Tacrolimus
These highlights do not include all the information needed to use TACROLIMUS CAPSULES safely and effectively. See full prescribing information for TACROLIMUS CAPSULES. TACROLIMUS capsules, for oral use Initial U.S. Approval: 1994
bd447ffa-9196-4c3c-accf-5adf29b84665
HUMAN PRESCRIPTION DRUG LABEL
Jan 5, 2024
Accord Healthcare Inc.
DUNS: 604222237
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Tacrolimus
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Tacrolimus
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Tacrolimus
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
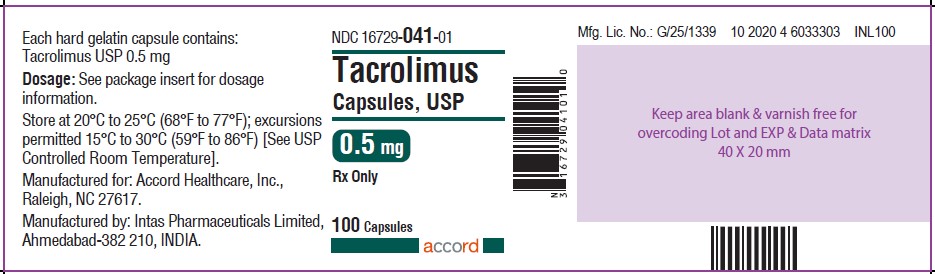
** Tacrolimus Capsules USP 0.5 mg-100 Capsules-Label**
Tacrolimus Capsules USP 1 mg-100 Capsules-Label

Tacrolimus Capsules USP 5 mg-100 Capsules-Label

WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Lymphoma and Other Malignancies
Patients receiving immunosuppressants, including tacrolimus, are at increased risk of developing lymphomas and other malignancies, particularly of the skin. The risk appears to be related to the intensity and duration of immunosuppression rather than to the use of any specific agent.
As usual for patients with increased risk for skin cancer, examine patients for skin changes; exposure to sunlight and UV light should be limited by wearing protective clothing and using a broad-spectrum sunscreen with a high protection factor.
Post-transplant lymphoproliferative disorder (PTLD) has been reported in immunosuppressed organ transplant recipients. The majority of PTLD events appear related to Epstein Barr Virus (EBV) infection. The risk of PTLD appears greatest in those individuals who are EBV seronegative, a population which includes many young children. Monitor EBV serology during treatment.
5.2 Serious Infections
Patients receiving immunosuppressants, including tacrolimus, are at increased risk of developing bacterial, viral, fungal, and protozoal infections, including opportunistic infections. These infections may lead to serious, including fatal, outcomes. Serious viral infections reported include:
- Polyomavirus-associated nephropathy (PVAN), mostly due to BK virus infection
- JC virus-associated progressive multifocal leukoencephalopathy (PML)
- Cytomegalovirus infections: CMV seronegative transplant patients who receive an organ from a CMV seropositive donor disease are at higher risk of developing CMV viremia and CMV disease.
Monitor for the development of infection and adjust the immunosuppressive regimen to balance the risk of rejection with the risk of infection [see Adverse Reactions (6.1, 6.2)] .
5.3 Not Interchangeable with Extended-Release Tacrolimus Products -
Medication Errors
Medication errors, including substitution and dispensing errors, between tacrolimus immediate-release products and tacrolimus extended-release products were reported outside the U.S. This led to serious adverse reactions, including graft rejection, or other adverse reactions due to under-or overexposure to tacrolimus. Tacrolimus is not interchangeable or substitutable for tacrolimus extended-release products. Changes between tacrolimus immediate-release and extended-release dosage forms must occur under physician supervision. Instruct patients and caregivers to recognize the appearance of tacrolimus dosage forms [see Dosage Forms and Strengths (3)] and to confirm with the healthcare provider if a different product is dispensed.
5.4 New Onset Diabetes After Transplant
Tacrolimus was shown to cause new onset diabetes mellitus in clinical trials of kidney, liver, or heart transplantation. New onset diabetes after transplantation may be reversible in some patients. African-American and Hispanic kidney transplant patients are at an increased risk. Blood glucose concentrations should be monitored closely in patients using tacrolimus [see Adverse Reactions (6.1)] .
5.5 Nephrotoxicity due to Tacrolimus and Drug Interactions
Tacrolimus, like other calcineurin inhibitors, can cause acute or chronic nephrotoxicity in transplant patients due to its vasoconstrictive effect on renal vasculature, toxic tubulopathy and tubular-interstitial effects. Nephrotoxicity was reported in clinical trials [see Adverse Reactions (6.1)].
Acute renal impairment associated with tacrolimus toxicity can result in high serum creatinine, hyperkalemia, decreased secretion of urea and hyperuricemia, and is usually reversible. In patients with elevated serum creatinine and tacrolimus whole blood trough concentrations greater than the recommended range, consider dosage reduction or temporary interruption of tacrolimus administration.
The risk for nephrotoxicity may increase when tacrolimus is concomitantly administered with CYP3A inhibitors (by increasing tacrolimus whole blood concentrations) or drugs associated with nephrotoxicity (e.g., aminoglycosides, ganciclovir, amphotericin B, cisplatin, nucleotide reverse transcriptase inhibitors, protease inhibitors). When tacrolimus is used concurrently with other known nephrotoxic drugs, monitor renal function and tacrolimus blood concentrations, and adjust doses of both tacrolimus and/or concomitant medications during concurrent use [see Drug Interactions (7.2)] .
5.6 Neurotoxicity
Tacrolimus may cause a spectrum of neurotoxicities. The most severe neurotoxicities include posterior reversible encephalopathy syndrome (PRES), delirium, seizure and coma; others include tremors, paresthesias, headache, mental status changes, and changes in motor and sensory functions [see Adverse Reactions (6.1, 6.2)] . As symptoms may be associated with tacrolimus whole blood trough concentrations at or above the recommended range, monitor for neurologic symptoms and consider dosage reduction or discontinuation of tacrolimus if neurotoxicity occurs.
5.7 Hyperkalemia
Hyperkalemia has been reported with tacrolimus use. Serum potassium levels should be monitored. Careful consideration should be given prior to use of other agents also associated with hyperkalemia (e.g., potassium-sparing diuretics, ACE inhibitors, angiotensin receptor blockers) during tacrolimus therapy [see Adverse Reactions (6.1)]. Monitor serum potassium levels periodically during treatment.
5.8 Hypertension
Hypertension is a common adverse effect of tacrolimus therapy and may require antihypertensive therapy [see Adverse Reactions (6.1)] . The control of blood pressure can be accomplished with any of the common antihypertensive agents, though careful consideration should be given prior to use of antihypertensive agents associated with hyperkalemia (e.g., potassium-sparing diuretics, ACE inhibitors, angiotensin receptor blockers) [see Warnings and Precautions (5.7)] . Calcium-channel blocking agents may increase tacrolimus blood concentrations and therefore require dosage reduction of tacrolimus [see Drug Interactions (7.2)].
5.9 Anaphylactic Reactions with Tacrolimus Injection
Anaphylactic reactions have occurred with injectables containing castor oil derivatives, including tacrolimus, in a small percentage of patients (0.6%). The exact cause of these reactions is not known. Tacrolimus injection should be reserved for patients who are unable to take tacrolimus orally. Monitor patients for anaphylaxis when using the intravenous route of administration [see Dosage and Administration (2.1)].
5.10 Not Recommended for Use with Sirolimus
Tacrolimus is not recommended for use with sirolimus:
- The use of sirolimus with tacrolimus in studies of de novoliver transplant patients was associated with an excess mortality, graft loss, and hepatic artery thrombosis (HAT), and is not recommended.
- The use of sirolimus (2 mg per day) with tacrolimus in heart transplant patients in a U.S. trial was associated with increased risk of renal function impairment, wound healing complications, and insulin-dependent post-transplant diabetes mellitus, and is not recommended [see Clinical Studies (14.3)] .
- The use of sirolimus with tacrolimus may increase the risk of thrombotic microangiopathy [see Warnings and Precautions (5.16)].
5.11 Interactions with CYP3A4 Inhibitors and Inducers
When co-administering tacrolimus with strong CYP3A4 inhibitors (e.g., telaprevir, boceprevir, ritonavir, ketoconazole, itraconazole, voriconazole, clarithromycin) and strong inducers (e.g., rifampin, rifabutin), adjustments in the dosing regimen of tacrolimus and subsequent frequent monitoring of tacrolimus whole blood trough concentrations and tacrolimus-associated adverse reactions are recommended. A rapid, sharp rise in tacrolimus levels has been reported after co-administration with a strong CYP3A4 inhibitor, clarithromycin, despite an initial reduction of tacrolimus dose. Early and frequent monitoring of tacrolimus whole blood trough levels is recommended [see Drug Interactions (7.2)].
5.12 QT Prolongation
Tacrolimus may prolong the QT/QTc interval and may cause Torsades de pointes. Avoid tacrolimus in patients with congenital long QT syndrome. In patients with congestive heart failure, bradyarrhythmias, those taking certain antiarrhythmic medications or other medicinal products that lead to QT prolongation, and those with electrolyte disturbances such as hypokalemia, hypocalcemia, or hypomagnesemia, consider obtaining electrocardiograms and monitoring electrolytes (magnesium, potassium, calcium) periodically during treatment.
When co-administering tacrolimus with other substrates and/or inhibitors of CYP3A4 that also have the potential to prolong the QT interval, a reduction in tacrolimus dose, frequent monitoring of tacrolimus whole blood concentrations, and monitoring for QT prolongation is recommended. Use of tacrolimus with amiodarone has been reported to result in increased tacrolimus whole blood concentrations with or without concurrent QT prolongation [see Drug Interactions (7.2)] .
5.13 Myocardial Hypertrophy
Myocardial hypertrophy has been reported in infants, children, and adults, particularly those with high tacrolimus trough concentrations, and is generally manifested by echocardiographically demonstrated concentric increases in left ventricular posterior wall and interventricular septum thickness. This condition appears reversible in most cases following dose reduction or discontinuance of therapy. In patients who develop renal failure or clinical manifestations of ventricular dysfunction while receiving tacrolimus therapy, echocardiographic evaluation should be considered. If myocardial hypertrophy is diagnosed, dosage reduction or discontinuation of tacrolimus should be considered [see Adverse Reactions (6.2)] .
5.14 Immunizations
Whenever possible, administer the complete complement of vaccines before transplantation and treatment with tacrolimus.
The use of live vaccines should be avoided during treatment with tacrolimus; examples include (not limited to) the following: intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines.
Inactivated vaccines noted to be safe for administration after transplantation may not be sufficiently immunogenic during treatment with tacrolimus.
5.15 Pure Red Cell Aplasia
Cases of pure red cell aplasia (PRCA) have been reported in patients treated with tacrolimus. A mechanism for tacrolimus-induced PRCA has not been elucidated. All patients reported risk factors for PRCA such as parvovirus B19 infection, underlying disease, or concomitant medications associated with PRCA. If PRCA is diagnosed, discontinuation of tacrolimus should be considered [see Adverse Reactions (6.2)] .
5.16 Thrombotic Microangiopathy (Including Hemolytic Uremic Syndrome and
Thrombotic Thrombocytopenic Purpura)
Cases of thrombotic microangiopathy (TMA), including hemolytic uremic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP), have been reported in patients treated with tacrolimus. TMA may have a multifactorial etiology. Risk factors for TMA that can occur in transplant patients include, for example, severe infections, graft-versus-host disease (GVHD), Human Leukocyte Antigen (HLA) mismatch, the use of calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors. These risk factors may, either alone or combined, contribute to the risk of TMA.
In patients with signs and symptoms of TMA, consider tacrolimus as a risk factor. Concurrent use of tacrolimus and mTOR inhibitors may contribute to the risk of TMA.
5.17 Cannabidiol Drug Interactions
When cannabidiol and tacrolimus are co-administered, closely monitor for an increase in tacrolimus blood levels and for adverse reactions suggestive of tacrolimus toxicity. A dose reduction of tacrolimus should be considered as needed when tacrolimus is co-administered with cannabidiol [see Dosage and Administration (2.2, 2.6)and Drug Interactions (7.3)] .
- Not Interchangeable with Extended-Release Tacrolimus Products- Medication Errors. Instruct patients or caregivers to recognize the appearance of tacrolimus capsules. ( 5.3)
- New Onset Diabetes After Transplant: Monitor blood glucose. ( 5.4)
- Nephrotoxicity (acute and/or chronic): Reduce the dose; use caution with other nephrotoxic drugs. ( 5.5)
- Neurotoxicity: Including risk of Posterior Reversible Encephalopathy Syndrome (PRES), monitor for neurologic abnormalities; reduce or discontinue tacrolimus. ( 5.6)
- Hyperkalemia: Monitor serum potassium levels. Consider carefully before using with other agents also associated with hyperkalemia. ( 5.7)
- Hypertension: May require antihypertensive therapy. Monitor relevant drug-drug interactions. ( 5.8)
- Anaphylactic Reactions with IV formulation: Observe patients receiving tacrolimus injection for signs and symptoms of anaphylaxis. ( 5.9)
- Not recommended for use with sirolimus: Not recommended in liver and heart transplant due to increased risk of serious adverse reactions. ( 5.10)
- Myocardial Hypertrophy: Consider dose reduction/discontinuation. ( 5.13)
- Immunizations: Avoid live vaccines. ( 5.14)
- Pure Red Cell Aplasia: Consider discontinuation of tacrolimus. ( 5.15)
- Thrombotic Microangiopathy, Including Hemolytic Uremic Syndrome and Thrombotic Thrombocytopenic Purpura: May occur, especially in patients with infections and certain concomitant medications. ( 5.16)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following serious and otherwise important adverse drug reactions are discussed in greater detail in other sections of labeling:
- Lymphoma and Other Malignancies [see Warnings and Precautions (5.1)]
- Serious Infections [see Warnings and Precautions (5.2)]
- New Onset Diabetes After Transplant [see Warnings and Precautions (5.4)]
- Nephrotoxicity [see Warnings and Precautions (5.5)]
- Neurotoxicity [see Warnings and Precautions (5.6)]
- Hyperkalemia [see Warnings and Precautions (5.7)]
- Hypertension [see Warnings and Precautions (5.8)]
- Anaphylactic Reactions with Tacrolimus Injection [see Warnings and Precautions (5.9)]
- Myocardial Hypertrophy [see Warnings and Precautions (5.13)]
- Pure Red Cell Aplasia [see Warnings and Precautions (5.15)]
- Thrombotic Microangiopathy, Including Hemolytic Uremic Syndrome and Thrombotic Thrombocytopenic Purpura [see Warnings and Precautions (5.16)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. In addition, the clinical trials were not designed to establish comparative differences across study arms with regards to the adverse reactions discussed below.
Kidney Transplantation
The incidence of adverse reactions was determined in three randomized kidney transplant trials. One of the trials used azathioprine (AZA) and corticosteroids and two of the trials used mycophenolate mofetil (MMF) and corticosteroids concomitantly for maintenance immunosuppression.
Tacrolimus-based immunosuppression in conjunction with azathioprine and corticosteroids following kidney transplantation was assessed in a trial where 205 patients received tacrolimus-based immunosuppression and 207 patients received cyclosporine-based immunosuppression. The trial population had a mean age of 43 years (mean ± SD was 43 ± 13 years on tacrolimus and 44 ± 12 years on cyclosporine arm), the distribution was 61% male, and the composition was White (58%), African-American (25%), Hispanic (12%), and Other (5%). The 12-month post-transplant information from this trial is presented below.
The most common adverse reactions (≥ 30%) observed in tacrolimus-treated kidney transplant patients are: infection, tremor, hypertension, abnormal renal function, constipation, diarrhea, headache, abdominal pain, insomnia, nausea, hypomagnesemia, urinary tract infection, hypophosphatemia, peripheral edema, asthenia, pain, hyperlipidemia, hyperkalemia, and anemia. Based on reported adverse reaction terms related to decreased renal function, nephrotoxicity was reported in approximately 52% of kidney transplantation patients.
Adverse reactions that occurred in ≥ 15% of kidney transplant patients treated with tacrolimus in conjunction with azathioprine are presented below:
Table 4. Kidney Transplantation: Adverse Reactions Occurring in ≥ 15% of Patients Treated with Tacrolimus in Conjunction with Azathioprine (AZA)|
Tacrolimus / AZA ** (N = 205)** |
Cyclosporine / AZA ** (N = 207)** | |
|
Nervous System | ||
|
Tremor |
54% |
34% |
|
Headache |
44% |
38% |
|
Insomnia |
32% |
30% |
|
Paresthesia |
23% |
16% |
|
Dizziness |
19% |
16% |
|
Gastrointestinal | ||
|
Diarrhea |
44% |
41% |
|
Nausea |
38% |
36% |
|
Constipation |
35% |
43% |
|
Vomiting |
29% |
23% |
|
Dyspepsia |
28% |
20% |
|
Cardiovascular | ||
|
Hypertension |
50% |
52% |
|
Chest Pain |
19% |
13% |
|
Urogenital | ||
|
Creatinine Increased |
45% |
42% |
|
Urinary Tract Infection |
34% |
35% |
|
Metabolic and Nutritional | ||
|
Hypophosphatemia |
49% |
53% |
|
Hypomagnesemia |
34% |
17% |
|
Hyperlipemia |
31% |
38% |
|
Hyperkalemia |
31% |
32% |
|
Diabetes Mellitus |
24% |
9% |
|
Hypokalemia |
22% |
25% |
|
Hyperglycemia |
22% |
16% |
|
Edema |
18% |
19% |
|
Hemic and Lymphatic | ||
|
Anemia |
30% |
24% |
|
Leukopenia |
15% |
17% |
|
Miscellaneous | ||
|
Infection |
45% |
49% |
|
Peripheral Edema |
36% |
48% |
|
Asthenia |
34% |
30% |
|
Abdominal Pain |
33% |
31% |
|
Pain |
32% |
30% |
|
Fever |
29% |
29% |
|
Back Pain |
24% |
20% |
|
Respiratory System | ||
|
Dyspnea |
22% |
18% |
|
Cough Increased |
18% |
15% |
|
Musculoskeletal | ||
|
Arthralgia |
25% |
24% |
|
Skin | ||
|
Rash |
17% |
12% |
|
Pruritus |
15% |
7% |
Two trials were conducted for tacrolimus-based immunosuppression in conjunction with MMF and corticosteroids. In the non-US trial (Study 1), the incidence of adverse reactions was based on 1195 kidney transplant patients that received tacrolimus (Group C, n = 403), or one of two cyclosporine (CsA) regimens (Group A, n = 384 and Group B, n = 408) in combination with MMF and corticosteroids; all patients, except those in one of the two cyclosporine groups, also received induction with daclizumab. The trial population had a mean age of 46 years (range 17 to 76); the distribution was 65% male, and the composition was 93% Caucasian. The 12-month post-transplant information from this trial is presented below.
Adverse reactions that occurred in ≥ 10% of kidney transplant patients treated with tacrolimus in conjunction with MMF in Study 1 [Note: This trial was conducted entirely outside of the United States. Such trials often report a lower incidence of adverse reactions in comparison to U.S. trials] are presented below:
Table 5. Kidney Transplantation: Adverse Reactions Occurring in ≥ 10% of Patients Treated with Tacrolimus in Conjunction with MMF (Study 1)|
Tacrolimus (Group C) |
Cyclosporine ** (Group A)** |
Cyclosporine ** (Group B)** | |
|
(N = 403) |
(N = 384) |
(N = 408) | |
|
Diarrhea |
25% |
16% |
13% |
|
Urinary Tract Infection |
24% |
28% |
24% |
|
Anemia |
17% |
19% |
17% |
|
Hypertension |
13% |
14% |
12% |
|
Leukopenia |
13% |
10% |
10% |
|
Edema Peripheral |
11% |
12% |
13% |
|
Hyperlipidemia |
10% |
15% |
13% |
|
Key: Group A = CsA/MMF/CS, B = CsA/MMF/CS/Daclizumab, C = Tac/MMF/CS/Daclizumab CsA = Cyclosporine, CS = Corticosteroids, Tac = Tacrolimus, MMF = mycophenolate mofetil |
In the U.S. trial (Study 2) with tacrolimus-based immunosuppression in conjunction with MMF and corticosteroids, 424 kidney transplant patients received tacrolimus (n = 212) or cyclosporine (n = 212) in combination with MMF 1 gram twice daily, basiliximab induction, and corticosteroids. The trial population had a mean age of 48 years (range 17 to 77); the distribution was 63% male, and the composition was White (74%), African-American (20%), Asian (3%), and Other (3%). The 12-month post-transplant information from this trial is presented below.
Adverse reactions that occurred in ≥ 15% of kidney transplant patients treated with tacrolimus in conjunction with MMF in Study 2 are presented below:
Table 6. Kidney Transplantation: Adverse Reactions Occurring in ≥ 15% of Patients Treated with Tacrolimus in Conjunction with MMF (Study 2)|
Tacrolimus/MMF ** (N = 212)** |
Cyclosporine/MMF ** (N = 212)** | |
|
Gastrointestinal Disorders | ||
|
Diarrhea |
44% |
26% |
|
Nausea |
39% |
47% |
|
Constipation |
36% |
41% |
|
Vomiting |
26% |
25% |
|
Dyspepsia |
18% |
15% |
|
Injury, Poisoning, and Procedural Complications | ||
|
Post-Procedural Pain |
29% |
27% |
|
Incision Site Complication |
28% |
23% |
|
Graft Dysfunction |
24% |
18% |
|
Metabolism and Nutrition Disorders | ||
|
Hypomagnesemia |
28% |
22% |
|
Hypophosphatemia |
28% |
21% |
|
Hyperkalemia |
26% |
19% |
|
Hyperglycemia |
21% |
15% |
|
Hyperlipidemia |
18% |
25% |
|
Hypokalemia |
16% |
18% |
|
Nervous System Disorders | ||
|
Tremor |
34% |
20% |
|
Headache |
24% |
25% |
|
Blood and Lymphatic System Disorders | ||
|
Anemia |
30% |
28% |
|
Leukopenia |
16% |
12% |
|
Miscellaneous | ||
|
Edema Peripheral |
35% |
46% |
|
Hypertension |
32% |
35% |
|
Insomnia |
30% |
21% |
|
Urinary Tract Infection |
26% |
22% |
|
Blood Creatinine Increased |
23% |
23% |
Less frequently observed adverse reactions in kidney transplantation patients are described under the subsection “Less Frequently Reported Adverse Reactions (> 3% and < 15%) in Liver, Kidney, and Heart Transplant Studies.”
Liver Transplantation
There were two randomized comparative liver transplant trials. In the U.S. trial, 263 adult and pediatric patients received tacrolimus and steroids and 266 patients received cyclosporine-based immunosuppressive regimen (CsA/AZA). The trial population had a mean age of 44 years (range 0.4 to 70); the distribution was 52% male, and the composition was White (78%), African- American (5%), Asian (2%), Hispanic (13%), and Other (2%). In the European trial, 270 patients received tacrolimus and steroids and 275 patients received CsA/AZA. The trial population had a mean age of 46 years (range 15 to 68); the distribution was 59% male, and the composition was White (95.4%), Black (1%), Asian (2%), and Other (2%).
The proportion of patients reporting more than one adverse event was > 99% in both the tacrolimus group and the CsA/AZA group. Precautions must be taken when comparing the incidence of adverse reactions in the U.S. trial to that in the European trial. The 12-month post-transplant information from the U.S. trial and from the European trial is presented below. The two trials also included different patient populations and patients were treated with immunosuppressive regimens of differing intensities. Adverse reactions reported in ≥ 15% in tacrolimus patients (combined trial results) are presented below for the two controlled trials in liver transplantation.
The most common adverse reactions (≥ 40%) observed in tacrolimus-treated liver transplant patients are: tremor, headache, diarrhea, hypertension, nausea, abnormal renal function, abdominal pain, insomnia, paresthesia, anemia, pain, fever, asthenia, hyperkalemia, hypomagnesemia, and hyperglycemia. These all occur with oral and IV administration of tacrolimus and some may respond to a reduction in dosing (e.g., tremor, headache, paresthesia, hypertension). Diarrhea was sometimes associated with other gastrointestinal complaints such as nausea and vomiting. Based on reported adverse reaction terms related to decreased renal function, nephrotoxicity was reported in approximately 40% and 36% of liver transplantation patients receiving tacrolimus in the U.S. and European randomized trials.
Table 7. Liver Transplantation: Adverse Reactions Occurring in ≥ 15% of Patients Treated with Tacrolimus|
U.S. TRIAL |
EUROPEAN TRIAL | |||
|
Tacrolimus**** |
Cyclosporine/AZA |
Tacrolimus (N = 264) |
Cyclosporine/AZA | |
|
Nervous System | ||||
|
Headache |
64% |
60% |
37% |
26% |
|
Insomnia |
64% |
68% |
32% |
23% |
|
Tremor |
56% |
46% |
48% |
32% |
|
Paresthesia |
40% |
30% |
17% |
17% |
|
Gastrointestinal | ||||
|
Diarrhea |
72% |
47% |
37% |
27% |
|
Nausea |
46% |
37% |
32% |
27% |
|
LFT Abnormal |
36% |
30% |
6% |
5% |
|
Anorexia |
34% |
24% |
7% |
5% |
|
Vomiting |
27% |
15% |
14% |
11% |
|
Constipation |
24% |
27% |
23% |
21% |
|
Cardiovascular | ||||
|
Hypertension |
47% |
56% |
38% |
43% |
|
Urogenital | ||||
|
Kidney Function Abnormal |
40% |
27% |
36% |
23% |
|
Creatinine Increased |
39% |
25% |
24% |
19% |
|
BUN Increased |
30% |
22% |
12% |
9% |
|
Oliguria |
18% |
15% |
19% |
12% |
|
Urinary Tract Infection |
16% |
18% |
21% |
19% |
|
Metabolic and Nutritional | ||||
|
Hypomagnesemia |
48% |
45% |
16% |
9% |
|
Hyperglycemia |
47% |
38% |
33% |
22% |
|
Hyperkalemia |
45% |
26% |
13% |
9% |
|
Hypokalemia |
29% |
34% |
13% |
16% |
|
Hemic and Lymphatic | ||||
|
Anemia |
47% |
38% |
5% |
1% |
|
Leukocytosis |
32% |
26% |
8% |
8% |
|
Thrombocytopenia |
24% |
20% |
14% |
19% |
|
Miscellaneous | ||||
|
Pain |
63% |
57% |
24% |
22% |
|
Abdominal Pain |
59% |
54% |
29% |
22% |
|
Asthenia |
52% |
48% |
11% |
7% |
|
Fever |
48% |
56% |
19% |
22% |
|
Back Pain |
30% |
29% |
17% |
17% |
|
Ascites |
27% |
22% |
7% |
8% |
|
Peripheral Edema |
26% |
26% |
12% |
14% |
|
Respiratory System | ||||
|
Pleural Effusion |
30% |
32% |
36% |
35% |
|
Dyspnea |
29% |
23% |
5% |
4% |
|
Atelectasis |
28% |
30% |
5% |
4% |
|
Skin and Appendages | ||||
|
Pruritus |
36% |
20% |
15% |
7% |
|
Rash |
24% |
19% |
10% |
4% |
Less frequently observed adverse reactions in liver transplantation patients are described under the subsection “Less Frequently Reported Adverse Reactions (> 3% and < 15%) in Liver, Kidney, and Heart Transplant Studies.”
Heart Transplantation
The incidence of adverse reactions was determined based on two trials in primary orthotopic heart transplantation. In a trial conducted in Europe, 314 patients received a regimen of antibody induction, corticosteroids, and azathioprine (AZA) in combination with tacrolimus (n = 157) or cyclosporine (n = 157) for 18 months. The trial population had a mean age of 51 years (range 18 to 65); the distribution was 82% male, and the composition was White (96%), Black (3%), and Other (1%).
The most common adverse reactions (≥ 15%) observed in tacrolimus-treated heart transplant patients are: abnormal renal function, hypertension, diabetes mellitus, CMV infection, tremor, hyperglycemia, leukopenia, infection, anemia, bronchitis, pericardial effusion, urinary tract infection, and hyperlipemia. Based on reported adverse reaction terms related to decreased renal function, nephrotoxicity was reported in approximately 59% of heart transplantation patients in the European trial.
Adverse reactions in heart transplant patients in the European trial are presented below:
Table 9. Heart Transplantation: Adverse Reactions Occurring in ≥ 15% of Patients Treated with Tacrolimus in Conjunction with Azathioprine (AZA)|
Tacrolimus/AZA |
Cyclosporine/AZA | |
|
Cardiovascular System | ||
|
Hypertension |
62% |
69% |
|
Pericardial Effusion |
15% |
14% |
|
Body as a Whole | ||
|
CMV Infection |
32% |
30% |
|
Infection |
24% |
21% |
|
Metabolic and Nutritional Disorders | ||
|
Diabetes Mellitus |
26% |
16% |
|
Hyperglycemia |
23% |
17% |
|
Hyperlipemia |
18% |
27% |
|
Hemic and Lymphatic System | ||
|
Anemia |
50% |
36% |
|
Leukopenia |
48% |
39% |
|
Urogenital System | ||
|
Kidney Function Abnormal |
56% |
57% |
|
Urinary Tract Infection |
16% |
12% |
|
Respiratory System | ||
|
Bronchitis |
17% |
18% |
|
Nervous System | ||
|
Tremor |
15% |
6% |
In the European trial, the cyclosporine trough concentrations were above the pre-defined target range (i.e., 100 to 200 ng/mL) at Day 122 and beyond in 32% to 68% of the patients in the cyclosporine treatment arm, whereas the tacrolimus trough concentrations were within the pre-defined target range (i.e., 5 to 15 ng/mL) in 74% to 86% of the patients in the tacrolimus treatment arm.
In a U.S. trial, the incidence of adverse reactions was based on 331 heart transplant patients that received corticosteroids and tacrolimus in combination with sirolimus (n = 109), tacrolimus in combination with MMF (n = 107) or cyclosporine modified in combination with MMF (n = 115) for 1 year. The trial population had a mean age of 53 years (range 18 to 75); the distribution was 78% male, and the composition was White (83%), African- American (13%) and Other (4%).
Only selected targeted treatment-emergent adverse reactions were collected in the U.S. heart transplantation trial. Those reactions that were reported at a rate of 15% or greater in patients treated with tacrolimus and MMF include the following: any target adverse reactions (99%), hypertension (89%), hyperglycemia requiring antihyperglycemic therapy (70%) ,hypertriglyceridemia (65%), anemia (hemoglobin < 10.0 g/dL) (65%), fasting blood glucose > 140 mg/dL (on two separate occasions) (61%), hypercholesterolemia (57%), hyperlipidemia (34%), WBCs < 3000 cells/mcL (34%), serious bacterial infections (30%), magnesium < 1.2 mEq/L (24%), platelet count < 75,000 cells/mcL (19%), and other opportunistic infections (15%).
Other targeted treatment-emergent adverse reactions in tacrolimus-treated patients occurred at a rate of less than 15%, and include the following: Cushingoid features, impaired wound healing, hyperkalemia, Candidainfection, and CMV infection/syndrome. Other less frequently observed adverse reactions in heart transplantation patients are described under the subsection “Less Frequently Reported Adverse Reactions (> 3% and < 15%) in Liver, Kidney and Heart Transplant Studies.”
New Onset Diabetes After Transplant
Kidney Transplantation
New Onset Diabetes After Transplant (NODAT) is defined as a composite of fasting plasma glucose ≥ 126 mg/dL, HbA 1C≥ 6%, insulin use ≥ 30 days, or oral hypoglycemic use. In a trial in kidney transplant patients (Study 2), NODAT was observed in 75% in the tacrolimus-treated and 61% in the NEORAL-treated patients without pre-transplant history of diabetes mellitus (Table 10) [see Clinical Studies (14.1)] .
Table 10. Incidence of New Onset Diabetes After Transplant at 1 year in Kidney Transplant Recipients in a Phase 3 Trial (Study 2)|
Parameter |
Treatment Group | |
|
Tacrolimus/MMF |
NEORAL/MMF | |
|
NODAT |
112/150 (75%) |
93/152 (61%) |
|
Fasting Plasma Glucose ≥ 126 mg/dL |
96/150 (64%) |
80/152 (53%) |
|
HbA 1c≥ 6% |
59/150 (39%) |
28/152 (18%) |
|
Insulin Use ≥ 30 days |
9/150 (6%) |
4/152 (3%) |
|
Oral Hypoglycemic Use |
15/150 (10%) |
5/152 (3%) |
In early trials of tacrolimus, Post-Transplant Diabetes Mellitus (PTDM) was evaluated with a more limited criterion of “use of insulin for 30 or more consecutive days with < 5-day gap” in patients without a prior history of insulin-dependent diabetes mellitus or non-insulin dependent diabetes mellitus. Data are presented in Tables 11 to 14. PTDM was reported in 20% of tacrolimus/Azathioprine (AZA)-treated kidney transplant patients without pre- transplant history of diabetes mellitus in a Phase 3 trial (Table 11). The median time to onset of PTDM was 68 days. Insulin dependence was reversible in 15% of these PTDM patients at one year and in 50% at 2 years post-transplant. African-American and Hispanic kidney transplant patients were at an increased risk of development of PTDM (Table 12).
Table 11. Incidence of Post-Transplant Diabetes Mellitus and Insulin Use at 2 Years in Kidney Transplant Recipients in a Phase 3 Trial using Azathioprine (AZA)
| ||
|
Status of PTDM****1 |
Tacrolimus/AZA |
CsA/AZA |
|
Patients without pre-transplant history of diabetes mellitus |
151 |
151 |
|
New onset PTDM 1, 1 stYear |
30/151 (20%) |
6/151 (4%) |
|
Still insulin-dependent at one year in those without prior history of diabetes |
25/151 (17%) |
5/151 (3%) |
|
New onset PTDM 1post 1 year |
1 |
0 |
|
Patients with PTDM 1at 2 years |
16/151 (11%) |
5/151 (3%) |
| ||
|
Patient Race |
Patients Who Developed PTDM****1 | |
|
Tacrolimus |
Cyclosporine | |
|
African-American |
15/41 (37%) |
3 (8%) |
|
Hispanic |
5/17 (29%) |
1 (6%) |
|
Caucasian |
10/82 (12%) |
1 (1%) |
|
Other |
0/11 (0%) |
1 (10%) |
|
Total |
30/151 (20%) |
6 (4%) |
Liver Transplantation
Insulin-dependent PTDM was reported in 18% and 11% of tacrolimus-treated liver transplant patients and was reversible in 45% and 31% of these patients at 1 year post-transplant, in the U.S. and European randomized trials, respectively (Table 13). Hyperglycemia was associated with the use of tacrolimus in 47% and 33% of liver transplant recipients in the U.S. and European randomized trials, respectively, and may require treatment [see Adverse Reactions (6.1)].
Table 13. Incidence of Post-Transplant Diabetes Mellitus and Insulin Use at 1 Year in Liver Transplant Recipients
| ||||
|
Status of PTDM****1 |
US Trial |
European Trial | ||
|
Tacrolimus |
Cyclosporine |
Tacrolimus |
Cyclosporine | |
|
Patients at risk 2 |
239 |
236 |
239 |
249 |
|
New Onset PTDM 1 |
42 (18%) |
30 (13%) |
26 (11%) |
12 (5%) |
|
Patients still on insulin at 1 year |
23 (10%) |
19 (8%) |
18 (8%) |
6 (2%) |
Heart Transplantation
Insulin-dependent PTDM was reported in 13% and 22% of tacrolimus-treated heart transplant patients receiving mycophenolate mofetil (MMF) or azathioprine (AZA) and was reversible in 30% and 17% of these patients at one year post- transplant, in the U.S. and European randomized trials, respectively (Table 14). Hyperglycemia, defined as two fasting plasma glucose levels ≥ 126 mg/dL was reported with the use of tacrolimus plus MMF or AZA in 32% and 35% of heart transplant recipients in the U.S. and European randomized trials, respectively, and may require treatment [see Adverse Reactions (6.1)].
Table 14. Incidence of Post-Transplant Diabetes Mellitus and Insulin Use at 1 Year in Heart Transplant Recipients
| ||||
|
Status of PTDM****1 |
US Trial |
European Trial | ||
|
Tacrolimus/ |
Cyclosporine/ |
Tacrolimus/ |
Cyclosporine/ | |
|
Patients at risk 2 |
75 |
83 |
132 |
138 |
|
New Onset PTDM 1 |
10 (13%) |
6 (7%) |
29 (22%) |
5 (4%) |
|
Patients still on insulin at 1 year 3 |
7 (9%) |
1 (1%) |
24 (18%) |
4 (3%) |
Less Frequently Reported Adverse Reactions (> 3% and < 15%) in Liver, Kidney,
and Heart Transplant Studies:
The following adverse reactions were reported in either liver, kidney, and/or
heart transplant recipients who were treated with tacrolimus in clinical
trials.
- Nervous System: Abnormal dreams, agitation, amnesia, anxiety, confusion, convulsion, crying, depression, elevated mood, emotional lability, encephalopathy, hemorrhagic stroke, hallucinations, hypertonia, incoordination, monoparesis, myoclonus, nerve compression, nervousness, neuralgia, neuropathy, paralysis flaccid, psychomotor skills impaired, psychosis, quadriparesis, somnolence, thinking abnormal, vertigo, writing impaired
- Special Senses: Abnormal vision, amblyopia, ear pain, otitis media, tinnitus
- Gastrointestinal: Cholangitis, cholestatic jaundice, duodenitis, dysphagia, esophagitis, flatulence, gastritis, gastroesophagitis, gastrointestinal hemorrhage, GGT increase, GI disorder, GI perforation, hepatitis, hepatitis granulomatous, ileus, increased appetite, jaundice, liver damage, esophagitis ulcerative, oral moniliasis, pancreatic pseudocyst, stomatitis
- Cardiovascular: Abnormal ECG, angina pectoris, arrhythmia, atrial fibrillation, atrial flutter, bradycardia, cardiac fibrillation, cardiopulmonary failure, congestive heart failure, deep thrombophlebitis, echocardiogram abnormal, electrocardiogram QRS complex abnormal, electrocardiogram ST segment abnormal, heart failure, heart rate decreased, hemorrhage, hypotension, phlebitis, postural hypotension, syncope, tachycardia, thrombosis, vasodilatation
- Urogenital: Acute kidney failure, albuminuria, BK nephropathy, bladder spasm, cystitis, dysuria, hematuria, hydronephrosis, kidney failure, kidney tubular necrosis, nocturia, pyuria, toxic nephropathy, urge incontinence, urinary frequency, urinary incontinence, urinary retention, vaginitis
- Metabolic/Nutritional: Acidosis, alkaline phosphatase increased, alkalosis, ALT (SGPT) increased, AST (SGOT) increased, bicarbonate decreased, bilirubinemia, dehydration, GGT increased, gout, healing abnormal, hypercalcemia, hypercholesterolemia, hyperphosphatemia, hyperuricemia, hypervolemia, hypocalcemia, hypoglycemia, hyponatremia, hypoproteinemia, lactic dehydrogenase increased, weight gain
- Endocrine: Cushing’s syndrome
- Hemic/Lymphatic: Coagulation disorder, ecchymosis, hematocrit increased, hypochromic anemia, leukocytosis, polycythemia, prothrombin decreased, serum iron decreased
- Miscellaneous: Abdomen enlarged, abscess, accidental injury, allergic reaction, cellulitis, chills, fall, flu syndrome, generalized edema, hernia, mobility decreased, peritonitis, photosensitivity reaction, sepsis, temperature intolerance, ulcer
- Musculoskeletal: Arthralgia, cramps, generalized spasm, leg cramps, myalgia, myasthenia, osteoporosis
- Respiratory: Asthma, emphysema, hiccups, lung function decreased, pharyngitis, pneumonia, pneumothorax, pulmonary edema, rhinitis, sinusitis, voice alteration
- Skin: Acne, alopecia, exfoliative dermatitis, fungal dermatitis, herpes simplex, herpes zoster, hirsutism, neoplasm skin benign, skin discoloration, skin ulcer, sweating
Additional pediatric use information is approved for Astellas Pharma US, Inc.’s Prograf (tacrolimus) products. However, due to Astellas Pharma US, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
6.2 Postmarketing Experience
The following adverse reactions have been reported from worldwide marketing experience with tacrolimus. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of the reporting, or (3) strength of causal connection to the drug.
Other reactions include:
- Cardiovascular: Atrial fibrillation, atrial flutter, cardiac arrhythmia, cardiac arrest, electrocardiogram T wave abnormal, flushing, myocardial infarction, myocardial ischemia, pericardial effusion, QT prolongation, Torsades de pointes, venous thrombosis deep limb, ventricular extrasystoles, ventricular fibrillation, myocardial hypertrophy
- Gastrointestinal: Bile duct stenosis, colitis, enterocolitis, gastroenteritis, gastroesophageal reflux disease, hepatic cytolysis, hepatic necrosis, hepatotoxicity, impaired gastric emptying, liver fatty, mouth ulceration, pancreatitis hemorrhagic, pancreatitis necrotizing, stomach ulcer, veno-occlusive liver disease
- Hemic/Lymphatic: Agranulocytosis, disseminated intravascular coagulation, hemolytic anemia, neutropenia, febrile neutropenia, pancytopenia, thrombocytopenic purpura, thrombotic thrombocytopenic purpura, pure red cell aplasia, thrombotic microangiopathy
- Infections: Cases of progressive multifocal leukoencephalopathy (PML), sometimes fatal; polyoma virus-associated nephropathy, (PVAN) including graft loss
- Metabolic/Nutritional: Glycosuria, increased amylase including pancreatitis, weight decreased
- Miscellaneous: Feeling hot and cold, feeling jittery, hot flushes, multi-organ failure, primary graft dysfunction
- Musculoskeletal and Connective Tissue Disorders: Pain in extremity including Calcineurin-Inhibitor Induced Pain Syndrome (CIPS)
- Nervous System: Carpal tunnel syndrome, cerebral infarction, hemiparesis, leukoencephalopathy, mental disorder, mutism, posterior reversible encephalopathy syndrome (PRES), progressive multifocal leukoencephalopathy (PML), quadriplegia, speech disorder, syncope
- Respiratory: Acute respiratory distress syndrome, interstitial lung disease, lung infiltration, respiratory distress, respiratory failure
- Skin: Stevens-Johnson syndrome, toxic epidermal necrolysis
- Special Senses: Blindness, optic neuropathy, blindness cortical, hearing loss including deafness, photophobia
- Urogenital: Acute renal failure, cystitis hemorrhagic, hemolytic-uremic syndrome
The most common adverse reactions (≥ 15%) were abnormal renal function, hypertension, diabetes mellitus, fever, CMV infection, tremor, hyperglycemia, leukopenia, infection, anemia, bronchitis, pericardial effusion, urinary tract infection, constipation, diarrhea, headache, abdominal pain, insomnia, paresthesia, peripheral edema, nausea, hyperkalemia, hypomagnesemia, and hyperlipemia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Accord Healthcare Inc. at 1-866-941-7875 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 Mycophenolic Acid
When tacrolimus capsules are prescribed with a given dose of a mycophenolic acid (MPA) product, exposure to MPA is higher with tacrolimus co- administration than with cyclosporine co-administration with MPA, because cyclosporine interrupts the enterohepatic recirculation of MPA while tacrolimus does not. Monitor for MPA-associated adverse reactions and reduce the dose of concomitantly administered mycophenolic acid products as needed.
7.2 Effects of Other Drugs on Tacrolimus
Table 15 displays the effects of other drugs on tacrolimus.
Table 15. Effects of Other Drugs/Substances on Tacrolimus****1
| ||
|
Drug/Substance Class or Name |
Drug Interaction Effect |
Recommendations |
|
Grapefruit or grapefruit juice 2 |
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.6, 5.11, 5.12)] . |
Avoid grapefruit or grapefruit juice. |
|
Strong CYP3A Inducers 3: Antimycobacterials (e.g., rifampin, rifabutin), anticonvulsants (e.g., phenytoin, carbamazepine and phenobarbital), St John’s wort |
May decrease tacrolimus whole blood trough concentrations and increase the risk of rejection [see Warnings and Precautions (5.11)] . |
Increase tacrolimus dose and monitor tacrolimus whole blood trough concentrations [see Dosage and Administration (2.2, 2.6)and Clinical Pharmacology (12.3)] . |
|
Strong CYP3A Inhibitors 3: Protease inhibitors (e.g., nelfinavir, telaprevir, boceprevir, ritonavir), azole antifungals (e.g., voriconazole, posaconazole, itraconazole, ketoconazole), antibiotics (e.g., clarithromycin, troleandomycin, chloramphenicol), nefazodone, letermovir, Schisandra sphenantheraextracts |
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation). A rapid, sharp rise in tacrolimus levels may occur early, despite an immediate reduction of tacrolimus dose [see Warnings and Precautions (5.6, 5.11, 5.12)] . |
Reduce tacrolimus dose (for voriconazole and posaconazole, give one-third of the original dose) and adjust dose based on tacrolimus whole blood trough concentrations [see Dosage and Administration (2.2, 2.6)and Clinical Pharmacology (12.3)] . Early and frequent monitoring of tacrolimus whole blood trough levels should start within 1 to 3 days and continue monitoring as necessary [see Warnings and Precautions (5.11)] . |
|
Mild or Moderate CYP3A Inhibitors: Clotrimazole, antibiotics (e.g., erythromycin, fluconazole), calcium channel blockers (e.g., verapamil, diltiazem, nifedipine, nicardipine), amiodarone, danazol, ethinyl estradiol, cimetidine, lansoprazole and omeprazole |
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.6, 5.11, 5.12)] . |
Monitor tacrolimus whole blood trough concentrations and reduce tacrolimus dose if needed [see Dosage and Administration (2.2, 2.6)and Clinical Pharmacology (12.3)] . |
|
Other drugs, such as: Magnesium and aluminum hydroxide antacids Metoclopramide |
May increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, QT prolongation) [see Warnings and Precautions (5.6, 5.11, 5.12)] . |
Monitor tacrolimus whole blood trough concentrations and reduce tacrolimus dose if needed [see Dosage and Administration (2.2, 2.6)and Clinical Pharmacology (12.3)] . |
|
Mild or Moderate CYP3A Inducers Methylprednisolone, prednisone |
May decrease tacrolimus whole blood trough concentrations. |
Monitor tacrolimus whole blood trough concentrations and adjust tacrolimus dose if needed [see Dosage and Administration (2.2, 2.6)] . |
|
Caspofungin |
May decrease tacrolimus whole blood trough concentrations. |
Monitor tacrolimus whole blood trough concentrations and adjust tacrolimus dose if needed [see Dosage and Administration (2.2, 2.6)]. |
Direct Acting Antiviral (DAA) Therapy
The pharmacokinetics of tacrolimus may be impacted by changes in liver function during DAA therapy, related to clearance of HCV virus. Close monitoring and potential dose adjustment of tacrolimus is warranted to ensure continued efficacy and safety [see Dosage and Administration (2.2, 2.6)] .
7.3 Cannabidiol
The blood levels of tacrolimus may increase upon concomitant use with cannabidiol. When cannabidiol and tacrolimus are co-administered, closely monitor for an increase in tacrolimus blood levels and for adverse reactions suggestive of tacrolimus toxicity. A dose reduction of tacrolimus should be considered as needed when tacrolimus is co-administered with cannabidiol [see Dosage and Administration (2.2, 2.6)and Warnings and Precautions (5.17)].
- Mycophenolic Acid Products: Can increase MPA exposure after crossover from cyclosporine to tacrolimus; monitor for MPA-related adverse reactions and adjust MMF or MPA dose as needed. ( 7.1)
- Nelfinavir and Grapefruit Juice: Increased tacrolimus concentrations via CYP3A inhibition; avoid concomitant use. ( 7.2)
- CYP3A Inhibitors: Increased tacrolimus concentrations; monitor concentrations and adjust tacrolimus dose as needed. ( 5.11, 7.2)
- CYP3A4 Inducers: Decreased tacrolimus concentrations; monitor concentrations and adjust tacrolimus dose as needed. ( 5.11, 7.2)
- Therapeutic drug monitoring and dose reduction for tacrolimus should be considered when tacrolimus is co-administered with cannabidiol( 5.17, 7.3)
SPL PATIENT PACKAGE INSERT SECTION
|
Patient Information Tacrolimus Capsules (ta-KROE-li-mus) | |
|
Read this Patient Information before you start taking tacrolimus capsules and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. | |
|
What is the most important information I should know about tacrolimus capsules? Tacrolimus capsules can cause serious side effects, including: ***Increased risk of cancer.**People who take tacrolimus capsules have an increased risk of getting some kinds of cancer, including skin and lymph gland cancer (lymphoma). ***Increased risk of infection.**Tacrolimus capsules is a medicine that affects your immune system. Tacrolimus capsules can lower the ability of your immune system to fight infections. Serious infections can happen in people receiving tacrolimus capsules that can cause death.Call your healthcare provider right away if you have any symptoms of an infection, including: | |
|
|
|
What are tacrolimus capsules?
| |
|
Who should not take tacrolimus capsules?
| |
|
What should I tell my healthcare provider before taking tacrolimus capsules? Before taking tacrolimus capsules, tell your healthcare provider about all of your medical conditions, including if you:
**Tell your healthcare provider about all the medicines you take, and when you start a new medicine or stop taking a medicine,**including prescription and over-the-counter medicines, vitamins, natural, herbal, or nutritional supplements. Especially tell your healthcare provider if you take:
Ask your healthcare provider or pharmacist if you are not sure if you take any of the medicines listed above. Tacrolimus capsules may affect the way other medicines work, and other medicines may affect how tacrolimus capsules work. Know the medicines you take. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine. | |
|
How should I take tacrolimus capsules?
Tacrolimus capsules: *Do notopen or crush tacrolimus capsules. | |
|
What should I avoid while taking tacrolimus capsules?
| |
|
What are the possible side effects of tacrolimus capsules? Tacrolimus capsules may cause serious side effects, including:
| |
|
|
|
***kidney problems.**Kidney problems are a serious and common side effect of tacrolimus capsules. Your healthcare provider may do blood tests to check your kidney function while you take tacrolimus capsules. ***nervous system problems.**Nervous system problems are a serious and common side effect of tacrolimus capsules. Call your healthcare provider right away if you get any of these symptoms while taking tacrolimus capsules. These could be signs of a serious nervous system problem: | |
|
|
|
***high levels of potassium in your blood.**Your healthcare provider may do blood tests to check your potassium level while you take tacrolimus capsules. ***high blood pressure.**High blood pressure is a serious and common side effect of tacrolimus capsules. Your healthcare provider will monitor your blood pressure while you take tacrolimus capsules and may prescribe blood pressure medicine for you, if needed. Your healthcare provider may instruct you to check your blood pressure at home. *changes in the electrical activity of your heart (QT prolongation). ***heart problems (myocardial hypertrophy).**Tell your healthcare provider right away if you get any of these symptoms of heart problems while taking tacrolimus capsules: | |
|
|
|
*severe low red blood cell count (anemia). ***blood clotting problems:**Tell your healthcare provider right away if you have fever and bruising under the skin that may appear as red dots, with or without unexplained tiredness, confusion, yellowing of the skin or eyes, decreased urination. When taken with sirolimus or everolimus, the risk of developing these symptoms may increase. The most common side effects of tacrolimus capsules in people who have received a kidney, liver, or heart transplant are: | |
|
|
|
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of tacrolimus capsules. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |
|
How should I store tacrolimus capsules?
Keep tacrolimus capsules and all medicines out of the reach of children. | |
|
General information about the safe and effective use of tacrolimus capsules.
For more information, go to www.accordhealthcare.us or call Accord Healthcare Inc. at 1-866-941-7875. | |
|
What are the ingredients in tacrolimus capsules? **Active ingredient:**tacrolimus **Inactive ingredients:**lactose monohydrate, hypromellose E5, croscarmellose sodium, and magnesium stearate. The 0.5 mg capsule shell contains gelatin, titanium dioxide, iron oxide yellow and sodium lauryl sulfate, the 1 mg capsule shell contains gelatin, titanium dioxide and sodium lauryl sulfate, and the 5 mg capsule shell contains gelatin, titanium dioxide, iron oxide red and sodium lauryl sulfate. Additional pediatric use information is approved for Astellas Pharma US, Inc.’s Prograf (tacrolimus) products. However, due to Astellas Pharma US, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information. Manufactured For: Manufactured By: 10 0108 9 6033306 |
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 12/2024
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Warnings and Precautions ( 5.5, 5.10, 5.16) |
11/2022 |
|
Warnings and Precautions, Cannabidiol Drug Interactions ( 5.17) |
08/2023 |
RECENT MAJOR CHANGES
Warnings and Precautions ( 5.5, 5.10, 5.16) 11/2022
Warnings and Precautions, Cannabidiol Drug Interactions ( 5.17) 08/2023
DESCRIPTION SECTION
11 DESCRIPTION
Tacrolimus, previously known as FK506, is the active ingredient in tacrolimus capsules. Tacrolimus is a calcineurin-inhibitor immunosuppressant produced by Streptomyces tsukubaensis. Chemically, tacrolimus is designated as [3 S-[3 R*[ E(1 S*,3 S*,4 S*)], 4 S*,5 R*,8 S*,9 E,12 R*,14 R*,15 S*,16 R*,18 S*,19 S*,26a R*]]-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-3-[2-(4-hydroxy-3-methoxycyclohexyl)-1-methylethenyl]-14,16-dimethoxy-4,10,12,18-tetramethyl-8-(2-propenyl)-15,19-epoxy-3H-pyrido[2,1- c][1,4]oxaazacyclotricosine-1,7,20,21(4H,23H)-tetrone, monohydrate.
The chemical structure of tacrolimus is:

Tacrolimus has an empirical formula of C 44H 69NO 12•H 2O and a formula weight of 822.03. Tacrolimus appears as white crystals or crystalline powder. It is practically insoluble in water, freely soluble in ethanol, and very soluble in methanol and chloroform.
Tacrolimus capsules, USP are available for oral administration containing 0.5 mg, 1 mg or 5 mg of tacrolimus. Inactive ingredients include lactose monohydrate, hypromellose E5, croscarmellose sodium, and magnesium stearate.
The 0.5 mg capsule shell contains gelatin, titanium dioxide, iron oxide yellow and sodium lauryl sulfate, the 1 mg capsule shell contains gelatin, titanium dioxide and sodium lauryl sulfate, and the 5 mg capsule shell contains gelatin, titanium dioxide, iron oxide red and sodium lauryl sulfate.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling ( Patient Information and Instructions for Use).
17.1 Administration
Advise the patient or caregiver to:
- Inspect their tacrolimus capsules medicine when they receive a new prescription and before taking it. If the appearance of the capsule is not the same as usual, or if dosage instructions have changed, advise patients to contact their healthcare provider as soon as possible to make sure that they have the right medicine. Other tacrolimus products cannot be substituted for tacrolimus capsules.
- Take tacrolimus capsules at the same 12-hour intervals every day to achieve consistent blood concentrations.
- Take tacrolimus capsules consistently either with or without food because the presence and composition of food decreases the bioavailability of tacrolimus.
- Not to eat grapefruit or drink grapefruit juice in combination with tacrolimus capsules [see Drug Interactions (7.2)].
17.2 Development of Lymphoma and Other Malignancies
Inform patients they are at increased risk of developing lymphomas and other malignancies, particularly of the skin, due to immunosuppression. Advise patients to limit exposure to sunlight and ultraviolet (UV) light by wearing protective clothing and using a broad spectrum sunscreen with a high protection factor [see Warnings and Precautions (5.1)] .
17.3 Increased Risk of Infection
Inform patients they are at increased risk of developing a variety of infections, including opportunistic infections, due to immunosuppression and to contact their physician if they develop any symptoms of infection such as fever, sweats or chills, cough or flu-like symptoms, muscle aches, or warm, red, painful areas on the skin [see Warnings and Precautions (5.2)] .
17.4 New Onset Diabetes After Transplant
Inform patients that tacrolimus can cause diabetes mellitus and should be advised to contact their physician if they develop frequent urination, increased thirst, or hunger [see Warnings and Precautions (5.4)] .
17.5 Nephrotoxicity
Inform patients that tacrolimus can have toxic effects on the kidney that should be monitored. Advise patients to attend all visits and complete all blood tests ordered by their medical team [see Warnings and Precautions (5.5)] .
17.6 Neurotoxicity
Inform patients that they are at risk of developing adverse neurologic reactions including seizure, altered mental status, and tremor. Advise patients to contact their physician should they develop vision changes, delirium, or tremors [see Warnings and Precautions (5.6)] .
17.7 Hyperkalemia
Inform patients that tacrolimus can cause hyperkalemia. Monitoring of potassium levels may be necessary, especially with concomitant use of other drugs known to cause hyperkalemia [see Warnings and Precautions (5.7)] .
17.8 Hypertension
Inform patients that tacrolimus can cause high blood pressure which may require treatment with antihypertensive therapy. Advise patients to monitor their blood pressure [see Warnings and Precautions (5.8)] .
17.9 Thrombotic Microangiopathy
Inform patients that tacrolimus can cause blood clotting problems. The risk of this occurring increases when patients take tacrolimus and sirolimus or everolimus concomitantly, or when patients develop certain infections. Advise them to seek medical attention promptly if they develop fever, petequiae or bruises, fatigue, confusion, jaundice, oliguria. [ see Warnings and Precautions (5.16)]
17.10 Drug Interactions
Instruct patients to tell their healthcare providers when they start or stop taking any medicines, including prescription medicines and nonprescription medicines, natural or herbal remedies, nutritional supplements, and vitamins. Advise patients to avoid grapefruit and grapefruit juice [see Drug Interactions (7)].
17.11 Pregnancy, Lactation and Infertility
Inform women of childbearing potential that tacrolimus can harm the fetus. Instruct male and female patients to discuss with their healthcare provider family planning options including appropriate contraception. Also, discuss with pregnant patients the risks and benefits of breastfeeding their infant [see Use in Specific Populations (8.1, 8.2, 8.3)] .
Encourage female transplant patients who become pregnant and male patients who have fathered a pregnancy, exposed to immunosuppressants including tacrolimus, to enroll in the voluntary Transplantation Pregnancy Registry International. To enroll or register, patients can call the toll free number 1-877-955-6877 or https://www.transplantpregnancyregistry.org/ [see Use in Specific Populations (8.1)] .
Based on animal studies, tacrolimus may affect fertility in males and females [see Nonclinical Toxicology (13.1)] .
17.12 Myocardial Hypertrophy
Inform patients to report symptoms of tiredness, swelling, and/or shortness of breath (heart failure).
17.13 Immunizations
Inform patients that tacrolimus capsules can interfere with the usual response to immunizations and that they should avoid live vaccines. [see Warnings and Precautions (5.14)] .
Manufactured For:
Accord Healthcare, Inc.,
8041 Arco Corporate Drive,
Suite 200,
Raleigh, NC 27617,
USA.
Manufactured By:
Intas Pharmaceuticals Limited,
Plot No : 457, 458,
Village – Matoda,
Bavla Road, Ta.- Sanand,
Dist.- Ahmedabad – 382210.
India.
10 0108 9 6033306
Issued December 2024
