Lutathera
These highlights do not include all the information needed to use LUTATHERA safely and effectively. See full prescribing information for LUTATHERA. LUTATHERA (lutetium Lu 177 dotatate) injection, for intravenous use Initial U.S. Approval: 2018
72d1a024-00b7-418a-b36e-b2cb48f2ab55
HUMAN PRESCRIPTION DRUG LABEL
Mar 7, 2023
Advanced Accelerator Applications USA, Inc
DUNS: 051714355
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Lutetium Lu 177 dotatate
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Drug Labeling Information
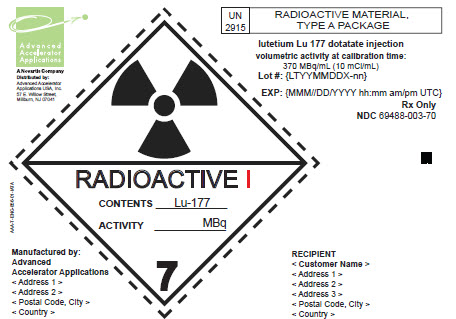
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
Type A Label (IATA)
lutetium Lu 177 dotatate injection
volumetric activity at calibration time:
370 MBq/mL (10 mCi/mL)
Rx Only
NDC 69488-003-70
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Risk from Radiation Exposure
LUTATHERA contributes to a patient’s overall long-term cumulative radiation exposure. Long-term cumulative radiation exposure is associated with an increased risk for cancer.
Radiation can be detected in the urine for up to 30 days following LUTATHERA administration. Minimize radiation exposure to patients, medical personnel, and household contacts during and after treatment with LUTATHERA consistent with institutional good radiation safety practices, patient management procedures, Nuclear Regulatory Commission patient-release guidance, and instructions to the patient for follow-up radiation protection at home [see Dosage and Administration (2.1), Clinical Pharmacology (12.3)].
5.2 Myelosuppression
In NETTER-1, myelosuppression occurred more frequently in patients receiving LUTATHERA with long-acting octreotide compared to patients receiving high-dose long-acting octreotide (all Grades/Grade 3 or 4): anemia (81%/0) versus (54%/1%); thrombocytopenia (53%/1%) versus (17%/0); and neutropenia (26%/3%) versus (11%/0). In NETTER-1, platelet nadir occurred at a median of 5.1 months following the first dose. Of the 59 patients who developed thrombocytopenia, 68% had platelet recovery to baseline or normal levels. The median time to platelet recovery was 2 months. Fifteen of the nineteen patients in whom platelet recovery was not documented had post-nadir platelet counts. Among these 15 patients, 5 improved to Grade 1, 9 to Grade 2, and 1 to Grade 3.
Monitor blood cell counts. Withhold dose, reduce dose, or permanently discontinue LUTATHERA based on the severity of myelosuppression [see Dosage and Administration (2.4)].
5.3 Secondary Myelodysplastic Syndrome and Leukemia
In NETTER-1, with a median follow-up time of 76 months in the main study, myelodysplastic syndrome (MDS) was reported in 2.3% of patients receiving LUTATHERA with long-acting octreotide compared to no patients receiving high- dose long-acting octreotide.
In ERASMUS, 16 patients (2.0%) developed MDS and 4 (0.5%) developed acute leukemia. The median time to onset was 29 months (9 to 45 months) for MDS and 55 months (32 to 125 months) for acute leukemia.
5.4 Renal Toxicity
In ERASMUS, 8 patients (< 1%) developed renal failure 3 to 36 months following LUTATHERA. Two of these patients had underlying renal impairment or risk factors for renal failure (e.g., diabetes or hypertension) and required dialysis.
Administer the recommended amino acid solution before, during and after LUTATHERA [see Dosage and Administration (2.3)] to decrease the reabsorption of lutetium Lu 177 dotatate through the proximal tubules and decrease the radiation dose to the kidneys. Advise patients to hydrate and to urinate frequently before, on the day of, and the day after administration of LUTATHERA.
Monitor serum creatinine and calculated creatinine clearance. Withhold dose, reduce dose, or permanently discontinue LUTATHERA based on the severity of renal toxicity [see Dosage and Administration (2.4)].
Patients with baseline renal impairment may be at increased risk of toxicity due to increased radiation exposure [see Use in Specific Populations (8.6)].
5.5 Hepatotoxicity
In ERASMUS, 2 patients (< 1%) were reported to have hepatic tumor hemorrhage, edema, or necrosis, with one patient experiencing intrahepatic congestion and cholestasis. Patients with hepatic metastasis may be at increased risk of hepatotoxicity due to radiation exposure.
Monitor transaminases, bilirubin, serum albumin and international normalized ratio (INR) during treatment. Withhold dose, reduce dose, or permanently discontinue LUTATHERA based on the severity of hepatotoxicity [see Dosage and Administration (2.4)].
5.6 Hypersensitivity Reactions
Hypersensitivity reactions, including angioedema, occurred in patients treated with LUTATHERA [see Adverse Reactions (6.2)]. Monitor patients closely for signs and symptoms of hypersensitivity reactions, including anaphylaxis, during and following LUTATHERA administration for a minimum of 2 hours in a setting where cardiopulmonary resuscitation medication and equipment are available. Discontinue the infusion upon the first observation of any signs or symptoms consistent with a severe hypersensitivity reaction and initiate appropriate therapy.
Premedicate patients with a history of Grade 1 or 2 hypersensitivity reactions to LUTATHERA before subsequent doses [see Dosage and Administration (2.3)]. Permanently discontinue LUTATHERA in patients who experience Grade 3 or 4 hypersensitivity reactions [see Dosage and Administration (2.4)].
5.7 Neuroendocrine Hormonal Crisis
Neuroendocrine hormonal crises, manifesting with flushing, diarrhea, bronchospasm and hypotension, occurred in < 1% of patients in ERASMUS and typically occurred during or within 24 hours following the initial LUTATHERA dose. Two (< 1%) patients were reported to have hypercalcemia.
Monitor patients for flushing, diarrhea, hypotension, bronchoconstriction or other signs and symptoms of tumor-related hormonal release. Administer intravenous somatostatin analogs, fluids, corticosteroids, and electrolytes as indicated.
5.8 Embryo-Fetal Toxicity
Based on its mechanism of action, LUTATHERA can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data on LUTATHERA use in pregnant women. No animal studies using lutetium Lu 177 dotatate have been conducted to evaluate its effect on female reproduction and embryo-fetal development; however, radioactive emissions, including those from LUTATHERA, can cause fetal harm.
Verify pregnancy status of females of reproductive potential prior to initiating LUTATHERA [see Dosage and Administration (2.1)].
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with LUTATHERA and for 7 months after the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with LUTATHERA and for 4 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
5.9 Risk of Infertility
LUTATHERA may cause infertility in males and females. The recommended cumulative dose of 29.6 GBq of LUTATHERA results in a radiation absorbed dose to the testes and ovaries within the range where temporary or permanent infertility can be expected following external beam radiotherapy [see Dosage and Administration (2.6), Use in Specific Populations (8.3)].
- Risk From Radiation Exposure: Minimize radiation exposure during and after treatment with LUTATHERA consistent with institutional good radiation safety practices and patient management procedures. (2.1, 5.1)
- Myelosuppression: Monitor blood cell counts. Withhold dose, reduce dose, or permanently discontinue based on the severity. (2.4, 5.2)
- Secondary Myelodysplastic Syndrome (MDS) and Leukemia: Median time to onset: MDS is 29 months; acute leukemia is 55 months. (5.3)
- Renal Toxicity: Advise patients to hydrate and to urinate frequently before, on the day of and the day after administration of LUTATHERA. Monitor serum creatinine and calculated creatinine clearance. Withhold dose, reduce dose, or permanently discontinue based on the severity. (2.3, 2.4, 5.4)
- Hepatotoxicity: Monitor transaminases, bilirubin, serum albumin and INR. (2.4, 5.5)
- Hypersensitivity Reactions: Monitor patients closely for signs and symptoms of hypersensitivity reactions, including anaphylaxis. Permanently discontinue LUTATHERA based on severity. (2.3, 2.4, 5.6)
- Neuroendocrine Hormonal Crisis: Monitor for flushing, diarrhea, hypotension, bronchoconstriction or other signs and symptoms. (5.7)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females and males of reproductive potential of the potential risk to a fetus and to use effective contraception. (5.8, 8.1, 8.3)
- Risk of Infertility: LUTATHERA may cause infertility. (5.9, 8.3)
RECENT MAJOR CHANGES SECTION
RECENT MAJOR CHANGES
|
Dosage and Administration (2.1, 2.3, 2.4, 2.5, 2.6) |
6/2022 |
|
Dosage and Administration (2.2, 2.3, 2.4, 2.5) |
3/2023 |
|
Warnings and Precautions (5.3, 5.5, 5.6, 5.8) |
6/2022 |
|
Warnings and Precautions (5.2, 5.4, 5.5) |
3/2023 |
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity and mutagenicity studies have not been conducted with lutetium Lu 177 dotatate; however, radiation is a carcinogen and mutagen.
No animal studies were conducted to determine the effects of lutetium Lu 177 dotatate on fertility.
13.2 Animal Toxicology and/or Pharmacology
The primary target organ in animal studies using the non-radioactive lutetium Lu 175 dotatate was the pancreas, a high SSTR2 expressing organ. Pancreatic acinar apoptosis occurred at lutetium Lu 175 dotatate doses ≥ 5 mg/kg in repeat dose toxicology studies in rats. Pancreatic acinar cell atrophy also occurred in repeat dose toxicology studies in dogs at doses ≥ 500 mcg/kg. These findings were consistent with high uptake of the radiolabeled peptide in the pancreas in animal biodistribution studies.
INFORMATION FOR PATIENTS SECTION
17 PATIENT COUNSELING INFORMATION
Risk From Radiation Exposure
Advise patients to minimize radiation exposure to household contacts during and after treatment with LUTATHERA consistent with institutional good radiation safety practices and patient management procedures [see Dosage and Administration (2.1), Warnings and Precautions (5.1)].
Myelosuppression
Advise patients to contact their healthcare provider for any signs or symptoms of myelosuppression or infection, such as fever, chills, dizziness, shortness of breath, or increased bleeding or bruising [see Warnings and Precautions (5.2)].
Secondary Myelodysplastic Syndrome and Leukemia
Advise patients of the potential for secondary cancers, including myelodysplastic syndrome and acute leukemia [see Warnings and Precautions (5.3)].
Renal Toxicity
Advise patients to hydrate and to urinate frequently before, on the day of, and the day after administration of LUTATHERA [see Warnings and Precautions (5.4)]. Advise patients to contact their healthcare provider for any signs or symptoms of renal toxicity [see Warnings and Precautions (5.4)].
Hepatotoxicity
Advise patients of the need for periodic laboratory tests to monitor for hepatotoxicity [see Warnings and Precautions (5.5)]. Advise patients to contact their healthcare provider for any signs or symptoms of hepatotoxicity [see Warnings and Precautions (5.5)].
Hypersensitivity
Advise patients that LUTATHERA may cause hypersensitivity reactions, including angioedema, and to seek immediate medical attention for signs or symptoms of hypersensitivity [see Warnings and Precautions (5.6)].
Neuroendocrine Hormonal Crises
Advise patients to contact their healthcare provider for signs or symptoms that may occur following tumor-related hormonal release, including severe flushing, diarrhea, bronchospasm, and hypotension [see Warnings and Precautions (5.7)].
Embryo-Fetal Toxicity
Advise pregnant women and males and females of reproductive potential of the potential risk to a fetus. Advise females to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.8), Use in Specific Populations (8.1, 8.3)].
Advise females of reproductive potential to use effective contraception during treatment with LUTATHERA and for 7 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
Advise male patients with female partners of reproductive potential to use effective contraception during treatment with LUTATHERA and for 4 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
Lactation
Advise females not to breastfeed during treatment with LUTATHERA and for 2.5 months after the last dose [see Use in Specific Populations (8.2)].
Infertility
Advise female and male patients that LUTATHERA may impair fertility [see Warnings and Precautions (5.9), Use in Specific Populations (8.3)].
Distributed by:
Advanced Accelerator Applications USA, Inc., Millburn NJ 07041
©2023 Advanced Accelerator Applications USA, Inc.
LUTATHERA® is a registered trademark of Novartis AG and/or its affiliates.
T2023-05
