Pacerone
These highlights do not include all the information needed to use PACERONE safely and effectively. See full prescribing information for PACERONE. PACERONE (amiodarone hydrochloride) tablets, for oral use Initial U.S. Approval: 1985
4c4ec9b0-13a5-49a8-b57b-b3f64e4316a7
HUMAN PRESCRIPTION DRUG LABEL
May 31, 2023
Upsher-Smith Laboratories, LLC
DUNS: 079111820
Products 3
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Amiodarone Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Amiodarone Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (8)
Amiodarone Hydrochloride
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (7)
Drug Labeling Information
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
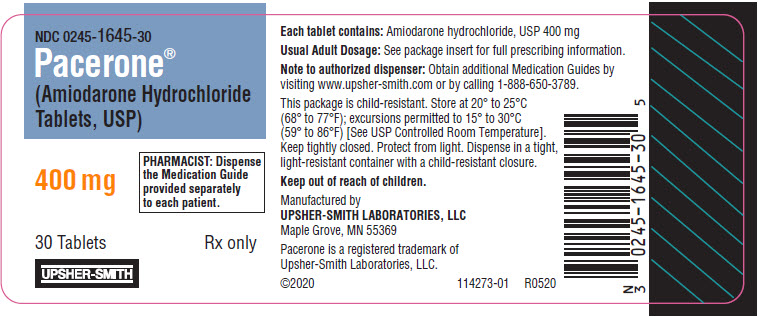
PRINCIPAL DISPLAY PANEL - 400 mg Tablet Bottle Label
NDC 0245-1645-30
Pacerone®
(Amiodarone Hydrochloride
Tablets, USP)
400 mg
PHARMACIST: Dispense
the Medication Guide
provided separately
to each patient.
30 Tablets
Rx only
UPSHER-SMITH
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Persistence of Adverse Effects
Because of the long half-life of amiodarone (15 to 142 days) and its active metabolite desethylamiodarone (14 to 75 days), adverse reactions and drug interactions can persist for several weeks following amiodarone discontinuation [see Clinical Pharmacology (12.3)].
5.2 Pulmonary Toxicity
Pacerone may cause a clinical syndrome of cough and progressive dyspnea accompanied by functional, radiographic, gallium-scan, and pathological data consistent with pulmonary toxicity. Pulmonary toxicity secondary to Pacerone may result from either indirect or direct toxicity as represented by hypersensitivity pneumonitis (including eosinophilic pneumonia) or interstitial/alveolar pneumonitis, respectively. Rates of pulmonary toxicity have been reported to be as high as 17% and is fatal in about 10% of cases. Obtain a baseline chest X-ray and pulmonary-function tests, including diffusion capacity, when Pacerone therapy is initiated. Repeat history, physical exam, and chest X-ray every 3 to 6 months or if symptoms occur. Consider alternative antiarrhythmic therapy if the patient experiences signs or symptoms of pulmonary toxicity. Prednisone 40 to 60 mg/day tapered over several weeks may be helpful in treating pulmonary toxicity.
Adult Respiratory Distress Syndrome (ARDS)
Postoperatively, occurrences of ARDS have been reported in patients receiving amiodarone hydrochloride therapy who have undergone either cardiac or noncardiac surgery. Although patients usually respond well to vigorous respiratory therapy, in rare instances the outcome has been fatal.
5.3 Hepatic Injury
Asymptomatic elevations of hepatic enzyme levels are seen frequently, but Pacerone can cause life-threatening hepatic injury. Histology has resembled that of alcoholic hepatitis or cirrhosis. Obtain baseline and periodic liver transaminases. If transaminases exceed three times normal, or doubles in a patient with an elevated baseline, discontinue or reduce dose of Pacerone, obtain follow-up tests and treat appropriately.
5.4 Worsened Arrhythmia
Pacerone can exacerbate the presenting arrhythmia in about 2% to 5% of patients or cause new ventricular fibrillation, incessant ventricular tachycardia, increased resistance to cardioversion, and polymorphic ventricular tachycardia associated with QTc prolongation (Torsade de Pointes [TdP]).
Correct hypokalemia, hypomagnesemia, and hypocalcemia before initiating treatment with amiodarone hydrochloride, as these disorders can exaggerate the degree of QTc prolongation and increase the potential for TdP. Give special attention to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or receiving drugs affecting electrolyte levels, such as diuretics, laxatives, systemic corticosteroids, or amphotericin B.
5.5 Visual Impairment and Loss of Vision
Optic Neuropathy and Optic Neuritis
Cases of optic neuropathy and optic neuritis, usually resulting in visual impairment and sometimes permanent blindness, have been reported in patients treated with amiodarone and may occur at any time during therapy. If symptoms of visual impairment appear, such as changes in visual acuity and decreases in peripheral vision, consider discontinuing Pacerone and promptly refer for ophthalmic examination. Regular ophthalmic examination, including funduscopy and slit-lamp examination, is recommended during administration of Pacerone [see Adverse Reactions (6.1)].
Corneal Microdeposits
Corneal microdeposits appear in the majority of adults treated with amiodarone hydrochloride. They are usually discernible only by slit-lamp examination but give rise to symptoms such as visual halos or blurred vision in as many as 10% of patients. Corneal microdeposits are reversible upon reduction of dose or termination of treatment. Asymptomatic microdeposits alone are not a reason to reduce dose or discontinue treatment [see Adverse Reactions (6.1)].
5.6 Thyroid Abnormalities
Amiodarone hydrochloride inhibits peripheral conversion of thyroxine (T4) to triiodothyronine (T3) and may cause increased thyroxine levels, decreased T3 levels, and increased levels of inactive reverse T3 (rT3) in clinically euthyroid patients. Amiodarone hydrochloride can cause either hypothyroidism (reported in up to 10% of patients) or hyperthyroidism (occurring in about 2% of patients). Monitor thyroid function prior to treatment and periodically thereafter, particularly in elderly patients, and in any patient with a history of thyroid nodules, goiter, or other thyroid dysfunction.
Hyperthyroidism may induce arrhythmia breakthrough. If any new signs of arrhythmia appear, the possibility of hyperthyroidism should be considered. Antithyroid drugs, β-adrenergic blockers, temporary corticosteroid therapy may be necessary to treat the symptoms of hyperthyroidism. The action of antithyroid drugs may be delayed in amiodarone-induced thyrotoxicosis because of substantial quantities of preformed thyroid hormones stored in the gland. Radioactive iodine therapy is contraindicated because of the low radioiodine uptake associated with amiodarone-induced hyperthyroidism. Pacerone-induced hyperthyroidism may be followed by a transient period of hypothyroidism.
Hypothyroidism may be primary or subsequent to resolution of preceding amiodarone-induced hyperthyroidism. Severe hypothyroidism and myxedema coma, sometimes fatal, have been reported in association with amiodarone therapy. In some clinically hypothyroid amiodarone-treated patients, free thyroxine index values may be normal. Manage hypothyroidism by reducing the dose of or discontinuing Pacerone and thyroid hormone supplementation.
5.7 Bradycardia
Pacerone causes symptomatic bradycardia or sinus arrest with suppression of escape foci in 2% to 4% of patients. The risk is increased by electrolytic disorders or use of concomitant antiarrhythmics or negative chronotropes [see Drug Interactions (7)]. Bradycardia may require a pacemaker for rate control.
Post-marketing cases of symptomatic bradycardia, some requiring pacemaker insertion and at least one fatal, have been reported when ledipasvir/sofosbuvir or sofosbuvir with simeprevir were initiated in patients on amiodarone. Bradycardia generally occurred within hours to days, but in some cases presented up to 2 weeks after initiating antiviral treatment. Bradycardia generally resolved after discontinuation of antiviral treatment. The mechanism for this effect is unknown. Monitor heart rate in patients taking or recently discontinuing amiodarone when starting antiviral treatment [see Drug Interactions (7)].
5.8 Implantable Cardiac Devices
In patients with implanted defibrillators or pacemakers, chronic administration of antiarrhythmic drugs may affect pacing or defibrillation thresholds. Therefore, at the inception of and during amiodarone treatment, pacing and defibrillation thresholds should be assessed.
5.9 Fetal Toxicity
Pacerone may cause fetal harm when administered to a pregnant woman. Fetal exposure may increase the potential for cardiac, thyroid, neurodevelopmental, neurological, and growth effects in neonate [see Use in Specific Populations (8.1)].
5.10 Peripheral Neuropathy
Chronic administration of Pacerone may lead to peripheral neuropathy, which may not resolve when Pacerone is discontinued.
5.11 Photosensitivity and Skin Discoloration
Pacerone induces photosensitization in about 10% of patients; some protection may be afforded sun-barrier creams or protective clothing. During long-term treatment, a blue-gray discoloration of the exposed skin may occur. The risk may be increased in patients of fair complexion or those with excessive sun exposure. Some reversal of discoloration may occur upon drug discontinuation.
5.12 Surgery
Volatile Anesthetic Agents
Patients on Pacerone therapy may be more sensitive to the myocardial depressant and conduction effects of halogenated inhalational anesthetics.
- Persistence of Adverse Effects: Adverse reactions and drug interaction can persist for several weeks following discontinuation. (5.1)
- Impaired Vision: Corneal microdeposits (common; reversible), optic neuropathy/neuritis (rare; may lead to blindness). (5.5)
- Thyroid Abnormalities: Hyperthyroidism or hypothyroidism. (5.6)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following serious adverse reactions are described in more detail in other sections of the prescribing information:
- Pulmonary Toxicity [see Warnings and Precautions (5.2)]
- Hepatic Injury [see Warnings and Precautions (5.3)]
- Worsened Arrhythmia [see Warnings and Precautions (5.4)]
- Visual Impairment and Loss of Vision [see Warnings and Precautions (5.5)]
- Thyroid Abnormalities [see Warnings and Precautions (5.6)]
- Bradycardia [see Warnings and Precautions (5.7)]
- Peripheral Neuropathy [see Warnings and Precautions (5.10)]
- Photosensitivity and Skin Discoloration [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
At the usual maintenance dose (400 mg/day) and above, amiodarone hydrochloride causes adverse reactions in about three-fourths of all patients, resulting in discontinuation in 7% to 18%.
In surveys of almost 5,000 patients treated in open U.S. studies and in published reports of treatment with amiodarone hydrochloride, the adverse reactions most frequently requiring discontinuation of amiodarone hydrochloride included pulmonary infiltrates or fibrosis, paroxysmal ventricular tachycardia, congestive heart failure, and elevation of liver enzymes. Other symptoms causing discontinuations less often included visual disturbances, photosensitivity, blue skin discoloration, hyperthyroidism, and hypothyroidism.
The following side-effect rates are based on a retrospective study of 241 patients treated for 2 to 1,515 days (mean 441.3 days):
Thyroid
Common: Hypothyroidism, hyperthyroidism.
Cardiovascular
Common: Congestive heart failure, cardiac arrhythmias, SA node dysfunction.
Gastrointestinal
Very common: Nausea, vomiting.
Common: Constipation, anorexia, abdominal pain.
Dermatologic
Common: Solar dermatitis/photosensitivity.
Neurologic
Common: Malaise and fatigue, tremor/abnormal involuntary movements, lack of coordination, abnormal gait/ataxia, dizziness, paresthesias, decreased libido, insomnia, headache, sleep disturbances.
Ophthalmic
Common: Visual disturbances.
Hepatic
Common: Abnormal liver-function tests, nonspecific hepatic disorders.
Respiratory
Common: Pulmonary inflammation or fibrosis.
Other
Common: Flushing, abnormal taste and smell, edema, abnormal salivation, coagulation abnormalities.
Uncommon: Blue skin discoloration, rash, spontaneous ecchymosis, alopecia, hypotension, and cardiac conduction abnormalities.
6.2 Post-marketing Experience
The following adverse reactions have been identified during post-approval use of amiodarone hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hematologic: hemolytic anemia, aplastic anemia, pancytopenia, neutropenia, thrombocytopenia, agranulocytosis, granuloma.
Immune: anaphylactic/anaphylactoid reaction (including shock), angioedema.
Neurologic: pseudotumor cerebri, parkinsonian symptoms such as akinesia and bradykinesia (sometimes reversible with discontinuation of therapy), demyelinating polyneuropathy.
Psychiatric: hallucination, confusional state, disorientation, delirium.
Cardiac: hypotension (sometimes fatal), sinus arrest.
Respiratory: eosinophilic pneumonia, acute respiratory distress syndrome in the post-operative setting, bronchospasm, bronchiolitis obliterans organizing pneumonia, pulmonary alveolar hemorrhage, pleural effusion, pleuritis.
Gastrointestinal: pancreatitis, acute pancreatitis.
Hepatic: hepatitis, cholestatic hepatitis, cirrhosis.
Skin and Subcutaneous Tissue Disorders: urticaria, toxic epidermal necrolysis (sometimes fatal), erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, bullous dermatitis, drug rash with eosinophilia and systemic symptoms (DRESS), eczema, pruritus, skin cancer, lupus-like syndrome.
Musculoskeletal: myopathy, muscle weakness, rhabdomyolysis.
Renal: renal impairment, renal insufficiency, acute renal failure.
Reproductive: epididymitis, impotence.
Body as a whole: fever, dry mouth.
Endocrine and metabolic: thyroid nodules/ thyroid cancer, syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Vascular: vasculitis.
- The most common reactions (>1%) leading to discontinuation of amiodarone include pulmonary toxicity, paroxysmal ventricular tachycardia, congestive heart failure, and elevation of liver enzymes. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Upsher-Smith Laboratories, LLC at 1-855-899-9180 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS SECTION
7 DRUG INTERACTIONS
Because of amiodarone's long half-life, expect drug interactions to persist for weeks to months after discontinuation of amiodarone.
Drug interactions with amiodarone are described in Table 1 below.
Table 1: Amiodarone Drug Interactions|
Concomitant Drug Class/Name |
Examples |
Clinical Comment |
|---|---|---|
|
Pharmacodynamic Interactions | ||
|
QT Prolonging Drugs |
class I and III antiarrhythmics, lithium, certain phenothiazines, tricyclic antidepressants, certain fluoroquinolone and macrolide antibiotics, azole antifungals, halogenated inhalation anesthetic agents |
Increased risk of Torsade de Pointes. Avoid concomitant use. |
|
Negative Chronotropes |
digoxin, beta blockers, verapamil, diltiazem, clonidine, ivabradine |
Potentiates the electrophysiologic and hemodynamic effects of amiodarone, resulting in bradycardia, sinus arrest, and AV block. Monitor heart rate. |
|
Pharmacokinetic Interactions | ||
|
CYP450 Inhibitors |
grapefruit juice, certain fluoroquinolone and macrolide antibiotics, azole antifungals, cimetidine, certain protease inhibitors |
Increased exposure of amiodarone. Avoid concomitant use. |
|
CYP450 Inducers |
St. John's Wort |
Reduced amiodarone serum levels. |
|
Cyclosporine |
Increased plasma levels of cyclosporine have been reported resulting in elevated creatinine, despite reduction of cyclosporine dose. Monitor cyclosporine drug levels and renal function with concomitant use. | |
|
Cholestyramine |
Reduced amiodarone serum levels. | |
|
Antiarrhythmics |
quinidine, procainamide, flecainide |
Reserve concomitant use for patients who are unresponsive to a single agent. Antiarrhythmic metabolism inhibited by amiodarone. Initiate antiarrhythmic at a lower than usual dose and monitor patient carefully. Reduce dose levels of previously administered antiarrhythmic by 30% to 50% for several days after transitioning to oral amiodarone. Evaluate continued need for antiarrhythmic. |
|
Digoxin |
Increased digoxin concentration. Reduce digoxin by half or discontinue. If continued, monitor for evidence of toxicity. | |
|
HMG-CoA Reductase Inhibitors |
simvastatin, lovastatin, atorvastatin |
Increased plasma concentration of HMG-CoA reductase inhibitor. |
|
Warfarin |
Potentiates anticoagulant response and can result in serious or fatal bleeding. Coadministration increases prothrombin time by 100% after 3 to 4 days. Reduce warfarin dose by one-third to one-half and monitor prothrombin times. | |
|
Phenytoin |
Increased steady-state levels of phenytoin. Monitor phenytoin levels. | |
|
Hepatitis C Direct Acting Antiviral |
sofosbuvir |
Cases of symptomatic bradyarrhythmia requiring pacemaker insertion have been reported in patients on oral maintenance amiodarone who initiated therapy with sofosbuvir. |
|
CYP3A Substrate |
lidocaine |
Sinus bradycardia has been reported with oral amiodarone in combination with lidocaine given for local anesthesia. Monitor heart rate. A lower starting dose of lidocaine may be required. |
|
CYP3A Substrate |
fentanyl |
Fentanyl in combination with amiodarone may cause hypotension, bradycardia, and decreased cardiac output. |
- Avoid coadministration of amiodarone with other antiarrhythmics and drugs known to prolong the QT interval. (7)
- Amiodarone is a substrate for CYP3A and CYP2C8, so inhibitors and inducers affect amiodarone exposure. (7)
- Amiodarone inhibits P-glycoprotein and CYP1A2, CYP2C9, CYP2D6, and CYP3A, increasing exposure to other drugs. (7)
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
Dosage must be individualized based on severity of arrhythmia and response. Use the lowest effective dose. Obtain baseline chest x-ray, pulmonary function tests, thyroid function tests, and liver aminotransferases. Correct hypokalemia, hypomagnesemia, and hypocalcemia before initiating treatment.
Recommended Dosage:
Initiate treatment with a loading dose of 800 to 1600 mg/day until initial therapeutic response occurs (usually 1 to 3 weeks). Once adequate arrhythmia control is achieved, or if side effects become prominent, reduce Pacerone tablet dose to 600 to 800 mg/day for one month and then to the maintenance dose, usually 400 mg/day.
Administration:
Administer Pacerone tablets consistently with regard to meals [see Clinical Pharmacology (12.3)]. Administration of Pacerone tablets in divided doses with meals is suggested for total daily doses of 1000 mg or higher, or when gastrointestinal intolerance occurs.
Initiate treatment with a loading dose of 800 to 1600 mg/day until initial therapeutic response occurs (usually 1 to 3 weeks). Once adequate arrhythmia control is achieved, or if side effects become prominent, reduce Pacerone tablets dose to 600 to 800 mg/day for one month and then to the maintenance dose, usually 400 mg/day. (2)
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Amiodarone hydrochloride was associated with a statistically significant, dose-related increase in the incidence of thyroid tumors (follicular adenoma and/or carcinoma) in rats. The incidence of thyroid tumors was greater than control at the lowest dose level tested, i.e., 5 mg/kg/day (approximately 0.08 times the maximum recommended human maintenance dose2).
Mutagenicity studies (Ames, micronucleus, and lysogenic tests) with amiodarone hydrochloride were negative.
In a study in which amiodarone hydrochloride was administered to male and female rats, beginning 9 weeks prior to mating, reduced fertility was observed at a dose level of 90 mg/kg/day (approximately 1.4 times the maximum recommended human maintenance dose2).
2
600 mg in a 60 kg patient (dose compared on a body surface area basis)
