Tafinlar
These highlights do not include all the information needed to use TAFINLAR safely and effectively. See full prescribing information for TAFINLAR. TAFINLAR (dabrafenib) capsules, for oral useTAFINLAR (dabrafenib) tablets for oral suspensionInitial U.S. Approval: 2013
fee1e6b1-e1a5-4254-9f2e-a70e0f8dbdea
HUMAN PRESCRIPTION DRUG LABEL
Mar 29, 2024
Novartis Pharmaceuticals Corporation
DUNS: 002147023
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
dabrafenib
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
dabrafenib
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (7)
dabrafenib
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (7)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC 0078-1154-21
Rx only
Tafinlar®
(dabrafenib)
Tablets for Oral Suspension*
10 mg per tablet
*DISPERSE TABLETS IN WATER PRIOR TO INGESTION.
DO NOT SWALLOW WHOLE, CHEW OR CRUSH.
Dispense and store in original container with the desiccant**.
Dispense with Medication Guide.
210 Tablets
NOVARTIS
CONTRAINDICATIONS SECTION
4** CONTRAINDICATIONS**
None.
None. (4)
DRUG INTERACTIONS SECTION
7** DRUG INTERACTIONS**
7.1 Effects of Other Drugs on TAFINLAR
Strong inhibitors of CYP3A4 or CYP2C8 may increase the concentration of dabrafenib [see Clinical Pharmacology (12.3)]. Substitution of strong inhibitors of CYP3A4 or CYP2C8 is recommended during treatment with TAFINLAR. If concomitant use of strong inhibitors of CYP3A4 or CYP2C8 is unavoidable, monitor patients closely for adverse reactions when taking strong inhibitors.
7.2 Effects of TAFINLAR on Other Drugs
Dabrafenib decreased the systemic exposures of midazolam (a CYP3A4 substrate), S-warfarin (a CYP2C9 substrate), and R-warfarin (a CYP3A4/CYP1A2 substrate) [see Clinical Pharmacology (12.3)]. Monitor international normalized ratio (INR) levels more frequently in patients receiving warfarin during initiation or discontinuation of dabrafenib. Coadministration of TAFINLAR with other substrates of these enzymes, including dexamethasone or hormonal contraceptives, can result in decreased concentrations and loss of efficacy [see Use in Specific Populations (8.1, 8.3)]. Substitute for these medications or monitor patients for loss of efficacy if use of these medications is unavoidable.
-
Avoid concurrent administration of strong inhibitors of CYP3A4 or CYP2C8. (7.1)
-
Concomitant use with agents that are sensitive substrates of CYP3A4, CYP2C8, CYP2C9, CYP2C19, or CYP2B6 may result in loss of efficacy of these agents. (7.2)
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Indications and Usage, BRAF V600E Mutation-Positive Unresectable or Metastatic Solid Tumors (1.6) |
8/2023 |
|
Warnings and Precautions, Hemophagocytic Lymphohistiocytosis (5.11) |
5/2023 |
DOSAGE FORMS & STRENGTHS SECTION
3** DOSAGE FORMS AND STRENGTHS**
TAFINLAR Capsules:
- 50 mg: Dark red capsule imprinted with ‘GS TEW’ and ‘50 mg’.
- 75 mg: Dark pink capsule imprinted with ‘GS LHF’ and ‘75 mg’.
TAFINLAR Tablets for Oral Suspension:
- 10 mg: White to slightly yellow, round, biconvex 6 mm tablet debossed with “D” on one side and “NVR” on the other, contains berry flavor.
TAFINLAR Capsules: 50 mg, 75 mg (3)
TAFINLAR Tablets for Oral Suspension: 10 mg (3)
OVERDOSAGE SECTION
10** OVERDOSAGE**
There is no information on overdosage of TAFINLAR. Since dabrafenib is highly bound to plasma proteins, hemodialysis is likely to be ineffective in the treatment of overdose with TAFINLAR.
CLINICAL PHARMACOLOGY SECTION
12** CLINICAL PHARMACOLOGY**
12.1 Mechanism of Action
Dabrafenib is an inhibitor of some mutated forms of BRAF kinases with in vitro IC50 values of 0.65, 0.5, and 1.84 nM for BRAF V600E, BRAF V600K, and BRAF V600D enzymes, respectively. Dabrafenib also inhibits wild-type BRAF and CRAF kinases with IC50 values of 3.2 and 5.0 nM, respectively, and other kinases, such as SIK1, NEK11, and LIMK1 at higher concentrations. Some mutations in the BRAF gene, including those that result in BRAF V600E, can result in constitutively activated BRAF kinases that may stimulate tumor cell growth [see Indications and Usage (1)]. Dabrafenib inhibits cell growth of various BRAF V600 mutation-positive tumors in vitro and in vivo.
Dabrafenib and trametinib target two different kinases in the RAS/RAF/MEK/ERK pathway. Use of dabrafenib and trametinib in combination resulted in greater growth inhibition of BRAF V600 mutation-positive tumor cell lines in vitro and prolonged inhibition of tumor growth in BRAF V600 mutation-positive tumor xenografts compared with either drug alone.
In the setting of BRAF-mutant colorectal cancer, induction of EGFR-mediated MAPK pathway re-activation has been identified as a mechanism of intrinsic resistance to BRAF inhibitors [see Indications and Usage (1.8)].
12.2 Pharmacodynamics
Cardiac Electrophysiology
The potential effect of TAFINLAR on QT interval was assessed in a dedicated multiple-dose study in 32 patients with BRAF V600 mutation-positive tumors. No large changes in the mean QT interval (i.e., > 20 ms) were detected with dabrafenib 300 mg administered twice daily (two times the recommended dosage).
In clinical trials, QTc (heart rate-corrected QT) prolongation to ≥ 500 ms occurred in 0.8% of 264 patients who received TAFINLAR with trametinib and in 1.5% of patients who received TAFINLAR as a single agent. The QTc was increased > 60 ms from baseline in 3.8% of patients who received TAFINLAR with trametinib and 3% of patients treated with TAFINLAR as a single agent.
12.3 Pharmacokinetics
Following administration of TAFINLAR capsules, dabrafenib Cmax and AUC increased in a dose-proportional manner across the dose range of 12 mg (0.08 times the approved recommended adult dose) to 300 mg (2 times the approved recommended adult dose), but the increase was less than dose-proportional after steady state twice-daily dosing. After twice-daily dosing, the mean accumulation ratio was 0.7, and the inter-subject variability (CV%) of AUC at steady-state was 38%.
Absorption
The median time to achieve peak plasma concentration (Tmax) is 2 hours. Mean absolute bioavailability of TAFINLAR capsules is 95% and TAFINLAR tablets for oral suspension is 76%.
Effect of Food
Following administration of TAFINLAR capsules, a high-fat meal (approximately 1000 calories, 58-75 grams fat, 58 grams carbohydrates, and 33 grams protein) decreased Cmax by 51%, decreased AUC by 31%, and delayed median Tmax by 3.6 hours as compared with the fasted state.
Distribution
Dabrafenib is 99.7% bound to human plasma proteins. The apparent volume of distribution (Vc/F) is 70.3 L.
Elimination
The mean terminal half-life is 8 hours. Hydroxy-dabrafenib terminal half-life (10 hours) parallels that of dabrafenib while the carboxy- and desmethyl- dabrafenib metabolites exhibit longer half-lives (21 to 22 hours). The apparent clearance of dabrafenib is 17 L/h after a single dose and 34 L/h after twice-daily dosing for 2 weeks.
Metabolism
The metabolism of dabrafenib is primarily mediated by CYP2C8 and CYP3A4 to form hydroxy-dabrafenib. Hydroxy-dabrafenib is further oxidized via CYP3A4 to form carboxy-dabrafenib and subsequently excreted in bile and urine. Carboxy- dabrafenib is decarboxylated to form desmethyl-dabrafenib; desmethyl- dabrafenib may be reabsorbed from the gut. Desmethyl-dabrafenib is further metabolized by CYP3A4 to oxidative metabolites. Mean metabolite-to-parent AUC ratios following repeat-dose administration are 0.9, 11, and 0.7 for hydroxy-, carboxy-, and desmethyl-dabrafenib, respectively. Based on systemic exposure, relative potency, and pharmacokinetic properties, both hydroxy- and desmethyl- dabrafenib are likely to contribute to the clinical activity of dabrafenib.
Excretion
Fecal excretion is the major route of elimination accounting for 71% of radioactive dose while urinary excretion accounted for 23% of total radioactivity as metabolites only.
Specific Populations
Age (18 to 93 years), sex, weight (36 to 170 kg), and renal impairment (eGFR 15 to 89 mL/min/1.73 m2) have no clinically relevant effect on the pharmacokinetics of dabrafenib.
Pediatric Patients
The pharmacokinetics of dabrafenib in glioma and other solid tumors were evaluated in 243 patients aged 1 to < 18 years following a single dose or multiple doses. Pharmacokinetic parameters in patients aged 1 to < 18 years are within range of values previously observed in adults given the same dose based on weight. Weight (6 to 156 kg) had a statistically significant effect on dabrafenib oral clearance in this population.
Patients with Hepatic Impairment
Mild hepatic impairment (bilirubin ≤ ULN and AST > ULN or bilirubin > 1x to 1.5x ULN and any AST) has no effect on systemic exposure to dabrafenib and its metabolites. No data are available in patients with moderate (bilirubin > 1.5x to 3x ULN and any AST) or severe (bilirubin > 3x to 10x ULN and any AST) hepatic impairment.
Drug Interaction Studies
Effect of Trametinib on Dabrafenib: Coadministration of TAFINLAR 75 mg twice daily with trametinib 2 mg daily resulted in a 23% increase in AUC of dabrafenib, a 33% increase in AUC of desmethyl-dabrafenib, and no change in AUC of hydroxy-dabrafenib as compared with administration of dabrafenib.
Effect of Strong Inhibitors of CYP3A4 or CYP2C8 on Dabrafenib: Coadministration of TAFINLAR 75 mg twice daily and ketoconazole (a strong CYP3A4 inhibitor) for 4 days increased dabrafenib AUC by 71%, hydroxy- dabrafenib AUC by 82%, and desmethyl-dabrafenib AUC by 68%.
Coadministration of TAFINLAR 75 mg twice daily and gemfibrozil (a strong CYP2C8 inhibitor) for 4 days increased dabrafenib AUC by 47%, with no change in the AUC of dabrafenib metabolites.
Effect of Strong Inducers of CYP3A4 or Moderate Inducers of CYP2C8 on Dabrafenib: Coadministration of TAFINLAR 150 mg twice daily and rifampin (a strong CYP3A4 and moderate CYP2C8 inducer) for 10 days decreased dabrafenib AUC by 34% and desmethyl-dabrafenib AUC by 30%, and had no effect on hydroxy- dabrafenib AUC.
Effect of Acid Reducing Agents on Dabrafenib: Coadministration of TAFINLAR 150 mg twice daily and rabeprazole for 4 days did not result in clinically relevant changes in exposures to dabrafenib and its metabolites.
Effect of Dabrafenib on CYP Substrates: Coadministration of TAFINLAR 150 mg twice daily for 15 days and a single dose of midazolam (a CYP3A4 substrate) decreased midazolam AUC by 65%. Coadministration of TAFINLAR 150 mg twice daily for 15 days and a single dose of warfarin decreased the AUC of S-warfarin (a CYP2C9 substrate) by 37% and the AUC of R-warfarin (CYP3A4/CYP1A2 substrate) by 33%.
In vitro data demonstrate that dabrafenib is an inducer of CYP3A4 and CYP2B6 via activation of the pregnane X receptor (PXR) and constitutive androstane receptor (CAR) nuclear receptors. Dabrafenib may also induce CYP2C enzymes via the same mechanism.
Effect of Transporters on Dabrafenib: Dabrafenib and its metabolites, hydroxyl-dabrafenib and desmethyl-dabrafenib, are substrates of human P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) but are not substrates of organic cation transporter (OCT1) or organic anion transporting polypeptide (OATP1A2, OATP1B1, OATP1B3, OATP2B1) in vitro.
Effect of Dabrafenib on Transporters: Coadministration of TAFINLAR 150 mg twice daily with a single dose of rosuvastatin (a sensitive OATP1B1 and OATP1B3 substrate) increased rosuvastatin Cmax by 2.6-fold but did not change its AUC.
Dabrafenib and its metabolites, hydroxy-dabrafenib, carboxy-dabrafenib, and desmethyl-dabrafenib, are inhibitors of organic anion transporter (OAT1 and OAT3) in vitro. Dabrafenib and desmethyl-dabrafenib are inhibitors of OCT2 and BCRP in vitro.
CLINICAL STUDIES SECTION
14** CLINICAL STUDIES**
14.1 BRAF V600E Mutation-Positive Unresectable or Metastatic Melanoma –
TAFINLAR As a Single Agent
BREAK-3 Study
The safety and efficacy of TAFINLAR as a single agent were evaluated in an international, multi-center, randomized (3:1), open-label, active-controlled trial (the BREAK-3 study; NCT01227889) conducted in 250 patients with previously untreated BRAF V600E mutation-positive, unresectable or metastatic melanoma. Patients with any prior use of BRAF inhibitors or MEK inhibitors were excluded. Patients were randomized to receive TAFINLAR 150 mg orally twice daily (n = 187) or dacarbazine 1000 mg/m2 intravenously every 3 weeks (n = 63). Randomization was stratified by disease stage at baseline [unresectable Stage III (regional nodal or in-transit metastases), M1a (distant skin, subcutaneous, or nodal metastases), or M1b (lung metastases) versus M1c melanoma (all other visceral metastases or elevated serum LDH)]. The main efficacy outcome measure was progression-free survival (PFS) as assessed by the investigator. In addition, an independent radiology review committee (IRRC) assessed the following efficacy outcome measures in pre-specified supportive analyses: PFS, confirmed overall response rate (ORR), and duration of response (DoR).
The median age of patients in the BREAK-3 study was 52 years. The majority of the trial population was male (60%), White (99%), had an ECOG performance status of 0 (67%), had M1c disease (66%), and had normal LDH (62%). All patients had tumor tissue with mutations in BRAF V600E as determined by a clinical trial assay at a centralized testing site. Tumor samples from 243 patients (97%) were tested retrospectively using an FDA-approved companion diagnostic test, tHxID™-BRAF assay.
The median durations of follow-up prior to initiation of alternative treatment in patients randomized to receive TAFINLAR was 5.1 months and in the dacarbazine arm was 3.5 months. Twenty-eight (44%) patients crossed over from the dacarbazine arm at the time of disease progression to receive TAFINLAR.
The BREAK-3 study demonstrated a statistically significant increase in progression-free survival in the patients treated with TAFINLAR. Table 20 and Figure 1 summarize the PFS results.
Table 20. Investigator-Assessed Progression-Free Survival and Confirmed Overall Response Results in the BREAK-3 Study|
Abbreviations: CI, confidence interval; DoR, duration of response; HR, hazard
ratio; NR, not reached. | ||
|
Investigator-Assessed Endpoints |
TAFINLAR |
Dacarbazine |
|
Progression-Free Survival | ||
|
Number of events (%) |
78 (42%) |
41 (65%) |
|
Progressive disease |
76 |
41 |
|
Death |
2 |
0 |
|
Median, months (95% CI) |
5.1 (4.9, 6.9) |
2.7 (1.5, 3.2) |
|
HRa (95% CI) |
0.33 (0.20, 0.54) | |
|
P valueb |
< 0.0001 | |
|
Confirmed Tumor Responses | ||
|
Overall response rate (95% CI) |
52% (44%, 59%) |
17% (9%, 29%) |
|
Complete response, n (%) |
6 (3%) |
0 |
|
Partial response, n (%) |
91 (48%) |
11 (17%) |
|
Duration of response | ||
|
Median DoR, months (95% CI) |
5.6 (5.4, NR) |
NR (5.0, NR) |

Figure 1. Kaplan-Meier Curves of Investigator-Assessed Progression-Free Survival in the BREAK-3 Study
In supportive analyses based on IRRC assessment and in an exploratory subgroup analysis of patients with retrospectively confirmed V600E mutation-positive melanoma with the tHxID™-BRAF assay, the PFS results were consistent with those of the primary efficacy analysis.
BREAK-MB Study
The activity of TAFINLAR for the treatment of BRAF V600E mutation-positive melanoma, metastatic to the brain was evaluated in a single-arm, open-label, two-cohort multi-center trial (the BREAK-MB study; NCT01266967). All patients received TAFINLAR 150 mg twice daily. Patients in Cohort A (n = 74) had received no prior local therapy for brain metastases, while patients in Cohort B (n = 65) had received at least one local therapy for brain metastases, including, but not limited to, surgical resection, whole brain radiotherapy, or stereotactic radiosurgery, such as gamma knife, linear-accelerated-based radiosurgery, or charged particles. In addition, patients in Cohort B were required to have evidence of disease progression in a previously treated lesion or an untreated lesion. Additional eligibility criteria were at least one measurable lesion of 0.5 cm or greater in largest diameter on contrast- enhanced MRI, stable or decreasing corticosteroid dose, and no more than two prior systemic regimens for treatment of metastatic disease. The major efficacy outcome measure was estimation of the overall intracranial response rate (OIRR) in each cohort.
The median age of patients in Cohort A was 50 years, 72% were male, 100% were White, 59% had a pre-treatment ECOG performance status of 0, and 57% had elevated LDH at baseline. The median age of patients in Cohort B was 51 years, 63% were male, 98% were White, 66% had a pre-treatment ECOG performance status of 0, and 54% had elevated LDH at baseline. The intracranial response rate as determined by an independent radiology review committee, masked to investigator response assessments, was 18% (95% CI: 10%, 28%) in Cohort A and 18% (95% CI: 10%, 30%) in Cohort B. The median duration of intracranial response was 4.6 months in both cohorts.
14.2 BRAF V600E or V600K Unresectable or Metastatic Melanoma – TAFINLAR
With Trametinib
COMBI-d Study and COMBI-v Study
The safety and efficacy of TAFINLAR administered with trametinib were evaluated in two international, randomized, active-controlled trials: one double-blind trial (the COMBI-d study; NCT01584648) and one open-label trial (the COMBI-v study; NCT01597908).
The COMBI-d study compared TAFINLAR and trametinib to TAFINLAR and placebo as first-line therapy for patients with unresectable (Stage IIIC) or metastatic (Stage IV) BRAF V600E or V600K mutation-positive cutaneous melanoma. Patients were randomized (1:1) to receive TAFINLAR 150 mg twice daily and trametinib 2 mg once daily or TAFINLAR 150 mg twice daily plus matching placebo. Randomization was stratified by LDH level (> ULN vs. ≤ ULN) and BRAF mutation subtype (V600E vs. V600K). The major efficacy outcome was investigator- assessed progression-free survival (PFS) per RECIST v1.1 with additional efficacy outcome measures of overall survival (OS) and confirmed overall response rate (ORR).
The COMBI-v study compared TAFINLAR and trametinib to vemurafenib as first- line treatment therapy for patients with unresectable (Stage IIIC) or metastatic (Stage IV) BRAF V600E or V600K mutation-positive cutaneous melanoma. Patients were randomized (1:1) to receive TAFINLAR 150 mg twice daily and trametinib 2 mg once daily or vemurafenib 960 mg twice daily. Randomization was stratified by lactate dehydrogenase (LDH) level (> ULN vs. ≤ ULN) and BRAF mutation subtype (V600E vs. V600K). The major efficacy outcome measure was overall survival. Additional efficacy outcome measures were PFS and ORR as assessed by investigator per RECIST v1.1.
In the COMBI-d study, 423 patients were randomized to TAFINLAR plus trametinib (n = 211) or TAFINLAR plus placebo (n = 212). The median age was 56 years (range: 22 to 89), 53% were male, > 99% were White, 72% had ECOG performance status of 0, 4% had Stage IIIC, 66% had M1c disease, 65% had normal LDH, and 2 patients had a history of brain metastases. All patients had tumor containing BRAF V600E or V600K mutations as determined by centralized testing with the FDA-approved companion diagnostic test; 85% with BRAF V600E mutations and 15% with BRAF V600K mutations.
In the COMBI-v study, 704 patients were randomized to TAFINLAR plus trametinib (n = 352) or single-agent vemurafenib (n = 352). The median age was 55 years (range: 18 to 91), 96% were White, 55% were male, 6% had Stage IIIC, 61% had M1c disease, 67% had normal LDH, 70% had ECOG performance status of 0, 89% had BRAF V600E mutation-positive melanoma, and one patient had a history of brain metastases.
The COMBI-d and COMBI-v studies demonstrated statistically significant improvements in OS and PFS. Table 21 and Figures 2 and 3 summarize the efficacy results.
Table 21. Efficacy Results in Patients with BRAF V600E or V600K Mutation-Positive Unresectable or Metastatic Melanomaa|
Abbreviations: DoR, duration of response; ORR, overall response rate; CI,
confidence interval; HR, hazard ratio; NR, not reached. | ||||
|
Endpoint |
COMBI-d Study |
COMBI-v Study | ||
|
TAFINLAR plus Trametinib |
TAFINLAR |
TAFINLAR plus Trametinib |
Vemurafenib | |
|
Overall Survival | ||||
|
Number of deaths (%) |
99 (47%) |
123 (58%) |
100 (28%) |
122 (35%) |
|
Median, months (95% CI) |
25.1 (19.2, NR) |
18.7 (15.2, 23.1) |
NR (18.3, NR) |
17.2 (16.4, NR) |
|
HR (95% CI) |
0.71 (0.55, 0.92) |
0.69 (0.53, 0.89) | ||
|
P value (log-rank test) |
0.01 |
0.005a | ||
|
Progression-Free Survival****b | ||||
|
Number of events (%) |
102 (48%) |
109 (51%) |
166 (47%) |
217 (62%) |
|
Median, months (95% CI) |
9.3 (7.7, 11.1) |
8.8 (5.9, 10.9) |
11.4 (9.9, 14.9) |
7.3 (5.8, 7.8) |
|
HR (95% CI) |
0.75 (0.57, 0.99) |
0.56 (0.46, 0.69) | ||
|
P value (log-rank test) |
0.035 |
< 0.001 | ||
|
Overall Response Rate****b | ||||
|
ORR (95% CI) |
66% (60%, 73%) |
51% (44%, 58%) |
64% (59%, 69%) |
51% (46%, 56%) |
|
P value |
< 0.001 |
< 0.001 | ||
|
Complete response |
10% |
8% |
13% |
8% |
|
Partial response |
56% |
42% |
51% |
43% |
|
Median DoR, months |
9.2 |
10.2 |
13.8 |
7.5 |
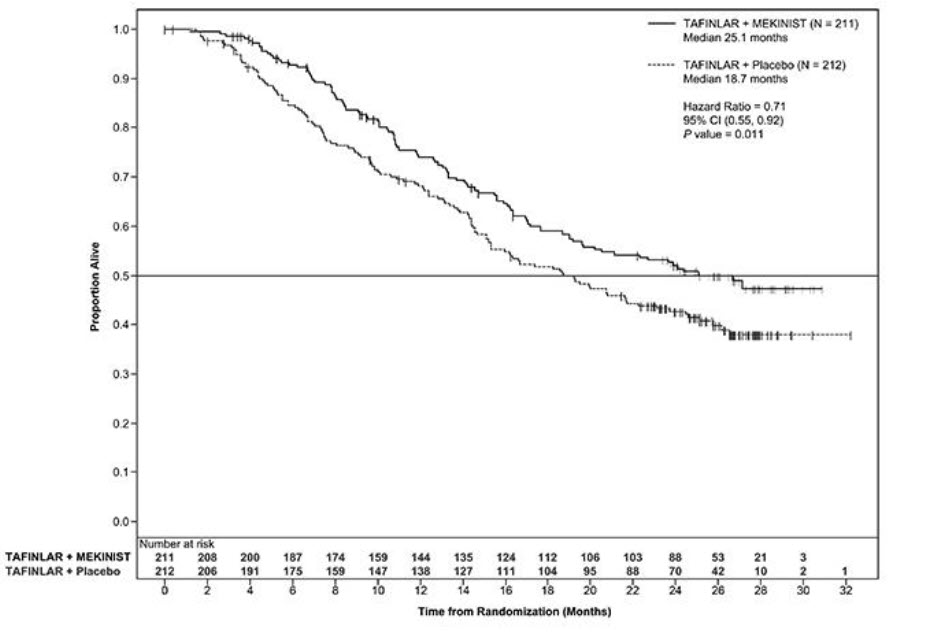
Figure 2. Kaplan-Meier Curves for Overall Survival in the COMBI-d Study
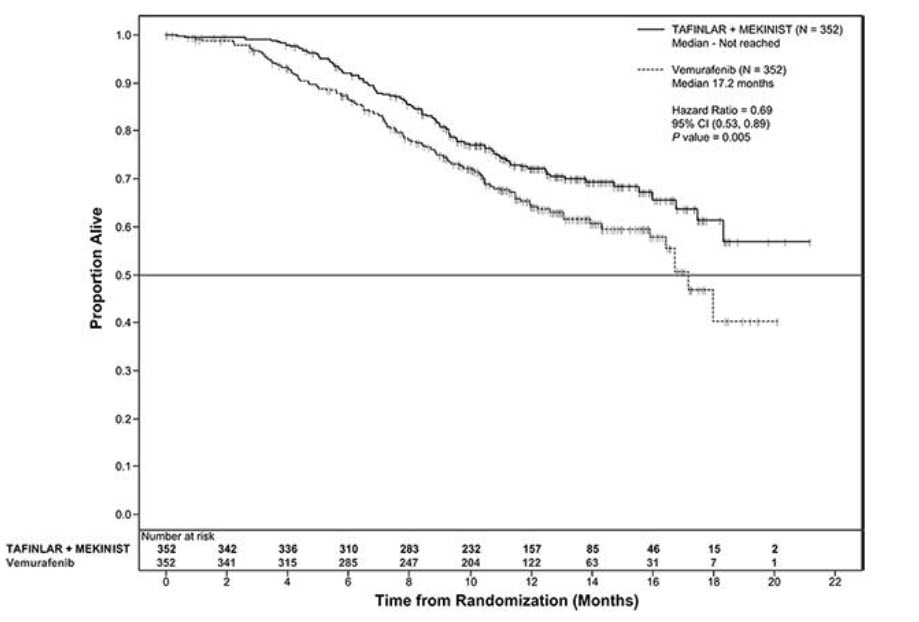
Figure 3. Kaplan-Meier Curves for Overall Survival in the COMBI-v Study
COMBI-MB Study
The activity of TAFINLAR with trametinib for the treatment of BRAF V600E or V600K mutation-positive melanoma, metastatic to the brain, was evaluated in a non-randomized, open-label, multi-center, multi-cohort trial (the COMBI-MB study; NCT02039947). Eligible patients were required to have at least one measurable intracranial lesion and to have no leptomeningeal disease, parenchymal brain metastasis greater than 4 cm in diameter, ocular melanoma, or primary mucosal melanoma. Patients received TAFINLAR 150 mg orally twice daily and trametinib 2 mg orally once daily until disease progression or unacceptable toxicity. The major efficacy outcome measure was intracranial response rate, defined as the percentage of patients with a confirmed intracranial response per RECIST v1.1, modified to allow up to five intracranial target lesions at least 5 mm in diameter, as assessed by independent review.
The COMBI-MB study enrolled 121 patients with a BRAF V600E (85%) or V600K (15%) mutation. The median age was 54 years (range: 23 to 84), 58% were male, 100% were White, 8% were from the United States, 65% had normal LDH at baseline, and 97% had an ECOG performance status of 0 or 1. Intracranial metastases were asymptomatic in 87% and symptomatic in 13% of patients, 22% received prior local therapy for brain metastases, and 87% also had extracranial metastases.
The intracranial response rate was 50% (95% CI: 41, 60), with a complete response rate of 4.1% and a partial response rate of 46%. The median duration of intracranial response was 6.4 months (range: 1 to 31). Of the patients with an intracranial response, 9% had stable or progressive disease as their best overall response.
14.3 Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
COMBI-AD (NCT 01682083) was an international, multi-center, randomized, double-blind, placebo-controlled trial that enrolled patients with Stage III melanoma with BRAF V600E or V600K mutations as detected by the tHxID™-BRAF assay and pathologic involvement of regional lymph node(s). Patients were randomized (1:1) to receive TAFINLAR 150 mg twice daily and trametinib 2 mg once daily or two placebos for up to 1 year. Enrollment required complete resection of melanoma with complete lymphadenectomy within 12 weeks prior to randomization. The trial excluded patients with mucosal or ocular melanoma, unresectable in-transit metastases, distant metastatic disease, or prior systemic anti-cancer treatment, including radiotherapy. Randomization was stratified by BRAF mutation status (V600E or V600K) and American Joint Committee on Cancer (AJCC; 7th Edition) Stage (IIIA, IIIB, or IIIC). The major efficacy outcome measure was relapse-free survival (RFS), defined as the time from randomization to disease recurrence (local, regional, or distant metastasis), new primary melanoma, or death from any cause, whichever occurred first as assessed by the investigator. Patients underwent imaging for tumor recurrence every 3 months for the first two years and every 6 months thereafter.
In COMBI-AD, a total of 870 patients were randomized: 438 to TAFINLAR administered with trametinib and 432 to placebo. Median age was 51 years (range: 18 to 89), 55% were male, 99% were White, and 91% had an ECOG performance status of 0. Disease characteristics were AJCC Stage IIIA (18%), Stage IIIB (41%), Stage IIIC (40%), stage unknown (1%); BRAF V600E mutation (91%), BRAF V600K mutation (9%); macroscopic lymph nodes (65%); and tumor ulceration (41%). The median duration of follow-up (time from randomization to last contact or death) was 2.8 years.
COMBI-AD showed a statistically significant improvement in RFS in patients randomized to TAFINLAR administered with trametinib compared to those randomized to placebo. Efficacy results are presented in Table 22 and Figure 4.
Table 22. Efficacy Results in COMBI-AD in the Adjuvant Treatment of Melanoma|
Abbreviations: HR, hazard ratio; CI, confidence interval; NE, not estimable. | ||
|
Endpoint |
TAFINLAR plus Trametinib |
Placebo |
|
Relapse-Free Survival | ||
|
Number of events (%) |
166 (38) |
248 (57) |
|
Median, months (95% CI) |
NE (44.5, NE) |
16.6 (12.7, 22.1) |
|
HR (95% CI)a |
0.47 (0.39, 0.58) | |
|
P valueb |
< 0.0001 |
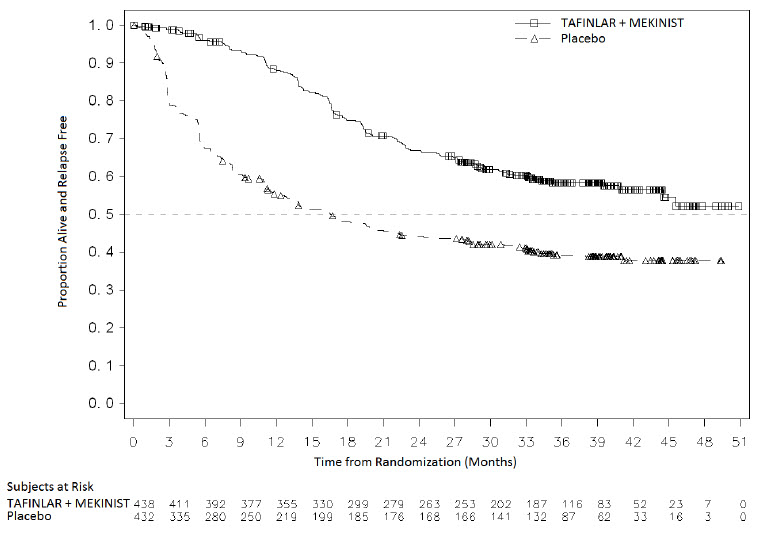
Figure 4. Kaplan-Meier Curves for Relapse-Free Survival in COMBI-AD in the Adjuvant Treatment of Melanoma
14.4 BRAF V600E Mutation-Positive Metastatic Non-Small Cell Lung Cancer
The safety and efficacy of TAFINLAR alone or administered with trametinib were evaluated in a multi-center, three-cohort, non-randomized, activity- estimating, open-label trial (Study BRF113928, NCT01336634). Key eligibility criteria were locally confirmed BRAF V600E mutation-positive metastatic NSCLC, no prior exposure to BRAF or MEK-inhibitor, and absence of EGFR mutation or ALK rearrangement (unless patients had progression on prior tyrosine kinase inhibitor therapy). Patients enrolled in Cohorts A and B were required to have received at least one previous platinum-based chemotherapy regimen for NSCLC with demonstrated disease progression but no more than three prior systemic regimens. Patients enrolled in Cohort C could not have received prior systemic therapy for metastatic NSCLC. Patients in Cohort A received TAFINLAR 150 mg twice daily. Patients in Cohorts B and C received TAFINLAR 150 mg twice daily and trametinib 2 mg once daily. The major efficacy outcome measure was overall response rate (ORR) per RECIST v1.1 as assessed by independent review committee (IRC) and DoR.
There were a total of 171 patients enrolled which included 78 patients enrolled in Cohort A, 57 patients enrolled in Cohort B, and 36 patients enrolled in Cohort C. The characteristics of the study population were: a median age of 66 years, 48% male; 81% White, 14% Asian, 3% Black, and 2% Hispanic; 60% former smokers, 32% never smokers, and 8% current smokers; 27% had ECOG performance status (PS) 0, 63% had ECOG PS 1, and 11% had ECOG PS of 2; 99% had metastatic disease of which 6% had brain metastasis at baseline and 14% had liver metastasis at baseline; 11% had systemic anti-cancer therapy in the adjuvant setting and 58% of the 135 previously treated patients had only one line of prior systemic therapy for metastatic disease; and 98% had non- squamous histology.
Efficacy results are summarized in Table 23.
Table 23. Efficacy Results Based on Independent Review in Study BRF113928|
Abbreviations: CI, confidence interval; DoR, duration of response; ORR,
overall response rate. | |||
|
Treatment |
TAFINLAR |
TAFINLAR + Trametinib | |
|
Population |
Previously Treated |
Previously Treated |
Treatment Naïve |
|
Overall Response Rate****a | |||
|
ORR (95% CI) |
27% (18%, 38%) |
61% (48%, 74%) |
61% (44%, 77%) |
|
Complete response |
1% |
5% |
8% |
|
Partial response |
26% |
56% |
53% |
|
Duration of Response****a |
n = 21 |
n = 35 |
n = 22 |
|
Median DoR, months (95% CI) |
18.0 (4.2, 40.1) |
9.0 (5.8, 26.2) |
15.2 (7.8, 23.5) |
In a subgroup analysis of patients with retrospectively, centrally confirmed BRAF V600E mutation-positive NSCLC with the Oncomine™ Dx Target Test, the ORR results were similar to those presented in Table 22.
14.5 BRAF V600E Mutation-Positive Locally Advanced or Metastatic Anaplastic
Thyroid Cancer
The safety and efficacy of TAFINLAR administered with trametinib was evaluated in an activity estimating, nine-cohort, multi-center, non-randomized, open- label trial (Study BRF117019; NCT02034110) in patients with rare cancers with the BRAF V600E mutation, including locally advanced, unresectable, or metastatic ATC with no standard locoregional treatment options. Trial BRF117019 excluded patients who could not swallow or retain the medication; who received prior treatment with BRAF or MEK inhibitors; with symptomatic or untreated CNS metastases; or who had airway obstruction. Patients received TAFINLAR 150 mg twice daily and trametinib 2 mg once daily. The major efficacy outcome measure was overall response rate (ORR) per RECIST v1.1 as assessed by independent review committee (IRC) and DoR.
Thirty-six patients were enrolled and were evaluable for response in the ATC cohort. The median age was 71 years (range: 47 to 85); 44% were male, 50% White, 44% Asian; and 94% had ECOG performance status of 0 or 1. Prior anti- cancer treatments included surgery and external beam radiotherapy (83% each), and systemic therapy (67%).
Efficacy results are summarized in Table 24.
Table 24. Efficacy Results in the ATC Cohort Based on Independent Review of Study BRF117019|
Abbreviations: ATC, anaplastic thyroid cancer; DoR, duration of response; CI, confidence interval; NE, not estimable; ORR, overall response rate. | |
|
ATC Cohort Population |
N = 36 |
|
Overall Response Rate | |
|
ORR (95% CI) |
53% (35.5%, 69.6%) |
|
Complete response |
6% |
|
Partial response |
47% |
|
Duration of Response |
n = 19 |
|
Median DoR, months (95% CI) |
13.6 (3.8, NE) |
|
% with DoR ≥ 6 months |
68% |
|
% with DoR ≥ 12 months |
53% |
14.6 BRAF V600E Mutation-Positive Unresectable or Metastatic Solid Tumors
The safety and efficacy of TAFINLAR in combination with trametinib for the treatment of BRAF V600E mutation-positive unresectable or metastatic solid tumors were evaluated in Trials BRF117019, NCI-MATCH, and CTMT212X2101, and supported by results in COMBI-d, COMBI-v [see Clinical Studies (14.2)], and BRF113928 [see Clinical Studies (14.4)]. In adult studies, patients received TAFINLAR 150 mg twice daily and trametinib 2 mg once daily. The major efficacy outcome measures were ORR per RECIST v1.1, RANO [HGG] or modified RANO [LGG] criteria and duration of response (DoR).
BRF117019 Study and NCI-MATCH Study
Study BRF117019 (NCT02034110) [see Clinical Studies (14.5)] is a multi-cohort, multi-center, non-randomized, open-label trial in adult patients with selected tumors with the BRAF V600E mutation, including high grade glioma (HGG) (n = 45), biliary tract cancer (BTC) (n = 43), low grade glioma (LGG) (n = 13), adenocarcinoma of small intestine (ASI) (n = 3), gastrointestinal stromal tumor (GIST) (n = 1), and anaplastic thyroid cancer [see Clinical Studies (14.5)]. Patients were enrolled based on local assessments of BRAF V600E mutation status; a central laboratory confirmed the BRAF mutation in 93 of 105 patients.
Arm H (EAY131-H) of the NCI-MATCH study (NCT02465060) is a single-arm, open- label study that enrolled patients with a BRAF V600E mutation. Patients with melanoma, thyroid cancer, or CRC were excluded. BRAF V600E mutation status for enrollment was determined either by central or local laboratory test. The study included adult patients with solid tumors including gastrointestinal tumors (n = 14), lung tumors (n = 7), gynecologic or peritoneal tumors (n = 6), CNS tumors (n = 4), and ameloblastoma of mandible (n = 1).
Among the 131 patients enrolled in BRF117019 and NCI-MATCH with the tumor types shown in Table 21, the baseline characteristics were: median age of 51 years with 20% age 65 or older; 56% female; 85% White, 9% Asian, 3% Black, 3% other; and 37% ECOG 0, 56% ECOG 1, and 6% ECOG 2. Of the 131 patients, 90% received prior systemic therapy.
Efficacy results in patients with solid tumors are summarized in Table 25.
Table 25. Efficacy Results Based on Independent Review in Studies BRF117019 and NCI-MATCH Arm H|
Abbreviations: PR, partial response. | ||||
|
Tumor Type****a |
N |
Objective Response Rate |
Duration of Response | |
|
% |
95% CI |
Range (months) | ||
|
Biliary tract cancerb |
48 |
46 |
(31, 61) |
1.8d, 40d |
|
High grade gliomac |
48 |
33 |
(20, 48) |
3.9, 44 |
|
Glioblastoma |
32 |
25 |
(12, 43) |
3.9, 27 |
|
Anaplastic pleomorphic xanthoastrocytoma |
6 |
67 |
(22, 96) |
6, 43 |
|
Anaplastic astrocytoma |
5 |
20 |
(0.5, 72) |
15 |
|
Astroblastoma |
2 |
100 |
(16, 100) |
15, 23d |
|
Undifferentiated |
1 |
PR |
(2.5, 100) |
6 |
|
Anaplastic ganglioglioma |
1 |
0 |
NA |
NA |
|
Anaplastic oligodendroglioma |
1 |
0 |
NA |
NA |
|
Low grade glioma |
14 |
50 |
(23, 77) |
6, 29d |
|
Astrocytoma |
4 |
50 |
(7, 93) |
7, 23 |
|
Ganglioglioma |
4 |
50 |
(7, 93) |
6, 13 |
|
Pleomorphic xanthoastrocytoma |
2 |
50 |
(1.3, 99) |
6 |
|
Pilocytic astrocytoma |
2 |
0 |
NA |
NA |
|
Choroid plexus papilloma |
1 |
PR |
(2.5, 100) |
29d |
|
Gangliocytoma/ganglioglioma |
1 |
PR |
(2.5, 100) |
18d |
|
Low grade serous ovarian carcinoma |
5 |
80 |
(28, 100) |
12, 42d |
|
Adenocarcinoma small intestine |
4 |
50 |
(7, 93) |
7, 8 |
|
Adenocarcinoma pancreas |
3 |
0 |
NA |
NA |
|
Mixed ductal/adenoneuroendocrine carcinoma |
2 |
0 |
NA |
NA |
|
Neuroendocrine carcinoma of colon |
2 |
0 |
NA |
NA |
|
Ameloblastoma of mandible |
1 |
PR |
(2.5, 100) |
30 |
|
Combined small cell-squamous carcinoma of lung |
1 |
PR |
(2.5, 100) |
5 |
|
Mucinous-papillary serous adenocarcinoma of peritoneum |
1 |
PR |
(2.5, 100) |
8 |
|
Adenocarcinoma of anus |
1 |
0 |
NA |
NA |
|
Gastrointestinal stromal tumor |
1 |
0 |
NA |
NA |
CTMT212X2101 (X2101) Study
Study X2101 (NCT02124772) was a multi-center, open-label, multi-cohort study in pediatric patients with refractory or recurrent solid tumors. Part C was a dose escalation of TAFINLAR in combination with trametinib in patients with a BRAF V600E mutation. Part D was a cohort expansion phase of TAFINLAR in combination with trametinib in patients with LGG with a BRAF V600E mutation. The major efficacy outcome measure was ORR as assessed by independent review committee per RANO criteria.
The efficacy of TAFINLAR in combination with trametinib was evaluated in 48 pediatric patients, including 34 patients with LGG and 2 patients with HGG.
For patients with BRAF V600E mutant LGG and HGG in Parts C and D, the median age was 10 years (range: 1 to 17); 50% were male, 75% White, 8% Asian, 3% Black; and 58% had Karnofsky/Lansky performance status of 100. Prior anti- cancer treatments included surgery (83%), external beam radiotherapy (2.8%), and systemic therapy (92%). The ORR was 25% (95% CI: 12%, 42%). For the 9 patients who responded, DoR was ≥ 6 months for 78% of patients and ≥ 24 months for 44% of patients.
CDRB436G2201 (G2201) Study – High-Grade Glioma Cohort
Study G2201 (NCT02684058) was a multi-center, randomized, open-label, Phase II study of dabrafenib and trametinib in chemotherapy naïve pediatric patients with BRAF V600E mutant low-grade glioma (LGG) and patients with relapsed or progressive BRAF V600E mutant HGG. Patients with HGG were enrolled in a single-arm cohort. The major efficacy outcome measure for the HGG cohort was ORR as assessed by independent review committee per RANO 2010 criteria.
The efficacy of TAFINLAR in combination with trametinib was evaluated in 41 pediatric patients with relapsed or progressive HGG.
For patients with BRAF V600E mutant HGG enrolled in the HGG cohort, the median age was 13 years (range: 2 to 17); 56% were female, 61% White, 27% Asian, 2.4% Black, and 37% had Karnofsky/Lansky performance status of 100. Prior anti- cancer treatments included surgery (98%), radiotherapy (90%), and chemotherapy (81%). The ORR was 56% (95% CI: 40, 72). The median DoR was not reached (95% CI: 9.2, NE). For the 23 patients who responded in the HGG cohort, DoR was ≥ 6 months for 78% of patients, ≥ 12 months for 48% of patients, and ≥ 24 months for 22% of patients.
14.7 BRAF V600E Mutation-Positive Low-Grade Glioma
CDRB436G2201 (G2201) Study – Low-Grade Glioma Cohort
The safety and efficacy of TAFINLAR in combination with trametinib for the treatment of BRAF V600E mutation-positive low-grade glioma (LGG) in pediatric patients aged 1 to < 18 years of age were evaluated in the multi-center, open- label trial (Study CDRB436G2201; NCT02684058). Patients with LGG (WHO grades 1 and 2) who required first systemic therapy were randomized in a 2:1 ratio to dabrafenib plus trametinib (D + T) or carboplatin plus vincristine (C + V).
BRAF mutation status was identified prospectively via a local assessment or a central laboratory test. In addition, retrospective testing of available tumor samples by the central laboratory was performed to evaluate BRAF V600E mutation status.
Patients received age- and weight-based dosing of TAFINLAR and trametinib until loss of clinical benefit or until unacceptable toxicity. Carboplatin and vincristine were dosed based on body surface area at doses 175 mg/m2 and 1.5 mg/m2 (0.05 mg/kg for patients < 12 kg), respectively, as one 10-week induction course followed by eight 6-week cycles of maintenance therapy.
The major efficacy outcome measure was overall response rate (ORR) by independent review based on RANO LGG (2017) criteria. Additional efficacy outcome measures were progression-free survival and overall survival. The primary analysis was performed when all patients had completed at least 32 weeks of therapy.
In the LGG cohort, 110 patients were randomized to D + T (n = 73) or C + V (n = 37). Median age was 9.5 years (range: 1 to 17); 60% were female. Study G2201 showed a statistically significant improvement in ORR and PFS in LGG patients randomized to D + T compared to those randomized to C + V. Efficacy results are shown in Table 26.
Table 26. Efficacy Results Based on Independent Review in Study G2201 (LGG Cohort)|
Abbreviations: CI, confidence interval; DoR, duration of response; NE, not
estimable; ORR, overall response rate. | ||
|
TAFINLAR plus Trametinib |
Carboplatin plus Vincristine | |
|
Overall Response Rate | ||
|
ORR% (95% CI)a |
46.6 (34.8, 58.6) |
10.8 (3.0, 25.4) |
|
P value |
< 0.001 | |
|
Complete response, n (%) |
2 (2.7) |
1 (2.7) |
|
Partial response, n (%) |
32 (44) |
3 (8) |
|
Duration of Response | ||
|
Median (95% CI)b, months |
23.7 (14.5, NE) |
NE (6.6, NE) |
|
% with observed DoR ≥ 12 months |
56 |
50 |
|
% with observed DoR ≥ 24 months |
15 |
25 |
|
Progression-Free Survival | ||
|
Median (95% CI)b, months |
20.1 (12.8, NE) |
7.4 (3.6, 11.8) |
|
Hazard ratio (95% CI)c |
0.31 (0.17, 0.55) | |
|
P value |
< 0.001 |
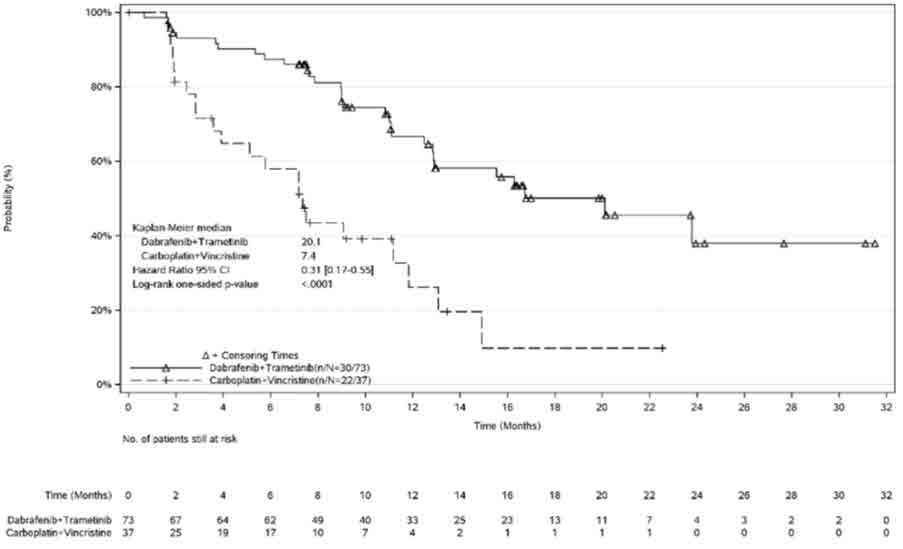
Figure 5. Kaplan-Meier Curves for Progression-Free Survival in Study G2201 (LGG Cohort)
At the time of the interim analysis of overall survival (OS), conducted when all patients had completed at least 32 weeks of treatment or had discontinued earlier, there was one death on the C + V arm. The OS results at interim analysis did not reach statistical significance.
HOW SUPPLIED SECTION
16** HOW SUPPLIED/STORAGE AND HANDLING**
TAFINLAR Capsules:
50 mg capsules: Dark red capsule imprinted with ‘GS TEW’ and ‘50 mg’ available in bottles of 120 with child-resistant closures (NDC 0078-0682-66). Each bottle contains a silica gel desiccant.
75 mg capsules: Dark pink capsule imprinted with ‘GS LHF’ and ‘75 mg’ available in bottles of 120 with child-resistant closures (NDC 0078-0681-66). Each bottle contains a silica gel desiccant.
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature]. Store and dispense in the original bottle with the desiccant.
TAFINLAR Tablets for Oral Suspension:
10 mg tablets for oral suspension: white to slightly yellow, round biconvex 6 mm tablet debossed with “D” on one side and “NVR” on the other side. Available in bottles of 210 with child-resistant closures (NDC 0078-1154-21). Each bottle contains 2 silica gel desiccants.
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature]. Store and dispense in the original bottle with the desiccant.
INSTRUCTIONS FOR USE SECTION
|
This Instructions for Use has been approved by the U.S. Food and Drug Administration. |
Revised: March 2024 |
|
INSTRUCTIONS FOR USE | |
|
This “Instructions for Use” contains information on how to prepare and take or give TAFINLAR tablets for oral suspension. | |
|
Important information you need to know before taking or giving TAFINLAR tablets for oral suspension | |
| |
|
The TAFINLAR pack should contain: | |
|
| |
|
You will also need drinking water. | |
|
Section A. Preparing and taking or giving a dose of the TAFINLAR oral suspension by swallowing directly from the dosing cup | |
|
If any of the TAFINLAR oral suspension comes into contact with your skin or
eyes when you are following the steps below, follow instructions in the
section**“Important information you need to know before taking or giving
TAFINLAR tablets for oral suspension”.**
To take or give a dose of TAFINLAR oral suspension by mouth (swallowing the TAFINLAR oral suspension), you or your child can drink it directly from the dosing cup. | |
|
Step 1. Wash and dry your hands before preparing TAFINLAR tablets as an oral suspension.
Note: The amount of water does not need to be exact.
|
|
|
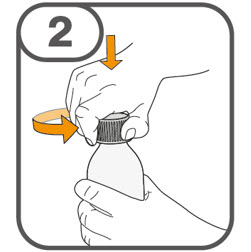
Step 2. Remove the bottle cap by pushing down and turning counter- clockwise in the direction of the arrow, as shown. *Do not throw away (dispose of) the cap.
|
|
|
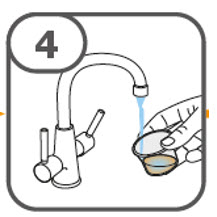
Step 3. Count out the prescribed number of tablets into your hand. |
|
|
|
|
|
|
Step 4. Place the cap back onto the bottle and turn it clockwise in the direction of the arrow, as shown to close it. |
|
|
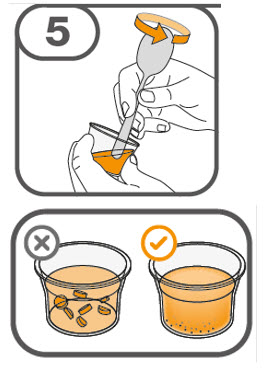
Step 5. With one hand, tilt the dosing cup.
|
|
|
Step 6. Drink the TAFINLAR oral suspension from the dosing cup. |
|
|
Step 7. Add about 5 mL of water to the empty dosing cup. |
|
|
Step 8. Stir with the handle of a teaspoon to loosen the remaining medicine residue. |
|
|
Step 9. Drink the water and medicine residue mixture. |
|
|
*If the prescribed dose is 1 to 4 tablets: Do Steps 7 through 9 one time. *If the prescribed dose is 5 to 15 tablets: Do Steps 7 through 9 two times. It is important to take or giveall of the medicine residue so that you get the full dose of TAFINLAR. | |
|
Step 10. Go toSection C. “Cleaning the dosing cup and oral syringe (if used)”. | |
|
Section B. Preparing and giving TAFINLAR tablets as an oral suspension via feeding tube or oral syringe | |
|
Important administration information
| |
|
Step 1. Follow Steps 1 through 5 in Section A to disperse the TAFINLAR tablets. If using a feeding tube, flush the feeding tube with drinking water then continue with Step 2 below. | |
|
Step 2. Draw up all of the TAFINLAR oral suspension from the dosing cup into an oral syringe by pulling back on the plunger. Be sure to use an oral syringe that can be used with the feeding tube or that can be used to give the TAFINLAR oral suspension by mouth. Ask your healthcare provider if you are not sure what oral syringe to use. |
|
|
Step 3. If giving the dose through a feeding tube, give the TAFINLAR oral suspension into the feeding tube according to the feeding tube manufacturer’s instructions. If giving a dose of TAFINLAR oral suspension using an oral syringe, place the open end of the oral syringe inside the mouth with the tip pointing toward the inside of either cheek. If you are giving a dose of the TAFINLAR oral suspension to a child, make sure they are sitting upright. Slowly push the plunger all the way down to give the full dose of TAFINLAR oral suspension. Warning: Giving TAFINLAR oral suspension directly into the throat or pushing down on the plunger too fast may cause choking. |
|
|
Step 4. Add about 5 mL of water to the empty dosing cup. |
|
|
Step 5. Stir with the handle of a teaspoon to loosen the remaining medicine residue inside the dosing cup. |
|
|
Step 6. Draw up the water and medicine residue mixture. |
|
|
Step 7. Give the water and medicine residue mixture through the feeding tube or into the inside of the cheek. |
|
| |
|
Step 8. After repeatingSteps 4 through 7 three times, flush the feeding tube with drinking water. Then go to the cleaning steps in Section C. | |
|
Section C. Cleaning the dosing cup and oral syringe (if used) | |
|
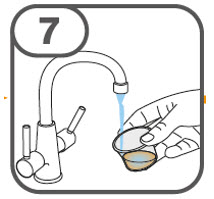
Use only clean water to rinse the dosing cup. Do not use soap or dishwashing liquid when cleaning the dosing cup. | |
|
Step 1. Rinse the dosing cup under clean cool water right away after dosing.
Note: Keep the dosing cup away from other kitchen items. |
|
|
Step 2. Rinse the teaspoon in clean cold water then wash in warm soapy water and dry using clean paper towels.
|
|
|
Step 3. Clean the used oral syringe, as instructed by your healthcare provider, or according to the manufacturer’s instructions. |
|
|
Section D. How to throw away TAFINLAR tablets or oral suspension that are expired or no longer needed, or old dosing cups | |
| |
|
Section E. How to clean up any spilled TAFINLAR oral suspension | |
|
If you accidentally spill any TAFINLAR oral suspension, clean up the spill as
follows: | |
|
How should I store TAFINLAR tablets for oral suspension? | |
Keep TAFINLAR and all medicines out of the reach of children. | |
|
Distributed by: © Novartis |
T2024-24
SPL MEDGUIDE SECTION
|
This Medication Guide has been approved by the U.S. Food and Drug Administration. |
Revised: March 2024 |
|
MEDICATION GUIDE | |
|
TAFINLAR® (TAFF-in-lar) |
TAFINLAR® (TAFF-in-lar) |
|
Important information: If your healthcare provider prescribes TAFINLAR for you to be taken or given with trametinib, also read the Patient Information leaflet that comes with trametinib. | |
|
What is the most important information I should know about TAFINLAR?
Your healthcare provider should check your skin before treatment with
TAFINLAR, every 2 months during treatment with TAFINLAR, and for up to 6
months after you stop taking TAFINLAR to look for any new skin cancers. | |
|
What is TAFINLAR?
TAFINLAR is not for use in treating people with colorectal cancer or wild-type
BRAF solid tumors. | |
|
Before you take or give TAFINLAR, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including
prescription and over-the-counter medicines, vitamins, and herbal supplements. | |
|
How should I take or give TAFINLAR?
TAFINLAR capsules:
TAFINLAR tablets for oral suspension:
| |
|
What are the possible side effects of TAFINLAR? *See “What is the most important information I should know about TAFINLAR?” *bleeding problems. TAFINLAR, when taken or given with trametinib, can cause serious bleeding problems, especially in your brain or stomach, that can lead to death. Call your healthcare provider and get medical help right away if you have any signs of bleeding, including: *heart problems, including heart failure. Your healthcare provider should check your heart function before and during treatment with TAFINLAR. Call your healthcare provider right away if you have any of the following signs and symptoms of a heart problem: *eye problems. TAFINLAR can cause severe eye problems that can lead to blindness. Call your healthcare provider right away if you get these symptoms of eye problems: *fever. Fever is common during treatment with TAFINLAR, but may also be serious. When taking TAFINLAR with trametinib, fever may happen more often or may be more severe. In some cases, chills or shaking chills, too much fluid loss (dehydration), low blood pressure, dizziness, or kidney problems may happen with the fever. *serious skin reactions. Skin rash is a common side effect of TAFINLAR. TAFINLAR can also cause other skin reactions. In some cases, these rashes and other skin reactions can be severe or serious and may need to be treated in a hospital or lead to death. Tell your healthcare provider if you get a skin rash or acne that bothers you or worsens. Tell your healthcare provider right away if you develop any of the following signs or symptoms of a severe skin reaction, including: | |
|
○ blisters or peeling of your skin |
○ blisters on your lips, or around your mouth or eyes |
|
*increased blood sugar (hyperglycemia). Some people may develop high blood sugar or worsening diabetes during treatment with TAFINLAR. If you are diabetic, your healthcare provider should check your blood sugar levels closely during treatment with TAFINLAR. Your diabetes medicine may need to be changed. Tell your healthcare provider if you have any of the following symptoms of severe high blood sugar:
* increased thirst
* urinating more often than normal, or urinating an increased amount of urine
*TAFINLAR may cause healthy red blood cells to break down too early in people with G6PD deficiency. This may lead to a type of anemia called hemolytic anemia where the body does not have enough healthy red blood cells. Tell your healthcare provider if you have any of the following signs or symptoms: *hemophagocytic lymphohistiocytosis (HLH). TAFINLAR when taken or given with trametinib may increase the risk of a type of overactivity of the immune system (hemophagocytic lymphohistiocytosis) that can cause fever, swollen glands, bruising, or skin rash. If you experience a combination of these symptoms, call your healthcare provider right away. The most common side effects of TAFINLAR when taken alone include: | |
|
• thickening of the outer layers of the skin |
• warts |
|
• headache |
• hair loss |
|
• fever |
• redness, swelling, peeling, or tenderness of hands or feet |
|
• joint aches | |
|
The most common side effects of TAFINLAR when taken with trametinib in people with melanoma that has spread to other parts of the body or cannot be removed by surgery include: | |
|
• fever |
• chills |
|
• rash |
• joint aches |
|
• headache |
• cough |
|
The most common side effects of TAFINLAR when taken with trametinib to help prevent melanoma from coming back after the cancer has been removed by surgery include: | |
|
• fever |
• chills |
|
• tiredness |
• diarrhea |
|
• nausea |
• vomiting |
|
• headache |
• joint aches |
|
• rash |
• muscle aches |
|
The most common side effects of TAFINLAR when taken with trametinib in people with NSCLC include: | |
|
• fever |
• rash |
|
• tiredness |
• swelling of face, arms, and legs |
|
• nausea |
• chills |
|
• vomiting |
• bleeding |
|
• diarrhea |
• cough |
|
• dry skin |
• shortness of breath |
|
• decreased appetite | |
|
The most common side effects of TAFINLAR when taken with trametinib in adults with solid tumors that cannot be removed by surgery or have spread to other parts of the body include: | |
|
• fever |
• bleeding |
|
• tiredness |
• cough |
|
• nausea |
• vomiting |
|
• rash |
• constipation |
|
• chills |
• diarrhea |
|
• headache |
• muscle and joint aches |
|
• swelling of your arms and legs | |
|
The most common side effects of TAFINLAR when taken or given with trametinib in children 1 year of age and older with solid tumors that cannot be removed by surgery or have spread to other parts of the body include: | |
|
• fever |
• acne |
|
• rash |
• headache |
|
• vomiting |
• stomach-area (abdominal) pain |
|
• tiredness |
• nausea |
|
• dry skin |
• bleeding |
|
• cough |
• constipation |
|
• diarrhea |
• skin infection around fingernails or toenails |
|
The most common side effects of TAFINLAR when taken or given with trametinib in children 1 year of age and older with low-grade glioma include: | |
|
• fever |
• dry skin |
|
• rash |
• diarrhea |
|
• headache |
• nausea |
|
• vomiting |
• bleeding |
|
• muscle and bone pain |
• stomach-area (abdominal) pain |
|
• tiredness |
• acne |
|
TAFINLAR may cause fertility problems in females. This could affect your
ability to become pregnant. Talk to your healthcare provider if this is a
concern for you. | |
|
How should I store TAFINLAR?
TAFINLAR tablets for oral suspension:
Keep TAFINLAR and all medicines out of the reach of children. | |
|
General information about the safe and effective use of TAFINLAR | |
|
What are the ingredients in TAFINLAR? Distributed by: Novartis Pharmaceuticals Corporation, East Hanover, New Jersey
07936 |
T2024-23
DOSAGE & ADMINISTRATION SECTION
2** DOSAGE AND ADMINISTRATION**
2.1 Patient Selection
Melanoma
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with TAFINLAR as a single agent [see Warnings and Precautions (5.2), Clinical Studies (14.1)].
- Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of treatment with TAFINLAR and trametinib [see Warnings and Precautions (5.2), Clinical Studies (14.2, 14.3)].
- Information on FDA-approved tests for the detection of BRAF V600 mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics.
NSCLC
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with TAFINLAR and trametinib [see Clinical Studies (14.4)].
- Information on FDA-approved tests for the detection of BRAF V600E mutations in NSCLC is available at: http://www.fda.gov/CompanionDiagnostics.
ATC
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with TAFINLAR and trametinib [see Clinical Studies (14.5)]. An FDA-approved test for the detection of BRAF V600E mutation in ATC is not currently available.
Solid Tumors
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with TAFINLAR and trametinib [see Clinical Studies (14.6)]. An FDA-approved test for the detection of BRAF V600E mutation in solid tumors other than melanoma and NSCLC is not currently available.
Low-Grade Glioma
- Confirm the presence of BRAF V600E mutation in tumor specimens prior to initiation of treatment with TAFINLAR and trametinib [see Clinical Studies (14.7)]. An FDA-approved test for the detection of BRAF V600E mutation in LGG is not currently available.
2.2 Recommended Dosage
TAFINLAR Capsules
Adult Patients
The recommended dosage for TAFINLAR capsules in adult patients is 150 mg taken orally twice daily [see Dosage and Administration (2.3)].
Pediatric Patients
The recommended dosage for TAFINLAR capsules in pediatric patients who weigh at least 26 kg is based on body weight (Table 1) [see Dosage and Administration (2.3)]. A recommended dosage of TAFINLAR capsules has not been established in patients who weigh less than 26 kg.
Table 1. Recommended Dosage for TAFINLAR Capsules in Pediatric Patients (Weight-based)|
Body Weight |
Recommended Dosage |
|
26 to 37 kg |
75 mg orally twice daily |
|
38 to 50 kg |
100 mg orally twice daily |
|
51 kg or greater |
150 mg orally twice daily |
TAFINLAR Tablets for Oral Suspension
The recommended dosage for TAFINLAR tablets for oral suspension is based on body weight (Table 2) [see Dosage and Administration (2.3)].
Table 2. Recommended Dosage for TAFINLAR Tablets for Oral Suspension (Weight-based)|
Body Weight |
Recommended Dosage |
|
8 to 9 kg |
20 mg twice daily |
|
10 to 13 kg |
30 mg twice daily |
|
14 to 17 kg |
40 mg twice daily |
|
18 to 21 kg |
50 mg twice daily |
|
22 to 25 kg |
60 mg twice daily |
|
26 to 29 kg |
70 mg twice daily |
|
30 to 33 kg |
80 mg twice daily |
|
34 to 37 kg |
90 mg twice daily |
|
38 to 41 kg |
100 mg twice daily |
|
42 to 45 kg |
110 mg twice daily |
|
46 to 50 kg |
130 mg twice daily |
|
≥ 51 kg |
150 mg twice daily |
- The recommended duration of treatment for patients with unresectable or metastatic melanoma or solid tumors, metastatic NSCLC, or locally advanced or metastatic anaplastic thyroid cancer is until disease progression or unacceptable toxicity.
- The recommended duration of treatment in the adjuvant melanoma setting is until disease recurrence or unacceptable toxicity for up to 1 year.
- The recommended duration of treatment for pediatric patients with LGG is until disease progression or until unacceptable toxicity.
Refer to the trametinib prescribing information for recommended trametinib dosing information.
2.3 Administration
- Take TAFINLAR at the same time each day, approximately 12 hours apart.
- Take TAFINLAR at least 1 hour before or 2 hours after a meal [see Clinical Pharmacology (12.3)].
- Do not take a missed dose of TAFINLAR within 6 hours of the next dose of TAFINLAR.
- If vomiting occurs after TAFINLAR administration, do not take an additional dose. Take the next dose at its scheduled time.
TAFINLAR Capsules
- Do not open, crush, or break TAFINLAR capsules.
TAFINLAR Tablets for Oral Suspension
- Prior to use of the oral suspension, instruct caregivers (and if appropriate, patients) on proper dosing and administration of TAFINLAR tablets for oral suspension.
- Do not swallow whole, chew or crush TAFINLAR tablets for oral suspension.
Preparation and Administration
- Prepare the oral suspension with approximately 5 mL of water for 1 to 4 tablets, and approximately 10 mL of water for 5 to 15 tablets in the provided dosing cup.
- Gently stir the water and prescribed number of tablets with the handle of a teaspoon until the tablets are fully dissolved. It may take at least 3 minutes to fully dissolve the tablets. Once the tablets are dissolved, the oral suspension will be cloudy white.
- Administer the oral suspension immediately after preparation from a dosing cup, oral syringe or feeding tube (10 French gauge or larger for 1 to 3 tablets; 12 French gauge or larger for 4 to 15 tablets).
- Discard the oral suspension if not administered within 30 minutes after preparation.
2.4 Dosage Modifications for Adverse Reactions
Dose reductions for adverse reactions associated with TAFINLAR are presented in Tables 3 and 4.
Table 3. Recommended Dosage Reductions for TAFINLAR Capsules for Adverse Reactions|
Recommended Dosage |
75 mg orally twice daily |
100 mg orally twice daily |
150 mg orally twice daily |
|
First dose reduction |
50 mg orally twice daily |
75 mg orally twice daily |
100 mg orally twice daily |
|
Second dose reduction |
N/A |
50 mg orally twice daily |
75 mg orally twice daily |
|
Third dose reduction |
N/A |
N/A |
50 mg orally twice daily |
|
Subsequent modification |
Permanently discontinue if unable to tolerate TAFINLAR capsules 50 mg orally twice daily. |
|
Body Weight |
First Dose Reduction |
Second Dose Reduction |
Third Dose Reduction |
|
Tablets for oral suspension twice daily | |||
|
8 to 9 kg |
10 mg twice daily |
N/A |
N/A |
|
10 to 13 kg |
20 mg twice daily |
10 mg twice daily |
N/A |
|
14 to 17 kg |
30 mg twice daily |
20 mg twice daily |
10 mg twice daily |
|
18 to 21 kg |
30 mg twice daily |
20 mg twice daily |
10 mg twice daily |
|
22 to 25 kg |
40 mg twice daily |
30 mg twice daily |
20 mg twice daily |
|
26 to 29 kg |
50 mg twice daily |
40 mg twice daily |
20 mg twice daily |
|
30 to 33 kg |
50 mg twice daily |
40 mg twice daily |
30 mg twice daily |
|
34 to 37 kg |
60 mg twice daily |
50 mg twice daily |
30 mg twice daily |
|
38 to 41 kg |
70 mg twice daily |
50 mg twice daily |
30 mg twice daily |
|
42 to 45 kg |
70 mg twice daily |
60 mg twice daily |
40 mg twice daily |
|
46 to 50 kg |
90 mg twice daily |
70 mg twice daily |
40 mg twice daily |
|
≥ 51 kg |
100 mg twice daily |
80 mg twice daily |
50 mg twice daily |
Dosage modifications for adverse reactions associated with TAFINLAR are presented in Table 5.
Table 5. Recommended Dosage Modifications for TAFINLAR for Adverse Reactions|
a National Cancer Institute Common Terminology Criteria for Adverse Events
(NCI CTCAE) version 4.0. | |
|
Severity of AdverseReactiona |
Dosage Modification for TAFINLAR****b |
|
New Primary Malignancies [see Warnings and Precautions (5.1)] | |
|
Non-Cutaneous RAS Mutation-positive Malignancies |
Permanently discontinue TAFINLAR. |
|
Cardiomyopathy [see Warnings and Precautions (5.4)] | |
|
Withhold TAFINLAR until LVEF improves to at least the institutional LLN and absolute decrease to less than or equal to 10% compared to baseline, then resume TAFINLAR at same dose. |
|
Uveitis [see Warnings and Precautions (5.5)] | |
|
For mild or moderate uveitis that does not respond to ocular therapy, or for severe uveitis, withhold TAFINLAR for up to 6 weeks.
|
|
Febrile Reactions [see Warnings and Precautions (5.6)] | |
|
Withhold TAFINLAR until fever resolves, then resume TAFINLAR at same or lower dose. |
|
Or
|
|
Skin Toxicities [see Warnings and Precautions (5.7)] | |
|
Withhold TAFINLAR for up to 3 weeks.
|
|
Permanently discontinue TAFINLAR. |
|
Other Adverse Reactionsc, including Hemorrhage [see Warnings and Precautions (5.3)] | |
|
Withhold TAFINLAR.
|
|
Or
|
|
Permanently discontinue TAFINLAR. |
Refer to the trametinib prescribing information for dose modifications for adverse reactions associated with trametinib.
- The recommended dosage of TAFINLAR in adult patients is 150 mg (two 75 mg capsules) orally twice daily. The recommended dosage for TAFINLAR in pediatric patients is based on body weight. Take TAFINLAR at least 1 hour before or at least 2 hours after a meal. (2)
USE IN SPECIFIC POPULATIONS SECTION
8** USE IN SPECIFIC POPULATIONS**
8.1 Pregnancy
Risk Summary
Based on findings from animal reproduction studies and its mechanism of action [see Clinical Pharmacology (12.1)], TAFINLAR can cause fetal harm when administered to a pregnant woman. There is insufficient data in pregnant women exposed to TAFINLAR to assess the risks. Dabrafenib was teratogenic and embryotoxic in rats at doses three times greater than the human exposure at the recommended adult clinical dose of 150 mg twice daily (see Data). Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In a combined female fertility and embryo-fetal development study in rats conducted during the period of organogenesis, developmental toxicity consisted of embryo-lethality, ventricular septal defects, and variation in thymic shape at a dabrafenib dose of 300 mg/kg/day [approximately three times the human exposure at the recommended adult dose based on area under the curve (AUC)]. At doses of 20 mg/kg/day or greater (equivalent to the human exposure at the recommended adult dose based on AUC), rats demonstrated delays in skeletal development and reduced fetal body weight.
8.2 Lactation
Risk Summary
There are no data on the presence of dabrafenib in human milk, or the effects of dabrafenib on the breastfed child or on milk production. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment with TAFINLAR and for 2 weeks following the last dose.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status in females of reproductive potential prior to initiating TAFINLAR.
Contraception
Based on data from animal studies and its mechanism of action, TAFINLAR can cause fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)].
Females
Advise female patients of reproductive potential to use effective contraception during treatment with TAFINLAR and for 2 weeks after the last dose. Counsel patients to use a non-hormonal method of contraception since TAFINLAR can render hormonal contraceptives ineffective [see Drug Interactions (7.2)].
Males
To avoid potential drug exposure to pregnant partners and female partners of reproductive potential, advise male patients (including those who have had vasectomies) with female partners of reproductive potential to use condoms during treatment with TAFINLAR and for 2 weeks after the last dose.
Infertility
Females
Advise female patients of reproductive potential that TAFINLAR may impair fertility. A reduction in fertility was observed in female rats at dose exposures equivalent to the human exposure at the recommended adult dose. A reduction in the number of corpora lutea was noted in pregnant rats at dose exposures approximately three times the human exposure at the recommended adult dose [see Nonclinical Toxicology (13.1)].
Males
Advise male patients of the potential risk for impaired spermatogenesis which may be irreversible. Effects on spermatogenesis have been observed in animals treated with dabrafenib at dose exposures up to three times the human exposure at the recommended adult dose [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
BRAF V600E Mutation-Positive Unresectable or Metastatic Solid Tumors and LGG
The safety and effectiveness of TAFINLAR in combination with trametinib have been established in pediatric patients 1 year of age and older with unresectable or metastatic solid tumors with BRAF V600E mutation who have progressed following prior treatment and have no satisfactory alternative treatment options; or with LGG with BRAF V600E mutation who require systemic therapy. Use of TAFINLAR in combination with trametinib for these indications is supported by evidence from studies X2101 and G2201 that enrolled 171 patients (1 to < 18 years) with BRAF V600 mutation-positive advanced solid tumors, of which 4 (2.3%) patients were 1 to < 2 years of age, 39 (23%) patients were 2 to < 6 years of age, 54 (32%) patients were 6 to < 12 years of age, and 74 (43%) patients were 12 to < 18 years of age [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), Clinical Studies (14.6, 14.7)].
The safety and effectiveness of TAFINLAR in combination with trametinib have not been established for these indications in pediatric patients less than 1 year old.
The safety and effectiveness of TAFINLAR as a single agent in pediatric patients have not been established.
Juvenile Animal Toxicity Data
In a repeat-dose toxicity study in juvenile rats, an increased incidence of kidney cysts and tubular deposits were noted at doses as low as 0.2 times the human exposure at the recommended adult dose based on AUC. Additionally, forestomach hyperplasia, decreased bone length, and early vaginal opening were noted at doses as low as 0.8 times the human exposure at the recommended adult dose based on AUC.
8.5 Geriatric Use
Of the 586 patients with various solid tumors who received single agent TAFINLAR, 22% were aged 65 years and older. Of the 187 patients with melanoma who received single-agent TAFINLAR in the BREAK-3 study, 21% were aged 65 years or older [see Clinical Studies (14.1)]. No overall differences in the effectiveness or safety of TAFINLAR were observed between geriatric patients as compared to younger adults in the BREAK-3 study.
Of the 994 patients with melanoma who received TAFINLAR plus trametinib in the COMBI-d, COMBI-v, and COMBI-AD studies [see Clinical Studies (14.2, 14.3)], 21% were aged 65 years and older and 5% were aged 75 years and older. No overall differences in the effectiveness of TAFINLAR plus trametinib were observed in geriatric patients as compared to younger adults across these melanoma studies. The incidences of peripheral edema (26% vs. 12%) and anorexia (21% vs. 9%) were increased in geriatric patients as compared to younger adults in these studies.
Of the 171 patients with NSCLC who received TAFINLAR in Study BRF113928, there were insufficient numbers of geriatric patients to determine whether they respond differently from younger adults [see Clinical Studies (14.4)].
Of the 26 patients with ATC who received TAFINLAR in Study BRF117019, 77% were aged 65 years and older, and 31% were aged 75 years and older [see Clinical Studies (14.5)]. This study in ATC did not include sufficient numbers of younger adults to determine whether they respond differently compared to geriatric patients.
8.6 Hepatic Impairment
Dose adjustment is not recommended for patients with mild (bilirubin ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN or bilirubin
1x to 1.5x ULN and any AST) hepatic impairment. As hepatic metabolism and biliary secretion are the primary routes of elimination of dabrafenib and its metabolites, patients with moderate (bilirubin > 1.5x to 3x ULN and any AST) to severe (bilirubin > 3x to 10x ULN and any AST) hepatic impairment may have increased exposure. An appropriate dosage has not been established for patients with moderate to severe hepatic impairment [see Clinical Pharmacology (12.3)].
-
Lactation: Do not breastfeed. (8.2)
-
Females and Males of Reproductive Potential: May impair fertility. (8.3)
DESCRIPTION SECTION
11** DESCRIPTION**
Dabrafenib mesylate is a kinase inhibitor. The chemical name for dabrafenib mesylate is N-{3-[5-(2-amino-4-pyrimidinyl)-2-(1,1-dimethylethyl)-1,3-thiazol-4-yl]-2-fluorophenyl}-2,6-difluorobenzene sulfonamide, methanesulfonate salt. It has the molecular formula C23H20F3N5O2S2•CH4O3S and a molecular weight of 615.68 g/mol. Dabrafenib mesylate has the following chemical structure:
![The following chemical structure for Dabrafenib mesylate is a kinase inhibitor. The chemical name for dabrafenib mesylate is N-{3-[5-(2-amino-4-pyrimidinyl)-2-(1,1-dimethylethyl)-1,3-thiazol-4-yl]-2-fluorophenyl}-2,6-difluorobenzene
sulfonamide, methanesulfonate salt. It has the molecular formula
C23H20F3N5O2S2•CH4O3S and a molecular weight of
615.68.](https://medical-cdn.nocode.com/data-engine/drug_fda/fee1e6b1-e1a5-4254-9f2e-a70e0f8dbdea/tafinlar_01_jpg/c01a9d1d0cedc8ad70ce589b03bf0273.jpg)
Dabrafenib mesylate is a white to slightly colored solid with three pKas: 6.6, 2.2, and -1.5. It is very slightly soluble at pH 1 and practically insoluble above pH 4 in aqueous media.
TAFINLAR (dabrafenib) capsules for oral use are supplied as 50 mg and 75 mg capsules for oral administration. Each 50 mg capsule contains 59.25 mg dabrafenib mesylate equivalent to 50 mg of dabrafenib free base. Each 75 mg capsule contains 88.88 mg dabrafenib mesylate equivalent to 75 mg of dabrafenib free base. The inactive ingredients of TAFINLAR capsules are colloidal silicon dioxide, magnesium stearate, and microcrystalline cellulose. Capsule shells contain hypromellose, red iron oxide (E172), and titanium dioxide (E171).
TAFINLAR (dabrafenib) tablets for oral suspension are supplied as 10 mg tablets for oral administration. Each 10 mg tablet contains 11.85 mg dabrafenib mesylate equivalent to 10 mg of dabrafenib base. The inactive ingredients of TAFINLAR tablets are acesulfame potassium, artificial berry flavor, colloidal silicon dioxide, crospovidone, hypromellose, magnesium stearate, mannitol, microcrystalline cellulose.
NONCLINICAL TOXICOLOGY SECTION
13** NONCLINICAL TOXICOLOGY**
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with dabrafenib have not been conducted. TAFINLAR increased the risk of cuSCCs in patients in clinical trials.
Dabrafenib was not mutagenic in vitro in the bacterial reverse mutation assay (Ames test) or the mouse lymphoma assay and was not clastogenic in an in vivo rat bone marrow micronucleus test.
In a combined female fertility and embryo-fetal development study in rats, a reduction in fertility was noted at doses greater than or equal to 20 mg/kg/day (equivalent to the human exposure at the recommended adult dose based on AUC). A reduction in the number of ovarian corpora lutea was noted in pregnant females at 300 mg/kg/day (which is approximately three times the human exposure at the recommended adult dose based on AUC).
Male fertility studies with dabrafenib have not been conducted; however, in repeat-dose studies, testicular degeneration/depletion was seen in rats and dogs at doses equivalent to and three times the human exposure at the recommended adult dose based on AUC, respectively.
13.2 Animal Toxicology and/or Pharmacology
Adverse cardiovascular effects were noted in dogs at dabrafenib doses of 50 mg/kg/day (approximately five times the human exposure at the recommended adult dose based on AUC) or greater, when administered for up to 4 weeks. Adverse effects consisted of coronary arterial degeneration/necrosis and hemorrhage, as well as cardiac atrioventricular valve hypertrophy/hemorrhage.
INFORMATION FOR PATIENTS SECTION
17** PATIENT COUNSELING INFORMATION**
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
New Primary Cutaneous and Non-Cutaneous Malignancies
Advise patients that TAFINLAR increases the risk of developing new primary cutaneous and non-cutaneous malignancies. Advise patients to contact their healthcare provider immediately for any new lesions, changes to existing lesions on their skin, or signs and symptoms of other malignancies [see Warnings and Precautions (5.1)].
Hemorrhage
Advise patients that TAFINLAR administered with trametinib increases the risk of intracranial and gastrointestinal hemorrhage. Advise patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual bleeding or hemorrhage [see Warnings and Precautions (5.3)].
Cardiomyopathy
Advise patients that TAFINLAR can cause cardiomyopathy and to immediately report any signs or symptoms of heart failure to their healthcare provider [see Warnings and Precautions (5.4)].
Uveitis
Advise patients that TAFINLAR can cause uveitis, including iritis and iridocyclitis and to contact their healthcare provider if they experience any changes in their vision [see Warnings and Precautions (5.5)].
Serious Febrile Reactions
Advise patients that TAFINLAR can cause pyrexia, including serious febrile reactions. Inform patients that the incidence and severity of pyrexia are increased when TAFINLAR is administered with trametinib. Instruct patients to contact their healthcare provider if they develop a fever while taking TAFINLAR [see Warnings and Precautions (5.6)].
Serious Skin Toxicities
Advise patients that TAFINLAR can cause serious skin toxicities and to contact their healthcare provider for progressive or intolerable rash. Advise patients to contact their healthcare provider immediately if they develop signs and symptoms of a severe skin reaction [see Warnings and Precautions (5.7)].
Hyperglycemia
Advise patients that TAFINLAR can impair glucose control in diabetic patients resulting in the need for more intensive hypoglycemic treatment and to contact their healthcare provider to report symptoms of severe hyperglycemia [see Warnings and Precautions (5.8)].
Glucose-6-phosphate Dehydrogenase (G6PD) Deficiency
Advise patients that TAFINLAR may cause hemolytic anemia in patients with G6PD deficiency. Advise patients with known G6PD deficiency to contact their healthcare provider to report signs or symptoms of anemia or hemolysis [see Warnings and Precautions (5.9)].
Embryo-Fetal Toxicity
- Advise pregnant women and females of reproductive potential of the potential risk to a fetus [see Warnings and Precautions (5.12), Use in Specific Populations (8.1, 8.3)].
- Advise females to contact their healthcare provider of a known or suspected pregnancy.
- Advise females of reproductive potential to use effective non-hormonal contraception during treatment and for 2 weeks after discontinuation of treatment with TAFINLAR.
- Advise male patients with female partners of reproductive potential to use condoms during treatment with TAFINLAR and for 2 weeks after the last dose.
Lactation
Advise women not to breastfeed during treatment with TAFINLAR and for 2 weeks after the last dose of TAFINLAR [see Use in Specific Populations (8.2)].
Infertility
Advise males and females of reproductive potential of the potential risk for impaired fertility with TAFINLAR [see Use in Specific Populations (8.3)].
Administration
Instruct patients to take TAFINLAR at least 1 hour before or at least 2 hours after a meal [see Dosage and Administration (2.3)].
tHxID™ is a trademark of bioMérieux.
Oncomine™ Dx Target Test is a trademark of Life Technologies Corporation, a part of Thermo Fisher Scientific Inc.
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2024-22