Dalfampridine
These highlights do not include all the information needed to use DALFAMPRIDINE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for DALFAMPRIDINE EXTENDED-RELEASE TABLETS. DALFAMPRIDINE extended-release tablets, for oral use Initial U.S. Approval: 2010
e10b2d92-2824-4395-8883-6fd52c784aa4
HUMAN PRESCRIPTION DRUG LABEL
Jan 30, 2023
Ascend Laboratories, LLC
DUNS: 141250469
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Dalfampridine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (7)
Drug Labeling Information
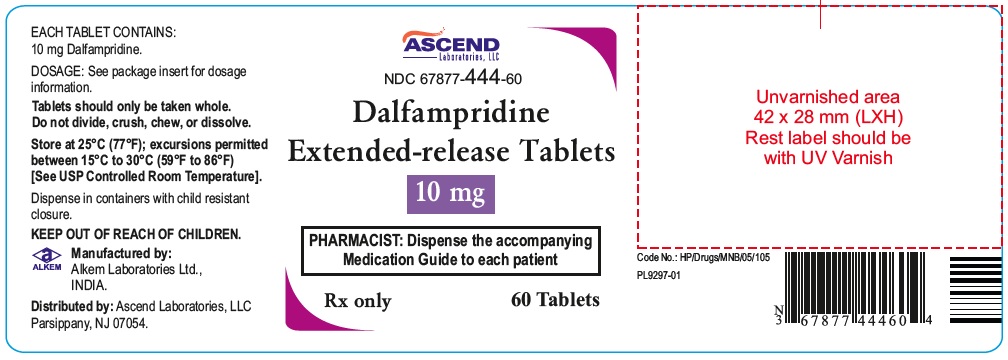
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Dalfampridine Extended-release Tablets
** Rx ONLY**
** 10 mg**
** PHARMACIST: Dispense the accompanying Medication Guide to each patient**
** 60 tablets**
**
**
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Seizures
Dalfampridine extended-release tablets can cause seizures. Increased incidence of seizures has been observed at 20 mg twice daily (2 times the maximum recommended dosage) in controlled clinical studies of 9 to 14 weeks duration with dalfampridine in patients with MS. In open-label extension trials in MS patients, the incidence of seizures during treatment with dalfampridine 15 mg twice daily (1.7/100PY) was over 4 times higher than the incidence during treatment with 10 mg twice daily (0.4/100PY). In the post-marketing period seizures have been reported. The majority of seizures occurred at the recommended dose and in patients without a history of seizures, and generally within days to weeks of starting therapy.
Dalfampridine extended-release tablets has not been evaluated in patients with a history of seizures or with evidence of epileptiform activity on an EEG, as these patients were excluded from clinical trials. The risk of seizures in patients with epileptiform activity on an EEG is unknown, and could be substantially higher than that observed in dalfampridine extended-release tablets clinical studies. Permanently discontinue dalfampridine extended- release tablets in patients who have a seizure while on treatment. Dalfampridine extended-release tablets are contraindicated in patients with a history of seizures [see Contraindications (4)].
5.2 Renal Impairment
Dalfampridine extended-release tablets are eliminated through the kidneys primarily as unchanged drug [see Clinical Pharmacology (12.3)].
Because patients with moderate to severe renal impairment (CrCl ≤50mL/min) would require a dose lower than 10 mg twice daily and no strength smaller than 10 mg is available, dalfampridine extended-release tablets are contraindicated in these patients [see Contraindications (4)].
In patients with mild renal impairment (CrCl 51 to 80 mL/min), dalfampridine extended-release tablets plasma levels may approach those seen at a dose of 15 mg twice daily, a dose that may be associated with an increased risk of seizures [see Warnings and Precautions (5.1)].
5.3 Concurrent Treatment with Other Forms of 4-Aminopyridine
Avoid concomitant use with other forms of 4-aminopyridine (4-AP, fampridine) since the active ingredient is the same. Instruct patients to discontinue use of any product containing 4-aminopyridine prior to initiating treatment with dalfampridine extended-release tablets in order to reduce the potential for dose-related adverse reactions.
5.4 Anaphylaxis
Dalfampridine extended-release tablets can cause anaphylaxis and severe allergic reactions. Signs and symptoms have included respiratory compromise, urticaria, and angioedema of the throat and or tongue. Dalfampridine extended- release tablets are contraindicated in patients with a history of hypersensitivity to dalfampridine extended-release tablets or 4-aminopyridine. Inform patients of the signs and symptoms of anaphylaxis and instruct them to discontinue dalfampridine extended-release tablets and seek immediate medical care should these signs and symptoms occur.
- Dalfampridine extended-release tablets can cause seizures; the risk of seizures increases with increasing dalfampridine extended-release tablets doses; discontinue dalfampridine extended-release tablets and do not restart if a seizure occurs (5.1)
- Avoid concomitant use with other forms of 4-aminopyridine (4-AP, fampridine), since the active ingredient is the same (5.3)
- Dalfampridine extended-release tablets can cause anaphylaxis. Discontinue and do not restart dalfampridine extended-release tablets if this occurs (5.4)
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
7.1 OCT2 Inhibitors
Concurrent treatment with OCT2 inhibitors, such as cimetidine, may cause increased exposure to dalfampridine [see Clinical Pharmacology (12.3)]. Elevated levels of dalfampridine increase the risk of seizures [see Warnings and Precautions (5.1, 5.2)]. The potential benefits of taking OCT2 inhibitors concurrently with dalfampridine extended-release tablets should be considered against the risk of seizures in these patients.
7.2 Baclofen
No interaction was identified between dalfampridine and baclofen [see Clinical Pharmacology (12.3)].
OCT2 Inhibitors: Concomitant use may cause an increased exposure and potential risk of seizures (7.1)
CLINICAL PHARMACOLOGY SECTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of action
The mechanism by which dalfampridine exerts its therapeutic effect has not been fully elucidated. Dalfampridine is a broad spectrum potassium channel blocker. In animal studies, dalfampridine has been shown to increase conduction of action potentials in demyelinated axons through inhibition of potassium channels.
12.2 Pharmacodynamics
Dalfampridine extended-release tablets does not prolong the QTc interval and does not have a clinically important effect on QRS duration.
12.3 Pharmacokinetics
Absorption and Distribution
Orally administered dalfampridine is rapidly and completely absorbed from the
gastrointestinal tract. Absolute bioavailability of dalfampridine extended-
release tablets has not been assessed, but relative bioavailability is 96%
when compared to an aqueous oral solution. The extended release tablet delays
absorption of dalfampridine relative to the solution formulation, giving a
slower rise to a lower peak concentration (Cmax), with no effect on the extent
of absorption (AUC). Single dalfampridine extended-release tablet 10 mg doses
administered to healthy volunteers in a fasted state gave peak concentrations
ranging from 17.3 ng/mL to 21.6 ng/mL occurring 3 to 4 hours post-
administration (Tmax). In comparison, Cmax with the same 10 mg dose of
dalfampridine in an oral solution was 42.7 ng/mL and occurred approximately
1.3 hours after dosing. Exposure increased proportionally with dose.
Dalfampridine is largely unbound to plasma proteins (97 to 99%). The apparent
volume of distribution is 2.6 L/kg.
There is no apparent difference in pharmacokinetic parameter values following
administration of dalfampridine extended-release tablets to either healthy
volunteers or patients with MS.
When dalfampridine is taken with food, there is a slight increase in Cmax (12
to 17%) and a slight decrease in AUC (4 to 7%). These changes in exposure are
not clinically significant, and therefore the drug may be taken with or
without food [see Dosage and Administration (2.2)].
Metabolism and Elimination
Dalfampridine and metabolites elimination is nearly complete after 24 hours,
with 95.9% of the dose recovered in urine and 0.5% recovered in feces. Most of
the excreted radioactivity in urine was parent drug (90.3%). Two metabolites
were identified: 3-hydroxy-4-aminopyridine (4.3%) and
3-hydroxy-4-aminopyridine sulfate (2.6%). These metabolites have been shown to
have no pharmacologic activity on potassium channels.
The apparent elimination half-life of dalfampridine following administration
of the extended release tablet formulation of dalfampridine is 5.2 to 6.5
hours. The plasma half-life of the sulfate conjugate is approximately 7.6
hours and the half-life of 3-hydroxy-4-aminopyridine could not be calculated
because concentrations for most subjects were close to or below the limit of
quantitation.
In vitro studies with human liver microsomes indicate that CYP2E1 was the major enzyme responsible for the 3-hydroxylation of dalfampridine. The identity of the CYP enzymes suspected of playing a minor role in the 3-hydroxylation of dalfampridine could not be established unequivocally.
Specific Populations
Pediatric
The safety and effectiveness in patients younger than 18 years of age have not
been established.
Geriatric
A population pharmacokinetic analysis showed that dalfampridine clearance
modestly decreased with increasing age, but not sufficiently to necessitate a
modification of dose.
Gender
A population pharmacokinetic analysis suggested that female patients would be
expected to have higher maximum dalfampridine plasma concentration than male
patients. The magnitude of these differences is small and does not necessitate
any dose modification.
Renal Impairment [see Contraindications (4) and Warnings and Precautions (5.2)]. The pharmacokinetics of dalfampridine was studied in 9 male and 11 female subjects with varying degrees of renal function. Elimination of the drug is significantly correlated with the creatinine clearance. Total body clearance of dalfampridine was reduced by about 45% in patients with mild renal impairment (CrCl 51 to 80 mL/min), by about 50% in patients with moderate renal impairment (CrCl = 30 to 50 mL/min), and by about 75% in patients with severe renal impairment (CrCl <30 mL/min). The terminal half- life of dalfampridine is about 3.3 times longer in patients with severe renal impairment but is not prolonged in patients with mild or moderate renal impairment.
Hepatic Impairment
The pharmacokinetics of dalfampridine in hepatically impaired subjects has not
been studied. Since dalfampridine is primarily excreted unchanged in the
urine, hepatic impairment is not expected to significantly affect
dalfampridine pharmacokinetics or recommended dosing.
Race
There were too few non-Caucasians in the patient population to evaluate the
effect of race.
Drug Interactions
Effects of Co-administered Drugs on Dalfampridine
Interferon
Dalfampridine kinetics were not affected by co-administration of subcutaneous
injections of 8 million units interferon beta-1b.
Baclofen
Based on a population analysis, dalfampridine kinetics were not affected by baclofen.
Cimetidine
In a single-dose clinical study, 23 healthy volunteers took the OCT2 inhibitor
cimetidine 400 mg every 6 hours concurrently with dalfampridine 10 mg single
dose. The test-reference ratio for AUC0–∞ was 125% (90% confidence interval:
121% to 130%) due to a reduction in the clearance of dalfampridine [see Drug Interactions (7.1)].
Effects of Dalfampridine on Co-administered Drugs
In vitro data with human liver microsomes showed that dalfampridine was not a direct or time-dependent inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, or CYP3A4/5. Dalfampridine is not likely to affect the pharmacokinetics of drugs that are substrates of these enzymes.
Other in vitro studies with cultured human hepatocytes with 0.025 μM, 0.25 μM,
2.5 μM, and 25 μM dalfampridine had little or no effect on CYP1A2, CYP2B6,
CYP2C9, CYP2C19, CYP2E1, or CYP3A4/5 enzyme activities. Consequently, the
potential for dalfampridine to induce human hepatocytes at therapeutic
concentrations is remote.
In vitro, dalfampridine is not a substrate or an inhibitor for the
p-glycoprotein transporter. The pharmacokinetics of dalfampridine extended-
release tablets are unlikely to be affected by drugs that inhibit the
p-glycoprotein transporter, and dalfampridine is not likely to affect the
pharmacokinetics of drugs that are substrates of the p-glycoprotein
transporter.
