Paroxetine
These highlights do not include all the information needed to use safely and effectively. See full prescribing information for . Initial U.S. Approval: 1992
1383d713-79b9-45bd-bd06-65707f28bc99
HUMAN PRESCRIPTION DRUG LABEL
Sep 1, 2023
Padagis US LLC
DUNS: 967694121
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
paroxetine
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (10)
Drug Labeling Information
WARNINGS AND PRECAUTIONS SECTION
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behaviors
Paroxetine capsules are not approved for any psychiatric condition.
Antidepressants, including those that contain an SSRI, increase the risk of suicidal thinking and behavior (suicidality) in pediatric and young adult patients when used to treat major depressive disorder (MDD) and other psychiatric disorders. There is limited information regarding suicidality in women who use paroxetine capsules for treatment of VMS. The paroxetine capsule trials excluded women with a presence or history of previous psychiatric disorders.
Consider discontinuing paroxetine capsules in patients with worsening depression or those who experience emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
All patients being treated with paroxetine capsules should be observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of treatment.
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania have been reported in patients being treated with antidepressants for MDD as well as for other psychiatric and nonpsychiatric indications. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Families and caregivers of patients being treated with paroxetine capsules should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers.
5.2 Serotonin Syndrome
Paroxetine capsules can precipitate serotonin syndrome, a potentially life- threatening condition. The risk is increased with concomitant use of other serotonergic agents (including triptans, tricyclic antidepressants, fentanyl, tramadol, meperidine, methadone, lithium, tryptophan, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e., monoamine oxidase inhibitors (MAOIs) [see Contraindications (4), Drug Interactions (7.3)]. Serotonin syndrome can also occur when these drugs are used alone.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Monitor patients for the emergence of serotonin syndrome.
The concomitant use of paroxetine capsules with MAOIs is contraindicated. Do not start paroxetine capsules in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking paroxetine capsules. Paroxetine capsules should be discontinued before initiating treatment with the MAOI [see Contraindications (4.1) and Dosage and Administration (2.2)].
If concomitant use of paroxetine capsules with other serotonergic drugs (e.g., triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort) is clinically warranted, consider the increased risk of serotonin syndrome and carefully observe the patient, particularly during treatment initiation [see Contraindications (4.1) Drug Interactions (7.3)].
Discontinue paroxetine capsules and any concomitant serotonergic agents immediately if the above events occur and initiate supportive symptomatic treatment.
5.3 Potential Impact on Tamoxifen Efficacy
It is uncertain whether the co-administration of paroxetine and tamoxifen has a significant adverse effect on the efficacy of tamoxifen. Some studies have shown that the efficacy of tamoxifen, as measured by the risk of breast cancer relapse/mortality, may be reduced when co-prescribed with paroxetine as a result of paroxetine’s irreversible inhibition of CYP2D6 [see Drug Interactions (7.1)]. However, other studies have failed to demonstrate such a risk. When tamoxifen is used for the treatment or prevention of breast cancer, weigh the likely benefit of paroxetine capsules for treating VMS vs. the risk of possible decreased tamoxifen effectiveness, and consider avoiding the concomitant use of paroxetine capsules for VMS treatment.
5.4 Abnormal Bleeding
SSRIs, including paroxetine capsules, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs have ranged from ecchymosis, hematoma, epistaxis, and petechiae to life-threatening hemorrhages. Caution patients about the risk of bleeding associated with the concomitant use of paroxetine capsules and NSAIDs, aspirin, or other drugs that affect coagulation [see Drug Interactions (7.1)].
5.5 Angle-Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressants and paroxetine capsules may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.6 Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs, including paroxetine capsules. Elderly patients may be at greater risk. In many cases, the hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported in patients using SSRIs. Also, patients taking diuretics or who are volume-depleted can be at greater risk. Consider discontinuation of paroxetine capsules in patients with symptomatic hyponatremia and institute appropriate medical intervention.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which can lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.7 Bone Fracture
Epidemiological studies on bone fracture risk following exposure to SSRIs have reported an association between SSRI treatment and fractures. It is unknown to what extent fracture risk is directly attributable to SSRI treatment. If a paroxetine capsule-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising, consider the possibility of a fragility fracture.
5.8 Screening Patients for Bipolar Disorder and Monitoring for
Mania/Hypomania
Paroxetine capsules are only indicated for the treatment of moderate to severe VMS and are not approved for use in treating either depression or bipolar depression. However, prior to initiating treatment with paroxetine capsules, all patients should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It is generally believed (though not established in controlled trials) that use of an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder.
5.9 Seizures
In premarketing testing of paroxetine, seizures occurred in 0.1% of paroxetine-treated patients. Use paroxetine capsules cautiously in patients with a history of seizures or with conditions that potentially lower the seizure threshold. Evaluate and consider discontinuing use in any patient who develops seizures.
5.10 Akathisia
The use of paroxetine or other SSRIs has been associated with the development of akathisia, which is characterized by an inner sense of restlessness and psychomotor agitation such as an inability to sit or stand still usually associated with subjective distress. This is most likely to occur within the first few weeks of treatment. Discontinue treatment with paroxetine capsules if akathisia occurs.
5.11 Potential for Cognitive and Motor Impairment
Paroxetine capsules have the potential to impair judgment, thinking, or motor skills. Patients should be cautioned about operating hazardous machinery, including motor vehicles, until they are reasonably certain that the drug treatment does not affect them adversely.
5.12 Sexual Dysfunction
Use of SSRIs, including paroxetine capsules, may cause symptoms of sexual dysfunction. In female patients, SSRI/SNRI use may result in decreased libido and delayed or absent orgasm.
It is important for prescribers to inquire about sexual function prior to initiation of paroxetine capsules and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported. When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including the underlying psychiatric disorder. Discuss potential management strategies to support patients in making informed decisions about treatment.
•
Suicidality: Monitor for suicidality or unusual changes in behavior (5.1)
•
Serotonin Syndrome: Paroxetine capsules can cause serotonin syndrome with increased risk when co-administered with other serotonergic agents, but also when taken alone. If it occurs, discontinue paroxetine capsules and serotonergic agents and initiate supportive measures (5.2, 7.3)
•
Tamoxifen: Efficacy of tamoxifen may be reduced when administered concomitantly with paroxetine capsules (5.3, 7.1)
•
Abnormal Bleeding: Caution patients about the risk of bleeding associated with the concomitant use of paroxetine capsules and non-steroidal anti-inflammatory drugs (NSAIDs), aspirin, or other drugs that affect coagulation (5.4, 7.1)
•
Angle-Closure Glaucoma: Angle closure glaucoma has occurred in patients who have untreated anatomically narrow angles and who are treated with antidepressants (5.5)
•
Hyponatremia: Can occur in association with syndrome of inappropriate antidiuretic hormone secretion (SIADH) (5.6)
•
Bone Fracture: Epidemiological studies have reported an association between SSRI treatment and fractures (5.7)
•
Activation of Mania/Hypomania: Screen for bipolar disorder and monitor for mania/hypomania (5.8)
•
Seizures: Use cautiously in patients with a history of seizures or with conditions that potentially lower the seizure threshold (5.9)
•
Akathisia: Can occur, most likely in the first few weeks of treatment (5.10)
•
Cognitive and Motor Impairment: May cause impairment; patients should not operate machinery or motor vehicles until certain that paroxetine capsules do not affect them adversely (5.11)
•
Sexual Dysfunction: paroxetine capsule use may cause symptoms of sexual dysfunction. (5.12)
DESCRIPTION SECTION
11 DESCRIPTION
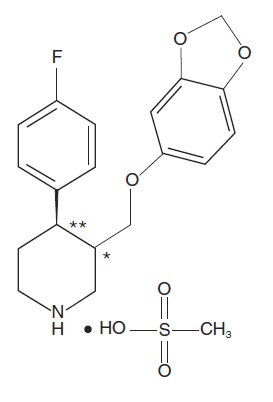
Paroxetine is an orally administered selective serotonin reuptake inhibitor (SSRI) for the treatment of moderate to severe VMS associated with menopause. It is identified chemically as (-)-trans -4R- (4’-fluorophenyl) - 3S - [(3’,4’-methylenedioxyphenoxy) methyl] piperidine mesylate and has the empirical formula of C19H20FNO3•CH3SO3H.
The molecular weight is 425.5 (329.4 as free base). The structural formula is:
The mesylate salt of paroxetine is an odorless, off-white powder, having a melting point range of 147° to 150°C and a solubility of more than 1 g/mL in water.
Each pink capsule contains 9.69 mg paroxetine mesylate equivalent to 7.5 mg paroxetine base.
Inactive ingredients consist of: dibasic calcium phosphate, sodium starch glycolate, magnesium stearate, gelatin, titanium dioxide, FD&C Yellow #6, FD&C Red #3, FD&C Red #40, shellac, and black iron oxide.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year carcinogenicity studies were conducted in rodents given paroxetine in the diet at 1, 5, and 25 mg/kg/day (mice) and 1, 5, and 20 mg/kg/day (rats). The doses used in these carcinogenicity studies were approximately 16 (mouse) and 26 (rat) times the MHRD for VMS. There was a significantly greater number of male rats in the high-dose group with reticulum cell sarcomas (1/100, 0/50, 0/50, and 4/50 for control, low-, middle-, and high-dose groups, respectively) and a significantly increased linear trend across groups for the occurrence of lymphoreticular tumors in male rats. Female rats were not affected. Although there was a dose-related increase in the number of tumors in mice, there was no drug-related increase in the number of mice with tumors. The relevance of these findings to humans is unknown.
Mutagenesis
Paroxetine produced no genotoxic effect in a battery of 5 in vitro and 2 in vivo assays that included the following: bacterial mutation assay, mouse lymphoma mutation assay, unscheduled DNA synthesis assay, and tests for cytogenetic aberrations in vivo in mouse bone marrow and in vitro in human lymphocytes and in a dominant lethal test in rats.
Impairment of Fertility
A reduced pregnancy rate was found in reproduction studies in rats at a paroxetine dose of 15 mg/kg/day, which is 19 times the MRHD for VMS on an mg/m2 basis. Irreversible lesions occurred in the reproductive tract of male rats after dosing in toxicity studies for 2 to 52 weeks. These lesions consisted of vacuolation of epididymal tubular epithelium at 50 mg/kg/day and atrophic changes in the seminiferous tubules of the testes with arrested spermatogenesis at 25 mg/kg/day (65 times and 32 times the MHRD for VMS on an mg/m2 basis, respectively).
CLINICAL STUDIES SECTION
14 CLINICAL STUDIES
The efficacy of paroxetine capsules as a treatment for moderate to severe VMS associated with menopause was established in two Phase 3 studies (at a dose of 7.5 mg once daily at bedtime) in 1174 postmenopausal women with a minimum of 7-8 moderate to severe vasomotor symptoms per day at baseline (≥ 50 per week) for 30 days prior to receiving study drug.
Study 1 was a 12-week, randomized, double-blind, placebo-controlled clinical trial with a total of 606 postmenopausal women (average age 55 years, 65% Caucasian and 33% African American, 18% surgically menopausal and 82% naturally menopausal).
Study 2 was a 24-week, randomized, double-blind, placebo-controlled clinical trial with a total of 568 postmenopausal women (average age 54 years, 76% Caucasian and 22% African American, 20% surgically menopausal and 81% naturally menopausal).
The co-primary efficacy endpoints for both studies were the reduction from baseline in VMS frequency and severity at Weeks 4 and 12. Data from Study 1 showed a statistically significant reduction from baseline in the frequency of moderate to severe vasomotor symptoms at Week 4 and Week 12 and a statistically significant reduction in the severity of moderate to severe VMS at Week 4 for paroxetine capsules compared to placebo (Table 4). Data from Study 2 showed a statistically significant reduction from baseline in the frequency and severity of moderate to severe vasomotor symptoms at Week 4 and Week 12 for paroxetine capsules compared to placebo (Table 5).
Table 4
Study 1: Changes in the Daily Frequency and Daily Severity of Moderate to Severe VMS at Weeks 4 and 12 (MITT Population)
|
Frequency |
Severity | |||
|
Paroxetine Capsules |
Placebo |
Paroxetine Capsules |
Placebo | |
|
Baseline | ||||
|
n Median |
301 10.4 |
305 10.4 |
301 2.5 |
305 2.5 |
|
Change from baseline at Week 4 | ||||
|
n Median Treatment Difference* P-value# |
289 -4.3 -1.2 <0.01 |
293 -3.1 |
281 -0.05 -0.05 <0.01 |
289 0.00 |
|
Change from baseline at Week 12 | ||||
|
n Median Treatment Difference* P-value# |
264 -5.9 -0.9 <0.01 |
274 -5.0 |
236 -0.06 -0.04 0.17 |
253 -0.02 |
MITT population: all consented and randomized subjects with valid baseline daily hot flash diary data who had taken at least 1 dose of study medication and had at least 1 day of on-treatment daily hot flash diary data.
- Treatment Difference: the difference between the median changes from baseline.
#P-value is obtained from rank-ANCOVA model.
Table 5
Study 2: Changes in the Daily Frequency and Daily Severity of Moderate to Severe VMS at Weeks 4 and 12 (MITT Population)
|
Frequency |
Severity | |||
|
Paroxetine Capsules |
Placebo |
Paroxetine Capsules |
Placebo | |
|
Baseline | ||||
|
n Median |
284 9.9 |
284 9.6 |
284 2.5 |
284 2.5 |
|
Change from baseline at Week 4 | ||||
|
n Median Treatment Difference* P-value# |
276 -3.8 -1.3 <0.01 |
274 -2.5 |
268 -0.04 -0.03 0.04 |
271 -0.01 |
|
Change from baseline at Week 12 | ||||
|
n Median Treatment Difference* P-value# |
257 -5.6 -1.7 <0.01 |
244 -3.9 |
245 -0.05 -0.05 <0.01 |
236 0.00 |
MITT population: all consented and randomized subjects with valid baseline daily hot flash diary data who had taken at least 1 dose of study medication and had at least 1 day of on-treatment daily hot flash diary data.
- Treatment Difference: the difference between the median changes from baseline.
#P-value is obtained from rank-ANCOVA model.
Persistence of benefit at 24 weeks in Study 2 was evaluated with a responder analysis where responders were defined as those patients who achieved ≥ 50% reduction from baseline in the frequency of moderate to severe VMS at Week 24. The proportion of patients achieving a ≥ 50% reduction in the frequency of moderate to severe VMS from baseline to Week 24 was 48% in the paroxetine capsules group and 36% in the placebo group at Week 24.
