Metoclopramide
These highlights do not include all the information needed to use METOCLOPRAMIDE TABLETS safely and effectively. See full prescribing information for METOCLOPRAMIDE TABLETS. METOCLOPRAMIDE tablets, for oral use Initial U.S. Approval: 1979
4ab8ddab-8226-4b5a-8774-308ed49d6bc4
HUMAN PRESCRIPTION DRUG LABEL
Feb 27, 2023
NCS HealthCare of KY, LLC dba Vangard Labs
DUNS: 050052943
Products 2
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
Metoclopramide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Metoclopramide
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (6)
Drug Labeling Information
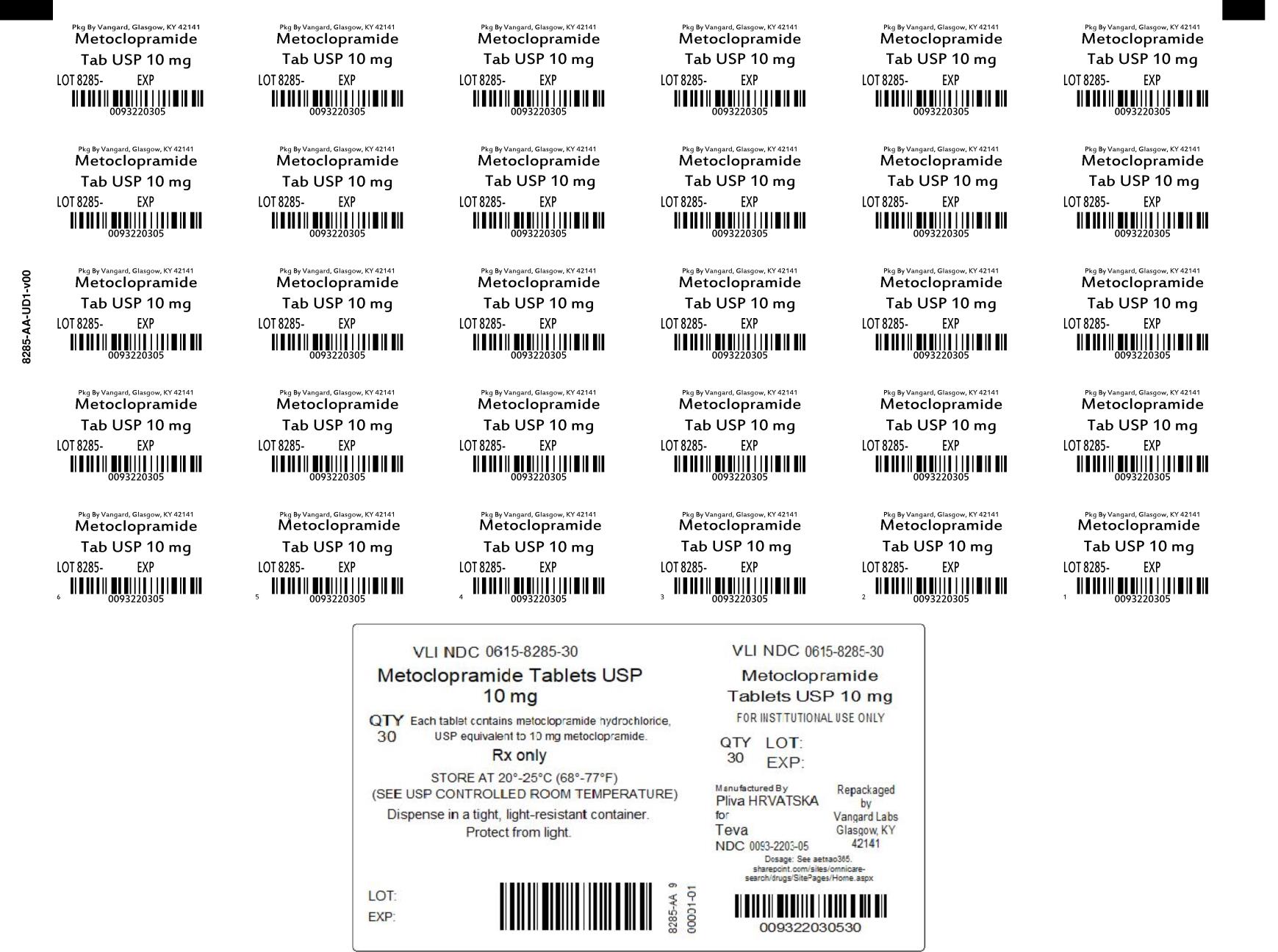
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL 10 MG UNIT DOSE
INDICATIONS & USAGE SECTION
1 INDICATIONS AND USAGE
Metoclopramide tablets are indicated for the:
- Treatment for 4 to 12 weeks of symptomatic, documented gastroesophageal reflux in adults who fail to respond to conventional therapy.
- Relief of symptoms in adults with acute and recurrent diabetic gastroparesis.
Limitations of Use:
Metoclopramide tablets are not recommended for use in pediatric patients due to the risk of developing tardive dyskinesia (TD) and other extrapyramidal symptoms as well as the risk of methemoglobinemia in neonates [see Use in Specific Populations (8.4)].
Metoclopramide tablets are indicated for the:
- Treatment for 4 to 12 weeks of symptomatic, documented gastroesophageal reflux in adults who fail to respond to conventional therapy. (1)
- Relief of symptoms in adults with acute and recurrent diabetic gastroparesis. (1)
Limitations of Use:
Metoclopramide tablets are not recommended for use in pediatric patients due to the risk of tardive dyskinesia (TD) and other extrapyramidal symptoms as well as the risk of methemoglobinemia in neonates. (1) (8.4)
ADVERSE REACTIONS SECTION
6 ADVERSE REACTIONS
The following adverse reactions are described, or described in greater detail, in other sections of the labeling:
- Tardive dyskinesia [see Boxed Warning and Warnings and Precautions (5.1)]
- Other extrapyramidal effects [see Warnings and Precautions (5.2)]
- Neuroleptic malignant syndrome [see Warnings and Precautions (5.3)]
- Depression [see Warnings and Precautions (5.4)]
- Hypertension [see Warnings and Precautions (5.5)]
- Fluid retention [see Warnings and Precautions (5.6)]
- Hyperprolactinemia [see Warnings and Precautions (5.7)]
- Effects on the ability to drive and operate machinery [see Warnings and Precautions (5.8)]
The following adverse reactions have been identified from clinical studies or postmarketing reports of metoclopramide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The most common adverse reactions (in approximately 10% of patients receiving 10 mg of metoclopramide four times daily) were restlessness, drowsiness, fatigue, and lassitude. In general, the incidence of adverse reactions correlated with the dosage and duration of metoclopramide administration.
Adverse reactions, especially those involving the nervous system, occurred after stopping metoclopramide including dizziness, nervousness, and headaches.
Central Nervous System Disorders
- Tardive dyskinesia, acute dystonic reactions, drug-induced parkinsonism, akathisia, and other extrapyramidal symptoms
- Convulsive seizures
- Hallucinations
- Restlessness, drowsiness, fatigue, and lassitude occurred in approximately 10% of patients who received 10 mg four times daily. Insomnia, headache, confusion, dizziness, or depression with suicidal ideation occurred less frequently.
- Neuroleptic malignant syndrome, serotonin syndrome (in combination with serotonergic agents).
Endocrine Disorders: Fluid retention secondary to transient elevation of aldosterone. Galactorrhea, amenorrhea, gynecomastia, impotence secondary to hyperprolactinemia
Cardiovascular Disorders: Acute congestive heart failure, possible atrioventricular block, hypotension, hypertension, supraventricular tachycardia, bradycardia, fluid retention
Gastrointestinal Disorders: Nausea, bowel disturbances (primarily diarrhea)
Hepatic Disorders: Hepatotoxicity, characterized by, e.g., jaundice and altered liver function tests, when metoclopramide was administered with other drugs with known hepatotoxic potential
Renal and Urinary Disorders: Urinary frequency, urinary incontinence
Hematologic Disorders: Agranulocytosis, neutropenia, leukopenia, methemoglobinemia, sulfhemoglobinemia
Hypersensitivity Reactions: Bronchospasm (especially in patients with a history of asthma), urticaria; rash; angioedema, including glossal or laryngeal edema
Eye Disorders: Visual disturbances
Metabolism Disorders: Porphyria
- Most common adverse reactions (>10%) are restlessness, drowsiness, fatigue, and lassitude. (6)
To report SUSPECTED ADVERSE REACTIONS, contact TEVA at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DOSAGE & ADMINISTRATION SECTION
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Avoid treatment with metoclopramide for longer than 12 weeks because of the increased risk of developing TD with longer-term use [see Dosage and Administration (2.2, 2.3), Warnings and Precautions (5.1)].
2.2 Dosage for Gastroesophageal Reflux
Metoclopramide tablets may be administered continuously or intermittently in patients with symptomatic gastroesophageal reflux who fail to respond to conventional therapy:
Continuous Dosing
The recommended adult dosage of metoclopramide is 10 to 15 mg four times daily for 4 to 12 weeks. The treatment duration is determined by endoscopic response. Administer the dosage thirty minutes before each meal and at bedtime. The maximum recommended daily dosage is 60 mg.
Table 1 displays the recommended daily dosage and maximum daily dosage for adults and dosage adjustments for patients with moderate or severe hepatic impairment (Child-Pugh B or C), in patients with creatinine clearance less than 60 mL/minute, in cytochrome P450 2D6 (CYP2D6) poor metabolizers, and with concomitant use with strong CYP2D6 inhibitors.
Intermittent Dosing
If symptoms only occur intermittently or at specific times of the day, administer metoclopramide in single dose up to 20 mg prior to the provoking situation. Consider dosage reductions for the populations and situations in Table 1.
Table 1. Recommended Metoclopramide Tablet Dosage in Patients with Gastroesophageal Reflux|
1 Elderly patients may be more sensitive to the therapeutic or adverse effects of metoclopramide; therefore, consider a lower starting dosage of 5 mg four times daily with titration to the recommended adult dosage of 10 to 15 mg four times daily based upon response and tolerability. | ||
|
Recommended Dosage |
Maximum Recommended Daily Dosage | |
|
Adult patients |
10 to 15 mg four times daily (thirty minutes before each meal and at bedtime) |
60 mg |
|
Mild hepatic impairment (Child-Pugh A) | ||
|
Elderly patients [see Use in Specific Populations (8.5)] |
5 mg1 four times daily (thirty minutes before each meal and at bedtime) | |
|
Moderate or severe hepatic impairment (Child-Pugh B or C) [see Use in Specific Populations (8.7)] |
5 mg four times daily (thirty minutes before each meal and at bedtime), or 10 mg taken three times daily |
30 mg |
|
CYP2D6 poor metabolizers [see Use in Specific Populations (8.9)] | ||
|
Concomitant use with strong CYP2D6 inhibitors (e.g., quinidine, bupropion, fluoxetine, and paroxetine) [see Drug Interactions (7.1)] | ||
|
Moderate or severe renal impairment (creatinine clearance less than or equal to 60 mL/minute) [see Use in Specific Populations (8.6)] | ||
|
Patients with End-Stage Renal Disease (ESRD) including those treated with hemodialysis and continuous ambulatory peritoneal dialysis [see Use in Specific Populations (8.6)] |
5 mg four times daily (thirty minutes before each meal and at bedtime) or 10 mg twice daily |
20 mg |
2.3 Dosage for Acute and Recurrent Diabetic Gastroparesis
The recommended adult dosage for the treatment of acute and recurrent diabetic gastroparesis is 10 mg four times daily for 2 to 8 weeks, depending on symptomatic response. Avoid metoclopramide treatment for greater than 12 weeks [see Warnings and Precautions (5.1)]. Administer the dosage thirty minutes before each meal and at bedtime. The maximum recommended daily dosage is 40 mg.
Table 2 displays the recommended daily dosage and maximum daily dosage for adults and dosage adjustments for patients with moderate or severe hepatic impairment (Child-Pugh B or C), in patients with creatinine clearance less than 60 mL/minute, in cytochrome P450 2D6 (CYP2D6) poor metabolizers, and with concomitant use with strong CYP2D6 inhibitors.
If patients with diabetic gastroparesis have severe nausea or vomiting and are unable to take oral metoclopramide tablets, consider starting therapy with metoclopramide injection given intramuscularly or intravenously for up to 10 days (see the prescribing information for metoclopramide injection). After patients are able to take oral therapy, switch to metoclopramide tablets.
Table 2. Recommended Metoclopramide Tablet Dosage in Patients with Acute and Recurrent Diabetic Gastroparesis|
1 Elderly patients may be more sensitive to the therapeutic or adverse effects of metoclopramide; therefore, consider a lower dosage of 5 mg four times daily with titration to the recommended adult dosage of 10 mg four times daily based upon response and tolerability. | ||
|
Recommended Dosage |
Maximum Recommended Daily Dosage | |
|
Adult Patients |
10 mg four times daily (30 minutes before each meal and at bedtime) |
40 mg |
|
Mild hepatic impairment (Child-Pugh A) | ||
|
Elderly patients [see Use in Specific Populations (8.5)] |
5 mg1 four times daily (30 minutes before each meal and at bedtime) | |
|
Moderate or severe hepatic impairment (Child-Pugh B or C) [see Use in Specific Populations (8.7)] |
5 mg four times daily (30 minutes before each meal and at bedtime) |
20 mg |
|
CYP2D6 poor metabolizers [see Use in Specific Populations (8.9)] | ||
|
Concomitant use with strong CYP2D6 inhibitors (e.g., quinidine, bupropion, fluoxetine, and paroxetine) [see Drug Interactions (7.1)] | ||
|
Moderate or severe renal impairment (creatinine clearance less than 60 mL/minute) [see Use in Specific Populations (8.6)] | ||
|
Patients with End-Stage Renal Disease (ESRD) including those treated with hemodialysis and continuous ambulatory peritoneal dialysis [see Use in Specific Populations (8.6)] |
5 mg twice daily |
10 mg |
Gastroesophageal Reflux (2.2)
- Administer metoclopramide continuously or intermittently:
- Continuous: Administer 10 to 15 mg, 30 minutes before each meal and at bedtime (maximum of 60 mg per day) for 4 to 12 weeks.
- Intermittent: Single doses up to 20 mg prior to provoking situation.
Acute and Recurrent Diabetic Gastroparesis (2.3)
- Administer 10 mg, 30 minutes before each meal and at bedtime (maximum of 40 mg per day) for 2 to 8 weeks
Dosage Adjustment in Specific Populations (2.2, 2.3)
- For gastroesophageal reflux and acute and recurrent diabetic gastroparesis, see Full Prescribing Information for recommended dosage reductions for elderly patients, in patients with moderate or severe hepatic or renal impairment, and cytochrome P450 2D6 (CYP2D6) poor metabolizers.
NONCLINICAL TOXICOLOGY SECTION
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
A 77-week study was conducted in rats with oral metoclopramide doses up to 40 mg/kg/day (about six times the maximum recommended human dose on body surface area basis). Metoclopramide elevated prolactin levels and the elevation persisted during chronic administration. An increase in mammary neoplasms was found in rodents after chronic administration of metoclopramide [see Warnings and Precautions (5.7)]. In a rat model for assessing the tumor promotion potential, a 2-week oral treatment with metoclopramide at a dose of 260 mg/kg/day (about 35 times the maximum recommended human dose based on body surface area) enhanced the tumorigenic effect of N-nitrosodiethylamine.
Mutagenesis
Metoclopramide was positive in the in vitro Chinese hamster lung cell/HGPRT forward mutation assay for mutagenic effects and in the in vitro human lymphocyte chromosome aberration assay for clastogenic effects. It was negative in the in vitro Ames mutation assay, the in vitro unscheduled DNA synthesis assay with rat and human hepatocytes, and the in vivo rat micronucleus assay.
Impairment of Fertility
Metoclopramide at intramuscular doses up to 20 mg/kg/day (about three times the maximum recommended human dose based on body surface area) was found to have no effect on fertility and reproductive performance of male and female rats.
DESCRIPTION SECTION
11 DESCRIPTION
Metoclopramide hydrochloride, USP, the active ingredient of metoclopramide tablets, USP is a dopamine-2 receptor antagonist. Metoclopramide hydrochloride (metoclopramide monohydrochloride monohydrate) is a white or practically white, crystalline, odorless or practically odorless powder. It is very soluble in water, freely soluble in alcohol, sparingly soluble in chloroform and practically insoluble in ether. Chemically, it is 4-amino-5-chloro-N-[2-(diethylamino)ethyl]-2-methoxy benzamide monohydrochloride monohydrate. Its structural formula is as follows:
C14H22ClN3O2•HCl•H2O M.W. 354.3
Metoclopramide tablets, USP are for oral administration. Metoclopramide tablets, USP are available in 5 mg and 10 mg tablets.
- Each metoclopramide tablet, USP 5 mg contains 5 mg metoclopramide (equivalent to 5.91 mg of metoclopramide hydrochloride, USP).
- Each metoclopramide tablet, USP 10 mg contains 10 mg metoclopramide (equivalent to 11.82 mg of metoclopramide hydrochloride, USP).
Inactive Ingredients
Corn starch, dibasic calcium phosphate anhydrous, magnesium stearate, microcrystalline cellulose, and sodium starch glycolate.
