FLUOCINONIDE
Fluocinonide Topical Solution USP, 0.05%Rx Only
272a4467-b5f8-430b-8fab-7fbb07dc8114
HUMAN PRESCRIPTION DRUG LABEL
Aug 1, 2025
QUAGEN PHARMACEUTICALS LLC
DUNS: 073645339
Products 1
Detailed information about drug products covered under this FDA approval, including NDC codes, dosage forms, ingredients, and administration routes.
FLUOCINONIDE
Product Details
FDA regulatory identification and product classification information
FDA Identifiers
Product Classification
Product Specifications
INGREDIENTS (5)
Drug Labeling Information
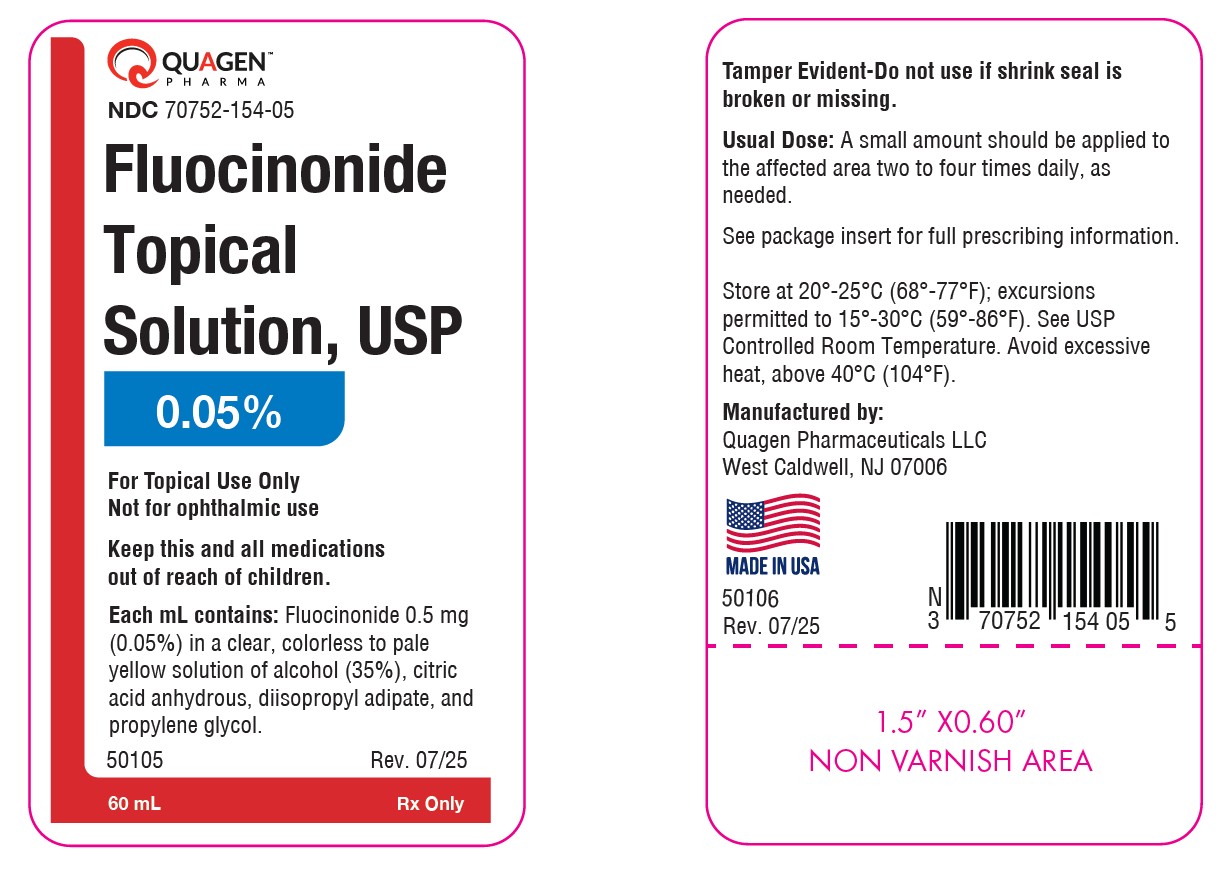
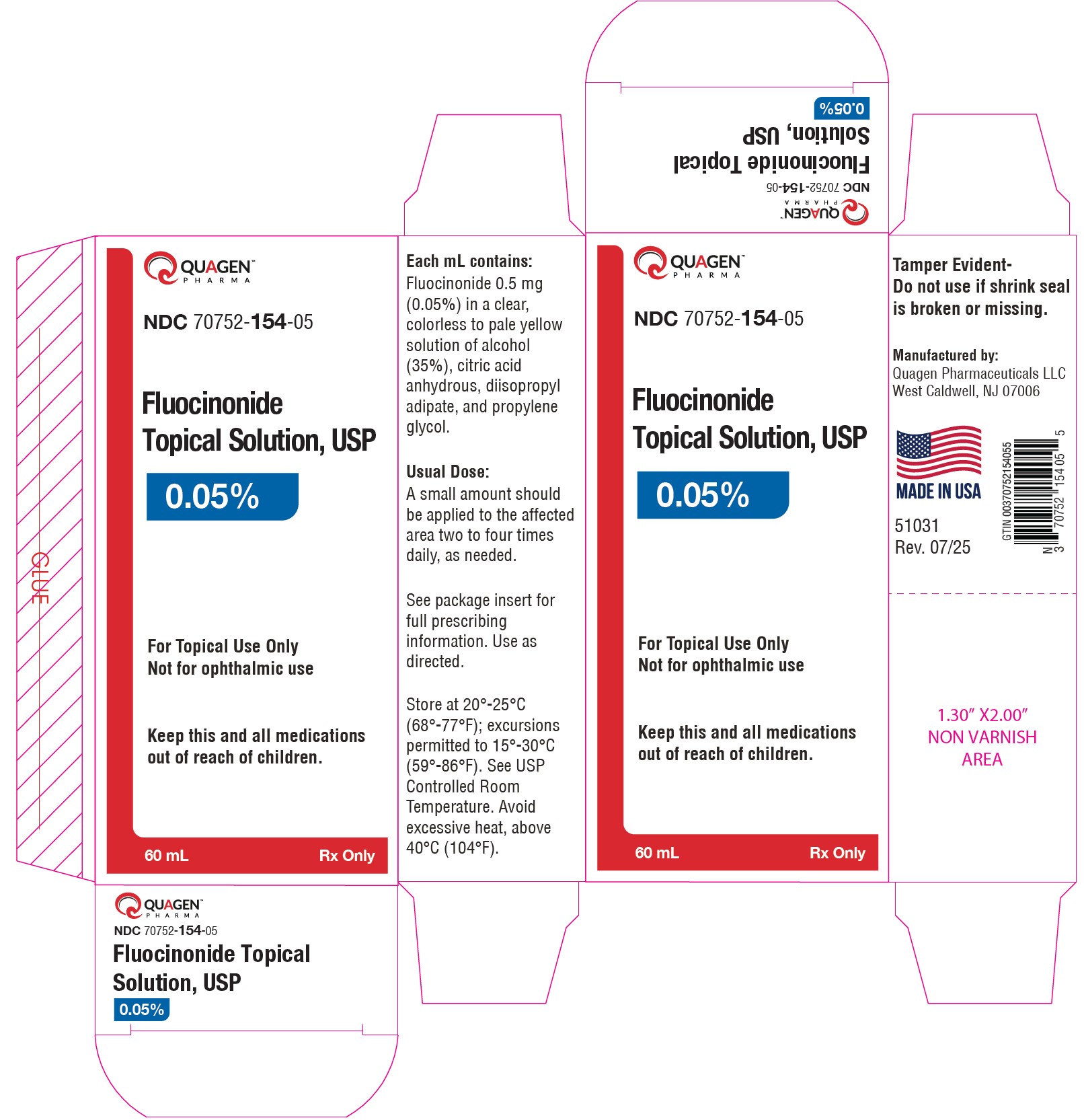
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC 70752-154-05
Fluocinonide Topical Solution, USP
0.05%
Rx only
60 mL
INDICATIONS & USAGE SECTION
INDICATIONS AND USAGE
Fluocinonide topical solution USP, 0.05% is indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses.
CONTRAINDICATIONS SECTION
CONTRAINDICATIONS
Topical corticosteroids are contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
ADVERSE REACTIONS SECTION
ADVERSE REACTIONS:
The following local adverse reactions are reported infrequently with topical corticosteroids, but may occur more frequently with the use of occlusive dressings. These reactions are listed in an approximate decreasing order of occurrence:
Burning
Itching
Irritation
Dryness
Folliculitis
Hypertrichosis
Acneiform eruptions
Hypopigmentation
Perioral dermatitis
Allergic contact dermatitis
Maceration of the skin
Secondary infection
Skin atrophy
Striae
Miliaria
To report SUSPECTED ADVERSE REACTIONS, contact Quagen Pharmaceuticals LLC. at 1-888-344-9603 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch for voluntary reporting of adverse reactions.
CLINICAL PHARMACOLOGY SECTION
CLINICAL PHARMACOLOGY
Topical corticosteroids share anti-inflammatory, anti-pruritic and vasoconstrictive actions. The mechanism of anti-inflammatory activity of the topical corticosteroids is unclear. Various laboratory methods, including vasoconstrictor assays, are used to compare and predict potencies and/or clinical efficacies of the topical corticosteroids. There is some evidence to suggest that a recognizable correlation exists between vasoconstrictor potency and therapeutic efficacy in man.
Pharmacokinetics
The extent of percutaneous absorption of topical corticosteroids is determined by many factors including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressings. A significantly greater amount of fluocinonide is absorbed from the solution than from the cream or gel formulations.
Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids. Thus, occlusive dressings may be a valuable therapeutic adjunct for treatment of resistant dermatoses. (SeeDOSAGE AND ADMINISTRATION.)
Once absorbed through the skin, topical corticosteroids are handled through pharmacokinetic pathways similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted into the bile.
DESCRIPTION SECTION
DESCRIPTION
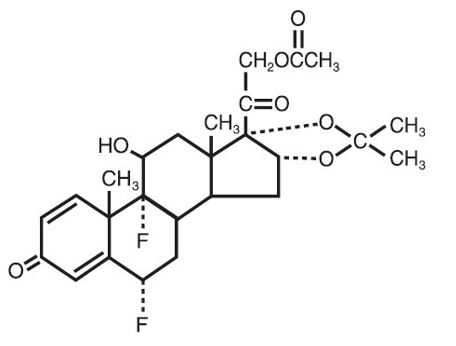
Fluocinonide topical solution USP, 0.05% is intended for topical administration. The active component is the corticosteroid fluocinonide, which is the 21-acetate ester of fluocinolone acetonide and has the chemical name pregna-1,4-diene-3,20-dione,21-(acetyloxy)-6,9-difluoro-11-hydroxy-16,17-[(1-methylethylidene)bis(oxy)]-,(6α,11β,16α)-. It has the following chemical structure:
Fluocinonide topical solution USP, 0.05% contains fluocinonide 0.5 mg/mL in a clear, colorless to pale yellow solution of alcohol (35%), citric acid anhydrous, diisopropyl adipate, and propylene glycol.
PRECAUTIONS SECTION
PRECAUTIONS
General
Systemic absorption of topical corticosteroids has produced reversible hypothalamic-pituitary-adrenal (HPA) axis suppression, manifestations of Cushing's syndrome, hyperglycemia, and glucosuria in some patients. Conditions which augment systemic absorption include the application of the more potent steroids, use over large surface areas, prolonged use, the addition of occlusive dressings, and dosage form.
Therefore, patients receiving a large dose of a potent topical steroid applied to a large surface area or under an occlusive dressing should be evaluated periodically for evidence of HPA axis suppression by using the urinary free cortisol and ACTH stimulation tests. If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent steroid.
Recovery of HPA axis function is generally prompt and complete upon discontinuation of the drug. Infrequently, signs and symptoms of steroid withdrawal may occur, requiring supplemental systemic corticosteroids.
Children may absorb proportionally larger amounts of topical corticosteroids and thus be more susceptible to systemic toxicity. (See PRECAUTIONS—Pediatric Use)
This preparation is not for ophthalmic use. Severe irritation is possible if fluocinonide solution contacts the eye. If that should occur, immediate flushing of the eye with a large volume of water is recommended.
If irritation develops, topical corticosteroids should be discontinued and appropriate therapy instituted.
As with any topical corticosteroid product, prolonged use may produce atrophy of the skin and subcutaneous tissues. When used on intertriginous or flexor areas, or on the face, this may occur even with short-term use. In the presence of dermatological infections, the use of an appropriate antifungal or antibacterial agent should be instituted. If a favorable response does not occur promptly, the corticosteroid should be discontinued until the infection has been adequately controlled.
Information for the Patient
Patients using topical corticosteroids should receive the following information and instructions:
- This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes. If there is contact with the eyes and severe irritation occurs, immediately flush with a large volume of water.
- Patients should be advised not to use this medication for any disorder other than for which it was prescribed.
- The treated skin area should not be bandaged or otherwise covered or wrapped as to be occlusive unless directed by the physician.
- Patients should report any signs of local adverse reactions especially under occlusive dressing.
- Parents of pediatric patients should be advised not to use tight-fitting diapers or plastic pants on a child being treated in the diaper area, as these garments may constitute occlusive dressings.
Laboratory Tests
The following tests may be helpful in evaluating the HPA axis suppression:
Urinary free cortisol test
ACTH stimulation test
Carcinogenesis, Mutagenesis, and Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential or the effect on fertility of topical corticosteroids.
Studies to determine mutagenicity with prednisolone and hydrocortisone have revealed negative results.
Pregnancy Category C
Corticosteroids are generally teratogenic in laboratory animals when administered systemically at relatively low dosage levels. The more potent corticosteroids have been shown to be teratogenic after dermal application in laboratory animals. There are no adequate and well-controlled studies in pregnant women on teratogenic effects from topically applied corticosteroids.
Therefore, topical corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Drugs of this class should not be used extensively on pregnant patients, in large amounts, or for prolonged periods of time.
Nursing Mothers
It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in breast milk. Systemically administered corticosteroids are secreted into breast milk in quantities not likely to have a deleterious effect on the infant. Nevertheless, caution should be exercised when topical corticosteroids are administered to a nursing woman.
Pediatric Use
Pediatric patients may demonstrate greater susceptibility to topical corticosteroid-induced HPA axis suppression and Cushing's syndrome than mature patients because of a larger skin surface area to body weight ratio.
Hypothalamic-pituitary-adrenal (HPA) axis suppression, Cushing's syndrome, and intracranial hypertension have been reported in children receiving topical corticosteroids.
Manifestations of adrenal suppression in children include linear growth retardation, delayed weight gain, low plasma cortisol levels, and absence of response to ACTH stimulation.
Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Administration of topical corticosteroids to children should be limited to the least amount compatible with an effective therapeutic regimen. Chronic corticosteroid therapy may interfere with the growth and development of children.
OVERDOSAGE SECTION
OVERDOSAGE
Topically applied corticosteroids can be absorbed in sufficient amounts to produce systemic effects. (SeePRECAUTIONS.)
DOSAGE & ADMINISTRATION SECTION
DOSAGE AND ADMINISTRATION
Fluocinonide topical solution USP, 0.05% is generally applied to the affected area as a thin film from two to four times daily depending on the severity of the condition.
Occlusive dressings may be used for the management of psoriasis or recalcitrant conditions.
If an infection develops, the use of occlusive dressings should be discontinued and appropriate antimicrobial therapy instituted.
HOW SUPPLIED SECTION
HOW SUPPLIED
Fluocinonide Topical Solution USP, 0.05% is a clear, colorless to pale yellow solution supplied in plastic squeeze bottle:
60 mL - NDC 70752-154-05
Tamper Evident - Do not use if shrink seal is broken or missing
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F). See USP Controlled Room Temperature. Avoid excess heat, above 40°C (104°F).
Manufactured by:
Quagen Pharmaceuticals LLC
West Caldwell, NJ 07006
52037
Rev. 04/25
