Ketorolac Tromethamine
mg Rx only
a2b0b02e-a345-44c3-afb8-6b99bf646547
HUMAN PRESCRIPTION DRUG LABEL
Jul 26, 2023
Unit Dose Services
DUNS: 831995316
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Ketorolac Tromethamine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (9)
Drug Labeling Information
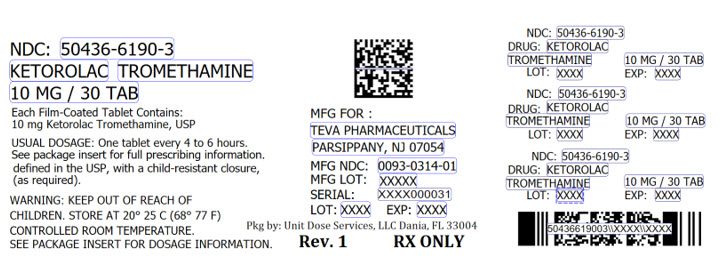
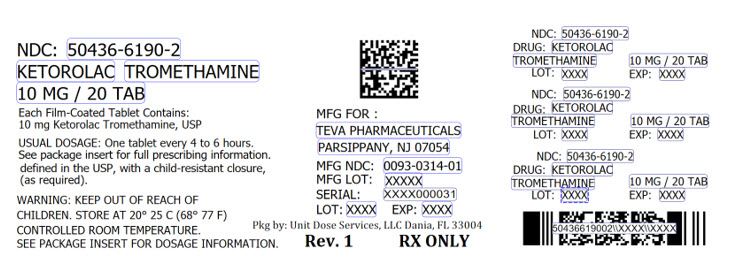
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Package/Label Display Panel
Ketorolac Tromethamine Tablets, USP
10 mg
PHARMACIST: Dispense the accompanying Medication Guide to each patient.
Rx only
BOXED WARNING SECTION
DESCRIPTION SECTION
DESCRIPTION
Ketorolac tromethamine tablets, USP are a member of the pyrrolo-pyrrole group of nonsteroidal anti-inflammatory drugs (NSAIDs). The chemical name for ketorolac tromethamine, USP is (±)-5-benzoyl-2,3-dihydro-1H-pyrrolizine-1-carboxylic acid, compound with 2-amino-2-(hydroxymethyl)-1,3-propanediol (1:1). The structural formula is:

C15H13NO3**.**C4H11NO3 M.W. 376.40
Ketorolac tromethamine, USP is a racemic mixture of [-]S and [+]R ketorolac tromethamine, USP. Ketorolac tromethamine, USP may exist in three crystal forms. All forms are equally soluble in water. Ketorolac tromethamine, USP has a pKa of 3.5 and an n-octanol/water partition coefficient of 0.26.
Ketorolac tromethamine tablets, USP are white, round, convex, unscored, film- coated tablets. Each tablet, for oral administration, contains 10 mg ketorolac tromethamine, USP, the active ingredient. In addition, each tablet contains the following inactive ingredients: hydroxypropyl cellulose, hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, and titanium dioxide.
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
Pharmacodynamics
Ketorolac tromethamine is a nonsteroidal anti-inflammatory drug (NSAID) that exhibits analgesic activity in animal models. The mechanism of action of ketorolac, like that of other NSAIDs, is not completely understood but may be related to prostaglandin synthetase inhibition. The biological activity of ketorolac tromethamine is associated with the S-form. Ketorolac tromethamine possesses no sedative or anxiolytic properties.
The peak analgesic effect of ketorolac tromethamine occurs within 2 to 3 hours and is not statistically significantly different over the recommended dosage range of ketorolac tromethamine. The greatest difference between large and small doses of ketorolac tromethamine is in the duration of analgesia.
Pharmacokinetics
Ketorolac tromethamine is a racemic mixture of [-]S- and [+]R-enantiomeric forms, with the S-form having analgesic activity.
Comparison of IV, IM and Oral Pharmacokinetics
The pharmacokinetics of ketorolac tromethamine, following IV and IM doses of ketorolac tromethamine and oral doses of ketorolac tromethamine, are compared inTable 1. In adults, the extent of bioavailability following administration of the ORAL form of ketorolac tromethamine and the IM form of ketorolac tromethamine was equal to that following an IV bolus.
Linear Kinetics
In adults, following administration of single ORAL doses of ketorolac tromethamine or IM or IV doses of ketorolac tromethamine in the recommended dosage ranges, the clearance of the racemate does not change. This implies that the pharmacokinetics of ketorolac tromethamine in adults, following single or multiple IM or IV doses of ketorolac tromethamine or recommended oral doses of ketorolac tromethamine, are linear. At the higher recommended doses, there is a proportional increase in the concentrations of free and bound racemate.
Absorption
Ketorolac tromethamine is 100% absorbed after oral administration (seeTable 1). Oral administration of ketorolac tromethamine after a high-fat meal resulted in decreased peak and delayed time-to-peak concentrations of ketorolac tromethamine by about 1 hour. Antacids did not affect the extent of absorption.
Distribution
The mean apparent volume (Vß) of ketorolac tromethamine following complete distribution was approximately 13 liters. This parameter was determined from single-dose data. The ketorolac tromethamine racemate has been shown to be highly protein bound (99%). Nevertheless, plasma concentrations as high as 10 mcg/mL will only occupy approximately 5% of the albumin binding sites. Thus, the unbound fraction for each enantiomer will be constant over the therapeutic range. A decrease in serum albumin, however, will result in increased free drug concentrations.
Ketorolac tromethamine is excreted in human milk (seePRECAUTIONS, Nursing Mothers).
Metabolism
Ketorolac tromethamine is largely metabolized in the liver. The metabolic products are hydroxylated and conjugated forms of the parent drug. The products of metabolism, and some unchanged drug, are excreted in the urine.
Excretion
The principal route of elimination of ketorolac and its metabolites is renal. About 92% of a given dose is found in the urine, approximately 40% as metabolites and 60% as unchanged ketorolac. Approximately 6% of a dose is excreted in the feces. A single-dose study with 10 mg ketorolac tromethamine (n = 9) demonstrated that the S-enantiomer is cleared approximately two times faster than the R-enantiomer and that the clearance was independent of the route of administration. This means that the ratio of S/R plasma concentrations decreases with time after each dose. There is little or no inversion of the R- to S- form in humans. The clearance of the racemate in normal subjects, elderly individuals and in hepatically and renally impaired patients is outlined in Table 2 (seeCLINICAL PHARMACOLOGY,Kinetics in Special Populations).
The half-life of the ketorolac tromethamine S-enantiomer was approximately 2.5 hours (SD ± 0.4) compared with 5 hours (SD ± 1.7) for the R-enantiomer. In other studies, the half-life for the racemate has been reported to lie within the range of 5 to 6 hours.
Accumulation
Ketorolac tromethamine administered as an IV bolus every 6 hours for 5 days to healthy subjects (n = 13), showed no significant difference in Cmax on Day 1 and Day 5. Trough levels averaged 0.29 mcg/mL (SD ± 0.13) on Day 1 and 0.55 mcg/mL (SD ± 0.23) on Day 6. Steady state was approached after the fourth dose.
Accumulation of ketorolac tromethamine has not been studied in special populations (geriatric, pediatric, renal failure or hepatic disease patients).
Kinetics in Special Populations
Geriatric Patients
Based on single-dose data only, the half-life of the ketorolac tromethamine racemate increased from 5 to 7 hours in the elderly (65 to 78 years) compared with young healthy volunteers (24 to 35 years) (see Table 2). There was little difference in the Cmax for the two groups (elderly, 2.52 mcg/mL ± 0.77; young, 2.99 mcg/mL ± 1.03) (seePRECAUTIONS,Geriatric Use (≥ 65 Years of Age)).
Pediatric Patients
Limited information is available regarding the pharmacokinetics of dosing of ketorolac tromethamine in the pediatric population. Following a single intravenous bolus dose of 0.5 mg/kg in 10 children 4 to 8 years old, the half- life was 5.8 ± 1.6 hours, the average clearance was 0.042 ± 0.01 L/hr/kg, the volume of distribution during the terminal phase (Vβ) was 0.34 ± 0.12 L/kg and the volume of distribution at steady state (Vss) was 0.26 ± 0.08 L/kg. The volume of distribution and clearance of ketorolac in pediatric patients was higher than those observed in adult subjects (see Table 1). There are no pharmacokinetic data available for administration of ketorolac tromethamine by the IM route in pediatric patients.
Renal Insufficiency
Based on single-dose data only, the mean half-life of ketorolac tromethamine in renally impaired patients is between 6 and 19 hours and is dependent on the extent of the impairment. There is poor correlation between creatinine clearance and total ketorolac tromethamine clearance in the elderly and populations with renal impairment (r = 0.5).
In patients with renal disease, the AUC∞ of each enantiomer increased by approximately 100% compared with healthy volunteers. The volume of distribution doubles for the S-enantiomer and increases by 1/5th for the R-enantiomer. The increase in volume of distribution of ketorolac tromethamine implies an increase in unbound fraction.
The AUC∞-ratio of the ketorolac tromethamine enantiomers in healthy subjects and patients remained similar, indicating there was no selective excretion of either enantiomer in patients compared to healthy subjects (seeWARNINGS, Renal Effects).
Hepatic Insufficiency
There was no significant difference in estimates of half-life, AUC∞ and Cmax in 7 patients with liver disease compared to healthy volunteers (see PRECAUTIONS,Hepatic Effect and Table 2).
Race
Pharmacokinetic differences due to race have not been identified.
Table 1: Table of Approximate Average Pharmacokinetic Parameters (Mean ± SD) Following Oral, Intramuscular and Intravenous Doses of Ketorolac Tromethamine|
Pharmacokinetic Parameters (units) |
Oral1 |
Intramuscular2 |
Intravenous Bolus3 | |||
|
10 mg |
15 mg |
30 mg |
60 mg |
15 mg |
30 mg | |
|
Bioavailability (extent) |
100% | |||||
|
Tmax6 (min) |
44 ± 34 |
33 ± 214 |
44 ± 29 |
33 ± 214 |
1.1 ± 0.74 |
2.9 ± 1.8 |
|
Cmax7 (mcg/mL) [single-dose] |
0.87 ± 0.22 |
1.14 ± 0.324 |
2.42 ± 0.68 |
4.55 ± 1.274 |
2.47 ± 0.514 |
4.65 ± 0.96 |
|
Cmax (mcg/mL) [steady state qid] |
1.05 ± 0.264 |
1.56 ± 0.444 |
3.11 ± 0.874 |
N/A5 |
3.09 ± 1.174 |
6.85 ± 2.61 |
|
Cmin8 (mcg/mL) [steady state qid] |
0.29 ± 0.074 |
0.47 ± 0.134 |
0.93 ± 0.264 |
N/A |
0.61 ± 0.214 |
1.04 ± 0.35 |
|
Cavg9 (mcg/mL) [steady state qid] |
0.59 ± 0.204 |
0.94 ± 0.294 |
1.88 ± 0.594 |
N/A |
1.09 ± 0.304 |
2.17 ± 0.59 |
|
Vβ10 (L/kg) |
0.175 ± 0.039 |
0.210 ±0.044 | ||||
|
% Dose metabolized ≤ 50 |
% Dose excreted in feces = 6 | |||||
|
% Dose excreted in urine = 91 |
% Plasma protein binding = 99 | |||||
|
1. Derived from PO pharmacokinetic studies in 77 normal fasted volunteers 2. Derived from IM pharmacokinetic studies in 54 normal volunteers 3. Derived from IV pharmacokinetic studies in 24 normal volunteers 4. Mean value was simulated from observed plasma concentration data and standard deviation was simulated from percent coefficient of variation for observed Cmax and Tmax data 5. Not applicable because 60 mg is only recommended as a single dose 6. Time-to-peak plasma concentration 7. Peak plasma concentration 8. Trough plasma concentration 9. Average plasma concentration 10. Volume of distribution |
|
**Total Clearance [in L/h/kg]**3 |
Terminal Half-Life [in hours] | |||
|
Type of Subjects |
IM |
ORAL |
IM |
ORAL |
|
Mean (range) |
Mean (range) |
Mean (range) |
Mean (range) | |
|
Normal Subjects IM (n = 54) mean age = 32, range = 18 to 60 Oral (n = 77) mean age = 32, range = 20 to 60 |
0.023 |
0.025 |
5.3 |
5.3 |
|
(0.010 to 0.046) |
(0.013 to 0.050) |
(3.5 to 9.2) |
(2.4 to 9) | |
|
Healthy Elderly Subjects IM (n = 13), Oral (n = 12) mean age = 72, range = 65 to 78 |
0.019 |
0.024 |
7 |
6.1 |
|
(0.013 to 0.034) |
(0.018 to 0.034) |
(4.7 to 8.6) |
(4.3 to 7.6) | |
|
Patients With Hepatic Dysfunction IM and Oral (n = 7) mean age = 51, range = 43 to 64 |
0.029 |
0.033 |
5.4 |
4.5 |
|
(0.013 to 0.066) |
(0.019 to 0.051) |
(2.2 to 6.9) |
(1.6 to 7.6) | |
|
Patients With Renal Impairment IM (n = 25), Oral (n = 9) serum creatinine = 1.9 to 5 mg/dL, mean age (IM) = 54, range = 35 to 71 mean age (Oral) = 57, range = 39 to 70 |
0.015 |
0.016 |
10.3 |
10.8 |
|
(0.005 to 0.043) |
(0.007 to 0.052) |
(5.9 to 19.2) |
(3.4 to 18.9) | |
|
Renal Dialysis Patients IM and Oral (n = 9) mean age = 40, range = 27 to 63 |
0.016 |
-- |
13.6 |
-- |
|
(0.003 to 0.036) |
(8 to 39.1) | |||
|
1. Estimated from 30 mg single IM doses of ketorolac tromethamine | ||||
|
2. Estimated from 10 mg single oral doses of ketorolac tromethamine | ||||
|
3. Liters/hour/kilogram |
IV Administration
In normal adult subjects (n = 37), the total clearance of 30 mg IV- administered ketorolac tromethamine was 0.030 (0.017 to 0.051) L/h/kg. The terminal half-life was 5.6 (4 to 7.9) hours (seeKinetics in Special Populations for use of IV dosing of ketorolac tromethamine in pediatric patients).
CLINICAL STUDIES SECTION
CLINICAL STUDIES
Adult Patients
In a postoperative study, where all patients received morphine by a PCA device, patients treated with ketorolac tromethamineIV as fixed intermittent boluses (e.g., 30 mg initial dose followed by 15 mg q3h), required significantly less morphine (26%) than the placebo group. Analgesia was significantly superior, at various postdosing pain assessment times, in the patients receiving ketorolac tromethamineIV plus PCA morphine as compared to patients receiving PCA-administered morphine alone.
Pediatric Patients
There are no data available to support the use of ketorolac tromethamine tablets in pediatric patients.
HOW SUPPLIED SECTION
HOW SUPPLIED
Ketorolac tromethamine tablets, USP are available as follows:
10 mg: White, round, convex, unscored, film-coated tablets, debossed "93" on one side and "314" on the other side. They are available in bottles of 100 tablets (NDC 0093-0314-01).
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
PROTECT FROM LIGHT AND EXCESSIVE HUMIDITY.
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
Dispense with Medication Guide available at: www.tevausa.com/medguides
Manufactured For:
Teva Pharmaceuticals
****Parsippany, NJ 07054
Rev. N 7/2021
SPL MEDGUIDE SECTION
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
|
Dispense with Medication Guide available at: www.tevausa.com/medguides | |
|
What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)? | |
|
NSAIDs can cause serious side effects, including: | |
|
***Increased risk of a heart attack or stroke that can lead to death.**This risk may happen early in treatment and may increase:
| |
|
Do not take NSAIDs right before or after a heart surgery called a “coronary artery bypass graft (CABG).” | |
|
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack. | |
|
*Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
| |
|
The risk of getting an ulcer or bleeding increases with: | |
| |
| |
|
|
|
|
|
|
|
|
|
NSAIDs should only be used: | |
| |
| |
| |
|
What are NSAIDs? | |
|
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain. | |
|
Who should not take NSAIDs? | |
|
Do not take NSAIDs: | |
| |
| |
|
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you: | |
| |
| |
| |
| |
| |
|
Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects.Do not start taking any new medicine without talking to your healthcare provider first. | |
|
What are the possible side effects of NSAIDs? | |
|
NSAIDs can cause serious side effects, including: | |
|
See “What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?” | |
|
|
|
|
|
|
| |
|
*Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness. | |
|
Get emergency help right away if you get any of the following symptoms: | |
|
|
|
|
| |
|
Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms: | |
|
|
|
|
|
is black and sticky like tar |
|
|
|
|
|
|
| |
|
If you take too much of your NSAID, call your healthcare provider or get medical help right away. | |
|
These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs. | |
|
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |
|
Other information about NSAIDs | |
| |
| |
|
General information about the safe and effective use of NSAIDs | |
|
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them. | |
|
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals. | |
|
This Medication Guide has been approved by the U.S. Food and Drug Administration. |
Manufactured For:
Teva Pharmaceuticals
****Parsippany, NJ 07054
Rev. B 7/2021
