developing thromboembolic disease
- Atrial fibrillation with embolization
- Treatment of acute and chronic consumptive coagulopathies (disseminated intravascular coagulation)
- Prevention of clotting in arterial and cardiac surgery
- Prophylaxis and treatment of peripheral arterial embolism
- Use as an anticoagulant in blood transfusions, extracorporeal circulation, and dialysis procedures
1 INDICATIONS AND USAGE
Heparin Sodium Injection is indicated for:
- Prophylaxis and treatment of venous thrombosis and pulmonary embolism
- Prevention of postoperative deep venous thrombosis and pulmonary embolism in patients undergoing major abdominothoracic surgery or who, for other reasons, are at risk of developing thromboembolic disease
- Atrial fibrillation with embolization
- Treatment of acute and chronic consumptive coagulopathies (disseminated intravascular coagulation)
- Prevention of clotting in arterial and cardiac surgery
- Prophylaxis and treatment of peripheral arterial embolism
- Anticoagulant use in blood transfusions, extracorporeal circulation, and dialysis procedures
CONTRAINDICATIONS SECTION
Highlight: * Severe thrombocytopenia (4)
- When suitable blood coagulation tests, e.g., the whole blood clotting time, partial thromboplastin time, etc., cannot be performed at appropriate intervals (4)
- An uncontrolled active bleeding state, except when this is due to disseminated intravascular coagulation (4)
4 CONTRAINDICATIONS
The use of heparin sodium is contraindicated in patients with the following conditions:
- History of heparin-induced thrombocytopenia and heparin-induced thrombocytopenia and thrombosis [see Warnings and Precautions (5.3)]
- Known hypersensitivity to heparin or pork products (e.g., anaphylactoid reactions) [see Adverse Reactions (6.1)]
- In whom suitable blood coagulation tests, e.g., the whole blood clotting time, partial thromboplastin time, etc., cannot be performed at appropriate intervals (this contraindication refers to full-dose heparin; there is usually no need to monitor coagulation parameters in patients receiving low-dose heparin)
- An uncontrolled active bleeding state [see Warnings and Precautions (5.4)], except when this is due to disseminated intravascular coagulation
WARNINGS AND PRECAUTIONS SECTION
Highlight: * Fatal Medication Errors: Confirm choice of correct strength prior to administration (5.1)
- Hemorrhage: Fatal cases have occurred. Use caution in conditions with increased risk of hemorrhage (5.2)
- HIT and HITTS: Monitor for signs and symptoms and discontinue if indicative of HIT and HITTS (5.3)
- Benzyl Alcohol Toxicity: Do not use this product in neonates and infants. (5.4)
- Monitoring: Blood coagulation tests guide therapy for full-dose heparin.
- Monitor platelet count and hematocrit in all patients receiving heparin (5.5, 5.6)
5 WARNINGS AND PRECAUTIONS
5.1 Fatal Medication Errors
Do not use heparin sodium as a “catheter lock flush” product. Heparin sodium is supplied in vials containing various strengths of heparin, including vials that contain a highly concentrated solution of 10,000 units in 1 mL. Fatal hemorrhages have occurred in pediatric patients due to medication errors in which 1 mL heparin sodium vials were confused with 1 mL “catheter lock flush” vials. Carefully examine all heparin sodium vials to confirm the correct vial choice prior to administration of the drug.
5.2 Hemorrhage
Avoid using heparin in the presence of major bleeding, except when the benefits of heparin therapy outweigh the potential risks.
Hemorrhage can occur at virtually any site in patients receiving heparin. Fatal hemorrhages have occurred. Adrenal hemorrhage (with resultant acute adrenal insufficiency), ovarian hemorrhage, and retroperitoneal hemorrhage have occurred during anticoagulant therapy with heparin [see Adverse Reactions (6.1)]. A higher incidence of bleeding has been reported in patients, particularly women, over 60 years of age [see Clinical Pharmacology (12.3)]. An unexplained fall in hematocrit, fall in blood pressure or any other unexplained symptom should lead to serious consideration of a hemorrhagic event.
Use heparin sodium with caution in disease states in which there is increased risk of hemorrhage, including:
- Cardiovascular - Subacute bacterial endocarditis, severe hypertension.
- Surgical - During and immediately following (a) spinal tap or spinal anesthesia or (b) major surgery, especially involving the brain, spinal cord, or eye.
- Hematologic - Conditions associated with increased bleeding tendencies, such as hemophilia, thrombocytopenia and some vascular purpuras.
- Patients with hereditary antithrombin III deficiency receiving concurrent antithrombin III therapy -The anticoagulant effect of heparin is enhanced by concurrent treatment with antithrombin III (human) in patients with hereditary antithrombin III deficiency. To reduce the risk of bleeding, reduce the heparin dose during concomitant treatment with antithrombin III (human).
- Gastrointestinal - Ulcerative lesions and continuous tube drainage of the stomach or small intestine.
- Other - Menstruation, liver disease with impaired hemostasis.
5.3 Heparin-Induced Thrombocytopenia and Heparin-Induced Thrombocytopenia
and Thrombosis
Heparin-induced thrombocytopenia (HIT) is a serious antibody-mediated reaction. HIT occurs in patients treated with heparin and is due to the development of antibodies to a platelet Factor 4-heparin complex that induce in vivo platelet aggregation. HIT may progress to the development of venous and arterial thromboses, a condition referred to as heparin-induced thrombocytopenia with thrombosis (HITT). Thrombotic events may also be the initial presentation for HITT. These serious thromboembolic events include deep vein thrombosis, pulmonary embolism, cerebral vein thrombosis, limb ischemia, stroke, myocardial infarction, mesenteric thrombosis, renal arterial thrombosis, skin necrosis, gangrene of the extremities that may lead to amputation, and possibly death. If the platelet count falls below 100,000/mm3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant.
HIT or HITT can occur up to several weeks after the discontinuation of heparin therapy. Patients presenting with thrombocytopenia or thrombosis after discontinuation of heparin sodium should be evaluated for HIT or HITT.
5.4 Risk of Serious Adverse Reactions in Infants Due to Benzyl Alcohol
Preservative
Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and infants treated with benzyl alcohol-preserved drugs, including heparin sodium multiple-dose vials. The “gasping syndrome” is characterized by central nervous system depression, metabolic acidosis, and gasping respirations.
When prescribing heparin sodium multiple-dose vials in infants consider the combined daily metabolic load of benzyl alcohol from all sources including heparin sodium multiple-dose vials (contains 10.42 mg of benzyl alcohol per mL) and other drugs containing benzyl alcohol. The minimum amount of benzyl alcohol at which toxicity may occur is not known [see Use in Specific Populations (8.4)].
5.5 Thrombocytopenia
Thrombocytopenia in patients receiving heparin has been reported at frequencies up to 30%. It can occur 2 to 20 days (average 5 to 9) following the onset of heparin therapy. Obtain platelet counts before and periodically during heparin therapy. Monitor thrombocytopenia of any degree closely. If the count falls below 100,000/mm3 or if recurrent thrombosis develops, promptly discontinue heparin, evaluate for HIT and HITT, and, if necessary, administer an alternative anticoagulant [see Warnings and Precautions (5.3)].
5.6 Coagulation Testing and Monitoring
When using a full dose heparin regimen, adjust the heparin dose based on frequent blood coagulation tests. If the coagulation test is unduly prolonged or if hemorrhage occurs, discontinue heparin promptly [see Overdosage (10)]. Periodic platelet counts and hematocrits are recommended during the entire course of heparin therapy, regardless of the route of administration [see Dosage and Administration (2.2)].
5.7 Heparin Resistance
Resistance to heparin is frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer, in postsurgical patients, and patients with antithrombin III deficiency. Close monitoring of coagulation tests is recommended in these cases. Adjustment of heparin doses based on anti-Factor Xa levels may be warranted.
5.8 Hypersensitivity
Patients with documented hypersensitivity to heparin should be given the drug only in clearly life-threatening situations.
Because heparin sodium is derived from animal tissue, it should be used with caution in patients with a history of allergy.
DRUG INTERACTIONS SECTION
Highlight: Drugs that interfere with platelet aggregation: May induce bleeding (7.2)
7 DRUG INTERACTIONS
7.1 Oral Anticoagulants
Heparin sodium may prolong the one-stage prothrombin time. Therefore, when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hours after the last intravenous dose or 24 hours after the last subcutaneous dose should elapse before blood is drawn, if a valid prothrombin time is to be obtained.
7.2 Platelet Inhibitors
Drugs such as NSAIDS (including salicylic acid, ibuprofen, indomethacin, and celecoxib), dextran, phenylbutazone, thienopyridines, dipyridamole, hydroxychloroquine, glycoprotein IIb/IIIa antagonists (including abciximab, eptifibatide, and tirofiban), and others that interfere with platelet- aggregation reactions (the main hemostatic defense of heparinized patients) may induce bleeding and should be used with caution in patients receiving heparin sodium. To reduce the risk of bleeding, a reduction in the dose of antiplatelet agent or heparin is recommended.
7.3 Other Interactions
Digitalis, tetracyclines, nicotine or antihistamines may partially counteract the anticoagulant action of heparin sodium. Intravenous nitroglycerin administered to heparinized patients may result in a decrease of the partial thromboplastin time with subsequent rebound effect upon discontinuation of nitroglycerin. Careful monitoring of partial thromboplastin time and adjustment of heparin dosage are recommended during coadministration of heparin and intravenous nitroglycerin.
Antithrombin III (human) – The anticoagulant effect of heparin is enhanced by concurrent treatment with antithrombin III (human) in patients with hereditary antithrombin III deficiency. To reduce the risk of bleeding, a reduced dosage of heparin is recommended during treatment with antithrombin III (human).
USE IN SPECIFIC POPULATIONS SECTION
Highlight: * Pregnancy: Preservative-free formulation recommended. Limited human data in pregnant women. (8.1)
- Lactation: Advise females not to breastfeed. (8.2)
- Pediatric Use: Use preservative-free formulation in neonates and infants. (8.4)
- Geriatric Use: A higher incidence of bleeding reported in patients, particularly women, over 60 years of age. (8.5)
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on heparin sodium use in pregnant women to inform a drug-associated risk of major birth defects and miscarriage. In published reports, heparin exposure during pregnancy did not show evidence of an increased risk of adverse maternal or fetal outcomes in humans. No teratogenicity, but early embryo-fetal death was observed in animal reproduction studies with administration of heparin sodium to pregnant rats and rabbits during organogenesis at doses approximately 10 times the maximum recommended human dose (MRHD) of 45,000 units/ day [see Data]. Consider the benefits and risks of heparin sodium for the mother and possible risks to the fetus when prescribing heparin sodium to a pregnant woman.
If available, preservative-free heparin sodium is recommended when heparin therapy is needed during pregnancy. There are no known adverse outcomes associated with fetal exposure to the preservative benzyl alcohol through maternal drug administration; however, the preservative benzyl alcohol can cause serious adverse events and death when administered intravenously to neonates and infants [see Warnings and Precautions (5.4)].
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
The maternal and fetal outcomes associated with uses of heparin via various dosing methods and administration routes during pregnancy have been investigated in numerous studies. These studies generally reported normal deliveries with no maternal or fetal bleeding and no other complications.
Animal Data
In a published study conducted in rats and rabbits, pregnant animals received heparin intravenously during organogenesis at a dose of 10,000 units/kg/day, approximately 10 times the maximum human daily dose based on body weight. The number of early resorptions increased in both species. There was no evidence of teratogenic effects.
8.2 Lactation
Risk Summary
If available, preservative-free heparin sodium is recommended when heparin therapy is needed during lactation. Benzyl alcohol present in maternal serum is likely to cross into human milk and may be orally absorbed by a nursing infant. There is no information regarding the presence of heparin sodium in human milk, the effects on the breastfed infant, or the effects on milk production. Due to its large molecular weight, heparin is not likely to be excreted in human milk, and any heparin in milk would not be orally absorbed by a nursing infant. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for heparin sodium and any potential adverse effects on the breastfed infant from heparin sodium or from the underlying maternal condition [see Use in Specific Populations (8.4)].
8.4 Pediatric Use
There are no adequate and well controlled studies on heparin use in pediatric patients. Pediatric dosing recommendations are based on clinical experience [see Dosage and Administration (2.4)].
Carefully examine all heparin sodium vials to confirm choice of the correct strength prior to administration of the drug. Pediatric patients, including neonates, have died as a result of medication errors in which heparin sodium vials have been confused with “catheter lock flush” vials [see Warnings and Precautions (5.1)].
Benzyl Alcohol Toxicity
Use preservative-free heparin sodium in neonates and infants.
Serious adverse reactions including fatal reactions and the “gasping syndrome” occurred in premature neonates and infants in the neonatal intensive care unit who received drugs containing benzyl alcohol as a preservative. In these cases, benzyl alcohol dosages of 99 to 234 mg/kg/day produced high levels of benzyl alcohol and its metabolites in the blood and urine (blood levels of benzyl alcohol were 0.61 to 1.378 mmol/L). Additional adverse reactions included gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Preterm, low- birth weight infants may be more likely to develop these reactions because they may be less able to metabolize benzyl alcohol.
8.5 Geriatric Use
There are limited adequate and well-controlled studies in patients 65 years and older, however, a higher incidence of bleeding has been reported in patients, particularly women, over 60 years of age [see Warnings and Precautions (5.2)]. Patients over 60 years of age may require lower doses of heparin.
Lower doses of heparin may be indicated in these patients [see Clinical Pharmacology (12.3)].
ADVERSE REACTIONS SECTION
Highlight: Most common adverse reactions are hemorrhage, thrombocytopenia, HIT and HITTS, injection site irritation, general hypersensitivity reactions, and elevations of aminotransferase levels. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sagent Pharmaceuticals, Inc. at 1-866-625-1618 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch.
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hemorrhage [see Warnings and Precautions (5.2)]
- Heparin-Induced Thrombocytopenia and Heparin-Induced Thrombocytopenia and Thrombosis [see Warnings and Precautions (5.3)]
- Risk of Serious Adverse Reactions in Infants Due to Benzyl Alcohol Preservative [see Warnings and Precautions (5.4)]
- Thrombocytopenia [see Warnings and Precautions (5.5)]
- Heparin Resistance [see Warnings and Precautions (5.7)]
- Hypersensitivity [see Warnings and Precautions (5.8)]
6.1 Postmarketing Experience
The following adverse reactions have been identified during post approval use of heparin sodium. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Hemorrhage is the chief complication that may result from heparin therapy [see Warnings and Precautions (5.2)]. Gastrointestinal or urinary tract bleeding during anticoagulant therapy may indicate the presence of an underlying occult lesion. Bleeding can occur at any site but certain specific hemorrhagic complications may be difficult to detect:
- Adrenal hemorrhage, with resultant acute adrenal insufficiency, has occurred with heparin therapy, including fatal cases.
- Ovarian (corpus luteum) hemorrhage developed in a number of women of reproductive age receiving short- or long-term heparin therapy.
- Retroperitoneal hemorrhage.
- HIT and HITT, including delayed onset cases [see Warnings and Precautions (5.3)].
- Local Irritation**–** Local irritation, erythema, mild pain, hematoma or ulceration may follow deep subcutaneous (intrafat) injection of heparin sodium. Because these complications are much more common after intramuscular use, the intramuscular route is not recommended.
- Histamine-like reactions – Such reactions have been observed at the site of injections. Necrosis of the skin has been reported at the site of subcutaneous injection of heparin, occasionally requiring skin grafting [see Warnings and Precautions (5.3)].
- Hypersensitivity**–** Generalized hypersensitivity reactions have been reported, with chills, fever and urticaria as the most usual manifestations, and asthma, rhinitis, lacrimation, headache, nausea and vomiting, and anaphylactoid reactions, including shock, occurring less frequently. Itching and burning, especially on the plantar side of the feet, may occur. [see Warnings and Precautions (5.8)].
- Elevations of aminotransferases**–** Significant elevations of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels have occurred in patients who have received heparin [see Drug Interactions (7.4)].
- Miscellaneous**–** Osteoporosis following long-term administration of high doses of heparin, cutaneous necrosis after systemic administration, suppression of aldosterone synthesis, delayed transient alopecia, priapism, and rebound hyperlipemia on discontinuation of heparin sodium have also been reported.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate carcinogenic potential of heparin. Also, no reproduction studies in animals have been performed concerning mutagenesis or impairment of fertility.
HOW SUPPLIED SECTION
16 HOW SUPPLIED/STORAGE AND HANDLING
Heparin Sodium Injection, USP preserved with benzyl alcohol is available as follows:
|
NDC |
Strength |
Vial Fill Volume |
Vial Type |
Package Factor |
|
25021-400-01 |
1,000 USP units per mL |
1 mL |
1 mL Vial |
25 vials per carton |
|
25021-400-10 |
10,000 USP units per 10 mL |
10 mL |
Multi-Dose Vial |
25 vials per carton |
|
25021-400-30 |
30,000 USP units per 30 mL |
30 mL |
Multi-Dose Vial |
25 vials per carton |
|
25021-402-01 |
5,000 USP units per mL |
1 mL |
1 mL Vial |
25 vials per carton |
|
25021-402-10 |
50,000 USP units per 10 mL |
10 mL |
Multi-Dose Vial |
25 vials per carton |
|
25021-403-01 |
10,000 USP units per mL |
1 mL |
1 mL Vial |
25 vials per carton |
|
25021-403-04 |
40,000 USP units per 4 mL |
4 mL |
Multi-Dose Vial |
25 vials per carton |
Sterile, Nonpyrogenic.
The container closure is not made with natural rubber latex.
Storage Conditions
****Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
