Regulatory Information
HSA regulatory responsibility and product classification details
Regulatory Responsibility
Product Classification
Formulation Information
INJECTION, POWDER, FOR SOLUTION
**4.2 Posology and method of administration** Reblozyl treatment should be initiated by a physician experienced in treatment of haematological diseases. Posology Prior to each Reblozyl administration, the haemoglobin (Hb) level of patients should be assessed. In case of a red blood cell (RBC) transfusion occurring prior to dosing, the pre-transfusion Hb level must be considered for dosing purposes. _Myelodysplastic syndromes_ The recommended starting dose of Reblozyl is 1.0 mg/kg administered once every 3 weeks by subcutaneous injection. In patients who are not RBC transfusion-free after at least 2 consecutive doses at the 1.0 mg/kg starting dose, the dose should be increased to 1.33 mg/kg. If patients are not RBC transfusion-free after at least 2 consecutive doses at the 1.33 mg/kg dose level, the dose should be increased to 1.75 mg/kg. The dose increase should not occur more frequently than every 6 weeks (2 administrations) and should not exceed the maximum dose of 1.75 mg/kg every 3 weeks. The dose should not be increased immediately after a dose delay. For patients with a pre-dose Hb level of > 9 g/dL and who have not yet achieved transfusion independence, a dose increase may be required at the physician’s discretion; the risk of Hb increasing above the target threshold with concomitant transfusion cannot be excluded. If a patient loses response (i.e., transfusion independence), the dose should be increased by one dose level. _β-thalassaemia_ The recommended starting dose of Reblozyl is 1.0 mg/kg administered once every 3 weeks by subcutaneous injection. In patients who do not achieve a response after ≥ 2 consecutive doses (6 weeks), at the 1.0 mg/kg starting dose, the dose should be increased to 1.25 mg/kg. Minimum response is defined as a reduction in RBC transfusion burden by at least a third after ≥ 2 consecutive doses (6 weeks), at the 1.0 mg/kg starting dose. The dose should not be increased beyond the maximum dose of 1.25 mg/kg every 3 weeks. If a patient loses response (if the RBC transfusion burden increases again after an initial response) the dose should be increased by one dose level. _MDS and β-thalassaemia_ _Dose reduction and dose delay_ In case of Hb increase > 2 g/dL within 3 weeks of luspatercept treatment in absence of transfusion, the Reblozyl dose should be reduced by one dose level. If the Hb is ≥ 11.5 g/dL in the absence of transfusion for at least 3 weeks, the dose should be delayed until the Hb is ≤ 11.0 g/dL. If there is also a concomitant rapid increase in Hb (> 2 g/dL within 3 weeks in absence of transfusion), a dose reduction to one step down (minimum 0.8 mg/kg) should be considered after the dose delay. Dose should not be reduced below 0.8 mg/kg. Dose reductions during treatment with luspatercept are provided below. 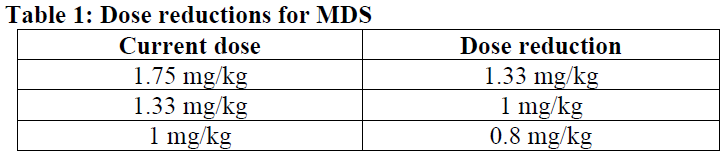 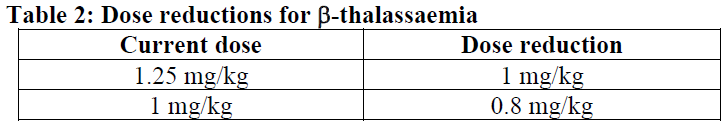 If patients experience persistent treatment-related Grade 3 or higher adverse reactions (see section 4.8 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_), the treatment should be delayed until toxicity has improved or returned to baseline. After a dose delay, patients should be re-started at their previous dose or at reduced dose as per dose reduction guidance. _β-thalassaemia_ In case of extramedullary haematopoietic (EMH) masses causing serious complications (see sections 4.4 and 4.8 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_), the treatment should be discontinued. _MDS and β-thalassaemia_ _Missed doses_ In case of a missed or delayed scheduled treatment administration, the patient should be administered Reblozyl as soon as possible and dosing continued as prescribed with at least 3 weeks between doses. _Patients experiencing a loss of response_ If patients experience a loss of response to Reblozyl, causative factors (e.g. a bleeding event) should be assessed. If typical causes for a loss of haematological response are excluded, dose increase should be considered as described above for the respective indication being treated. _Discontinuation_ Reblozyl should be discontinued if patients do not experience a reduction in transfusion burden after 9 weeks of treatment (3 doses) at the maximum dose level if no alternative explanations for response failure are found (e.g. bleeding, surgery, other concomitant illnesses) or if unacceptable toxicity occurs at any time. Special populations _Elderly_ No starting dose adjustment is required for Reblozyl (see section 5.2 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). _Hepatic impairment_ No starting dose adjustment is required for patients with total bilirubin (BIL) > upper limit of normal (ULN) and/or alanine aminotransferase (ALT) or aspartate aminotransferase (AST) < 3 x ULN (see section 5.2 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). No specific dose recommendation can be made for patients with ALT or AST ≥ 3 x ULN or liver injury CTCAE Grade ≥ 3 due to lack of data (see section 5.2 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). _Renal impairment_ No starting dose adjustment is required for patients with mild to moderate renal impairment (estimated glomerular filtration rate \[eGFR\] < 90 and ≥ 30 mL/min/1.73 m2). No specific dose recommendation can be made for patients with severe renal impairment (eGFR < 30 mL/min/1.73 m2) due to lack of clinical data (see section 5.2 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). Patients with renal impairment at baseline should be closely monitored for renal function as per standard of care. _Paediatric population_ There is no relevant use of Reblozyl in the paediatric population for the indication of myelodysplastic syndromes, or in paediatric patients less than 6 months of age in β-thalassaemia. For non-clinical data, see section 5.3 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_. The safety and efficacy of Reblozyl in the paediatric patients aged from 6 months to less than 18 years have not yet been established in β-thalassaemia. For non-clinical data, see section 5.3 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_. Method of administration For subcutaneous use. After reconstitution, Reblozyl solution should be injected subcutaneously into the upper arm, thigh or abdomen. The exact total dosing volume of the reconstituted solution required for the patient should be calculated and slowly withdrawn from the single-dose vial(s) into a syringe. The recommended maximum volume of medicinal product per injection site is 1.2 mL. If more than 1.2 mL is required, the total volume should be divided into separate similar volume injections and administered across separate sites. If multiple injections are required, a new syringe and needle must be used for each subcutaneous injection. No more than one dose from a vial should be administered. If the Reblozyl solution has been refrigerated after reconstitution, it should be removed from the refrigerator 15–30 minutes prior to injection to allow it to reach room temperature. This will allow for a more comfortable injection. For instructions on reconstitution of the medicinal product before administration, see section 6.6 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_.
SUBCUTANEOUS
Medical Information
**4.1 Therapeutic indications** Reblozyl is indicated for the treatment of adult patients with transfusion-dependent anaemia due to very low, low and intermediate-risk myelodysplastic syndromes (MDS) with ring sideroblasts, who had an unsatisfactory response to or are ineligible for erythropoietin-based therapy (see section 5.1 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). Reblozyl is indicated for the treatment of adult patients with transfusion-dependent anaemia associated with beta-thalassaemia (see section 5.1 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_). Limitation of use Reblozyl is not indicated for use as a substitute for red blood cell (RBC) transfusions in patients who require immediate correction of anaemia.
**4.3 Contraindications** - Hypersensitivity to the active substance or to any of the excipients listed in section 6.1 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_. - Pregnancy (see section 4.6 – _please refer to the Product Insert/Patient Information Leaflet published on HSA for the full drug information_).
B03XA06
luspatercept
Manufacturer Information
BRISTOL-MYERS SQUIBB (SINGAPORE) PTE. LTD.
Patheon Italia S.p.A.
Active Ingredients
Documents
Package Inserts
REBLOZYL POWDER FOR SOLUTION FOR INJECTION_PI_CLEAN.pdf
Approved: May 31, 2023
